Abstract
Immediate breast reconstruction provides breast cancer patients with a valuable opportunity to restore breast shape. However, post-reconstruction breast asymmetry remains a common issue that affects patient satisfaction. This study aims to quantify breast asymmetry after surgery using magnetic resonance imaging (MRI) and assess its impact on both breast satisfaction and overall outcome satisfaction, offering scientific evidence to guide improvements in preoperative evaluation. We retrospectively collected MRI images and demographic characteristics from 98 patients who underwent unilateral immediate breast reconstruction. All patients underwent breast MRI scans post-reconstruction, and the MRI images were converted into 3D models using 3D Slicer software. The implant volumes were measured and compared with the actual implant volumes inserted during surgery to assess the accuracy of the MRI measurements. Breast symmetry after surgery was quantified using MRI-measured breast volumes, and patient satisfaction was analyzed through BREAST-Q questionnaires to explore the relationship between breast symmetry, post-reconstruction breast satisfaction, and overall outcome satisfaction. The implant volumes measured in the 3D reconstructed MRI images exhibited high concordance with the volumes recorded during surgery (r = 0.980, p < 0.001). Breast asymmetry values were significantly higher in the high BMI group compared to the low BMI group (P = 0.013), while the asymmetry ratio was significantly lower in the high weight group compared to the low weight group (P = 0.006). The asymmetry ratio showed a weak correlation with breast satisfaction (r = − 0.341, P = 0.002) and outcome satisfaction (r = − 0.371, P = 0.004). When grouped by low asymmetry (asymmetry > 10%), there was no significant difference in breast satisfaction (P = 0.054) or outcome satisfaction scores (P = 0.23) between the groups. However, in cases of high asymmetry (asymmetry ratio > 40%), breast satisfaction (P = 0.003) and outcome satisfaction scores (P = 0.005) were significantly lower in the asymmetry group compared to the symmetry group. Breast volume asymmetry after immediate breast reconstruction is associated with patient satisfaction, with a significant decrease in satisfaction when asymmetry exceeds 40%. This suggests that preoperative evaluation should focus on breast symmetry to improve post-reconstruction patient satisfaction and surgical outcomes.
Similar content being viewed by others
Introduction
Breast cancer is among the most prevalent malignant tumors globally and significantly contributes to cancer incidence and mortality rates in women1. Mastectomy remains a critical treatment modality for breast cancer. With the improved survival rates of r breast cancer patients post-surgery, there is an increase demand for enhanced quality of life, prompting more women to opt immediate breast reconstruction2. Although breast reconstruction can restore the shape of the breast, asymmetry remains one of the most common post-reconstruction issues. Previous studies have shown a correlation between post-reconstruction breast volume asymmetry and patient satisfaction3, but how this asymmetry specifically impacts post-reconstruction satisfaction remains unclear.
Various methods have been proposed for measuring breast volume, including three-dimensional scanner imaging, Archimedes’ principle measurement, linear measurements, mammography, computed tomography, and ultrasound4. While these methods have provided some assistance in selecting the appropriate implant size for breast cancer patients, they all present limitations, such as operational complexity, high cost, and significant measurement errors5. Magnetic Resonance Imaging (MRI) is a highly accurate method for measuring breast volume, and it has shown higher accuracy compared to other measurement techniques. Existing studies indicate a strong correlation between MRI-measured breast volume and the volume of mastectomy specimens, which are considered the gold standard. Additionally, MRI offers excellent soft tissue resolution and poses no radiation hazard, allowing for clear delineation of the internal and external breast structures6.
This study aims to use MRI to measure breast volume in breast cancer patients following immediate reconstruction, quantitatively assess post-reconstruction breast symmetry, and explore the impact of breast asymmetry on patient satisfaction with both breast aesthetics and overall outcomes. The findings will provide scientific evidence to optimize preoperative assessment and post-reconstruction care.
Methods
Ethical consideration
The study was approved by the Third Affiliated Hospital of Kunming Medical University (No. KYLX2023-110). Informed consent was waived due to the retrospective nature of the study by the Third Affiliated Hospital of Kunming Medical University (No. KYLX2023-110). All methods used in this research were performed in accordance with the relevant guidelines and regulations.
Datasets
We retrospectively collected data from 98 breast cancer patients who underwent breast cancer surgery with immediate breast reconstruction and subsequent MRI examinations between January 2020 and January 2023. The exclusion criteria were bilateral breast reconstruction, reconstruction using autologous tissue, the presence of disease or structural abnormalities in the contralateral breast, and missing clinical data. The collected clinical data included the patients’ age, height, weight, body mass index (BMI), type of surgical excision, operative side, tumor pathology type, Tumor, Node, Metastasis (TNM) stage, lymph node dissection status, implant volume during breast implantation, final follow-up interval, and history of chemotherapy, radiotherapy, and targeted therapy (Table 1).
Surgery
All patients underwent immediate breast reconstruction following mastectomy, sentinel lymph node biopsy, or axillary lymph node dissection. After mastectomy, the weight of each breast sample was measured via an electronic scale, and the volume was determined via the water displacement method. During surgery, high-frequency electric and ultrasonic scalpels were used to dissect the entire breast gland. The surgical range extended from the second rib to 2 cm below the inframammary fold and from the parasternal region to the mid-axillary line. The breast was separated along the deep surface of the pectoralis major fascia, hemostasis was achieved, and the wound was irrigated with warm iodine povidone solution. The pectoralis major and minor spaces were subsequently dissected, the implant was placed, and the implant was wrapped with acellular dermal matrix, which was then sutured to the pectoralis major. A drain was placed subcutaneously in the breast and in the implant cavity and connected to a disposable vacuum-assisted drainage device to perform closed wound negative pressure drainage. The surgical incision was closed with absorbable sutures via an intradermal suture technique. Throughout the surgery and post-reconstruction, antibiotics were administered.
MRI imaging and breast volume measurement
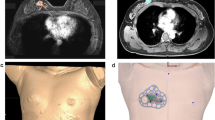
Patients were positioned prone with both breasts naturally hanging down and fitted with a specialized breast MRI measurement coil. Scanning was performed via a Siemens 3.0 T machine with a T1W sequence. The specific parameters were as follows: FOV = 340 × 340 mm2, TR = 5600 ms, TE = 56 ms, slice thickness = 4 mm, and average = 2. 3D Slicer software (version 5.1.0, http://www.slicer.org) was used to measure the volume of the implants and both breast mounds. On the T1-weighted transverse MR images, the implants and both breast mounds were contoured layer by layer to generate the volumes of the implants and both breast mounds (Fig. 1A,D). In this study, the breast mound was defined as outside breast on the ventral aspect of the pectoralis (Fig. 1).The ventral boundary was determined as the parallel line of chest wall curvature in front of the rib and the anterior border corresponded to the transition from the skin to the surrounding air. The edge of the sternum was used as the medial border, and the lateral border was placed at the point where the thickness of the breast was equal to the thickness of the surrounding skin7,8 (Fig. 1D,E).
Asymmetry criteria of breast volume
On the basis of the study by Kayar et al., we adopted two criteria for measuring breast asymmetry: the asymmetry value and the asymmetry ratio9. The asymmetry value is defined as the difference in volume between the two breasts, whereas the asymmetry ratio is the ratio of the asymmetry value to the volume of the smaller breast.
The larger the asymmetry value or asymmetry ratio is, the more asymmetric the breasts are.
Evaluation of patient post-reconstruction breast satisfaction and outcome satisfaction
We conducted follow-up interviews with patients via telephone and used the BREAST-Q questionnaire10 to assess their satisfaction with their breasts and surgical outcomes. The BREAST-Q questionnaire, released in 2009, was specifically developed for breast cancer patients undergoing breast surgery and has been used in studies involving over 22,000 women who have undergone various types of breast surgery. We selected two sections of the questionnaire: breast satisfaction and outcome satisfaction. Breast satisfaction includes evaluations of size, shape, position, appearance, and overall symmetry. Outcome satisfaction encompasses the patient’s experiences with the surgical process, the achievement of expected goals, and the impact on their life. For each scale, higher scores indicate better breast perception or greater satisfaction with the outcomes.
Statistical analysis
Descriptive statistics (means ± standard deviations, medians, ranges, frequencies, percentages) were used to summarize the basic information of patients who underwent immediate breast reconstruction. Spearman’s correlation coefficient and Bland‒Altman plots were employed to analyze the consistency between the implant volumes measured on the MR images and those recorded during surgery. Independent sample t tests were used to detect differences in the mean asymmetry value and asymmetry ratio of bilateral breasts across various factors. Spearman correlation coefficients and independent sample t tests were used to analyze the relationships between the degree of breast asymmetry (asymmetry ratio and asymmetry value) and patient post-reconstruction breast satisfaction and outcome satisfaction. All the data were analyzed via SPSS software, with α = 0.05 as the significance level and P < 0.05 indicating statistical significance.
Results
Patient baseline characteristics
A total of 98 patients were evaluated in this study, with an average age of 42.2 years [standard deviation (SD), 8.44 years; range, 22–63 years]. The mean height and weight were 158.43 cm (SD, 4.68 cm; range, 150–170 cm) and 53.88 kg (SD, 6.82 kg; range, 40–72 kg), respectively. The average BMI was 21.46 kg/m2 (SD, 2.50 kg/m2; range, 16.82–28.04 kg/m2). Details of the patients’ history of chemotherapy, radiotherapy, and endocrine therapy are presented in Table 1. Among the 98 patients enrolled, 65 (66.3%) underwent nipple-sparing mastectomy, 24 (24.5%) underwent skin-sparing mastectomy, and 9 (9.2%) underwent total mastectomy. Regarding the type of implant, Mentor was used in 88 patients (89.8%) and Allergan in 10 (10.2%). Since this study is a retrospective analysis, only 82 patients participated in the post-reconstruction satisfaction survey. The average time from MRI to satisfaction survey was 11.88 months (SD, 4.83 months; range, 5–32 months).
Accuracy of MRI
To verify the reliability of MRI volumetric measurements, we determined the correlation and consistency between the implant volume measured by MRI and the actual implant volume inserted during surgery (Fig. 2). The Spearman rank correlation coefficient showed a strong correlation between the MRI-measured implant volume and the actual implant volume (r = 0.980; P < 0.001). The Bland–Altman plot shows good agreement between the implant volume measured by MRI and the actual implant volume recorded during surgery (bias, − 11.37 ml; 95% limits of agreement: − 34.89 ml, 12.16 ml).
Symmetry of bilateral breasts
We analyzed the impact of various factors on the mean asymmetry value and asymmetry ratio between both breasts (Table 2). There were no significant differences in breast asymmetry value or asymmetry ratio among patients of different ages or heights (P > 0.05). Heavier patients (≥ 53 kg) had a lower mean asymmetry ratio (P = 0.006) but no difference in the mean asymmetry value (P = 0.696). Patients with a higher BMI (≥ 21.25 kg/m2) had a significantly higher asymmetry value compared to those with a lower BMI (P = 0.013). There were no significant differences in asymmetry value (P = 0.441) or asymmetry ratio (P = 0.240) based on different reconstruction methods. Figure 3 shows the distribution of contralateral breast volume measured by MRI for all patients in the study. Table 3 lists the ranges of contralateral breast volumes, mean actual implant sizes, and corresponding symmetry indices. Despite individual variations, there was a positive correlation between breast volume measured by MRI and implant size.
Relationship between post-reconstruction breast symmetry and satisfaction
Table 4 shows the correlation between breast symmetry and satisfaction in breast cancer patients after reconstruction surgery. There was only a weak correlation between breast asymmetry ratio and breast satisfaction (r = − 0.341, p = 0.002) and outcome satisfaction (r = − 0.371, p = 0.004). The asymmetry value was weakly correlated with breast satisfaction (r = − 0.306, p = 0.005), but no significant correlation was found with outcome satisfaction (p = 0.100). A strong positive correlation was observed between breast satisfaction and outcome satisfaction (r = 0.860, p < 0.001).
Patients were divided into symmetrical and asymmetrical groups on the basis of the quartiles of the breast asymmetry ratio, and an independent sample t test was conducted to examine group differences. The results showed that when grouped by low asymmetry (< 10%), there was no significant difference in breast satisfaction scores (p = 0.054) and outcome satisfaction scores (p = 0.23). However, at high degree of asymmetry (> 40%), significant differences were observed in breast satisfaction scores (p = 0.003) and outcome satisfaction scores (p = 0.005) between the two groups. (Table 5).
Discussion
This study measured breast volume using MRI images after immediate breast reconstruction in breast cancer patients, analyzing the relationship between post-reconstruction breast symmetry and patient satisfaction. MRI demonstrated high accuracy for volume measurement, with no significant deviation between implant volume measured by MRI and the actual implant volume recorded during surgery (r = 0.980, P < 0.001). Significant differences in post-reconstruction breast symmetry were observed among patients with different body weights and BMI (P < 0.05). Although the post-reconstruction breast asymmetry ratio showed only a weak correlation with the BREAST-Q scores (r = − 0.341, p = 0.002; r = − 0.371, p = 0.004), patient satisfaction significantly decreased when a high degree of asymmetry (> 40%) was present. This suggests that breast volume symmetry may be an important factor affecting patient satisfaction after immediate breast reconstruction in breast cancer patients. Controlling volume symmetry during surgery could be valuable for post-reconstruction satisfaction, and MRI can serve as a reliable tool for volume measurement.
The volume of the implant is a crucial factor in determining post-reconstruction breast symmetry, as it directly influences the degree of match between the reconstructed breast and the contralateral breast11. Previous studies have found that the density of the subcutaneous breast tissue is approximately 1 g/mL, meaning that the intraoperative measurement of breast weight in grams generally equals the volume in milliliters. There is a strong correlation between the weight and volume of excised breast specimens during surgery, however, breast density plays a significant role in affecting this correlation12. Due to substantial variability in individual breast density, younger patients may have denser glandular tissue, while breast cancer patients may experience changes in breast density due to neoadjuvant chemotherapy and other treatments13. Consequently, relying solely on breast weight is inadequate for accurately determining the optimal implant volume during surgery, and additional evaluation methods are needed to achieve a more precise volume assessment.
We highlighted the application of MRI in the measurement of breast volume after breast reconstruction in breast cancer patients. The results showed a high correlation between the breast implant volume measured by MRI images and the actual implant volume recorded during surgery (r = 0.980, P < 0.001), consistent with previous studies6, further confirming the high accuracy of MRI in breast volume measurement. Various methods for measuring breast volume have been reported, including non-imaging techniques such as water displacement, linear measurement, and 3D scanning, as well as imaging methods such as mammography, CT, and MRI5. Water displacement is often considered the gold standard for breast volume measurement, but it can be inaccurate for intact breasts and is unsuitable for preoperative planning due to its inconvenience for patients14. Linear measurement is cost-effective and comfortable for patients, but its heavy reliance on formulas raises questions about its accuracy15,16. 3D scanning is widely used and shows high accuracy and reliability in measurements, but errors can occur owing to the complexity of different breast shapes, requiring further refinement17. Among imaging methods, mammography is easy to perform and provides sufficiently accurate results compared to MRI, but it often causes significant discomfort for patients18. CT scans can quickly reconstruct 3D models to calculate volume quickly and at a lower cost than MRI, but they are slightly less accurate19. This may be because CT scans are performed in the supine position, making it harder to define the breast boundaries than in the prone position used in MRI. Additionally, CT involves radiation exposure20.
Our study revealed that the post-reconstruction breast asymmetry value in the higher BMI group (≥ 21.5) was significantly greater than in the lower BMI group. This finding is consistent with Losken et al.'s research, which also indicated a marked increase in breast asymmetry among individuals with higher BMI in the general population21. Similarly, Kayar et al. reported that breast cancer patients with a higher BMI (> 30) exhibited significantly greater differences in bilateral breast volumes compared to healthy controls9. Preoperative asymmetries in breast symmetry may contribute to post-reconstruction breast asymmetry, as most healthy women may naturally exhibit physiological asymmetry, while some breast cancer patients may present with pathological asymmetry due to tumor burden22,23. In breast cancer patients with higher BMI, preoperative breast asymmetry may already be more pronounced24. However, the results of this study may not be generalizable to patients across all BMI categories, and further research is needed to investigate the effects of different BMI levels on breast symmetry both before and after reconstruction surgery. On the other hand, the asymmetry ratio may be a more accurate reflection of breast symmetry compared to the absolute asymmetry value. This is because, with the same volume difference, asymmetry tends to be more noticeable in patients with smaller breasts compared to those with larger breasts9. Our study also found that patients with lower body weight (< 52 kg) had a significantly higher asymmetry ratio than those with higher body weight. This may be due to the fact that patients with higher body weight typically have more subcutaneous fat in the breast, resulting in larger breast volumes compared to those with lower body weight25. As a result, even though the volume difference between the two groups was not significant, patients with lower body weight exhibited more pronounced asymmetry. However, excessive body weight may reduce the sensitivity of the asymmetry ratio in detecting breast symmetry9.
When MRI-assessed breast volume asymmetry is high, there is a significant difference in both breast satisfaction and outcome satisfaction among patients. In immediate breast reconstruction surgery, the selection of the implant shape, texture, and size is crucial in the surgical plan, with volume being one of the most important factors for determining breast symmetry26. Despite the surgeon’s decision-making process and symmetry assessment, patient satisfaction remains the primary goal of breast reconstruction. Although objective measurement of volume symmetry is essential, it cannot completely replace patient satisfaction27. Therefore, we studied the relationship between objectively measured symmetry and patient-reported satisfaction. The correlation between the volume difference between the left and right breasts measured by MRI and patient satisfaction was lower than the correlation with the asymmetry ratio. This may be because the relative distribution of volume differences plays a more important role in the perceived volume difference by patients than does the absolute volume difference. The asymmetry ratio of breast volume is moderately negatively correlated with patient satisfaction with their breasts and the surgical outcome. We found that the breast volume asymmetry ratio had only a weak correlation with patient satisfaction (r = − 0.341, P = 0.002) and outcome satisfaction (r = − 0.371, P = 0.004), suggesting that volume symmetry is likely just one of many factors influencing satisfaction. Other factors, such as psychological expectations, quality of post-reconstruction care, and the visibility of scars, may also play a significant role28. When grouped by low asymmetry (asymmetry ratio > 10%), there was no significant difference in satisfaction between the groups (P > 0.05). However, when the asymmetry ratio exceeded 40%, patient satisfaction significantly decreased (P < 0.05), with both breast and outcome satisfaction notably lower in the high asymmetry group. This may be because patients tend to tolerate minor asymmetries, but once the asymmetry ratio surpasses 40%, the visual discrepancy becomes more noticeable, leading to increased discomfort and a marked decline in satisfaction. Nevertheless, we cannot definitively determine whether a 40% asymmetry ratio represents the minimum threshold affecting satisfaction, and further research is required to confirm this finding. For breast surgeons, achieving symmetry during breast reconstruction is the most challenging yet crucial goal. While breast shape is also essential for symmetry, volume is more critical because each patient’s breast shape is unique, and the fixed style of implants limits precise matching with the contralateral breast shape29. In contrast, breast volume symmetry is more controllable and has a more direct impacts patient-reported satisfaction.
Our study has several limitations. First, our sample contains a higher proportion of younger women, which may introduce an age bias likely because younger women are more inclined to opt for breast reconstruction surgery. Additionally, due to sample limitations, BMI does not represent all categories, and therefore further stratified analysis was not conducted. Second, this was a retrospective study with a small sample size, limiting its generalizability. Larger sample sizes and longer-term follow-up data on patient satisfaction are needed to verify the impact of MRI-measured breast volume asymmetry on patient satisfaction. Third, we do not have preoperative MRI imaging data for the patients, which prevents us from assessing the symmetry of the breasts before surgery. Fourth, this study only assessed volume data, as we consider volume a critical factor for breast symmetry. However, future research should include shape data for a prospective analysis. On the other hand, although MRI is generally considered more accurate than other methods for measuring breast volume, it still has certain limitations when evaluating changes in breast size. Since breast MRI is typically performed in the prone position, the contour of the breast may change after the implant is placed, causing some surrounding tissue to be either expanded or excluded from the defined boundaries, which introduces systematic error8,30. Fifth, the standards for post-reconstruction breast symmetry and asymmetry have not been defined, and there is still debate regarding the minimum threshold. Additionally, variations in follow-up times among patients may also impact their satisfaction with their breasts and surgical outcomes.
Conclusion
MRI is an effective tool for volume measurement, and the breast volume asymmetry assessed after immediate breast reconstruction in breast cancer patients is associated with breast satisfaction and overall outcome satisfaction. When the asymmetry ratio exceeds 40%, patient satisfaction significantly decreases. Breast volume symmetry is a key factor influencing patient satisfaction after breast reconstruction, and preoperative evaluation and planning should focus on ensuring symmetry to improve overall patient satisfaction post-reconstruction.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to the risk of a breach of patient data privacy. However, anonymized data are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CT:
-
Computed tomography
- FOV:
-
Field of view
- TE:
-
Echo time
- TR:
-
Repetition time
- MRI:
-
Magnetic resonance imaging
- NSM:
-
Nipple-sparing mastectomy
- SSM:
-
Skin-sparing mastectomy
- TM:
-
Total mastectomy
- SD:
-
Standard deviation
References
Trapani, D. et al. Global challenges and policy solutions in breast cancer control. Cancer Treat. Rev. 104, 102339 (2022).
Ilonzo, N., Tsang, A., Tsantes, S., Estabrook, A. & Thu Ma, A. M. Breast reconstruction after mastectomy: A ten-year analysis of trends and immediate postoperative outcomes. Breast Edinb. Scotl. 32, 7–12 (2017).
Guyomard, V., Leinster, S. & Wilkinson, M. Systematic review of studies of patients’ satisfaction with breast reconstruction after mastectomy. The Breast 16, 547–567 (2007).
Xi, W. et al. Objective breast volume, shape and surface area assessment: A systematic review of breast measurement methods. Aesthetic Plast. Surg. 38, 1116–1130 (2014).
Choppin, S. B., Wheat, J. S., Gee, M. & Goyal, A. The accuracy of breast volume measurement methods: A systematic review. The Breast 28, 121–129 (2016).
Kim, H. et al. Preoperative magnetic resonance imaging-based breast volumetry for immediate breast reconstruction. Aesthetic Plast. Surg. 39, 369–376 (2015).
Kim, M. J., Kim, T. W., Hahn, H. M. & Lee, I. J. Clinical use of perioperative magnetic resonance imaging-based breast volumetric analysis in final implant volume prediction for two-stage breast reconstruction. Ann. Surg. Treat. Res. 103, 195 (2022).
Herly, M. et al. The current gold standard breast volumetry technique seems to overestimate fat graft volume retention in the breast: A validation study. J. Plast. Reconstr. Aesthet. Surg. 72, 1278–1284 (2019).
Kayar, R. & Çilengiroğlu, Ö. V. Breast Volume asymmetry value, ratio, and cancer risk. Breast Cancer Basic Clin. Res. 9, BCBCR.S32789 (2015).
Pusic, A. L. et al. Development of a new patient-reported outcome measure for breast surgery: The BREAST-Q. Plast. Reconstr. Surg. 124, 345–353 (2009).
Zingaretti, N. et al. A prospective investigation of predictive parameters for preoperative volume assessment in breast reconstruction. J. Clin. Med. 10, 5216 (2021).
Parmar, C., West, M., Pathak, S., Nelson, J. & Martin, L. Weight versus volume in breast surgery: An observational study. JRSM Short Rep. 2, 1–5 (2011).
Skarping, I. et al. Mammographic density changes during neoadjuvant breast cancer treatment: NeoDense, a prospective study in Sweden. The Breast 53, 33–41 (2020).
Yip, J. M. et al. Accurate assessment of breast volume: A study comparing the volumetric gold standard (direct water displacement measurement of mastectomy specimen) with a 3D laser scanning technique. Ann. Plast. Surg. 68, 135–141 (2012).
Kayar, R. et al. Five methods of breast volume measurement: A comparative study of measurements of specimen volume in 30 mastectomy cases. Breast Cancer Basic Clin. Res. 5, 43–52 (2011).
Xi, W. et al. Objective breast volume, shape and surface area assessment: A systematic review of breast measurement methods. Aesthetic Plast. Surg. 38, 1116–1130 (2014).
Fearn, N. et al. Reliability and measurement error of breast volume calculation using three-dimensional surface imaging. Lymphat. Res. Biol. https://doi.org/10.1089/lrb.2022.0015 (2022).
Itsukage, S., Sowa, Y., Goto, M., Taguchi, T. & Numajiri, T. Breast volume measurement by recycling the data obtained from 2 routine modalities. Mammography and Magnetic Resonance Imaging. Eplasty 17, e39 (2017).
Kim, H. et al. Preoperative magnetic resonance imaging-based breast volumetry for immediate breast reconstruction. Aesthetic Plast. Surg. 39, 369–376 (2015).
Osman, N. M., Botros, S. M., Ghany, A. F. A. & Farid, A. M. Contralateral breast volume measurement during chest CT for postmastectomy breast reconstruction. Int. J. Comput. Assist. Radiol. Surg. 10, 141–147 (2015).
Losken, A., Fishman, I., Denson, D. D., Moyer, H. R. & Carlson, G. W. An objective evaluation of breast symmetry and shape differences using 3-dimensional images. Ann. Plast. Surg. 55, 571–575 (2005).
Stahl, S. et al. Definitions of abnormal breast size and asymmetry: A cohort study of 400 women. Aesthetic Plast. Surg. 47, 2242–2252 (2023).
Estler, A. et al. Quantification of breast volume according to age and bmi: A three-dimensional mri analysis of 400 women. Aesthetic Plast. Surg. 47, 1713–1724 (2023).
Cheong, A. L. et al. Natural breast symmetry in preoperative breast cancer patients. Plast. Reconstr. Surg. - Glob. Open 7, e2297 (2019).
Kim, Y. S. et al. Prediction of implant size based on breast volume using mammography with fully automated measurements and breast MRI. Ann. Surg. Oncol. 29, 7845–7854 (2022).
Hidalgo, D. A. & Spector, J. A. Breast augmentation. Plast. Reconstr. Surg. 133, 567e–583e (2014).
O’Connell, R. L. et al. The potential role of three-dimensional surface imaging as a tool to evaluate aesthetic outcome after Breast Conserving Therapy (BCT). Breast Cancer Res. Treat. 164, 385–393 (2017).
Shammas, R. L. et al. Dissatisfaction After post-mastectomy breast reconstruction: A mixed-methods study. Ann. Surg. Oncol. 29, 1109–1119 (2022).
Baek, W. Y. et al. Patient satisfaction with implant based breast reconstruction associated with implant volume and mastectomy specimen weight ratio. J. Breast Cancer 20, 98–103 (2017).
Glovinski, P. V. et al. Avoiding a systematic error in assessing fat graft survival in the breast with repeated magnetic resonance imaging. Plast. Reconstr. Surg. - Glob. Open 4, e1023 (2016).
Acknowledgements
We are grateful to the breast cancer patients who provided data for this study.
Funding
The study was supported by the National Natural Science Foundation of China (Grant No. 82160340) and the Yunnan Talents Support Program (Grant No. XDYC-MY-2022–0064).
Author information
Authors and Affiliations
Contributions
X.L.D., C.D.L. and T.F.K. created the concept and design of this study. X.Y.Z., N.T. and G.C.L. were responsible for the statistical analysis. X.R.D. and C.D.L. drafted, revised, and edited the manuscript. All the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Du, X., Duan, X., Zhou, X. et al. A study on the correlation between MRI-assessed breast volume asymmetry and patient satisfaction after immediate breast reconstruction in breast cancer patients. Sci Rep 14, 30737 (2024). https://doi.org/10.1038/s41598-024-80522-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-80522-y