Abstract
Nail-patella syndrome (NPS) is a rare genetic disease characterized by dysplastic nails, patella abnormalities, skeletal malformation, and chronic pain. Although chronic pain in NPS is mainly due to bone and musculoskeletal symptoms, it can also result from neurological dysfunction. Conventional analgesics are often insufficient to relieve NPS-associated chronic pain. Cannabinoids, which act on the serotonergic and/or noradrenergic pain systems, may therefore represent valuable non-psychoactive alternatives for managing pain in these patients. The effectiveness and safety of synthetic cannabidiol (CBD) for the management of NPS-associated pain was assessed using real-world data from a pilot cohort of patients with NPS who received a 3-month treatment with oral CBD. The treatment (median dose of 900 mg/day) was associated with a significant reduction in pain intensity (mean score of 7.04 ± 0.24 at initiation versus 4.04 ± 0.38 at 3 months, N = 28, p < 0.0001), which correlated with changes in the peripheral concentration of noradrenaline (r = 0.705, 95% CI [0.44–0.86], p < 0.0001). Health-related quality of life and other NPS-associated symptoms also improved in most patients. CBD treatment was well tolerated and no elevations in liver enzyme levels were reported. Synthetic CBD therefore appears to be a safe and effective treatment option for managing NPS-associated chronic pain.
Similar content being viewed by others
Introduction
Chronic pain is a major concern for patients with nail-patella syndrome (NPS) and has a major impact on patient quality of life (QoL)1. This rare autosomal genetic disease is caused by dominant heterozygous loss-of-function mutations in the LMX1B gene, and is characterized by dysplastic nails, absent or hypoplastic patellae, and skeletal abnormalities2,3,4. Renal, gastrointestinal, ocular, and neurological symptoms are also present in some cases2,3,4,5. Bone symptoms and cartilage inflammation are the main causes of chronic pain in patients with NPS6,7. However, as the LMX1B protein is also a key homeodomain transcription factor for the differentiation of dopaminergic and serotonergic neurons during embryogenesis8,9,10,11,12,13, LMX1B mutations may also trigger cognitive disorders (e.g., symptoms of attention deficit hyperactivity disorder and major depressive disorder)5 and pain sensation anomalies3, both of which are aggravating factors for chronic pain. In particular, patients with NPS have arthropathies that cause recurrent nociceptive pain14 and impaired perception of afferent sensory neuron stimuli leading to numbness, tingling, and neuropathic pain, which predominantly affects the distal limbs in a non-peripheral nerve or dermatomal pattern and can become chronic15.
The interweaving of chronic musculoskeletal pain with nociceptive, neuropathic, and psychological components makes the pain associated with NPS difficult to manage with conventional analgesics. Indeed, multiple peripheral pathways are likely involved in pain signaling in patients with tissue and nerve damage and mixed pain syndromes such as NPS, although pain perception is probably mediated by a central processing mechanism that filters the various peripheral pain signals16. Peripheral pain signals are mediated by both the ascending (spinal cord to the thymus and cortex, with a parallel pathway to the limbic brain) and descending (midbrain and brainstem projecting to the dorsal horn of the spinal cord) control pathways. The descending pathway represents a mechanism through which the transmitted pain signal may be facilitated (enhancing pain sensations) or inhibited (reducing pain sensations). It is alterations in this descending control system that are believed to modulate the levels of perceived pain and contribute to chronic pain17. The monoamine neurotransmitters, noradrenaline and serotonin (5-hydroxytryptamine; 5-HT), are key modulators of the descending pain control pathway16. Alterations in the levels of serotonin and noradrenaline, and in key components of the synthesis and signaling pathways of these monoamines, have already been identified in patients with mastocytosis and fibromyalgia18,19,20, both of which are syndromes with diffuse chronic pain, depression, and cognitive impairment profiles similar to those of NPS21,22. Although the baseline peripheral serotonergic and noradrenergic state of patients with NPS has not yet been documented, the LMX1B gene mutations carried by these patients likely lead to neurological malformations that impact the peripheral and central pain systems. Rescue of the serotonergic and/or noradrenergic inhibitory systems may therefore help relieve or prevent the establishment of chronic pain in patients with NPS.
The limited effectiveness of conventional analgesics in some patients with chronic pain or mixed pain syndromes has led to an increase in studies evaluating the effects and underlying mechanisms of action of endocannabinoids, synthetic cannabinoids and phytocannabinoids for pain management23. Laboratory studies have generated substantial evidence supporting the hypothesis of cannabinoid-induced analgesia, indicating that the antinociceptive actions of these compounds are mediated mainly by their effects on the serotonergic and adrenergic pathways24. In particular, cannabidiol (CBD), a phytocannabinoid that has no psychoactive effect, has been shown to act on the serotonergic and adrenergic pathways through its 5-HT1a receptor agonistic properties, its potential to rebalance the tryptophan catabolic pathway towards serotonin synthesis, and its ability to modulate noradrenaline release25,26,27,28,29,30,31. Although high quality evidence from large randomized clinical trials is currently lacking23, medicinal cannabinoids have already been shown to provide effective pain relief in patients with refractory or chronic pain associated with other conditions, including mastocytosis and fibromyalgia32,33,34,35,36. Moreover, the safety and tolerability profile of oral CBD is considered acceptable, with mostly mild and moderate adverse events (AEs)37.
The main aim of the current study was therefore to evaluate the real-world effectiveness of a 3-month treatment with synthetic pharmaceutical-grade CBD for the management of chronic pain in patients with NPS. The effects on pain intensity, health-related QoL and NPS-associated symptoms were evaluated at the end of the treatment period. Product safety and biological parameters were also assessed. In particular, serum levels of serotonin and noradrenaline were evaluated, as an indicator of peripheral serotonergic and noradrenergic state, to determine whether these data provided useful information for optimizing the management of NPS-associated chronic pain.
Results
Study participants
Data from 32 CBD-treated patients with NPS were included in the study. This study population was made up of 21 females (65.6%) and 11 males (34.4%), and included 7 subjects ≤ 18 years old (21.9%). The median age was 40.5 years (range: 10–66 years). The demographic and clinical characteristics of the patients are shown in Table 1. None of the patients had renal insufficiency. Of the included patients, 28 completed the 3-month treatment course, whereas 4 adult patients (12.5%) had to stop the treatment within the first month because of severe asthenia. The patients who withdrew were excluded from the effectiveness analysis. The median dose of oral CBD at Month 3 (M3) was 900 mg/day (range: 500–1200 mg/day, N = 28), with most patients reaching this dose at M1.
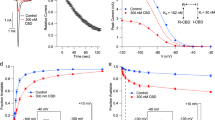
Pain intensity
The mean (± SEM) numerical rating scale (NRS) pain score significantly decreased from 7.04 ± 0.24 before treatment to 4.04 ± 0.38 after 3 months of CBD therapy (N = 28 with paired data, p < 0.0001) (Fig. 1a; Table 2). NRS pain scores decreased by two or more points in 71.4% (20/28) of patients. None of the patients had an increase in NRS score. Moreover, 63.0% (17/27) of patients who initially took analgesics (Table 1) stopped all other analgesic medications between M2 and M3 of CBD treatment. Among the 17 patients who stopped using other analgesics, 15 of them stopped using tramadol. For 10 of these patients, the reason given for stopping tramadol was superior effectiveness of CBD. For the remaining 5 patients, the effectiveness of the two treatments was considered similar and concern over addiction to tramadol was reported as the key motivation for stopping this treatment. In addition, only small numbers of patients reported occasionally using paracetamol (3/27) and NSAIDs (4/27), and 3 patients who continued taking morphine reduced the dose administered by 50%.
Changes in pain scores and their correlation with changes in plasma noradrenaline concentrations between baseline and 3 months (M3) of synthetic cannabidiol treatment. (a) Mean (± SEM) numerical rating scale (NRS) pain scores at baseline (month 0, M0) and M3 for subjects with paired data (N = 28). ***p < 0.0001. (b) Correlation analysis between the decrease in NRS pain scores and the changes in plasma noradrenaline concentration from M0 to M3 for each patient with paired data (N = 28, Spearman correlation and simple linear regression).
Health-related quality of life
QoL related to physical and mental health also globally improved post-treatment (N = 27, Fig. 2a). Mean scores were higher than at baseline for all 8 domains, and the difference was statistically significant for 4 domains (RE, MH, SF and BP, p < 0.05, Table S1). Moreover, individual data showed that QoL scores improved in most patients in each ___domain (48–70% of patients, Fig. 2b).
Health-related quality of life (QoL) in patients with NPS assessed using the RAND 36-Item Short Form (SF-36) health survey at baseline (M0) and after 3 months (M3) of treatment with synthetic cannabidiol. (a) Radar plots of mean QoL scores for the 8 domains of physical and mental health in subjects with paired data (N = 27): physical functioning (PF), role limitations due to physical health problems (RF), bodily pain (BP), perception of general health (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (MH). *p < 0.05, and **p < 0.001. (b) Individual changes between baseline and M3 in scores for the 8 domains presented as stacked histograms showing the number and percentage of patients by category for each ___domain: health-related QoL improved, unchanged or worsened at M3 (N = 27).
NPS-associated symptoms
At baseline, 56.3% (18/32) of the patients had constipation (Table 1), which had resolved in most cases at M3 (76.5%, 13/17). Diarrhea was initially reported in 18.8% (6/32) of patients, and did not resolve following treatment. One patient (3.1%) with constipation at initiation reported diarrhea at M3. Moreover, 78.1% (25/32) of the patients initially reported having symptoms of attention disorders, 81.3% (26/32) reported symptoms of sleep disorders, and 68.8% (22/32) reported having symptoms of both. These symptoms had improved or resolved at M3 in 25.0% (7/28) of patients for attention disorder symptoms, and in 46.4% (13/28) of patients for sleep disorder symptoms.
Biological parameters
The baseline mean plasma noradrenaline concentration was above the upper limit of normal (ULN) of 2.2 nmol/L (3.64 ± 2.72 nmol/L, Table 1), and most of the patients (81.3%, 26/32) had higher-than-normal plasma noradrenaline concentrations (Table 2). The baseline mean blood serotonin concentration was < ULN of 0.90 µmol/L in adults (0.86 ± 0.37 µmol/L), but > ULN of 0.75 µmol/L in subjects ≤ 18 years old (0.85 ± 0.28 µmol/L, Table 1). Overall, 48.2% of the patients (13/27, after excluding one patient who already took a selective serotonin reuptake inhibitor [SSRI] at M0) had a higher-than-normal serotonin concentration (Table 2). The other measured biological parameters were within the normal ranges (Table 1).
Following the 3-month CBD treatment, no significant changes were observed in the levels of the biological markers that were within the normal ranges at baseline (Table S2). The mean plasma noradrenaline concentration was still > ULN (3.59 ± 3.23 nmol/L), but analyses of changes in individual patients revealed a trend toward decreased plasma noradrenaline concentrations at M3, and fewer patients had concentrations > ULN at M3 than at baseline (57.1%, 16/28, Table 2). For serotonin, mean blood concentrations were > ULN in both adults and subjects ≤ 18 years old (0.93 ± 0.45 and 1.04 ± 0.51 µmol/L, respectively, Table 2) and tended to be higher at M3 compared to baseline. After excluding four patients who took SSRIs, 63.6% (14/22) of patients had higher-than-normal serotonin concentrations at M3.
Correlation analyses
The relationship between the change (Δ: M3-M0) in NRS pain scores and neurotransmitter concentrations was further assessed by correlation analyses. A significant positive correlation was found between Δ NRS pain scores and Δ noradrenaline concentrations (N = 28, r = 0.705, 95%CI [0.44–0.86], p < 0.0001). These data fitted the simple linear regression model, with a moderate effect (r² = 0.334 ± 0.095, p = 0.0013; Fig. 1b). No correlation was found between Δ NRS pain scores and Δ serotonin concentrations (N = 19, excluding patients with paired data who took SSRIs: r = 0.343, 95%CI [–0.146 to 0.697], p = 0.150).
Safety
Asthenia led to treatment discontinuation in 12.5% (4/32) of patients before the M1 visit. This effect is a common non-serious AE reported with cannabinoid use. No elevations in the levels of liver enzymes were observed following the 3-month CBD therapy.
Discussion
This study provided the first evidence supporting the effectiveness of a dose-increasing schedule of oral CBD for reducing pain intensity in patients with NPS. The treatment also led to improvements in several NPS-associated symptoms and in health-related QoL in most of the patients. No major safety issues were encountered during the study period, apart from common non-serious AEs already known to be associated with CBD. Notably, we found a significant correlation between decreased NRS pain scores and changes in plasma noradrenaline concentrations at 3 months.
In a pilot study conducted in 44 patients with mastocytosis and refractory pain, oral treatment with synthetic CBD was shown to significantly reduce pain from one month of treatment, with a mean decrease in NRS pain score of three points34. These patients reported additional improvements in mood, sleep, asthenic sensations, and anxiety after 3 months of treatment. In this previous study, the median dose of CBD administered was lower than that used in our study involving patients with NPS (300 mg/day vs. 900 mg/day), but the mean reduction in NRS score was similar to that observed in the patients with NPS at 3 months post-treatment. Moreover, as in our cohort, a subset of the patients with mastocytosis treated with CBD were able to discontinue or reduce their previous analgesic medications. CBD may also be a promising treatment for pain in patients with sickle cell disease, as indicated by a report involving a young patient refractory to conventional analgesics who achieved pain relief with oral synthetic CBD after only 2 weeks of treatment33. Several other studies have reported on the beneficial effects of oral CBD for relieving chronic pain of various origins, as well as for improving sleep and QoL38,39. However, despite these encouraging results and a relatively good safety profile, clinical evidence demonstrating the effectiveness and safety of synthetic CBD remains too limited to provide clear recommendations for its use in chronic pain management.
The mechanism of action of CBD on chronic pain is also not well understood, and its specific role in patients with NPS and in the context of LMX1B loss of function has not yet been investigated. In the brain, LMX1B is involved in specific neuronal circuits. In the dopaminergic system, LMX1B is required for the differentiation, survival and architectural organization of the dopaminergic tissue in the isthmic organizer region10,12, and for the maintenance of the differentiated phenotype of mesencephalic dopaminergic neurons. In the serotonergic system, loss of LMX1B functionality has been shown to lead to dedifferentiation and reduced survival of 5-HT nerves after birth, particularly in the raphe nuclei9,13. A lower pain threshold and reduced sensitivity to SSRIs have also been demonstrated in an LMX1B knock-out mouse model13, with these alterations likely being due to the effects of loss of LMX1B on the descending pain signaling system.
Several studies have shown that a reduction in descending pain signal inhibition may be a shared characteristic of patients with chronic pain, but the exact role of noradrenaline and serotonin is not well known as these neurotransmitters can have nociceptive, antinociceptive, or biphasic effects depending on the levels of these molecules, the type of receptor, and the anatomical region17,40. Only a few studies have investigated the changes in plasma monoamine levels that occur in the context of chronic pain. Most of these studies analyzed serotonin concentrations and all failed to show differences between chronic-pain and pain-free groups41,42,43,44. Moreover, the two studies that assessed plasma noradrenaline levels in patients with chronic pain found inconsistent findings43,45. On the one hand, Parent et al. showed a deficit in descending pain inhibition and lower plasma concentrations of noradrenaline and metanephrines in subjects with chronic musculoskeletal pain compared to pain-free controls43. On the other hand, Tsigos et al. showed that noradrenaline levels positively correlated with the severity of neuropathic pain in patients with diabetes45.
In our study, most of the patients with NPS had higher-than-normal plasma noradrenaline concentrations at baseline, and these concentrations tended to decrease following CBD treatment. We found that this decline in plasma noradrenaline concentration from baseline correlated significantly with a decrease in pain scores. However, we cannot exclude the possibility that the changes detected in the plasma noradrenaline concentrations may not have provided an accurate reflection of the changes occurring at the central level under CBD treatment. While in the spinal cord noradrenaline blocks nociceptive transmission, both antinociception and pronociception have been reported after noradrenaline release in the brain46,47. CBD could therefore act differently at the peripheral and central levels. Synthetic CBD could directly act as an agonist of α2 adrenergic receptors or help increase stimulation of α2 receptors by noradrenaline48,49 to block pain signal transmission to the central system. Moreover, although no direct correlation was found between Δ NRS pain scores and Δ blood serotonin concentrations, we observed a trend toward an increase in peripheral serotonin concentrations after CBD treatment, which may have contributed to the reduction in pain in the treated patients. Indeed, while at the peripheral level CBD could directly agonize 5-HT antinociceptive receptors on C fibers, CBD could also increase central serotonin levels through its effect on the kynurenine/tryptophan ratio, as suggested by in vitro findings31,50. However, central concentrations of these molecules could not be recorded in our study to confirm this hypothesis. It has also been shown in a mouse neuropathic pain model that repeated CBD administration could desensitize 5-HT1A autoreceptors, which could thus enhance the antinociceptive effects of CBD. The combination of these various effects of CBD on central and peripheral neurotransmitters likely explains the effectiveness of CBD for pain relief in our population of patients with NPS.
This study has several limitations. The rarity of the disease did not allow for the recruitment of a large number of subjects, which may have limited the power of this study to detect significant differences between some of the variables over time and prevented any subgroup analyses. The real-world design of the study did not allow for the inclusion of a control group to directly compare the effectiveness of CBD with a placebo or other analgesics that modify the monoaminergic system, such as SNRIs. While such future studies could in theory be useful for confirming the efficacity of CBD, our evidence from real-world clinical practice indicates that pain in patients with NPS is often resistant to standard analgesics and that these patients may be at increased risk of developing serotonin syndrome after taking SNRIs. The study period was short and did not allow assessment of the long-term effects and safety of the treatment. Although the lack of serious AEs indicated a good safety profile for CBD in our patient population, only limited evidence is available supporting the safety and tolerability of CBD in patients with renal insufficiency51, which affects 10–40% of NPS patients52. As renal insufficiency was not present in any of the patients included in our cohort, the safety of CBD in NPS patients with renal manifestations requires further evaluation in future studies. The results of this study provide potential insights into the mechanism of action of CBD on noradrenergic and serotonergic pathways, but these mechanisms need to be further elucidated in experimental studies, more specifically in LMX1B loss-of-function models. In addition, the clinical effectiveness of CBD in patients with NPS needs to be confirmed in larger prospective controlled trials. These additional data will help to confirm the potential role of synthetic CBD as a valuable non-psychoactive analgesic for relieving NPS-associated chronic pain, and allow for more extensive assessments of its psychological impact in patients with NPS, in particular the impact of CBD on depression.
Conclusion
Oral treatment with synthetic CBD was associated with a significant reduction in pain in most of the patients with NPS included in our study, and led to improvements in most of the NPS-associated symptoms analyzed. Hence, synthetic oral CBD appears to be a safe and effective treatment option for NPS-associated pain, and may be an alternative to conventional analgesics for managing chronic pain in this pathology.
Methods
Study design and ethics
This observational, open-label, pilot study was conducted using real-world data collected during routine clinical practice in the department of pain management and palliative care of the Necker-Enfants Malades Hospital (Assistance Publique–Hôpitaux de Paris [AP-HP], Paris, France) between 02 January 2022, and 01 July 2023. The institutional review board of the reference center for constitutional bone diseases, the MOC-Necker-Hospital (Paris, France), approved the study. In line with French legislation on studies conducted as part of routine clinical practice, the study protocol was registered by the AP-HP the 16/05/2022 under the reference MR004-2022-0516123418. The study was performed in accordance with the Declaration of Helsinki and its subsequent amendments, good clinical practice guidelines (CHMP/ICH/135/1995 and integrated addendum), and the general data protection regulation (GDPR, Regulation (EU) N°2016/679 and local regulations). Written informed consent was obtained from the patients, or their legal guardians for children (< 18 years old), for the publication of their data included in this article.
Participants
Patients with NPS were referred to the pain care unit if they had persistent chronic muscle, joint, bone or abdominal pain (defined as an NRS pain score of 4 or more for more than 3 months), despite prior treatment with conventional analgesics (e.g., paracetamol, non-steroidal anti-inflammatory drugs [NSAIDs], opioids, and serotonin and norepinephrine reuptake inhibitors [SNRIs]) or poor tolerance to these prior treatments. The data used in the current study were extracted from the medical records of patients referred to the unit with a confirmed diagnosis of NPS caused by an identified LMX1B variant, without hepatic or cardiac insufficiency or a history of consumption of any cannabis or cannabidiol product, who were prescribed CBD according to regular clinical practice of the department.
Administration of CBD
The synthetic CBD prescribed to the patients was Canapure® PH), manufactured by Symrise (Holzminden, Germany) from the limonene of orange peels according to GMP guidelines. Canapure® PH was obtained via the Belgian pharmaceutical retailer PharmaChemicals®, which re-analyzed the CanapurePH® to confirm compliance to the German Drug Codex (DAC) monograph. The substance is nature-identical to CBD, with no detectable traces of the psychoactive compound tetrahydrocannabinol (THC). Doses were prepared on demand and provided in the form of oral capsules.
Based on clinical experience within the department of pain management for patients with other genetic disorders (e.g., erythromelalgia, Hailey-Hailey disease, Olmsted Syndrome, carriers of FOXP1 mutations, and sickle cell disease) and on the results of the study published by Rossignol et al. 34 on the effective use of CBD in patients with mast cell disease, CBD was initiated (at M0) at a dosage of 50 mg t.i.d (150 mg/day), and increased to 100 mg t.i.d at day (D)7, then by 100 mg t.i.d every 7 days depending on pain intensity.
Patient follow-up
Pain intensity, heath-related QoL, NPS-associated symptoms (gastrointestinal, attention and sleep disorder symptoms) and the occurrence of AEs, were evaluated by the physician during teleconsultations on day D7, D15, D21, and during face-to-face consultations at M1, M2, and M3. These visits were part of the routine follow-up of the patients. Patients were asked to keep a record of their pain and consumption of other analgesics in a diary, which was then evaluated at the monthly visits. A blood sample, used for routine liver enzyme assays and evaluation of other biological markers, was also taken during the monthly visits. The dose of CBD was reduced if AEs occurred and increased if the pain score had not decreased by more than 20% compared to baseline.
Assessment criteria
The primary assessment criterion was the effectiveness of CBD for relieving pain after 3 months of treatment. The secondary assessment criteria were the safety of CBD therapy, and its effectiveness for improving QoL related to physical and mental health and for relieving symptoms associated with NPS. Changes in biological parameters between baseline and M3 were also assessed, including changes in the peripheral levels of neurotransmitters (serotonin [µmol/L], noradrenaline [nmol/L], and dopamine [nmol/L]), and of tryptophan (µmol/L) and factors involved in its metabolism (i.e., kynurenine [µmol/L], IDO1 [% activity] and tryptase [µg/L]).
Assessment methods
Pain intensity
Pain intensity was measured on a numerical rating scale (NRS) ranging from 0 (“no pain”) to 10 (“worst imaginable pain”).
Health-related quality of life
Physical and mental health was assessed using the RAND 36-Item Short Form (SF-36) Health Survey (version 1.0), previously developed as part of the Medical Outcomes Study53. This survey is one of the most widely used measures of health-related QoL and has been applied to various populations. It consists of 36 items covering 8 domains of physical and mental health: physical functioning (PF), role limitations due to physical health problems (RF), bodily pain (BP), perception of general health (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (MH). Scoring was done using a scale from 0 to 100, with higher scores indicating more favorable physical functioning and psychological well-being. Patients were evaluated at baseline and M3.
NPS-associated symptoms
Gastrointestinal symptoms, and symptoms of attention, and sleep disorders, which have been reported to be associated with NPS5, were assessed by open-ended questions to the patients.
Biological parameters
Whole blood serotonin concentrations were measured using ultra-performance liquid chromatography (UPLC) with fluorometric detection. Plasma levels of adrenaline, noradrenaline and dopamine were measured by UPLC using the ChromSystems kit for catecholamines in plasma (ChromSystems Instruments & Chemicals GmbH, Munich, Germany). Plasma samples were taken after the patients had been resting undisturbed in a quiet environment for at least 5 min. Tryptophan and kynurenine were assayed using UPLC coupled to coulometric detection, and IDO1 activity was estimated by calculating the kynurenine/tryptophan ratio. Tryptase was quantified using the ImmunoCAP™ Tryptase kit and Phadia™ 250 automated instrument (Thermo Fischer Scientific Inc., France).
The normal ranges for biological parameters were provided by the biological analysis laboratory (Laboratory of Biochemistry and Molecular Biology, Hôpital Lariboisière, AP-HP, Paris). Normal whole blood serotonin concentrations should range between 0.1 and 0.9 µmol/L for adults and between 0.09 and 0.75 µmol/L for subjects ≤ 18 years old. The plasma upper limit of normal (ULN) was 2.2 nmol/L for noradrenaline, 0.45 nmol/L for adrenaline, 0.56 nmol/L for dopamine, and 8.4 µg/L for tryptase. The normal plasma ranges for tryptophan and kynurenine were 35–90 µmol/L and 1.0–3.0 µmol/L, respectively, and the normal level for IDO activity was < 5%.
Liver function tests, including alanine transaminase (ALT), aspartate transaminase (AST), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), serum bilirubin, and total protein and albumin, were performed according to standard clinical protocols.
Adverse events
AEs were recorded using the standard hospital system, based on Medical Dictionary for Regulatory Activities (MedDRA) terminology, and graded as severe (serious or life-threatening), moderate (non-serious but requiring treatment discontinuation), or mild (non-serious allowing treatment continuation).
Statistical analysis
Descriptive data are presented as the mean ± standard deviation (SD) or standard error of the mean (SEM), median (range), or number (N) and percentage (%). Baseline and M3 NRS pain scores were compared using the paired two-tailed t-test, and SF-36 scores were compared using the Wilcoxon test. Spearman correlation and simple linear regression were used for correlation analyses. The Spearman correlation coefficient was tested for significance against the null hypothesis using a two-tailed t-test, and the simple linear regression was tested using a F test. The threshold for statistical significance was set to p < 0.05. All statistical analyses were performed using the Prism software (version 8.0, GraphPad Software, San Diego, CA).
Data availability
All data supporting the findings of this study are available within the paper and its Supplementary Information.
References
Geerts-Crabbe, L. et al. Difficulties adapting to nail-Patella syndrome: a qualitative study of patients’ perspectives. J. Genet. Couns. 28, 1011–1020. https://doi.org/10.1002/jgc4.1153 (2019).
Bongers, E. M., Gubler, M. C. & Knoers, N. V. Nail-patella syndrome. Overview on clinical and molecular findings. Pediatr. Nephrol. 17, 703–712. https://doi.org/10.1007/s00467-002-0911-5 (2002).
Sweeney, E. et al. in GeneReviews((R)) (eds M. P. Adam (1993).
Witzgall, R. Nail-patella syndrome. Pflugers Arch. 469, 927–936. https://doi.org/10.1007/s00424-017-2013-z (2017).
Lopez-Arvizu, C. et al. Increased symptoms of attention deficit hyperactivity disorder and major depressive disorder symptoms in nail-patella syndrome: potential association with LMX1B loss-of-function. Am. J. Med. Genet. B Neuropsychiatr Genet. 156B, 59–66. https://doi.org/10.1002/ajmg.b.31138 (2011).
Beguiristain, J. L., de Rada, P. D. & Barriga, A. Nail-patella syndrome: long term evolution. J. Pediatr. Orthop. B. 12, 13–16. https://doi.org/10.1097/01.bpb.0000043727.21564.e9 (2003).
Lippacher, S., Mueller-Rossberg, E., Reichel, H. & Nelitz, M. Correction of malformative patellar instability in patients with nail-patella syndrome: a case report and review of the literature. Orthop. Traumatol. Surg. Res. 99, 749–754. https://doi.org/10.1016/j.otsr.2013.03.031 (2013).
Dai, J. X., Johnson, R. L. & Ding, Y. Q. Manifold functions of the nail-Patella syndrome gene Lmx1b in vertebrate development. Dev. Growth Differ. 51, 241–250. https://doi.org/10.1111/j.1440-169X.2008.01083.x (2009).
Ding, Y. Q. et al. Lmx1b is essential for the development of serotonergic neurons. Nat. Neurosci. 6, 933–938. https://doi.org/10.1038/nn1104 (2003).
Doucet-Beaupre, H. et al. Lmx1a and Lmx1b regulate mitochondrial functions and survival of adult midbrain dopaminergic neurons. Proc. Natl. Acad. Sci. U S A. 113, E4387–4396. https://doi.org/10.1073/pnas.1520387113 (2016).
Wever, I., Largo-Barrientos, P., Hoekstra, E. J. & Smidt, M. P. Lmx1b influences correct post-mitotic coding of mesodiencephalic dopaminergic neurons. Front. Mol. Neurosci. 12, 62. https://doi.org/10.3389/fnmol.2019.00062 (2019).
Yan, C. H., Levesque, M., Claxton, S., Johnson, R. L. & Ang, S. L. Lmx1a and lmx1b function cooperatively to regulate proliferation, specification, and differentiation of midbrain dopaminergic progenitors. J. Neurosci. 31, 12413–12425. https://doi.org/10.1523/JNEUROSCI.1077-11.2011 (2011).
Zhao, Z. Q. et al. Lmx1b is required for maintenance of central serotonergic neurons and mice lacking central serotonergic system exhibit normal locomotor activity. J. Neurosci. 26, 12781–12788. https://doi.org/10.1523/JNEUROSCI.4143-06.2006 (2006).
Albishri, J. Arthropathy and proteinuria: nail-patella syndrome revisited. Ger. Med. Sci. 12, Doc16. https://doi.org/10.3205/000201 (2014).
Dunston, J. A. et al. A neurological phenotype in nail patella syndrome (NPS) patients illuminated by studies of murine Lmx1b expression. Eur. J. Hum. Genet. 13, 330–335. https://doi.org/10.1038/sj.ejhg.5201332 (2005).
Bannister, K. & Dickenson, A. H. What do monoamines do in pain modulation? Curr. Opin. Support Palliat. Care. 10, 143–148. https://doi.org/10.1097/spc.0000000000000207 (2016).
Ossipov, M. H., Morimura, K. & Porreca, F. Descending pain modulation and chronification of pain. Curr. Opin. Support Palliat. Care. 8, 143–151. https://doi.org/10.1097/SPC.0000000000000055 (2014).
Georgin-Lavialle, S. et al. Mast cells’ involvement in inflammation pathways linked to depression: evidence in mastocytosis. Mol. Psychiatry. 21, 1511–1516. https://doi.org/10.1038/mp.2015.216 (2016).
Light, K. C. et al. Adrenergic dysregulation and pain with and without acute beta-blockade in women with fibromyalgia and temporomandibular disorder. J. Pain. 10, 542–552. https://doi.org/10.1016/j.jpain.2008.12.006 (2009).
Al-Nimer, M. S. M., Mohammad, T. A. M. & Alsakeni, R. A. Serum levels of serotonin as a biomarker of newly diagnosed fibromyalgia in women: its relation to the platelet indices. J. Res. Med. Sci. 23, 71. https://doi.org/10.4103/jrms.JRMS_859_17 (2018).
Hermine, O. et al. Case-control cohort study of patients’ perceptions of disability in mastocytosis. PLoS One. 3, e2266. https://doi.org/10.1371/journal.pone.0002266 (2008).
Sarzi-Puttini, P., Giorgi, V., Marotto, D. & Atzeni, F. Fibromyalgia: an update on clinical characteristics, aetiopathogenesis and treatment. Nat. Rev. Rheumatol. 16, 645–660 (2020).
Haroutounian, S. et al. International Association for the Study of Pain Presidential Task Force on Cannabis and Cannabinoid Analgesia: research agenda on the use of cannabinoids, cannabis, and cannabis-based medicines for pain management. Pain. 162, S117–s124. https://doi.org/10.1097/j.pain.0000000000002266 (2021).
Dogrul, A., Seyrek, M., Yalcin, B. & Ulugol, A. Involvement of descending serotonergic and noradrenergic pathways in CB1 receptor-mediated antinociception. Prog Neuropsychopharmacol. Biol. Psychiatry. 38, 97–105. https://doi.org/10.1016/j.pnpbp.2012.01.007 (2012).
Russo, E. B., Burnett, A., Hall, B. & Parker, K. K. Agonistic properties of cannabidiol at 5-HT1a receptors. Neurochem Res. 30, 1037–1043. https://doi.org/10.1007/s11064-005-6978-1 (2005).
Pertwee, R. G. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br. J. Pharmacol. 153, 199–215. https://doi.org/10.1038/sj.bjp.0707442 (2008).
Zlebnik, N. E. & Cheer, J. F. Beyond the CB1 receptor: is Cannabidiol the answer for disorders of Motivation? Annu. Rev. Neurosci. 39, 1–17. https://doi.org/10.1146/annurev-neuro-070815-014038 (2016).
Romero, T. R., Resende, L. C., Guzzo, L. S. & Duarte, I. D. CB1 and CB2 cannabinoid receptor agonists induce peripheral antinociception by activation of the endogenous noradrenergic system. Anesth. Analg. 116, 463–472. https://doi.org/10.1213/ANE.0b013e3182707859 (2013).
Rezende, B., Alencar, A. K. N., de Bem, G. F., Fontes-Dantas, F. L. & Montes, G. C. Endocannabinoid System: chemical characteristics and biological activity. Pharmaceuticals (Basel). 16. https://doi.org/10.3390/ph16020148 (2023).
Pertwee, R. G., Ross, R. A., Craib, S. J. & Thomas, A. -)-Cannabidiol antagonizes cannabinoid receptor agonists and noradrenaline in the mouse vas deferens. Eur. J. Pharmacol. 456, 99–106. https://doi.org/10.1016/s0014-2999(02)02624-9 (2002).
Jenny, M., Schrocksnadel, S., Uberall, F. & Fuchs, D. The potential role of cannabinoids in modulating Serotonergic Signaling by their influence on Tryptophan Metabolism. Pharmaceuticals (Basel). 3, 2647–2660. https://doi.org/10.3390/ph3082647 (2010).
Dhadwal, G. & Kirchhof, M. G. The risks and benefits of Cannabis in the Dermatology Clinic. J. Cutan. Med. Surg. 22, 194–199. https://doi.org/10.1177/1203475417738971 (2018).
Mayrand, L. et al. Dramatic efficacy of cannabidiol on refractory chronic pain in an adolescent with sickle cell disease. Am. J. Hematol. 98, E295–E297. https://doi.org/10.1002/ajh.27049 (2023).
Rossignol, J., Hatton, S., Ridley, A., Hermine, O. & Greco, C. The effectiveness and safety of Pharmaceutical-Grade Cannabidiol in the treatment of Mastocytosis-Associated Pain: a pilot study. Biomedicines. 11 https://doi.org/10.3390/biomedicines11020520 (2023).
Russo, E. et al. Chronic cannabis use in the compassionate investigational New Drug program: an examination of benefits and adverse effects of legal clinical Cannabis. J. Cannabis Ther. 2, 3–57 (2002).
Strand, N. H. et al. Cannabis for the treatment of Fibromyalgia: a systematic review. Biomedicines. 11 https://doi.org/10.3390/biomedicines11061621 (2023).
Souza, J. D. R. et al. Adverse Effects of Oral Cannabidiol: An Updated Systematic Review of Randomized Controlled Trials (2020–2022). Pharmaceutics 14, doi: (2022). https://doi.org/10.3390/pharmaceutics14122598
Verma, R. et al. Cannabis, a Miracle Drug with Polyvalent Therapeutic Utility: preclinical and clinical-based evidence. Med. Cannabis Cannabinoids. 4, 43–60. https://doi.org/10.1159/000515042 (2021).
Villanueva, M. R. B. et al. Efficacy, Safety, and regulation of Cannabidiol on Chronic Pain: a systematic review. Cureus. 14, e26913. https://doi.org/10.7759/cureus.26913 (2022).
Paredes, S., Cantillo, S., Candido, K. D. & Knezevic, N. N. An Association of Serotonin with Pain disorders and its modulation by Estrogens. Int. J. Mol. Sci. 20 https://doi.org/10.3390/ijms20225729 (2019).
D’Andrea, G. et al. Tryptamine levels are low in plasma of chronic migraine and chronic tension-type headache. Neurol. Sci. 35, 1941–1945. https://doi.org/10.1007/s10072-014-1867-5 (2014).
Legangneux, E. et al. Cerebrospinal fluid biogenic amine metabolites, plasma-rich platelet serotonin and [3H]imipramine reuptake in the primary fibromyalgia syndrome. Rheumatol. (Oxford). 40, 290–296. https://doi.org/10.1093/rheumatology/40.3.290 (2001).
Parent, A. J. et al. Relationship between blood- and cerebrospinal fluid-bound neurotransmitter concentrations and conditioned pain modulation in pain-free and chronic pain subjects. J. Pain. 16, 436–444. https://doi.org/10.1016/j.jpain.2015.01.007 (2015).
Paul-Savoie, E. et al. A deficit in peripheral serotonin levels in major depressive disorder but not in chronic widespread pain. Clin. J. Pain. 27, 529–534. https://doi.org/10.1097/AJP.0b013e31820dfede (2011).
Tsigos, C., Reed, P., Weinkove, C., White, A. & Young, R. J. Plasma norepinephrine in sensory diabetic polyneuropathy. Diabetes Care. 16, 722–727. https://doi.org/10.2337/diacare.16.5.722 (1993).
Martins, I. et al. Increased noradrenergic neurotransmission to a pain facilitatory area of the brain is implicated in facilitation of chronic pain. Anesthesiology. 123, 642–653. https://doi.org/10.1097/ALN.0000000000000749 (2015).
Wei, H. & Pertovaara, A. Spinal and pontine alpha2-adrenoceptors have opposite effects on pain-related behavior in the neuropathic rat. Eur. J. Pharmacol. 551, 41–49. https://doi.org/10.1016/j.ejphar.2006.08.064 (2006).
Cathel, A. M. et al. Cannabinoid modulation of alpha2 adrenergic receptor function in rodent medial prefrontal cortex. Eur. J. Neurosci. 40, 3202–3214. https://doi.org/10.1111/ejn.12690 (2014).
Gutierrez, T. et al. Effects of neurotoxic destruction of descending noradrenergic pathways on cannabinoid antinociception in models of acute and tonic nociception. Brain Res. 987, 176–185. https://doi.org/10.1016/s0006-8993(03)03324-9 (2003).
Jenny, M., Santer, E., Pirich, E., Schennach, H. & Fuchs, D. Delta9-tetrahydrocannabinol and cannabidiol modulate mitogen-induced tryptophan degradation and neopterin formation in peripheral blood mononuclear cells in vitro. J. Neuroimmunol. 207, 75–82. https://doi.org/10.1016/j.jneuroim.2008.12.004 (2009).
Tayo, B. et al. Parallel-Group, single-dose trial of the Pharmacokinetics, Safety, and tolerability of Cannabidiol in subjects with mild to severe renal impairment. Clin. Pharmacokinet. 59, 747–755. https://doi.org/10.1007/s40262-019-00841-6 (2020).
Najafian, B., Smith, K., Lusco, M. A., Alpers, C. E. & Fogo, A. B. AJKD Atlas of Renal Pathology: nail-Patella syndrome–Associated Nephropathy. Am. J. Kidney Dis. 70, e19–e20 (2017).
Ware, J. E. Jr. & Sherbourne, C. D. The MOS 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med. Care. 30, 473–483 (1992).
Acknowledgements
The authors thank all the patients and the health care professional who cared for the patients. They also thank Drs Cécile Desjobert, Emma Pilling and Marielle Romet (Santé Active Edition-Synergy Pharm) for medical writing assistance.
Funding
C.G. was funded partially by the Fondation Bettencourt-Schueller during the study period. Medical writing assistance was funded by Inserm DR Paris-IDF Centre Nord. No other specific funding for this research was received from agencies or organizations in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: V.CD., C.G.; methodology: T.L., S.H, C.G.; validation: V.CD., C.G; formal analysis: T.L., C.G.; investigation: T.L., S.H, J.C. and C.G.; data curation: C.G, S.H.; writing-original draft preparation: T.L., J.C, C.G.; writing—review and editing: T.L., J.C, V.CD.; supervision: C.G.; project administration: C.G.; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
All the patients enrolled in this prospective study, or their legal guardian for patients aged ≤ 18 years, provided written informed consent for the publication of their data included in this article.
Institutional review board Statement
The institutional review board of the reference center for constitutional bone diseases, the MOC-Necker-Hospital (Paris, France), approved the study. In line with the French legislation on studies conducted in routine clinical practice, the study protocol was registered by the Assistance Publique–Hôpitaux de Paris the 16/05/2022 under the following reference: MR004-2022-0516123418.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lebret, T., Hatton, S., Callebert, J. et al. Evidence for therapeutic use of cannabidiol for nail-patella syndrome-induced pain in a real-world pilot study. Sci Rep 14, 30105 (2024). https://doi.org/10.1038/s41598-024-79239-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-79239-9