Abstract
This study aimed to confirm the hypothesis that continuous ACB (CACB) combined with a popliteal plexus block (PPB) can improve posterior knee pain, reduce nalbuphine consumption, and shorten the length of hospital stay. Patients who underwent TKA were allocated to the CACB + sham block (SHAM) or CACB + PPB groups. The primary outcome was the maximum pain score originating from the posterior knee within 4 h after TKA. Secondary outcomes included the maximum pain score originating from the posterior and anterior knees within 72 h after TKA, range of motion on postoperative day (POD) 1–3, postoperative nalbuphine consumption within 72 h of surgery, length of hospital stay, and complications. The maximum pain score of the posterior knee was lower in the CACB + PPB group than in the CACB + SHAM group within 0–12 h after surgery. Nalbuphine consumption within 24 h after surgery was lower in the CACB + PPB group than in the CACB + SHAM group. The range of motion was better in the CACB + PPB group than in the CACB + SHAM group on POD1 and 2. The length of hospital stay was shorter in the CACB + PPB group than in the CACB + SHAM group. The incidence of clinical significant nausea and vomiting was lower in the CACB + PPB group than in the CACB + SHAM group. This study found that PPB combined with CACB could relieve pain in the posterior knee within at least 12 h after TKA, reduce nalbuphine consumption within 24 h after TKA, improve the range of motion on POD1 and 2, and shorten the length of hospital stay for patients who underwent TKA.
Similar content being viewed by others
Introduction
Knee osteoarthritis is common in the elderly population in China. Total knee arthroplasty (TKA), which usually has a high success rate and satisfactory therapeutic effect, is commonly performed to treat end-stage knee osteoarthritis1,2. However, moderate-to-severe postoperative pain usually necessitates TKA, which delays the functional recovery of the knee joint, causes adhesion of the knee joint, and requires secondary surgical treatment3. Multimodal pain management has been widely used to improve postoperative pain control and accelerate knee function rehabilitation4. Owing to its reliable analgesic effect, peripheral nerve blocks have become an indispensable part of multimodal analgesia4. Adductor canal block (ACB) as well as the femoral triangle block anesthetize the anteromedial aspect of the knee, which could provide comparable analgesia to femoral nerve block for patients who underwent TKA5,6. However, the posterior joint capsule can be damaged by surgeries such as relaxation of the posterior knee joint capsule, removal of soft tissue from the popliteal fossa, and resection of the popliteal cyst during TKA, which can cause varying degrees of pain on the posterior side of the knee joint. Generally, 72-89% of patients complained of moderate-to-severe pain originating from the posterior knee7. Hence, it is worth studying ways to improve postoperative pain in the posterior knee after TKA.
Recent studies have found that sciatic nerve block or selected tibial nerve block can effectively control postoperative acute pain in the posterior knee after TKA7,8,9,10. However, motor block, originating from the sciatic nerve block or selected tibial nerve block, could delay early rehabilitation exercise and even increase the risk of falling in the hospital. The interspace between the popliteal artery and capsule of the posterior knee (IPACK) block, as a motor-sparing nerve block, can effectively improve acute pain originating from the posterior knee11,12. However, the limited duration of analgesia with IPACK is insufficient to avoid the need for opioids in patients undergoing TKA11. Moreover, the IPACK block is close to surgical procedures, which could result in resistance from surgeons based on sterility requirements.
Gardner found that the PPB sends genicular branches to the posterior knee capsule and intraarticular structures13. A recent cadaveric study by Runge et al. indicated that a distal adductor canal injection, called popliteal plexus block (PPB), could dye the popliteal plexus and genicular branch of the posterior obturator nerve14. A non-random, and unblinded study found that PPB could relieve postoperative pain originating from the posterior knee from numeric rating scale 5.5 to ≤ 1.515. PPB combined with femoral triangle block could decrease the 24-h postoperative opioid consumption after TKA16. PPB facilitates nerve catheter placement and prolongs the duration of analgesia. Moreover, the PPB is located far from the surgical area, making it easier to meet sterile requirements. Therefore, we hypothesized that continuous ACB combined with PPB could provide more perfect postoperative analgesic effect for TKA. And this study aimed to evaluate the effects of continuous ACB combined with PPB on analgesia in patients who underwent TKA.
Materials and methods
This randomized controlled trial was approved by the Ethics Committee of First Central Hospital of Baoding (No. [2021]112) and complied with the Declaration of Helsinki. This study was retrospectively registered in the Chinese Clinical Trial Registry (ChiCTR2200055535; registration date: 11/01/2022; enrollment date: 18/01/2022 (01/09/2021 in pilot study); http://www.chictr.org.cn/ ).
Patients who were scheduled for primary unilateral TKA, aged 18–80 years, with a body mass index of 20–35 kg/m2, and American Society of Anesthesiologists (ASA) classification I–III, were recruited from the First Central Hospital of Baoding. Patients with moderate to severe intraoperative knee malformations (pronation and flexion malformations) and joint stiffness; chronic kidney disease or cardiac insufficiency; mental disease; gastrointestinal ulcers; chronic use of analgesics (daily use opioids or paracetamol or celecoxib for > 4 weeks), psychotropics, or alcohol; allergy to anaesthetic drugs and sulfa; surgical limb neuropathy; language impairment; and inability to perform the visual analogue scale (VAS) were excluded from this study. Written informed consent was obtained from all participants.
Participants were randomly allocated to the CACB + SHAM group (receiving continuous ACB plus sham block) and the CACB + PPB group (receiving continuous ACB plus PPB) in a 1:1 ratio based on a computer-generated randomisation sequence. Random allocation was performed using a sealed envelope containing numbered cards which were not opened until the nerve block was administered. Patients were educated and familiarised with VAS score. All nerve block procedures were performed by the same senior anaesthesiologist before anaesthesia induction, whereas all assessments were performed by junior anaesthesiologists. Except for the nerve block team, which included a senior anaesthesiologist and an anaesthesia nurse, other participants, including junior anaesthesiologists participating in the assessment, floor nurses, surgeons, and patients, were blinded to randomisation.
US-guided CACB
All patients received CACB as reported by Sørensen JK (Fig. 1a)16. At the level of midthigh, the femoral artery was traced by a linear tranducer until it was located approximately midway between the lateral and medial borders of the sartorius muscle. Guided by ultrasound, an 80 mm short-beveled needle (PAJUNK®, PAJUNK GmbH Medizintechnologie, Germany) was inserted lateral to the transducer and advanced in-plane through the sartorius muscle and the fascia, extending from the vastus medialis to the adductor muscles, until the tip was located within the neurovascular sheath anterolateral to the artery. Hydrodissection was used to place the position of the needle tip. Then, a 19 G perineural catheter was inserted 3 cm past the needle tip. Catheters, in a cephalad direction, were tunneled subcutaneously to avoid disturbance of surgery. Fifteen millilitres of 0.5% ropivacaine were injected into the adductor canal after confirming the ___location of the catheter. Patient-controlled continuous adductor canal block with 0.2% ropivacaine was used as postoperative analgesia. The background infusion rate of the patient-controlled nerve block analgesia was 5 mL/h, with a bolus of 5 mL, and the lockout time was 30 min.
US-guided PPB
PPB was performed as described by Runge C (Fig. 1b)15. The linear transducer was slid distally along the femoral artery until the artery deviated from the sartorius muscle in the distal part of the adductor canal towards the adductor hiatus. The needle was advanced through the vastus medialis muscle using an in-plane approach from anterolateral to posteromedial and reached the distal end of the adductor canal close to the adductor hiatus. After confirmation of the needle tip, patients assigned to the CACB + PPB group received 20 mL of 0.5% ropivacaine. Patients assigned to the CACB + SHAM group received sham PPB with 20 mL of 0.9% sodium chloride injection.
General anaesthesia and postoperative analgesia
Anaesthesia was induced after confirming the effect of ACB. Propofol, remifentanil, sevoflurane, and cisatracurium were used for the induction and maintenance of anaesthesia. Besides remifentanyl, patients did not receive any other opioids before the end of the general anesthesia. Ventilation using a laryngeal mask and end-tidal carbon dioxide was maintained at 35–40 mmHg. During the surgery, bispectral index was maintained at 45 to 55, and the fluctuation of mean arterial pressure and heart rate were not more than ± 10% of the baseline value. All TKA procedures, with similar surgical steps and prostheses, were performed by the same surgeon. A tourniquet was not used during TKA to achieve sufficient haemostasis and reduce postoperative drainage. Perioperatively, the patients orally received paracetamol (1000 mg, twice per day) and celecoxib (200 mg, twice per day) as part of a multimodal analgesic regimen. Periarticular infiltration was not used to assess the analgesic effects of the PPB and ACB. When the VAS score was > 4, 10 mg of nalbuphine [nalbuphine (IV/IM/SC) 10 mg = morphine (IV/IM/SC) 10 mg] was administered by intravenous injection as an analgesic within 72 h after surgery.
Outcomes
The primary outcome was the maximum pain score originating from the posterior knee within 4 h after TKA. Patients were presented with a chart to display the four possible pain locations (anterior, medial, lateral, and posterior) as reported by Ochroch17. Postoperative pain was measured by VAS (0–10; 0: no pain, 10: worst pain).
Secondary outcomes included the maximum pain score originating from the posterior knee within 4–12, 12–24, 24–48, and 48–72 h after TKA; the maximum pain score originating from the anterior knee within 0–4, 4–12, 12–24, 24–48, and 48–72 h after TKA; range of motion on postoperative day (POD) 1–3, postoperative nalbuphine consumption within 72 h after surgery; length of hospital stay; and complications (dizziness, clinically significant postoperative nausea and vomiting, nerve injury, vascular injury, in-hospital falls, motor block of the quadriceps and gastrocnemius muscle, deep venous thrombosis, and infection). Clinically significant PONV was defined as a score of ≥ 5 on the PONV intensity scale18. This scale captures the frequency and severity of nausea and vomiting, the frequency of antiemetic administration, and also the impact of PONV on daily activities, and provides a summated score. Motor block was evaluated at 4, 8, and 24 h after surgery by knee extension and plantar or dorsal flexion of the ankle using a 3-point scale: 0 = normal movement (extension or flexion against gravity and resistance); 1 = paresis (extension or flexion against gravity but not resistance); and 3 = paralysis (extension or flexion impossible). Paresis and paralysis were delimited as motor block19,20.
Sample size calculation
In our pilot test, the mean maximum pain score originating from the posterior knee within 4 h after TKA was 5 points in the CACB + SHAM group, with a standard deviation of 2. According to Myles’s report, a VAS score of ≤ 3.3 was signified as an acceptable minimal clinically important pain improvement21. We presumed that the mean maximum pain score originating from the posterior knee within 4 h after TKA was 3.3 points in the CACB + PPB group, with a standard deviation of 2. A sample size of 46 patients was required to achieve 80% power to detect a difference at the 5% level of a two-tailed type I error. To prevent loss of power due to an unanticipated 20% dropout rate or protocol violation, 60 individuals were enrolled in this study.
Statistical analysis
Statistical analyses were performed using SPSS version 16.0 (IBM Corp., Armonk, NY, USA). The Kolmogorov–Smirnov and Shapiro–Wilk test were used to test the normal distribution of the data. Age and length of hospital stay are presented as mean ± standard deviation and were tested using t test. Body mass index, pain score, range of motion, duration of surgery, and nalbuphine consumption are presented as medians (interquartile ranges) and were tested using the Mann-Whitney U test. Sex, ASA, and complication are presented as number (%) and were tested using χ2 test. P < 0.05 was considered statistically significant.
Results
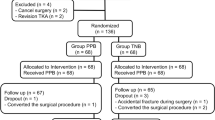
Ninety-eight patients were initially enrolled, and 60 completed the study (Fig. 2). Patient characteristics are presented in Table 1. There were no significant differences in patient characteristics, preoperative maximum pain scores, range of motion, or duration of surgery between the two groups (Table 1; P > 0.05).
The maximum pain score of the posterior knee was lower in the CACB + PPB group than in the CACB + SHAM group within 0–4 h [2 (2–3) vs. 4.5 (4–5); p = 0.000] and 4–12 h [2 (2–3) vs. 4.5 (3.75–5); p = 0.000] after surgery.
The maximum pain score of the posterior knee was lower in the CACB + PPB group than in the CACB + SHAM group within 4–12 h after surgery (Table 2). Nalbuphine consumption within 24 h after surgery was lower in the CACB + PPB group than in the CACB + SHAM group (Table 2). The range of motion was better in the CACB + PPB group than in the CACB + SHAM group on POD1 and POD2 (Table 2). The length of hospital stay was shorter in the CACB + PPB group than in the CACB + SHAM group (Table 2). The incidence of clinical significant nausea and vomiting was lower in the CACB + PPB group than in the CACB + SHAM group (Table 2). There were no significant differences in the maximum pain score of the posterior knee within 12–72 h after surgery, maximum pain score of the anterior knee within 72 h after surgery, nalbuphine consumption within 24–72 h, range of motion on POD 3, and incidence of adverse reactions such as dizziness, nerve injury, vascular injury, motor block of quadriceps and gastrocnemius muscle, in-hospital falls, deep venous thrombosis, and infection (Table 2).
Discussion
This study aimed to evaluate the effects of CACB combined with PPB on analgesia and functional recovery in patients who underwent TKA. The results showed that PPB could effectively improve maximum pain in the posterior knee at least within 12 h after TKA. Meanwhile, the addition of PPB to CACB reduced nalbuphine consumption within 24 h and improved the range of motion on POD1-2 after TKA. Furthermore, PPB combined with CACB facilitated discharge and reduced the incidence of clinical significant nausea and vomiting.
A peripheral nerve block, an important component of multimodal pain management, is recommended to improve outcomes in patients who have undergone TKA4. ACB can provide postoperative analgesia comparable to femoral nerve block; however, moderate-to-severe pain originating from the posterior knee still plagues patients who undergo TKA7,22. Based on anatomical evidence, the sensation in the anterior knee is innervated by the saphenous nerve, nerve to the vastus medialis muscle, and lateral and medial femoral cutaneous nerves23,24,25. Sensation in the posterior knee is innervated by the tibial nerve, posterior branch of the obturator nerve, and common peroneal nerve23,24,25. A femoral nerve block combined with a sciatic nerve block or a selected tibial nerve block can effectively control postoperative pain after TKA10,26. However, a motor block caused by a sciatic nerve block or a selected tibial nerve block may not be conducive to enhanced recovery after surgery.
A recent cadaveric study indicated that distal adductor canal injection could dye the popliteal plexus and genicular branch of the posterior obturator nerve14. In this study, patients who received PPB combined with CACB had effectively improved maximum pain in the posterior knee within at least 12 h after TKA, indicating that PPB could effectively control postoperative acute pain in the posterior knee. Consistent with our findings, Runge et al. found that supplementary PPB could relieve postoperative pain originating from the posterior knee. PPB was performed after surgery when a pain NRS score > 3 was reported by Runge15, whereas PPB was performed preoperatively in our study. Nociceptive stimulation originating from TKA can promote central and peripheral pain sensitisation formation27. Preoperative nerve block could play an important role in preventive analgesia by inhibiting central sensitisation and blocking the transmission of peripheral nociceptive stimulation to the central nervous system28. Moreover, the improvement in postoperative pain translated to a reduction in opioid consumption. In the present study, PPB significantly reduced opioid consumption, consistent with the findings of Mahmoud et al.29. Mahmoud et al. found that after arthroscopic anterior cruciate ligament reconstruction, opioid consumption was reduced from 30 mg13 to 12 mg4 by the addition of PPB to ACB compared with ACB alone29. However, postoperative opioid consumption was lower in patients who received combined CACB and PPB (10 [0–20] mg) than in those who received CACB and SHAM block (25 [10–32.5] mg) in this study. The difference in the reduction in opioid consumption might be related to the discrepancy in the type of local anaesthetic (bupivacaine vs. ropivacaine) and surgery (arthroscopic anterior cruciate ligament reconstruction vs. TKA). Furthermore, the improvement in postoperative pain originating from the posterior knee did not last for the first 24 h after surgery. Therefore, a single PPB cannot meet the analgesic requirements for breakthrough pain in the early stages after TKA. Adjuvants of local anaesthetics (adrenaline, dexamethasone, or clonidine) and continuous PPB analgesia could resolve the problem of a short analgesic duration. Recently, several studies reported that the IPACK block could alleviate postoperative acute pain originating from the posterior knee after TKA17,30. However, the effectiveness of adding an IPACK block to an ACB was also still debated. A meta-analysis found that in the context of periarticular local infiltration analgesia, adding IPACK to ACB did not improve analgesic outcomes following TKA31. Hussain et al. found that IPACK only provided analgesia for pain in the posterior knee over 12 h after TKA31. The limited duration of analgesia is not sufficient to be associated with other meaningful functional benefits, including first time out of bed or length of stay31. Continuous nerve block prolongs duration of postoperative analgesia. However, another limitation is that the technique of the IPACK block has been modified several times, which may reflect the uncertainty of the optimal ___location of needle injection and the anatomical position is also close to the sterile surgical field, that could result in a resistance from surgeons based on the requirement for sterility32,33. The advantage of the PPB is that the operation don’t need to changing patients position, which may save time and implement easily. And, the injection site for PPB is far from the sterile surgical field, which makes continuous PPB possible for patients who have undergone TKA15.
Fast-track recovery after TKA requires effective analgesia and superior muscle strength retention. Runge et al. found that knee extension and ankle flexion strength were not weakened by PPB15. In the present study, there was no significant difference in the incidence of quadriceps and gastrocnemius muscle motor block between PPB combined with CACB and CACB alone, which is consistent with the findings of Runge15. The adductor canal is a continuation of femoral triangle, high-volume local anesthetic may via the adductor canal spread to the common femoral nerve, which minimized quadriceps muscle strength. Some studies have pointed out that an ACB with 20 ml may cause a lower muscle strength than lower doses34. We also considered some other important influencing factors such as patients’ anatomical structure and BMI35. In this study, PPB combined with CACB improved the range of motion on POD 1–2 and shorten the length of hospital stay. The perfect analgesic effect of PPB combined with CACB and the excellent muscle strength retention made early functional recovery possible. However, in this study, one motor block of the ankle occurred after PPB. The muscle strength of the ankle returned to normal 4 h after surgery. Ankle motor weakness caused by the sciatic nerve block may be a contributing factor. Although the incidence was low, we still need to be vigilant about adverse events due to ankle muscle strength weakness. A recent dissection study found that the popliteal plexus, rather than the sciatic nerve, was dyed by injecting 10 mL of dye in the distal part of the adductor canal14. Runge et al. found that the strength of dorsal and plantar ankle flexion was not affected after the injection of 10 mL of bupivacaine into the distal part of the adductor canal15, which was consistent with the above dissection study14. Goffin et al. found that the sciatic nerve was dyed by injecting 20 mL of a dye-containing solution of a local anaesthetic into the adductor canal in fresh human cadavers36. The two-fold increase in the capacity for PPB may cause extensive spread of the local anaesthetic to the trunk of the sciatic nerve, resulting in ankle motor weakness. This finding indicates that the appropriate capacity of local anaesthetics for PPB should be explored in future studies.
The present study has several limitations. First, the nerve block team were not blinded in the block procedure. However, the senior anesthesiologist and the nurse in the nerve block team didn’t participate in anesthesia management and postoperative follow-up. Second, owing to the small sample size, some unexpected complications of PPB (including motor block, in-hospital falls, and infection) might have been overlooked. Third, periarticular infiltration was not used to confirm the analgesic action of PPB, which could have led to inadequate analgesia. The last but not least, the benefits of PPB may be limited by the short duration of a single nerve block. Extension of the duration of PPB by a local anaesthetic adjuvant or the placement of perineural catheters may solve this problem.
Conclusions
PPB combined with CACB could relieve pain in the posterior knee within at least 12 h after TKA, reduce nalbuphine consumption within 24 h after TKA, improve the range of motion on POD 1–2, and shorten the length of hospital stay of patients undergoing TKA.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Weinstein, A. M. et al. Estimating the burden of total knee replacement in the United States. J. Bone Joint Surg. Am. 95(5), 385–392 (2013).
Price, A. J. et al. Knee replacement. Lancet 392(10158), 1672–1682 (2018).
Sardana, V., Burzynski, J. M. & Scuderi, G. R. Adductor canal block or local infiltrate analgesia for pain control after total knee arthroplasty? A systematic review and meta-analysis of randomized controlled trials. J. Arthroplasty 34(1), 183–189 (2019).
Kandarian, B. S. et al. Updates on multimodal analgesia and regional anesthesia for total knee arthroplasty patients. Best Pract. Res. Clin. Anaesthesiol. 33(1), 111–123 (2019).
Grevstad, U. et al. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: a randomized, blinded study. Reg. Anesth. Pain Med. 40(1), 3–10 (2015).
Runge, C. et al. The analgesic effect of obturator nerve block added to a femoral triangle block after total knee arthroplasty: a randomized controlled trial. Reg. Anesth. Pain Med. 41(4), 445–451 (2016).
Abdallah, F. W. et al. The analgesic effect of proximal, distal, or no sciatic nerve block on posterior knee pain after total knee arthroplasty: a double-blind placebo-controlled randomized trial. Anesthesiology 121(6), 1302–1310 (2014).
Zorrilla-Vaca, A. & Li, J. The role of sciatic nerve block to complement femoral nerve block in total knee arthroplasty: a meta-analysis of randomized controlled trials. J. Anesth. 32(3), 341–350 (2018).
Sinha, S. K. et al. Femoral nerve block with selective tibial nerve block provides effective analgesia without foot drop after total knee arthroplasty: a prospective, randomized, observer-blinded study. Anesth. Analg. 115(1), 202–206 (2012).
Kampitak, W. et al. Motor-sparing effect of iPACK (interspace between the popliteal artery and capsule of the posterior knee) block versus tibial nerve block after total knee arthroplasty: a randomized controlled trial. Reg. Anesth. Pain Med. 45(4), 267–276 (2020).
Mou, P. et al. Adductor canal block combined with IPACK Block for postoperative analgesia and function recovery following total knee arthroplasty: a prospective, double-blind, randomized controlled study. J. Arthroplasty 37(2), 259–266 (2022).
Abdullah, M. A., Abu Elyazed, M. M. & Mostafa, S. F. The Interspace between Popliteal artery and posterior Capsule of the knee (IPACK) block in knee arthroplasty: a prospective randomized trial. Pain Physician 25(3), E427–E433 (2022).
Gardner, E. The innervation of the knee joint. Anat. Rec. 101(1), 109–130 (1948).
Runge, C. et al. The spread of Ultrasound-guided injectate from the adductor canal to the genicular branch of the posterior obturator nerve and the popliteal plexus: a cadaveric study. Reg. Anesth. Pain Med. 42(6), 725–730 (2017).
Runge, C. et al. The analgesic effect of a popliteal plexus blockade after total knee arthroplasty: a feasibility study. Acta Anaesthesiol. Scand. 62(8), 1127–1132 (2018).
Sørensen, J. K., Grevstad, U., Jaeger, P., Nikolajsen, L. & Runge, C. Effects of popliteal plexus block after total knee arthroplasty: a randomized clinical trial. Reg. Anesth. Pain Med. https://doi.org/10.1136/rapm-2024-105747 (2024).
Ochroch, J. et al. Analgesic efficacy of adding the IPACK block to a multimodal analgesia protocol for primary total knee arthroplasty. Reg. Anesth. Pain Med. 45(10), 799–804 (2020).
Myles, P. S. & Wengritzky, R. Simplified postoperative nausea and vomiting impact scale for audit and post-discharge review. Br. J. Anaesth. 108(3), 423–429 (2012).
Aliste, J. et al. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total hip arthroplasty. Reg. Anesth. Pain Med. 46(10), 874–878 (2021).
Cappelleri, G. et al. Intraneural ultrasound-guided sciatic nerve block: minimum effective volume and electrophysiologic effects. Anesthesiology 129(2), 241–248 (2018).
Myles, P. S. et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br. J. Anaesth. 118(3), 424–429 (2017).
Zhao, X. Q. et al. The comparison of adductor canal block with femoral nerve block following total knee arthroplasty: a systematic review with meta-analysis. J. Anesth. 30(5), 745–754 (2016).
Bendtsen, T. F. et al. The optimal anglgesic block for total knee arthroplasty. Reg. Anesth. Pain Med. 41, 711–719 (2016).
Hirasawa, Y. et al. Nerve distribution to the human knee joint: anatomical and immunohistochemical study. Int. Orthop. 24, 1–4 (2000).
Kennedy, J. C., Alexander, I. J. & Hayes, K. C. Nerve supply of the human knee and its functional importance. Am. J. Sports Med. 10, 329–335 (1982).
Ardon, A. E. et al. Opioid consumption in total knee arthroplasty patients: a retrospective comparison of adductor canal and femoral nerve continuous infusions in the presence of a sciatic nerve catheter. J. Clin. Anesth. 31, 19–26 (2016).
Kurien, T. et al. Chronic postoperative pain after total knee arthroplasty: the potential contributions of synovitis, pain sensitization and pain catastrophizing—an explorative study. Eur. J. Pain 26(9), 1979–1989 (2022).
O’Neill, A. & Lirk, P. Multimodal analgesia. Anesthesiol. Clin. 40(3), 455–468 (2022).
Mahmoud, A. et al. Analgesic impact of a popliteal plexus block to standard adductor canal block in arthroscopic anterior cruciate ligament reconstruction: a randomized blind clinical trial. Pain Res. Manag.2021, 1723471 (2021).
Wang, C. G. et al. The effect of continuous adductor canal block combined with distal interspace between the popliteal artery and capsule of the posterior knee block for total knee arthroplasty: a randomized, double-blind, controlled trial. BMC Anesthesiol. 22(1), 175 (2022).
Hussain, N. et al. Does the addition of iPACK to adductor canal block in the presence or absence of periarticular local anesthetic infiltration improve analgesic and functional outcomes following total knee arthroplasty? A systematic review and meta-analysis. Reg. Anesth. Pain Med. 46(8), 713–721 (2021).
Chan, E., Howle, R., Onwochei, D. & Desai, N. Infiltration between the popliteal artery and the capsule of the knee (IPACK) block in knee surgery: a narrative review. Reg. Anesth. Pain Med. 46(9), 784–805 (2021).
Kampitak, W., Tanavalee, A., Ngarmukos, S. & Tantavisut, S. Motor-sparing effect of iPACK (interspace between the popliteal artery and capsule of the posterior knee) block versus tibial nerve block after total knee arthroplasty: a randomized controlled trial. Reg. Anesth. Pain Med. 45(4), 267–276 (2020).
Jæger, P. et al. Optimal volume of local anaesthetic for adductor canal block: using the continual reassessment method to estimate ED95. Br. J. Anaesth. 115(6), 920–926 (2015).
Yee, E. J., Gapinski, Z. A., Ziemba-Davis, M., Nielson, M. & Meneghini, R. M. Quadriceps weakness after single-shot adductor canal block: a multivariate analysis of 1,083 primary total knee arthroplasties. J. Bone Joint Surg. Am. 103(1), 30–36 (2021).
Goffin, P. et al. Interfascial spread of injectate after adductor canal injection in fresh human cadavers. Anesth. Analg. 123(2), 501–503 (2016).
Funding
This work was supported by the Medical Science Technology Project of Hebei (20230253).
Author information
Authors and Affiliations
Contributions
CGW, BWJ contributed to the study conception, design, drafting and revision of manuscript; MYY, QZ, JNL and MNG contributed to data collection, YG and HJZ contributed to data analysis, XWW and FYR contributed to material preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiang, Bw., Guo, Y., Yang, My. et al. The analgesic effect of continuous adductor canal block combined with popliteal plexus block for total knee arthroplasty: a randomized controlled trial. Sci Rep 14, 27757 (2024). https://doi.org/10.1038/s41598-024-79487-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-79487-9