Abstract
The combined impact of concurrent primary Sjögren’s syndrome (pSS) and autoimmune thyroid disease (AITD) on pregnancy outcomes remains underreported. A retrospective analysis was conducted on 115 pregnant patients diagnosed with pSS and delivering at the Third Affiliated Hospital of Guangzhou Medical University from January 2009 to July 2023. The effects of AITD on maternal and neonatal outcomes were examined and compared to a control group without AITD. In the group with pSS and AITD, the pregnancy loss rate was significantly higher than in the non-AITD group (P = 0.015), primarily reflected in the increased rate of neonatal death (P = 0.029). The proportion of term births and vaginal deliveries in the AITD group was notably reduced compared to the non-AITD group (54% vs. 81.5%; 16.0% vs. 41.5%; P = 0.001 and P = 0.003, respectively). No significant differences were observed in other maternal pregnancy outcomes, including induced abortion, spontaneous abortion, therapeutic abortion, and premature delivery (P > 0.05). The average birth weight of newborns in the pSS with AITD group was significantly lower than in the pSS without AITD group (2587.70 ± 720.50 g vs. 2812.54 ± 495.30 g, P < 0.001). Additionally, the rate of low-birth-weight infants in the pSS with AITD group was higher than in the pSS without AITD group (39.0% vs. 19.7%, P = 0.032). However, no significant differences were found between the two groups in the rates of fetal death, neonatal live birth, and fetal distress (P > 0.05). These results emphasize the importance of monitoring and managing thyroid health during pregnancy to optimize maternal and neonatal outcomes. Further exploration is essential to unravel the precise mechanisms through which AITD impacts fetal growth and to identify potential interventions to mitigate these effects.
Similar content being viewed by others
Introduction
Sjögren’s Syndrome (SS) is a chronic and systemic autoimmune disease characterized by the progressive lymphocytic and plasmacytic infiltration of salivary and lacrimal glands, resulting in xerostomia and dry keratoconjunctivitis, accompanied by the production of autoantibodies1. The global prevalence of SS is approximately 0.3 –1‰, primarily affecting women 2. Although SS does not affect fertility in female patients, it may mutually interact with pregnancy, leading to adverse pregnancy outcomes.
Primary Sjögren’s Syndrome (pSS) refers to the condition occurring independently, not associated with definitive diagnoses of connective tissue diseases (CTD) such as rheumatoid arthritis, systemic lupus erythematosus (SLE), or polymyositis. AITD is a set of thyroid disorders resulting from autoimmunity dysregulation and represents the most common human autoimmune disease, with overall prevalence rates of approximately 5%3.
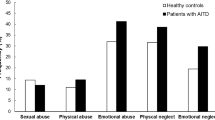
A significant correlation between AITD and rheumatic maladies, particularly Systemic Lupus Erythematosus (SLE) and Sjögren’s Syndrome (SS), has been underscored. In recent years, many studies have reported that although pSS does not affect the fertility of women of childbearing age, it can interact with pregnancy and lead to adverse pregnancy outcomes. A research team, spearheaded by Ji Linong, discovered that thyroid peroxidase antibody (TPOAb) positivity correlates with preterm birth among pregnant women with normal thyroid function4. Negro et al. documented a heightened incidence of miscarriage and preterm birth in TPOAb-positive euthyroid pregnant women compared to their TPOAb-negative counterparts5. Elena Borodina’s group administered IgG derived from TPOAb-positive patients into a mouse model, authenticated the correlation between thyroid autoantibodies and fetal loss, which study uncovered smaller mouse embryos, diminished placental weight, elevated pregnancy loss, and delayed fetal development6. The existence of TPOAb not only correlates with diminished serum anti-Müllerian hormone (AMH) levels and reduced antral follicle counts but also directly affects the oocyte zona pellucida, leading to compromised quality and developmental potential. Consequently, females suffering from autoimmune thyroiditis exhibit a decreased fertilization rate and a diminished proportion of high-quality embryos.
Research showed that approximately 16% of patients with SS concurrently endure AITD7. And, upon assessing thyroid autoantibodies in 33 patients with pSS, researchers discovered that 45% were positive for anti-TPOAb and 18% for anti-thyroglobulin antibody (TGAb)3. It’s worth noting that approximately 40% of individuals with SS concurrently suffer from thyroid disease, with AITD being the most prevalent8. The concurrent presence of SS and AITD is prevalent and may be attributed to shared pathogenic mechanisms. However, research exploring the impact of pSS accompanied by AITD on pregnancy outcomes is relatively scarce. This study collected clinical data from pSS pregnant patients and divided them into two groups: those concurrent with AITD and those without AITD. A retrospective analysis was conducted to scrutinize the influence of concomitant AITD on pregnancy outcomes in pSS pregnant patients. The findings emphasize the necessity of comprehensive care and meticulous monitoring for pregnant women with pSS and concurrent AITD, contributing to the development of tailored therapeutic approaches in the management of these complex conditions.
Patients and methods
Patients and data collection
Pregnant women diagnosed with primary Sjögren’s syndrome at the Third Affiliated Hospital of Guangzhou Medical University from 2009 to 2023 were collected and analyzed. The maternal and neonatal outcomes between pregnant women with and without autoimmune thyroid disease (AITD) were compared. A total of 115 cases were included, with 50 cases of pregnant women concomitant with AITD and 65 cases without AITD. All of the hospitalized pregnant women underwent EchoCG, had an ejection fraction EF > 50%, no heart failure, and no abnormal structural changes of the heart. The diagnosis of primary Sjögren’s syndrome in all patients met the 2012 SICCA SS classification criteria.
The following data were collected for all pregnant women with primary Sjögren’s syndrome: age, BMI, duration of Sjögren’s syndrome, parity, history of adverse pregnancy outcomes, current pregnancy outcomes (induced abortion, neonatal death, spontaneous abortion, therapeutic abortion and premature delivery), mode of pregnancy termination (vaginal delivery or cesarean section), fetal growth restriction (FGR), Fetal distress, and birth weight of newborns. The differences in maternal and neonatal outcomes between patients with and without concomitant AITD were analyzed. All methods were performed in accordance with the institution guidelines and regulations. Informed consent was obtained from all subjects and/or their legal guardian(s).
Definition of adverse pregnancy outcomes (APO)
Pregnancy loss included induced abortion, neonatal death, spontaneous abortion, and therapeutic abortion. Induced abortion was defined as the intentional termination of pregnancy for various reasons. Spontaneous abortion refers to pregnancy interruption before 20 weeks due to natural factors. Neonatal death refers to death in utero after 20 weeks of gestation. Premature delivery refers to live births before 37 weeks of gestation. Intrauterine growth restriction (IUGR) is defined as a birth weight below two standard deviations from the mean weight of fetuses of the same gestational age and gender, or below the 10th percentile for normal weight at the same gestational age. Fetal distress, often referred to by healthcare professionals as “nonreassuring fetal status,” occurs when there is concern regarding the adequacy of the baby’s oxygen supply in utero, either prior to or during labor9. It is a multifaceted condition and serves as one of the principal indicators for the need for cesarean delivery. Continuous monitoring of the fetal heart rate over a period of 20 to 40 minute typically reveals a normal baseline heart rate ranging from 120 to 160 beats per minute. A lack of significant accelerations in the fetal heart rate during periods of fetal movement, coupled with a baseline variability of less than 3 beats per minute, suggests the presence of fetal distress. In near-term pregnancies, a healthy fetal movement pattern consists of more than 20 movements within a 24-hour period. This can be assessed by instructing pregnant women to track the number of fetal movements for one hour each in the morning, afternoon, and evening, then multiplying the total by 4 to estimate movements over a 12-hour period. Diminished fetal movement is a critical indicator of fetal distress, and regular monitoring of fetal activity is essential for assessing fetal well-being. Severe neonatal APO includes preterm birth < 34 weeks (early and middle preterm) or birth weight ≤ 1500 g.
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS) software V 25.0, https://spss.en.softonic.com. Normally distributed continuous variables were presented as mean ± standard deviation (s), and independent samples t-test was used for group comparisons. Categorical data were presented as counts (n) and percentages (%). Group comparisons of continuous variables were performed using t-tests, while categorical data were analyzed using frequency or composition ratios, with chi-square tests for group comparisons. A p-value < 0.05 was considered statistically significant.
Results
Demographic data
The average age of patients with pSS and concurrent AITD was higher than that of patients without concurrent AITD, and the difference was statistically significant. Patients with pSS and concurrent AITD had a shorter duration of dryness and a higher number of new cases of pSS, and the difference was statistically significant. The mean pre-pregnancy BMI of the group with concurrent AITD was higher than that of the group without concurrent AITD, and the difference was statistically significant. Pregnant women were routinely assessed thyroid function during prenatal check-ups. In cases of hypothyroidism, pregnant women were administered levothyroxine supplementation to ensure that FT4 levels were restored to normal. The proportions of multiparous women and women with a history of adverse pregnancies were compared between the two groups and no statistically significant differences were found (P > 0.05), see Table 1 for further details.
Adverse pregnancy outcomes analysis
The rate of pregnancy loss was higher in the pSS with AITD group than in the pSS without AITD group, and the difference was statistically significant (P < 0.05). Among pSS patients with concomitant AITD, there were 11 cases (22%, 11/50) of premature deliveries and 27 cases (54%, 27/50) of term births. In the non-AITD group, there were 53 cases (81.5%, 53/65) of term births, which was significantly higher than in the AITD concomitant group, and the difference was statistically significant (P = 0.001). The rate of vaginal delivery was lower in the AITD concomitant group than in the AITD nonconcomitant group, and the difference was statistically significant (P < 0.05). Pre-eclampsia occurred in 2 (4.0%) in pSS with AITD group, 3 (4.6%) in pSS without AITD group (P = 0.873). No congenital malformations, genetic diseases and atrioventricular block abnormalities were observed in all subjects. See Table 2 for further details.
Causes for premature delivery
Preterm birth was mainly associated with several factors, including twin pregnancy, which occurred in 3 out of 11 cases (27.3%) in the pSS with AITD group and in 2 out of 7 cases (28.6%) in the pSS without AITD group. Intrauterine distress was present in 4 out of 11 cases (36.4%) in the pSS with AITD group and 3 out of 7 cases (42.9%) in the pSS without AITD group. In addition, preterm premature rupture of membranes was observed in 3 out of 11 cases (27.3%) in the pSS with AITD group and 2 out of 7 cases (28.6%) in the pSS without AITD group. Finally, placenta previa was observed in 1 out of 11 cases (9.1%) in the pSS with AITD group and none in the pSS without AITD group (Table 2).
Analysis of neonatal outcomes
The birth weight of newborns in the AITD group was lower than that of newborns in the non-AITD group, and the incidence of low birth weight was higher in the AITD group, with statistically significant differences. There were no statistically significant differences in the incidence of fetal death, neonatal live birth, intrauterine growth restriction and fetal distress between the AITD and non-AITD groups. The causes of fetal death comprised one case of severe pneumonia in the mother and one case of severe anemia in the mother. The causes of neonatal death included two cases of maternal pancytopenia, along with two cases attributed to undetermined factors. See Table 3 for more details.
Discussion
In this study, of the 50 pregnancies complicated by pSS and AITD, 12 resulted in pregnancy loss, 11 involved premature deliveries, 27 concluded with full-term births, and only 8 experienced vaginal deliveries. In contrast, among the 65 pSS pregnancies without AITD, 5 suffered pregnancy loss, 7 had premature deliveries, 53 reached full-term gestation, and 27 occurred vaginal deliveries. This revelation indicates that pregnancy complications predominantly encompassed pregnancy loss and premature delivery, occurring at respective rates of 24.0% and 22.0% in pSS with AITD pregnancies.
In the concurrent AITD group, patients with pSS display an advanced age and a higher baseline body mass index in comparison to their non-AITD counterparts. In contrast, the disease progression of pSS is abbreviated within the concurrent AITD group, accompanied by a heightened incidence of newly diagnosed cases during pregnancy. Age occupies a pivotal role in the emergence of autoimmune disorders such as AITD10, and patients in the concurrent AITD group exhibit an older demographic, contributing to a greater prevalence of AITD. Moreover, obesity serves as a risk factor for autoimmune diseases, including AITD11. The elevated BMI in the AITD group may imply a higher prevalence of obesity and, consequently, an increased risk of developing AITD. The abbreviated disease course in the concomitant AITD group can be attributed to accelerated disease progression, leading to earlier diagnosis and more frequent medical consultations. This expedited progression might arise from patients’ increased awareness of pregnancy-related autoimmune disorders and the associated detection rates12. Pregnancy-related stressors may also prompt the onset or exacerbation of AITD in certain patients13. As such, this study underscores the significance of comprehensive care and meticulous monitoring for pSS patients, particularly those with concurrent AITD.
Upon conducting an assessment of the pregnancy outcomes among two distinct groups of pregnant women with primary Sjogren’s syndrome (pSS), a significant disparity was noted in the pregnancy loss rates. The rate in the group concurrent with AITD (24%) notably exceeded that in the group without AITD (7.7%). Furthermore, the gestational weeks terminated in the concomitant AITD group were fewer in comparison to the non-AITD group. The presence of AITD instigates heightened immune reactivity against the developing fetus, thereby escalating the probability of miscarriage12. As a result, patients with concurrent AITD experience elevated rates of adverse pregnancy outcomes14. These factors can detrimentally impact a patient’s quality of life and overall health, leading to amplified stress and miscarriage. Immunosuppressive or immunomodulatory therapies, although effective, may exacerbate the risk of infection and unfavorable pregnancy outcomes, including miscarriage15. Moreover, specific genetic mutations or polymorphisms are linked with an increased risk of miscarriage and adverse pregnancy outcomes16. Collectively, these factors contribute to the discrepancy in miscarriage rates and gestational weeks of pregnancy loss between the concurrent AITD group and the non-AITD group.
Regarding the preference for childbirth mode, the proportion of vaginal deliveries was markedly decreased in the concurrent AITD group (16%) compared to the non-AITD group (41.5%). The significantly lower number of vaginal deliveries observed in patients with pSS and AITD can be attributed to several interrelated factors that have been highlighted in both domestic and international research17. Women with pSS and AITD face increased risks of gestational hypertension, preeclampsia, and placental insufficiency, potentially leading to unfavorable labor outcomes17. Such complications increase the probability of cesarean sections being recommended. Moreover, active autoimmune disease during pregnancy may intensify, causing worry about the transmission of autoantibodies between mother and fetus and presenting immunological challenges, thus potentially favoring cesarean deliveries as the safer option. AITD patients, in particular, may experience thyroid abnormalities that can further complicate pregnancy, requiring meticulous management and potentially heightening the risk of cesarean sections. Anxiety and concerns about the safety of delivery among patients with underlying autoimmune disorders can lead to a heightened preference for cesarean sections. Healthcare providers may adopt a conservative approach when managing pregnancies in patients with pSS and AITD, given the intricate interplay of risks associated with these conditions. This cautious stance often contributes to the observed trend of lower rates of vaginal deliveries. Additionally, specific clinical profiles in patients with pSS and AITD may necessitate specialized prenatal care, which can further skew delivery methods towards cesarean sections on account of individualized risk assessments.
The median birth weight of newborns in the concomitant AITD group was less than that in the non-AITD group, with a higher proportion of low-birth-weight infants amounting to 39%, in contrast to the non-AITD group’s 19.7%. There was no statistically significant disparity in the incidence of fetal distress and intrauterine growth restriction between the two groups of newborns. Consequently, it is postulated that the primary influence of AITD on infants in pSS-affected pregnant patients is exemplified by birth weight. AITD has the capacity to instigate inflammation and lesions in various organs and tissues, including the reproductive system, resulting in pregnancy complications and making natural childbirth more arduous or risky. The immune dysfunction associated with AITD disrupts the normal immune processes during pregnancy, thereby escalating the rates of miscarriage, premature birth, and low birth weight12. Owing to the augmented risk of complications, women afflicted with AITD might require medical intervention during labor, encompassing induction of labor or caesarean section. Such intervention effectively diminishes the likelihood of a natural delivery. Furthermore, women with AITD might possess pre-existing medical conditions such as uterine fibroids or pelvic floor dysfunction that influence their choice of childbirth mode, Consequently, resulting in a decreased rate of spontaneous birth. Patients with AITD could potentially harbor underlying conditions or complications that may influence fetal growth, including pre-eclampsia, gestational diabetes, or infection12,18. Although a considerable disparity in the incidence of fetal distress and restricted fetal growth was not observed between the two groups, AITD potentially contributed to these complications. Furthermore, AITD may indeed independently contribute to adverse maternal and infant outcomes. Several studies have suggested that thyroid dysfunction during pregnancy can be associated with complications such as fetal demise and low birth weight19. Although our current study did not include a separate group for AITD, our study focuses primarily on the interaction between Sjögren’s syndrome and AITD, and the combined effect of these conditions on pregnancy outcomes.
In light of these considerations, the study highlights the importance of comprehensive care and close monitoring for pregnant women with pSS associated with AITD. In conclusion, healthcare providers should be aware of the potential risks associated with AITD during pregnancy and closely monitor fetal growth to ensure timely intervention and optimal maternal and fetal outcomes. When patients with pSS become pregnant, it is recommended that the combination of thyroid autoantibodies and thyroid colour Doppler ultrasound screening be used simultaneously to determine whether AITD is present. Multidisciplinary consultations should be organized for pregnant pSS patients with concomitant AITD, and under the joint guidance of endocrinologists, obstetricians and rheumatologists, monitoring of the pregnancy should be improved, and joint efforts should be made to reduce the occurrence of adverse pregnancy outcomes and to achieve better maternal and infant outcomes. It is also important to consider the potential impact of obesity rates on our findings. Obesity is a known risk factor for pregnancy complications, including pregnancy loss and preterm birth. Therefore, differences in obesity rates between the study populations may have contributed to the observed differences in outcomes. Future studies should aim to control for obesity rates or look more closely at its effect on pregnancy outcomes.
Data availability
Data AvailabilityThe datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Jridi, M., Cherif, Y., Derbal, S., Dahmen, F. B. & Abdallah, M. Pulmonary involvement in primary Sjogren’s syndrome: contribution of the different means in the systematic investigation. Pan Afr. Med. J. 46, 42. https://doi.org/10.11604/pamj.2023.46.42.36534 (2023).
Ming, B., Zhu, Y., Zhong, J. & Dong, L. Immunopathogenesis of Sjogren’s syndrome: Current state of DAMPs. Semin. Arthritis Rheum. 56, 152062 (2022).
Conigliaro, P. et al. Autoimmune thyroid disorders and rheumatoid arthritis: A bidirectional interplay. Autoimmun. Rev. 19(6), 102529. https://doi.org/10.1016/j.autrev.2020.102529 (2020).
Yuan, N. et al. Relationship between anti-thyroid peroxidase antibody positivity and pregnancy-related and fetal outcomes in Euthyroid women: a single-center cohort study. BMC Pregnancy Childbirth 20(1), 491. https://doi.org/10.1186/s12884-020-03176-4 (2020).
Negro, R. et al. Euthyroid women with autoimmune disease undergoing assisted reproduction technologies: the role of autoimmunity and thyroid function. J. Endocrinol. Investig. 30(1), 3–8. https://doi.org/10.1007/BF03347388 (2007).
Borodina, E. et al. The pathogenic role of circulating Hashimoto’s Thyroiditis-derived TPO-positive IgG on fetal loss in naive mice. Am. J. Reprod. Immunol. 85(1), e13331. https://doi.org/10.1111/aji.13331 (2021).
Safarian, G. K. et al. Impact of antithyroperoxidase antibodies (anti-TPO) on ovarian reserve and early embryo development in assisted reproductive technology cycles. Int. J. Mol. Sci. https://doi.org/10.3390/ijms24054705 (2023).
Giron-Pillado, M. et al. Autoimmune thyroid disease in primary Sjogren’s syndrome: real-life screening practice and clinical outcomes. Curr. Rheumatol. Rev. 18(3), 272–277. https://doi.org/10.2174/1573397118666220127105546 (2022).
Yared, G. et al. Uterine sacrifice in obstetric emergencies case series: Complex cases of fetal distress, labor challenges, and life-saving interventions. SAGE Open Med. Case Rep. https://doi.org/10.1177/2050313X241261487 (2024).
van Straalen, J. W. et al. Juvenile idiopathic arthritis patients with positive family history of autoimmune thyroid disease might benefit from serological screening: analysis of the international Pharmachild registry. Pediatr. Rheumatol .Online J. 21(1), 19. https://doi.org/10.1186/s12969-023-00802-1 (2023).
Galusca, D. et al. Vitamin D implications and effect of supplementation in endocrine disorders: autoimmune thyroid disorders (Hashimoto’s disease and Grave’s disease), diabetes mellitus and obesity. Medicina (Kaunas) https://doi.org/10.3390/medicina58020194 (2022).
Bogovic Crncic, T. et al. Innate immunity in autoimmune thyroid disease during pregnancy. Int. J. Mol. Sci. https://doi.org/10.3390/ijms242015442 (2023).
Vaivode, I. et al. Stress-related immune response and selenium status in autoimmune thyroid disease patients. Int. J. Mol. Sci. https://doi.org/10.3390/ijms24032440 (2023).
Wu, D. et al. Resistance to thyroid hormone beta in autoimmune thyroid disease: a case report and review of literature. BMC Pregnancy Childbirth 18(1), 468. https://doi.org/10.1186/s12884-018-2110-9 (2018).
Nazarpour, S. et al. Effects of levothyroxine treatment on pregnancy outcomes in pregnant women with autoimmune thyroid disease. Eur. J. Endocrinol. 176(2), 253–265. https://doi.org/10.1530/EJE-16-0548 (2017).
Sun, S. et al. Identifying risk variants for embryo aneuploidy using ultra-low coverage whole-genome sequencing from preimplantation genetic testing. Am. J. Hum. Genet. 110(12), 2092–2102. https://doi.org/10.1016/j.ajhg.2023.11.002 (2023).
Amador-Patarroyo, M. J. et al. Sjogren’s syndrome at the crossroad of polyautoimmunity. J. Autoimmun. 39(3), 199–205. https://doi.org/10.1016/j.jaut.2012.05.008 (2012).
Grulet, H. et al. Three consecutive pregnancies in a patient with chronic autoimmune thyroid disease associated with hypothyroidism and extremely high levels of anti-thyrotropin receptor antibodies. Thyroid 29(5), 743–747. https://doi.org/10.1089/thy.2018.0098 (2019).
Sahu, M. T., Das, V., Mittal, S., Agarwal, A. & Sahu, M. Overt and subclinical thyroid dysfunction among Indian pregnant women and its effect on maternal and fetal outcome. Arch. Gynecol. Obstet. 281(2), 215–220. https://doi.org/10.1007/s00404-009-1105-1 (2010).
Acknowledgements
Data Availability StatementData that support the findings of this study are available from the corresponding author upon reasonable request.
Funding
This study was supported by the Medical Science and Technology Research Fund of Guangdong Province (No.A2022485), the Science and Technology Projects in Guangzhou (No. 202201020122), the Plan on enhancing scientific research in Guangzhou Medical University, Guangdong Municipal Department of Science and Technology, Municipal Schools (Institutes) Jointly Funded Project (NO.2023A03J0386, 2023A03J0395) and Guangzhou Medical University for the First-class Professional Construction Project in 2022-Enhancement of Undergraduates’ Scientific Research and Innovation Ability Project (NO.02-408-2203-2059).
Author information
Authors and Affiliations
Contributions
Yuyi Chen and Yingjun Xie carried out study design. Yanmei Dong and Yijuan Xie performed the experiments. Siqi Huang and Naifeng Liang prepared the figures, Shiyun Wen and Yaojie Zhai prepared tables. Miaoguan Peng, Taizhen Luo and Xiaoshi Weng wrote the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was obtained for this study from the Third Affiliated Hospital of Guangzhou Medical University (2024049). Informed consent was obtained from all subjects and/or their legal guardian(s).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Peng, M., Luo, T., Weng, X. et al. A retrospective analysis on maternal and neonatal outcomes in pSS/AITD pregnancies. Sci Rep 15, 3437 (2025). https://doi.org/10.1038/s41598-024-83937-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-83937-9