Abstract
Vitamin D is crucial for maintaining bone health and development, and bone mineral accumulation during childhood and adolescence affects long-term bone health. Vitamin D deficiency has been widely recognized as one of the main causes of osteoporosis and fractures, especially during the growth and development stage of children. Recent studies have shown that vitamin D deficiency may affect the deviation of bone development in children by mediating lipid metabolism disorders, but its specific mechanism of action has not been fully elucidated. In this study, through clinical correlation analysis, it was found that vitamin D deficiency was negatively correlated with lipid metabolism levels. Subsequently, lipidomic analysis of vitamin D-deficient mice and children showed that triglycerides were the main lipid metabolites. It was found that the triglyceride synthesis pathway plays a key role in bone development in vitamin D-deficient obese children. Our study found that vitamin D deficiency mediates bone dysplasia by affecting triglyceride synthesis. These findings provide new insights into the mechanisms by which vitamin D deficiency affects bone development in children, which may guide more precise clinical interventions and support the development of new clinical treatments.
Similar content being viewed by others
Introduction
Overweight, obesity, and deviations in bone development have recently emerged as significant public health concerns affecting the physical and mental health of children in China and adolescents globally. Obesity during childhood and adolescence is frequently accompanied by abnormal bone development, which increases the risk of early-onset chronic diseases such as cardiovascular disease and osteoporosis in adulthood. This scenario poses a substantial threat to health and imposes heavy burdens on individuals, families, and society1. According to the World Health Organization (WHO), more than 390 million children and adolescents aged 5–19 years are overweight, with the prevalence of overweight and obesity rising dramatically in this population2. Childhood obesity exerts excessive stress on the musculoskeletal system, leading to joint, bone, and muscle injuries, particularly in the large mid-axis joints. Consequently, obese children exhibit significantly higher rates of musculoskeletal discomfort, bone fractures, lower limb deformities, and mobility problems compared to their normal-weight peers3. Addressing obesity-related bone development issues in children is, therefore, of urgent importance.
Vitamin D is crucial for maintaining bone health and development, and bone mineral accumulation during childhood and adolescence affects long-term bone health4. Vitamin D deficiency has been widely recognized as one of the main causes of osteoporosis and fractures, especially during the growth and development stage of children5. Recent studies have shown that vitamin D deficiency may affect the deviation of bone development in children by mediating lipid metabolism disorders, but its specific mechanism of action has not been fully elucidated. Clinical interventions for bone growth deviations frequently involve oral or intravenous administration of alfa-osteol (1-hydroxyvitamin D3), osteotriol (1,25-dihydroxyvitamin D3), vitamin D3, or calcium carbonate with vitamin D36. Vitamin D absorption is influenced by ultraviolet radiation7, and excessive supplementation can increase the metabolic burden on the liver and kidneys in children. Additionally, the response to vitamin D supplementation in children with bone development deviations varies, and the overall efficacy is often unsatisfactory8. Clinically, it has been observed that obese or overweight children are frequently vitamin D deficient, exhibit more severe bone development deviations, and respond poorly to vitamin D supplementation.
Elevated plasma cholesterol levels have been demonstrated to downregulate the Wnt signaling pathway, thereby affecting the differentiation of mesenchymal stem cells (MSCs) into osteoblasts9,10. Additionally, oxidized lipids and cholesterol disrupt the balance of bone remodeling between osteoblasts and osteoclasts. Oxidized lipids prompt osteoblasts to secrete receptor activator of nuclear factor-κB ligand (RANKL), which in turn leads to the over-differentiation of osteoclasts and subsequent bone resorption11. Recent clinical studies have established a link between vitamin D and lipid metabolism12,13,14, revealing that low serum vitamin D levels are associated with an increased risk of lipid metabolism disorders15. Literature suggests that lipid metabolism may influence the effects of vitamin D on bone development by impacting adipocyte differentiation and function. Thus, maintaining optimal levels of both vitamin D and lipids is essential for normal bone development and function16,17. However, whether vitamin D influences bone development in children through lipid metabolism remains unclear.
In the present study, based on the initial 1562 samples from the Growth and Development Clinic, a negative correlation was identified between vitamin D deficiency and lipid levels, as evidenced by changes in serum 25(OH)D levels and lipid markers. To investigate whether vitamin D deficiency leads to lipid metabolism disorders or if lipid metabolism disorders progressively worsen vitamin D deficiency, we used a vitamin D-deficient dietary mouse model. This model demonstrated that vitamin D deficiency triggers weight gain and lipid metabolism disorders.Further analysis of targeted lipid metabolism revealed that vitamin D deficiency primarily induces lipid metabolism disorders through the glycerol ester metabolic pathway. We explored the potential mechanism by which vitamin D deficiency influences the glycerol ester metabolic pathway, leading to lipid metabolism disorders and subsequently affecting bone growth and development. These findings offer new insights and a foundation for diagnosing and treating children with clinical vitamin D deficiency.
Materials and methods
Experiments related to children
Study participants
A retrospective analytical study was conducted using the database of the paediatric growth and development clinic of the Gangnam University Hospital. Participants’ 25(OH)D, bone density, blood biochemistry indicator results and examination dates were extracted between 2020 and 2023 during visits for growth and development problems. Among 1562 children, we excluded individuals with incomplete personal information, incomplete indicator results, age < 3 or > 16 years, and comorbidities with other serious diseases. Finally, the analysis included 1200 children. All medical records underwent de-identification. This pilot study was approved by the research ethics committees of the Affiliated Hospital of Jiangnan University (Approval Number: LS2020046). All participants were fully informed about the study and provided written consent. We confirm that informed consent was obtained from all subjects and/or their legal guardians. We confirm that all methods have been carried out in accordance with the relevant guidelines and regulations. The study was reported in accordance with ARRIVE guidelines.
Evaluation criteria
-
①
Vitamin D deficiency: serum 25(OH)D level < 20 ng/ml; Vitamin D insufficiency: serum 25(OH)D level 20–< 30 ng/ml; Vitamin D sufficiency: serum 25(OH)D level ≥ 30 ng/ml.
-
②
Referring to the Classification Standard for Body Mass Index Values for Screening Overweight and Obesity in Chinese School-Age Children and Adolescents18, overweight: body mass index (BMI) ≥ 85th percentile value for the same age and gender (P85); obesity: BMI ≥ 95th percentile value for the same age and gender (P95).
Analysis of serum levels of 25(OH)D and lipid markers in children
Calculation formula: The calculation formula for Pearson correlation coefficient is r = ∑ [(xi–\({\overline{\text{x}}}\)) (yi−\({\overline{\text{y}}}\))]/√ [∑ (xi−\({\overline{\text{x}}}\))2 ∑ (yi–\({\overline{\text{y}}}\))2], where xi and yi represent the values of two variables at each observation point, \({\overline{\text{x}}}\) and \({\overline{\text{y}}}\) represent the mean of the variables, and ∑ represents the summation sign.Value range: The Pearson correlation coefficient ranges between − 1 and 1. A value close to 1 indicates a strong positive correlation between two variables. A value close to − 1 indicates a strong negative correlation between two variables. A value close to 0 indicates that there is no clear linear relationship between two variables.
AUC (Area Under Curve) is defined as the area under the ROC curve. The ROC curve, also known as receiver operating characteristic curve, is a curve plotted based on a series of different binary classification methods (threshold or threshold), with true positive rate (sensitivity) as the y-axis and false positive rate (1-specificity) as the x-axis. When the AUC was between 0.7 and 0.9, the gene or metabolite was considered to have some differentiation between groups, and when the AUC > 0.9, the gene or metabolite was considered to have good differentiation between groups. Otherwise, statistical significance was observed in all ROC models.
Inclusion criteria
The included research subjects were all free from abnormalities in vital organs such as the liver, kidneys, and heart, as well as endocrine system diseases and abnormalities or deformities in physical development. Additionally, they had obtained the consent of their child’s guardian, who voluntarily signed an informed consent form.
Experimental animals and groups
SPF C57BL/6J mice (female, 4 weeks old, provided by Beijing huafukang Biotechnology Co., Ltd.) were divided into natural diet group (ND) and vitamin D deficiency diet (VDD) group, with six mice in each group. All experimental procedures followed the National Institute of Health’s guidelines and were approved by the Animal Ethics Association of Jiangnan University (approval ID: JN.No20230830c0241230[346]). All efforts were made to reduce the number of animals sacrificed and ensure minimal suffering. The experimental design was shown in Fig. 3A. All mice were housed at 20–24 °C and 50% relative humidity with a 12-h light/dark cycle. Mouse euthanasia process: Carbon dioxide method. The experimental animals were put into the carbon dioxide anaesthesia box, the carbon dioxide gas valve was opened, and when the animals gradually lost consciousness, the carbon dioxide concentration was increased to 100%, the animals showed an unconscious state, and the ventilation was continued for 2 min in order to determine the death of the mice. The study was reported in accordance with ARRIVE guidelines.
Micro-CT analysis
The mouse femurs isolated from ageand sex-matched mice were skinned and fixed in 70% ethanol. Scanning was performed with the Skyscan1276 Micro-CT. The mouse femurs were scanned at a 9-μm resolution for quantitative analysis. Three-dimensional (3D) images were reconstructed using a fixed threshold.
Dietary components
Natural diet: moisture ≤ 100, crude protein ≥ 180, crude fat ≥ 40, crude fiber ≤ 50, crude ash ≤ 80, calcium 10–18, phosphorus 6–12. Vitamin D deficiency diet: moisture ≤ 100, crude protein ≥ 180, crude fat ≥ 40, crude fiber ≤ 50, crude ash ≤ 80, phosphorus 6–12.
Statement
We confirm that informed consent was obtained from all subjects and/or their legal guardians. We confirm that all methods have been carried out in accordance with the relevant guidelines and regulations. The study was reported in accordance with ARRIVE guidelines.
Hematoxylin eosin (HE) staining and Masson staining
A mouse was randomly selected from each group, and femur tissues were collected to be conventionally immersed in 4% paraformaldehyde at room temperature for one night, routinely dehydrated, embedded, prepared, and stained with HE and Masson. The specimens were then observed under an optical microscope (microscope model: NIKON Eclipse ci; imaging system: NIKON digital sight DS-FI2). Each slice in each group selected three fields of vision to take photos, and as many tissues as possible filled the entire field of vision to ensure that the background light of each photo was consistent with Image-Pro Plus 6.0.
Quantitative real-time PCR
Total RNA was isolated from femur tissue using TRIzol (Takara, Shiga, Japan) according to the manufacturer’s protocol.Subsequently, RNA extracted from each sample was reverse transcribed into complementary DNA (cDNA) using the PrimeScriptTM RT kit (Takara, Shiga, Japan). The relative expression of mRNA was determined by the 2-ΔΔCT method and the expression values were normalised to the glyceraldehyde 3-phosphate dehydrogenase (GAPDH) gene. The specific sequences used in this study are shown in Table 1.
Western blot analysis
The samples underwent a 10-min boiling process, followed by separation using sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) and subsequent transfer to polyvinylidene fluoride (PVDF) membranes (Millipore, Billerica, MA, USA). These membranes were then treated with bovine serum albumin and exposed to primary antibody overnight at a 4 °C temperature, suitably diluted. Following three washes with tris-buffered saline and Tween (TBST), the membranes were subjected to incubation with horseradish peroxidase (HRP)-conjugated secondary antibody at room temperature for 1 h. Specifics regarding the antibodies utilized in the Western blot analysis are outlined in Table 2. Subsequently, the membranes underwent incubation with the Enhanced Chemiluminescence (ECL) detection kit (Proteintech Group, Inc., Rosemont, IL, USA) to facilitate membrane visualization. The density of protein bands was quantified using Image J software (Pierce, Rockford, IL, USA), and the obtained data were normalized to GAPDH.
Absolute quantitative lipidomics
Metabolite extraction and quality control sample
After the serum samples were thawed slowly at 4 °C, take an appropriate amount of samples and add 200 μL of methanol, vortex to mix, add 10 μL of internal standard mixture, add 800 μL of methyl tertiary-butyl ether (MTBE), vortex to mix, sonicate for 20 min in a low-temperature water bath, and then leave it at room temperature for 30 min, add 200 μL of mass spectrometry-grade water, vortex to mix, and then centrifuge at 14,000 rpm for 15 min at 4 °C. For mass spectrometry analysis, add 200 μL of 90% isopropanol/acetonitrile solution, vortex thoroughly, centrifuge at 14,000 rpm for 15 min at 4 °C, and take the supernatant into the sample for analysis.
The separation of the samples was carried out on an LC-30AD UHPLC system using C18 and Amino columns. C18 column: column temperature 45 °C; flow rate 0.35 mL/min; mobile phase composition A: 70% acetonitrile + 30% water + 5 mM ammonium acetate, B: isopropanol solution, the gradient elution procedure was as follows: 0–5.0 min, B varied linearly from 20 to 60%, 5.0–13.0 min, B varied linearly from 60 to 100%, 13.1–17.0 min, B was maintained at 60% to 100%. The gradient elution procedure was as follows: 0–5.0 min, B varied linearly from 20 to 60%, 5.0–13.0 min, B varied linearly from 60 to 100%, 13.1–17.0 min, B was maintained at 20%.
A: 2 mM ammonium acetate + 50% methanol + 50% acetonitrile, B: 2 mM ammonium acetate + 50% acetonitrile + 50% water, the gradient elution procedure was as follows: 0–3.0 min, B was maintained at 3%, 3.0–13.0 min, B varied linearly from 3 to 100%, 13.0 min- 17.0 min, B was maintained at 20%. From 3.0 to 13.0 min, B was linearly varied from 3 to 100%, from 13.0 min to 17.0 min, B was maintained at 100%, and from 17.1 min to 22.0 min, B was maintained at 3%. The samples were placed in an autosampler at 10 °C throughout the analysis. To avoid the effects caused by fluctuations in the instrumental detection signal, the samples were analysed sequentially in a random order.
Detection was carried out using electrospray ionisation (ESI) in positive and negative ion modes, respectively. The samples were separated by UHPLC and analysed by mass spectrometry using an AB 6500 + QTRAP mass spectrometer (AB SCIEX).The ESI source conditions were as follows: Source temperature: 400 °C, Ion Source Gas1 (GS1): 50, Ion Source Gas2 (GS2): 55, Curtain Gas (CUR): 35, IonSpray Voltage (IS): + 3000 V or − 2500 V in Curtain Gas (CUR): 35, IonSpray Voltage (IS): + 3000 V or − 2500 V in positive or negative modes, respectively, monitored in MRM mode.
Multivariate statistical analysis
Orthogonal partial least squares discriminate analysis (OPLS-DA) was used for statistical analysis to determine global metabolic changes between comparable groups. All metabolite variables were scaled to Pareto Scaling before conducting OPLS-DA. The model validity was evaluated from model parameters R2 and Q2, which provide information regarding the interpretability and predictability, respectively, of the model and avoid the risk of over-fitting. Variable importance in the projection (VIP) was calculated in OPLS-DA model. P-values were estimated using the paired Student’s t-test on singledimensional statistical analysis.
Differential metabolites analysis
Statistically significant groups were selected with a VIP value of more than 1 and a p-value of less than 0.05. The differential metabolites between the two groups were summarized and mapped into their biochemical pathways through metabolic enrichment and pathway analysis based on a database search (KEGG, http://www.genome.jp/kegg/). These metabolites can be categorized based on the pathways or functions in which they participate. Enrichment analysis examines the presence or absence of a group of metabolites in a function node. The principle is that the annotation analysis of a single metabolite develops into an annotation analysis of a group of metabolites. scipy.stats (Python packages) (https://docs.scipy.org/doc/scipy/) was used to identify a statistically significantly enriched pathway using Fisher’s exact test.
Statistical analyses
The data were analysed using SPSS 27.0 software, and the count data were expressed as the number of cases (n) and percentage (%) using the χ2 test; the serum 25(OH)D level was expressed as the mean ± standard deviation (χ ± S), and comparisons between multiple groups were made using one-way ANOVA, and comparisons between two groups were made using the t-test; and the relationship between BMI and serum 25(OH)D level was analysed using Pearson’s correlation analysis.
Results
Vitamin D deficiency is significantly and negatively associated with elevated triglyceride levels in growing children
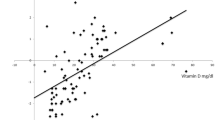
In order to study whether there is a correlation between 25(OH)D levels and lipid metabolism, we collated 1562 original child cases from the growth and development clinic, from which 1200 cases were screened and analysed (Fig. 1A, Supplementary Table 1). The average serum 25(OH)D level of 1200 children was (25.66 ± 9.46)nmol/L, and the overall proportion of vitamin D deficiency and insufficiency was as high as 74.08% (889/1200). The adequate rate of vitamin D was only 25.93%, and there was no statistically significant difference in serum 25 (OH) D levels between children of different genders (all P > 0.05), as shown in Table 3. The correlation analysis heatmap showed that 25(OH)D level was negatively correlated with triglyceride and cholesterol levels, and positively correlated with bone mineral density level (Fig. 1B). Pearson correlation analysis showed that triglyceride (TG) was negatively correlated with serum 25(OH)D level, cholesterol (CHOL) was negatively correlated with serum 25(OH)D level (p ≤ 0.001), and bone mineral density was positively correlated with serum 25(OH)D levels were positively correlated (Fig. 1C). There was no significant linear correlation between HDL, LDL and alkaline phosphatase and 25(OH)D levels. Based on 1200 outpatient cases, the ROC curves plotted by 25(OH)D levels and lipid-related metabolites are shown in Fig. 1D. When the AUC was between 0.7 and 0.9, the gene or metabolite was considered to have some differentiation between groups, and when the AUC > 0.9, the gene or metabolite was considered to have good differentiation between groups. Otherwise, statistical significance was observed in all ROC models. As shown in Fig. 1E, elevated triglyceride (TG) levels increased the risk of 25(OH)D deficiency, increased bone mineral density (BMD) decreased the risk of 25(OH)D deficiency, and the remaining metrics were not statistically significant. The above results indicate that the level of 25(OH)D is correlated with the level of lipid metabolism, especially triglyceride (TG) is significantly negatively correlated with 25(OH)D level.
Vitamin D deficiency is significantly and negatively associated with elevated triglyceride levels in growing children. (A) Clinical sample collection experimental design. (B) Heatmap of lipid correlation analysis with 25(OH)D. (C) Pearson correlation analysis of 25(OH)D with TG, CHOL, and BMD. (D) The receiver operating characteristic curve (ROC) of 25(OH)D-related indicators. (E) Forest plot of the relevant metabolic indicators associated with 25(OH)D deficiency.
Changes in lipid metabolites and functional analyses in serum from clinical samples
Similarly, to further explore the correlation between vitamin D deficiency and lipid metabolism, we performed lipid metabolomics on sera from children with vitamin D deficiency (VDD) and normal vitamin D (CON).OPLS-DA plots explained 26% and 11.6% of the total variance for Component 1 and Component 2, respectively (Fig. 2A). The distances between the plots reflect relative differences in community structure, suggesting that vitamin D deficiency alters the expression of lipid metabolites. up- or down-regulation of differential TG expression in sera from the CON and VDD groups is highlighted (Fig. 2B). Using |log2fc|> 0.5, p < 0.05 as a criterion, vitamin D deficiency caused elicited significant differences in 80 metabolites, of which 35 were up-regulated and 45 were down-regulated (Fig. 2B, Supplementary Table 2). The heatmap depicted the changes in the expression of the top differential metabolites among the differential metabolites, and the changes were mainly focused on the triglyceride metabolites, further demonstrating the involvement of vitamin D deficiency in the changes in the expression of certain metabolites in lipid metabolism (Fig. 2C). In order to reveal the specific biological functional pathways designed for the differential metabolites associated with the interaction of vitamin D deficiency with lipid metabolism, differential enrichment of differential genes in the metabolite libraries was performed using the KEGG database. Differential metabolites were mainly enriched for glycerophospholipid metabolism, fat digestion and absorption, and triglyceride metabolism (Fig. 2D). Vitamin D-deficient and vitamin D-normal children differed at the level of serum lipid metabolite expression, with the major differential metabolites concentrated in triglyceride metabolites, and with differential metabolite distribution in glycerophospholipid metabolism, fat digestion and absorption, and glyceride metabolism pathways.
Changes in lipid metabolites and functional analyses in serum from clinical samples. (A) PLS-DA plots explain 26% and 11.6% of the total variance for Component 1 and Component 2, respectively. The distance between plots reflects the relative differences in community structure. (B) Differences in lipid metabolite expression between the CON and VDD groups. Up- or down-regulated genes are highlighted. (C) Heatmap analysis of the top 20 selected genes in the kidneys of the CON and VDD groups. (D) Top 20 KEGG-enriched pathways based on differential metabolite ranking.
Disorders of lipid metabolism and deviations in bone development in mice due to a vitamin D-deficient diet
To explore whether vitamin D deficiency causes disorders of lipid metabolism or vitamin D deficiency due to disorders of lipid metabolism, we conducted animal experiments with vitamin D-deficient feed interventions (Fig. 3A). Mice fed with vitamin D deficient food showed significant obesity and a significant decrease in serum 25 (OH) D levels (Fig. 3B) and gained significant weight (Fig. 3C). When bone density and microstructure were analysed by micro-computed tomography (micro-CT), it was found that bone trabecular mass was significantly reduced in vitamin D-deficient feed-fed mice (Fig. 3D), and compared with the control (Control) group, the bone trabecular volume/total volume (BV/TV), the number of trabeculae (Tb.N), the thickness of the trabeculae (Tb.Th), and the separation of the trabeculae (Tb. Sp), and increased structural pattern index (SMI) (Fig. 3E).HE staining was used to observe pathological changes in bone trabeculae (Fig. 3F), and the number of bone trabeculae was significantly reduced in vitamin D-deficient diet mice. These findings suggest that mice with a vitamin D-deficient diet may have disrupted lipid metabolism and inhibited bone development.
Disorders of lipid metabolism and deviations in bone development in mice due to a vitamin D-deficient diet. (A) Experimental design for vitamin D deficiency dietary intervention in mice. (B) Comparison of body size of mice in ND and VDD groups. (C) Comparison of body weights of mice in ND and VDD groups. (n = 6, mean ± SEM; ***p < 0.01). (D) Representative micro-CT images of femur trabecular bone (scale bar, 9 mm) from 12-week-old C57BL/6 J mice. (E) Quantification of femur trabecular bone. (n = 6, mean ± SEM; ***p < 0.01). (F) HE staining of femur (scale bar, 20 μm), quantitative evaluation of femur trabecular bone (n = 6, mean ± SEM; ***p < 0.01).
Changes in lipid metabolites and functional analysis in mouse serum
To investigate the role played by vitamin D deficiency in disorders of lipid metabolism, lipid metabolomics was performed in normal and vitamin D-deficient groups of mice. OPLS-DA plots explained 41.9% and 19.2% of the total variance in Component 1 and Component 2, respectively. The distances between plots reflected relative differences in community structure (Fig. 4A), suggesting that vitamin D deficiency altered the expression of lipid metabolites. up- or down-regulation of differential TG expression in serum from the ND and VDD groups was highlighted (Fig. 4B). Using |log2fc|> 0.5, p < 0.05 as a criterion, vitamin D deficiency caused caused significant differences in 600 metabolites, of which 530 were up-regulated and 70 were down-regulated (Fig. 4B, Supplementary Table 3). The heatmap depicted the changes in the expression of the top differential metabolites among the differential metabolites, and the changes were mainly focused on triglyceride metabolites, further demonstrating the involvement of vitamin D deficiency in the changes in the expression of certain metabolites in lipid metabolism (Fig. 4C). In order to reveal the specific biological functional pathways designed for the differential metabolites associated with the interaction of vitamin D deficiency with lipid metabolism, differential enrichment of differential genes in the metabolite libraries was performed using the KEGG database. Differential metabolites were mainly enriched for glycerophospholipid metabolism, fat digestion and absorption, and triglyceride metabolism (Fig. 4D). Vitamin D-deficient and vitamin D-normal mice differed at the level of serum lipid metabolite expression, with the major differential metabolites concentrated in triglyceride metabolites, and with differential metabolite distribution in glycerophospholipid metabolism, fat digestion and absorption, and glyceride metabolism pathways.
Changes in lipid metabolites and functional analysis in mouse serum. (A) PLS-DA plots explained 41.9% and 19.2% of the total variance for Component 1 and Component 2, respectively. The distances between the plots reflect the relative differences in community structure. (B) Differences in lipid metabolite expression between ND and VDD groups. Up- or down-regulated genes are highlighted. (C) Heatmap analysis of the top 20 selected genes in the kidneys of the ND and VDD groups. (D) Top 20 KEGG-enriched pathways based on differential metabolite ranking.
Validation of glycerol ester pathway-related proteins and gene expression
The above studies showed that the common differential metabolites that were upregulated in children and mice were predominantly triglycerides and that the differential metabolites were enriched in the triglyceride pathway. Wayne diagram analysis showed that 19 common differential metabolites were screened in mice and children (Fig. 5A). These common differential metabolites were predominantly triglyceride metabolites (Fig. 5B). Masson staining showed that vitamin D-deficient mice had a significantly diminished capacity for dietary new bone (Fig. 5C). We examined the expression of osteogenesis-related proteins runx2 and COL-1, and the results showed that vitamin D-deficient (VDD) mice had lower protein expression of RUNX2 and COL-1 compared with the control (ND) group (Fig. 5D). Similarly, we examined the expression of GPAT4, AGPAT1, and DGAT2 proteins in the triglyceride synthesis pathway. The results showed higher expression of GPAT4, AGPAT1, and DGAT2 proteins in vitamin D-deficient mice (Fig. 5E). qPCR results showed the same support for the above results at the gene level, with lower expression of RUNX2 and COL-1 genes in vitamin D-deficient mice (Fig. 5F), and higher expression of GPAT4, AGPAT1, and DGAT2 genes (Fig. 5G). These findings suggest that vitamin D deficiency may reduce osteogenic transformation by affecting the triglyceride synthesis pathway in the glyceride pathway (Fig. 5H).
Validation of glycerol ester pathway-related proteins and gene expression. (A) Venn diagram summarising changes in lipid metabolites on a vitamin D-deficient diet. (B) The common differential metabolite in children and mice was triglycerides. (C) Masson staining of femur (scale bar, 20 μm) for quantitative evaluation of new bone (n = 6, mean ± SEM; *p < 0.05,** < 0.01,***p < 0.001). (D) Western-blotting showing RUNX2, COL-1 protein levels in ND and VDD groups. (n = 3, mean ± SEM; *p < 0.05,** < 0.01,***p < 0.001). (E) Western-blotting showing GPAT4, AGPAT1, DGAT2 protein levels in ND and VDD groups. (n = 3, mean ± SEM; *p < 0.05,** < 0.01,***p < 0.001) (F) Real-time quantitative PCR showing the levels of RUNX2, COL-1 genes in ND and VDD groups. (n = 6, mean ± SEM; *p < 0.05,** < 0.01,***p < 0.001) (G) Real-time quantitative PCR showing the levels of GPAT4, AGPAT1, DGAT2 genes in ND and VDD groups. (n = 6, mean ± SEM; *p < 0.05,** < 0.01,***p < 0.001) (H) Triglyceride synthesis pathway.
Discussion
In recent years, an increasing number of studies have been carried out on the role of vitamin D in the human body, due to its multiple effects on health19. To explore these effects, we utilized a mouse model to examine the impact of a vitamin D-deficient diet on lipid metabolism and bone health. Our study revealed that mice on a vitamin D-deficient diet exhibited disrupted lipid metabolism, aligning with epidemiological findings that indicate lower serum 25(OH)D levels in obese individuals20,21. Circulating concentrations of 25(OH)D are now considered to be the best marker of vitamin D status22. Consequently, we focused on the relationship between 25(OH)D levels and lipid metabolism, and we explored potential mechanisms through which these interactions may influence bone development.
Vitamin D and its metabolite 25(OH)D have been reported to be stored in adipose tissue. Consistent with current findings, a meta-analysis examining vitamin D status and lipid levels in children and adolescents revealed that serum 25-hydroxyvitamin D levels were negatively correlated with hypertriglyceridemia, hypercholesterolemia, and high LDL-C levels, while being directly associated with serum hypercholesterolemia23. Additionally, a meta-analysis of randomized controlled trials found that vitamin D supplementation significantly reduced LDL-C levels24. Another meta-analysis in adults demonstrated that vitamin D supplementation had a significant positive impact on various lipid profiles, including total cholesterol, low-density lipoproteins (LDL-C), and high-density lipoproteins (HDL-C), leading to improved lipid levels25.
Current studies have proposed several mechanisms to explain the relationship between serum 25-hydroxyvitamin D levels and lipid metabolism. Firstly, vitamin D inhibits the activity of sterol regulatory element-binding proteins, which are essential for the synthesis and absorption of cholesterol and fatty acids in the body26. Secondly, increased calcium uptake in the gut, facilitated by serum 25-hydroxyvitamin D, reduces hepatic triglyceride (TG) secretion and synthesis27. Thirdly, vitamin D’s inhibition of parathyroid hormone function suppresses lipogenesis, leading to decreased serum TG levels28. Lastly, vitamin D deficiency impairs insulin sensitivity, which in turn elevates TG and LDL-C production while reducing HDL-C synthesis29.
Thus, vitamin D deficiency plays an important role in lipid metabolism disorders and may affect bone growth and development.
In this study, utilizing an initial sample of 1562 cases from a growth and development clinic, we observed a negative correlation between vitamin D deficiency and lipid levels, as indicated by changes in serum 25(OH)D levels and lipid markers. To further investigate whether vitamin D deficiency leads to disordered lipid metabolism or is a consequence of it, we used a vitamin D-deficient dietary mouse model. This model demonstrated that vitamin D deficiency induced weight gain and disrupted lipid metabolism. Further analysis of targeted lipid metabolism suggests that vitamin D deficiency may mainly lead to lipid metabolism disorders through the glyceryl ester metabolism pathway. We explored the potential mechanisms by which vitamin D deficiency affects the glycerol ester metabolic pathway, leading to lipid metabolism disorders and consequently impacting bone growth and development. These findings offer new insights and a foundation for diagnosing and treating vitamin D deficiency in children in clinical settings.
Clinical and basic research indicates that vitamin D deficiency mediates lipid metabolism disorders, which in turn affect bone growth and development. In vivo animal experiments have shown that there may be a relationship between lipid metabolism and bone metabolism homeostasis. This paper examines the impact of vitamin D deficiency and lipid metabolism disorders on bone growth and development, aiming to elucidate the molecular mechanisms involved. However, since lipid metabolism involves multiple organs and cells with complex regulatory mechanisms, further research is needed to clarify the relationship between different types of lipids and their metabolism, and bone growth and development. Although this study observed some associations between vitamin D deficiency and lipid metabolism disorders and bone development, it did not provide direct evidence to confirm the specific effects of lipid metabolism disorders on bone development. Further exploration is needed in this area for future research.
In conclusion, accumulating evidence supports the notion that vitamin D deficiency-mediated lipid metabolism disorders are closely linked to the development of bone deviations. This provides new insights for the safe and rational selection of pharmacological therapies for preventing and treating bone growth and developmental deviations in children.
Conclusion
This study demonstrated that the lipid metabolism disorder mediated by vitamin D deficiency affecting bone development may be closely related to the triglyceride synthesis pathway. In summary, this study emphasizes the potential role of lipid metabolism disorders in bone deviation and suggests that the triglyceride synthesis pathway may be a key mechanism. Taken together, this study emphasizes the potential role of lipid metabolism disorders in bone deviation and suggests that the triglyceride synthesis pathway may be a key mechanism.
Data availability
Data supporting the results of this study are not publicly available due to sensitivity reasons and can be obtained from the corresponding author upon reasonable request. The data are stored in controlled access data storage at the Affiliated Hospital of Jiangnan University.
Abbreviations
- VDD:
-
Vitamin D deficiency
- ND:
-
Normal diet
- CON:
-
Control group
References
Zeljkovic, A., Vekic, J. & Stefanovic, A. Obesity and dyslipidemia in early life: impact on cardiometabolic risk. Metabolism 156, 155919 (2024).
Chen, S. T. et al. Meeting 24-h movement guidelines: prevalence, correlates, and the relationships with overweight and obesity among Chinese children and adolescents. J. Sport Health Sci. 10(3), 349–359 (2021).
Pollock, N. K. Childhood obesity, bone development, and cardiometabolic risk factors. Mol. Cell Endocrinol. 410, 52–63 (2015).
Holick, M. F. Vitamin D deficiency. N. Engl. J. Med. 357(3), 266–281 (2007).
Winzenberg, T. et al. Effects of vitamin D supplementation on bone density in healthy children: systematic review and meta-analysis. BMJ 342, c7254 (2011).
Rao, Y. K. et al. Increment in vitamin D level and bone mineral accrual in children with vitamin D deficiency. Korean J. Pediatr. 59(7), 292–297 (2016).
Saponaro, F., Saba, A. & Zucchi, R. An update on vitamin D metabolism. Int. J. Mol. Sci. 21(18), 6573 (2020).
Winzenberg, T. M. et al. Vitamin D supplementation for improving bone mineral density in children. Cochrane Database Syst. Rev. 2010(10), CD006944 (2010).
You, L. et al. High cholesterol diet increases osteoporosis risk via inhibiting bone formation in rats. Acta Pharmacol. Sin. 32(12), 1498–1504 (2011).
Lin, G. L. & Hankenson, K. D. Integration of BMP, Wnt, and notch signaling pathways in osteoblast differentiation. J. Cell Biochem. 112(12), 3491–3501 (2011).
Tintut, Y. & Demer, L. L. Effects of bioactive lipids and lipoproteins on bone. Trends Endocrinol. Metab. 25(2), 53–59 (2014).
de Souza Silva, J. et al. Obesity, related diseases and their relationship with vitamin D deficiency in adolescents. Nutr. Hospital. 33(4), 856–864 (2016).
Ceruti, D. et al. Vitamin D levels and lipid profile in children and adolescents: a tight correlation. Miner. Pediatr. (Torino) (2024).
Jorde, R. & Grimnes, G. Vitamin D and metabolic health with special reference to the effect of vitamin D on serum lipids. Prog. Lipid Res. 50(4), 303–312 (2011).
Singh, A. & Singh, N. Vitamin D intervention as a curative measure for glucose intolerance in obese children and adolescents: a systematic review on randomized control trials. Eur. J. Pediatr. 2024, 1–9 (2024).
Gu, P. et al. Effects of vitamin D deficiency on blood lipids and bone metabolism: a large cross-sectional study. J. Orthop. Surg. Res. 18(1), 20 (2023).
Bao, L. et al. Vitamin D deficiency linked to abnormal bone and lipid metabolism predicts high-risk multiple myeloma with poorer prognosis. Front. Endocrinol. (Lausanne) 14, 1157969 (2023).
Zhonghua, L., Xing, B. & Xue, Z. Z. Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Zhonghua Liu Xing Bing Xue Za Zhi 25(2), 97–102 (2004).
Dibaba, D. T. Effect of vitamin D supplementation on serum lipid profiles: a systematic review and meta-analysis. Nutr. Rev. 77(12), 890–902 (2019).
Cheng, L. The convergence of two epidemics: vitamin D deficiency in obese school-aged children. J. Pediatr. Nurs. 38, 20–26 (2018).
Pereira Santos, M. et al. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes. Rev. 16(4), 341–349 (2015).
Zerwekh, J. E. Blood biomarkers of vitamin D status. Am. J. Clin. Nutr. 87(4), 1087S-1091S (2008).
Valensi, P. et al. Atherogenic dyslipidemia and risk of silent coronary artery disease in asymptomatic patients with type 2 diabetes: a cross-sectional study. Cardiovasc. Diabetol. 15, 1–10 (2016).
Wang, H. et al. Influence of vitamin D supplementation on plasma lipid profiles: a meta-analysis of randomized controlled trials. Lipids Health Dis. 11, 1–9 (2012).
Mirhosseini, N., Rainsbury, J. & Kimball, S. M. Vitamin D supplementation, serum 25 (OH) D concentrations and cardiovascular disease risk factors: a systematic review and meta-analysis. Front. Cardiovasc. Med. 5, 87 (2018).
Asano, L. et al. Vitamin D metabolite, 25-hydroxyvitamin D, regulates lipid metabolism by inducing degradation of SREBP/SCAP. Cell Chem. Biol. 24(2), 207–217 (2017).
Cho, H. et al. The possible role of Ca2+ on the activation of microsomal triglyceride transfer protein in rat hepatocytes. Biol. Pharmaceut. Bull. 28(8), 1418–1423 (2005).
Zemel, M. B. et al. Regulation of adiposity by dietary calcium. FASEB J. 14(9), 1132–1138 (2000).
Sung, C. et al. Role of vitamin D in insulin resistance. BioMed Res. Int. 2012, 1–12 (2012).
Funding
The study was supported by the Jiangsu Provincial Medical Association paediatric special scientific research surface project (SYH-32034-0074(20230021)), Wuxi Science and Technology Bureau of Taihu Lake Light Scientific Research Top Level Project (Y20222005).
Author information
Authors and Affiliations
Contributions
TT W, X T, CY Z participated in study design. TT W, H W, TZ C, YT Y searched databases, conducted animal experiment operation. TT W, ZY Z, helped to draft and revise the manuscript. TT W, DS M,BJ Z, WX Q carried out the statistical analysis of data.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This pilot study was approved by the research ethics committees of the Affiliated Hospital of Jiangnan University (Approval Number: LS2020046). All experimental procedures followed the National Institute of Health’s guidelines and were approved by the Animal Ethics Association of Jiangnan University (approval ID: JN.No20230830c0241230[346]).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, T., Wang, H., Zhang, Zy. et al. A new perspective on bone development in vitamin D deficiency-associated obese children. Sci Rep 14, 31482 (2024). https://doi.org/10.1038/s41598-024-83079-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-83079-y