Abstract
This study assessed the accuracy of robotic computer-aided implant surgery (rCAIS) in partially edentulous patients using a standard operation procedure. Patients who underwent implant placement surgeries using the robotic system under a standard operation procedure were recruited. Deviations of dental implants were calculated after superimposition of the preoperative and postoperative cone-beam computed tomography (CBCT) images. The possible effects of the implant regions on these deviations were investigated. A total of 30 participants were enrolled in the study and 44 implants were inserted. The median (25th-75th percentile) global coronal deviation, global apical deviation, and angular deviation were 0.62 mm (0.46–1.00), 0.62 mm (0.49–1.01) and 1.16 (0.69–1.69) °, respectively. The jaw was a factor in the lateral coronal, vertical coronal, and vertical apical deviations (P < 0.05). Both the lateral coronal and apical deviations were greater for immediate implant placements than for delayed implant placements (P < 0.05). The implant dimensions significantly affected the apical deviation (P < 0.05). These results indicate that rCAIS based on a standard operation procedure is safe and accurate in partially edentulous patients. However, there remains a need to optimize robotic systems to simplify the workflow and improve their ability to recognize and respond to complex bone structures. Further clinical studies should also focus on comparing the long-term implant success rate and related complications of rCAIS with traditional approaches.
Similar content being viewed by others
Introduction
The position, angle, and depth of an implant in the jawbone are critical to the functional and aesthetic outcomes of the implant and its long-term success rate 1. Virtual planning allows clinicians to determine the ideal dental implant positions based on a prosthetic plan defined by superimposing available three-dimensional (3D) imaging datasets2,3. In dentistry, computer-assisted implant surgery (CAIS) is often used to reproduce the virtually planned implant position at the surgical site. CAIS is considered as a minimally invasive and accurate innovative procedure4,5,6,7. CAIS can be categorized into two types: static computer‐aided implant surgery (sCAIS) and dynamic computer‐aided implant surgery (dCAIS)8,9. sCAIS requires a surgical guide to accurately transfer the preoperatively designed implant position10, while dCIAS uses real-time tracking by an optical tracker and feedback from a computer screen about the relative positions of the drill and jaw to guide the operator to place the implant in desired position11. Several studies have demonstrated that the implant accuracy of static guides and dynamic navigation are comparable, and both are superior to freehand12,13,14,15,16. However, static guides have several disadvantages, such as the need for a certain manufacturing period and a special tool kit, insufficient water cooling, and the impossibility of changing the surgical plan intraoperatively17. In addition, static guides are often difficult to use in the posterior region due to limited mouth opening18. Dynamic navigation can avoid the aforementioned disadvantages of static guides19. Dynamic navigation is performed in a manner that is closer to freehand implant placement20, does not obstruct the vision and interfere with the entry of cooling water to the surgical area during cavity preparation19,21, and is favorable in cases where the patient has a slightly restricted mouth opening, especially in the posterior region19. However, dynamic navigation is often difficult to master, with a steep learning curve to master13,22. Further, due to the lack of physical constraints, surgeons may still deviate from the plan when drilling. Additionally, during surgery, the surgeon may focus more on the visual feedback on the screen than on the surgical site, which may result in less haptic feedback. This can lead to a discontinuous and prolonged procedure13,23. The operator is also prone to hand fatigue with this approach due to the heavy handpiece with a reference frame24,25. Therefore, human error (e.g., hand tremors, fatigue, inadequate surgical skills) cannot be avoided with both static guides or dynamic navigation26.
Robotic computer-aided implant surgery (rCAIS), an emerging computer-assisted technique in oral and maxillofacial surgery, is rapidly becoming a major hotspot in the field of dental implantology. The dental implant robot has a stable robotic arm that integrates robotics and dynamic navigation to allow for timely and efficient adjustment of the drill during implant insertion. This also avoids the influence of subjective factors, such as hand tremors and fatigue, on surgical outcomes27,28. The first commercial dental implant robot, Yomi, was approved by the Food and Drug Administration (FDA) in 2017. Subsequently, two autonomous dental implant robotic systems, Remebot and Yakebot, were authorized by China’s National Medical Products Administration in 2021. As a result, dental implant robots have been increasingly used in clinical settings29,30,31. Based on the interaction between the operator and the robotic arm, dental implant robots can be categorized as passive, semi-active, or active robots. For passive robots, the operator must hold the handpiece to enter and exit the mouth, prepare the cavity and place the implants. For semi-active robots, the robotic arm can automatically prepare the cavity and place the implants, but the operator needs to guide the robotic arm in and out of the mouth. For active robots, the robotic arm can enter and exit the mouth, prepare the osteotomy and place the implants automatically32,33. The Remebot used in this study is a semi-active robot as its robotic arm requires traction from the operator to enter and exit the oral cavity. Yakebot and Yomi are active and passive robots, respectively34. In addition to displaying the position, orientation, and depth of the drill tip in real time, Remebot’s operating system can also display the drilling force, which can help surgeons predict bone quality. However, the robotic system still lacks the ability to eliminate lateral force of the drill29.
In recent years, several studies have reported the favourable implant accuracy for dental implant robots. In addition to their application in routine dental implant surgeries, significant breakthroughs have also been made in their use for complex cases, such as immediate implant placements, zygomatic implant placements and implant placements for completely edentulous arches2,29,35,36,37,38,39. In the clinical setting, dentition defects are the most common type of missing teeth. When examining the implant accuracy of a passive robotic system in partially edentulous patients, Chen et al.27reported that the 3D coronal, 3D apical, and angular deviations were 0.53 mm, 0.53 mm, and 2.81°, respectively. In two other studies examining the accuracy of autonomous robots, the implant deviations were 0.65 mm, 0.66 mm, and 1.52°, respectively, in the study by Wang et al.40 and 0.61 mm, 0.79 mm, and 2.56°, respectively, in the study of Wu et al.41. In addition, Jia et al.42 and Zhang et al.43 compared the accuracy of dental implant robots with static guides and dynamic navigation in partially edentulous patients. The results of both studies indicated that the implant accuracy of the robot was higher. However, a recent in vitro study by Mozer et al44 found that the accuracy and precision of the robot were not as good as the static guide. This may be related to the lower level of autonomy of the robotic system used in Mozer’s study.
Nonetheless, robotic systems also have several limitations. The large-scale equipment required for robotic systems takes up space in operating rooms and can easily interfere with the work of surgeons and dental assistants45. Moreover, compared to traditional implant surgery, the introduction of a dental implant robot extends the duration of implant surgery and increases the training costs for surgeons and their assistants 45,46,47. Moreover, the complicated surgical procedure is associated with an increased risk of errors during rCAIS as a result of human error. Errors may also derive from inadequate sharpness of CBCT images48, displacement and looseness of the positioning marker 49, as well as errors related to calibration, registration, and the robotic arm itself 27. Thus, in order to improve the surgical efficiency and reduce errors in rCAIS, it is imperative to analyse and summarize the characteristics of the rCAIS procedures based on changes in the surgical methods and the surgical environment48. Different robotic systems have different principles and workflows. At present, little is known about the operation procedures of rCAIS, and to the best of our knowledge, no prior studies have explored the effect of the operation procedure on the accuracy of robotic implant surgery.
Thus, the first aim of this study was to describe the standardized and uniform operation procedure of a semi-active robot in partially edentulous patients. The second aim was to assess the implant accuracy of rCAIS and analyze the effect of the implant region, implant timeline, implant dimensions, and other factors on the accuracy of the robotic system.
Materials and methods
Study design
This study was conducted in full accordance with the World Medical Association Declaration of Helsinki and was approved by the Biomedical Research Ethics Committee of Stomatology Hospital of Fujian Medical University (Ref. [2022] NO.59). Written informed consent was obtained from all participants. Written informed consent was also obtained from all participants to publish their information and images in an online open access publication.
Patients with planned robotic implant surgery at the Affiliated Stomatological Hospital of Fujian Medical University from May 2022 to November 2022 were enrolled.
The inclusion criteria were as follows: (1) 18 to 70 years-old; (2) sufficient bone in the edentulous areas (including immediate implant placements and implant placements with simultaneous bone grafting); (3) no obvious inflammation or damage of oral soft tissue at surgical sites; (4) good oral hygiene and general health; (5) mouth opening ≥ 30 mm. The exclusion criteria were as follows: (1) pregnancy or lactating; (2) uncontrolled systemic diseases (e.g., hypertension, immunodeficiency, diabetes, and blood diseases, etc.); (3) previous intake or intravenous use of bisphosphonates; (4) sever bruxism; (5) heavy smoking (≥ 20 cigarettes per day) and alcohol abuse; (6) untreated or active periodontal disease.
In this study, the preoperative virtual planning was performed by two experts (Z.S.H. and C.J.) in the field of prosthodontics and dental implantology. The implant surgeries were performed by two implant specialists (W.D. and C.J.). The implant accuracy was measured by an engineer (W.X.Q.) of the robotic system. Statistical analysis was performed by the same experimenter (L.Y.J.).
The robotic system
The robotic system (Remebot, Baihui Weikang Technology Co., Ltd, Beijing, China) employed in the study was semi-active25. It comprised of three main parts: a robot arm with a terminal executor, an optical tracker, and an operating system15(Fig. 1).
The robotic arm was a RemeDent motion execution unit, which utilizes a UR5 robotic arm (Universal Robots Inc., Odense, Denmark) with six degrees of freedom and six-dimensional force feedback capabilities. It has a “follow-up” function (follow-up response time of 0.2 s) and can be calibrated within 100 µm of the planned implant position (repeated positioning error < 0.1 mm, angular positioning error < 0.1°), realizing the tracking and positioning of the patient’s surgical region. The robotic arm can automatically complete positioning, osteotomy preparation and drill lifting, etc. The operator controls the movement of the robotic arm and the traction of the robotic arm in and out of the patient’s mouth through a foot pedal.
The optical tracker consists of a trinocular stereo camera (MicronTracker, ClaroNav Inc., Toronto, Canada) and a camera mount. It uses ambient light recognition technology, which can recognize the black and white blocks on the positioning marker under natural lighting conditions, and collect the image data of the patient and the surrounding environment at the same time. The optical tracker captures the patient’s position in real time at a frequency of 1000 times per minute and monitors the displacement up to 0.1 mm.
The robotic surgical navigation software (RemeDent, Baihui Weikang Technology Co., Ltd, Beijing, China) includes case management, surgical planning, surgical registration, surgical navigation and surgical verification modules. In the surgical planning module, the software supports the reading, parsing and display of DICOM and STL format image data, and automatically segments out important structures such as the mandibular canal, teeth, maxillary sinus, etc., to help the surgeon quickly design the optimal implant position. In the surgical registration module, the calibration plate is attached to the handpiece, and registration and calibration can be completed automatically by moving the robotic arm in six positions around the patient’s mouth according to the system prompts. After that, the spatial relationship between the robotic arm and the optical tracker can be established by the calibration plate with the black and white blocks, which can be recognized by the optical tracker. The software then retrieves the coordinates of the radiological marker points on the positioning marker under the optical tracker and in the preoperative CBCT, and the spatial relationship between the optical tracker and the preoperative CBCT is established by coordinate transformation. The optical tracker can precisely locate the spatial position of the jawbone by tracking the positioning marker (with the radiological marker points and black and white blocks), which is fixed to the patient’s teeth. Finally, the spatial positional relationship between the patient, the optical tracker, the robotic arm and the preoperative CBCT is established. In the surgical navigation module, the deviations (position, depth and orientation) of the drill from the planned implant position in different planes as well as the forces transmitted to the robotic arm, are displayed on the screen in real time.
Preoperative imaging and virtual planning
Surgical assistants assisted surgeons in explaining the surgery protocol to patients to eliminate any fears and concerns. Subsequently, patients that agreed to place implants using the robotic system were instructed to sign the written informed consent form. The surgical assistants guided patients to take CBCT examinations with an i-CAT FLX V10 (KaVo, Germany) after a positioning marker was fixed to stable residual teeth in the corresponding jaw using a self-cured acrylic resin (3 M ESPE, Germany, Fig. 2). The scanning parameters were as follows: 120 kV, 5.0 mA, voxel size of 0.2mm3, field of view of 16 cm x 8 cm, and exposure time of 26.9 s. CBCT images were exported in standard digital imaging and communications in medicine (DICOM) formats. The voxel size of the CBCT should be no more than 0.3 mm3 according to the manufacturer of the robotic system. These were then imported to the robotic navigation software (RemeDent, Beijing, China) to design the implant positions based on the prosthetically driven principal (Fig. 2), and drilling sequences were set up according to the selected implant types. Implant types included Straumann Bone Level (Institute Straumann AG, Basel, Switzerland), NobelReplace Conical Connection (Nobel biocare service sag, Gothenburg, Sweden), NobelActive (Nobel biocare service sag, Gothenburg, Sweden), AstraTech OsseoSpeed TX (Dentsply Sirona, Gothenburg, Sweden), and Bicon (Bicon, Columbus, Ohio, America).
Surgical process of robotic system and postoperative assessment. (A), The positioning marker was fixed to the residual teeth. (B), Preoperative planning in the robotic navigation software. (C), The implant osteotomy was automatically performed by the robotic system. (D), Dental implant insertion. (E), The positioning marker was removed. (F), Postoperative assessment of the deviations between the planned and achieved implants.
rCAIS operation procedure
Preoperatively, the elected operating room was spacious enough to accommodate the robotic devices and was routinely sterilized prior to the operations. Surgical assistants then prepared all surgical instruments and positioned the robotic devices. Typically, the patient and surgical chair was located in the center of the room, the optical tracker was adjusted at about 70 mm above the patient’s head, the robotic arm moved in front of the patient, and the screen and its software control system were to the right of the patient, which enabled surgeons and surgical assistants to monitor the surgical process in real-time. Finally, the robotic system was powered up to test whether it was functional.
Intraoperatively, the surgical assistants and surgeons were careful not to cause displacement of the positioning marker when disinfecting and draping. Then, the surgical assistants cooperated with the surgeons to place a sterile plastic case and mount a sterile handpiece (DSG201L, NSK, Nakanishi Inc., Tochigi, Japan) on the robotic arm. The calibration plate was assembled into the handpiece to perform registration between the robotic arm and the optical tracker. After local anaesthesia was administered with Primacaine® (4% Articaine, 1/100,000 adrenaline, ACTEON), an incision was made by the surgeon in order to raise the full-thickness mucoperiosteal flap. The surgeon moved the robotic arm near to the patient’s mouth to prompt the robotic system to complete its calibration automatically. The surgeon and surgical assistants ensured that the optical tracker was kept immobile after registration and calibration, otherwise it would require re-registration. It is important to note that the back joint of the robotic arm did not compress the patient’s chest when the surgical robot was calibrated. Subsequently, the robotic arm would automatically prepared the osteotomy according to the preoperative plan (Fig. 2). The patient was told to maintain a stable position and keep their mouth open while the robot was preparing the osteotomy. The surgical assistants monitored the displayed site, the angle deviation, the drilling force, and the condition of the surgical area on the computer interface in real-time, adjusting the drilling parameters and steps promptly according to the surgeon’s instructions and reminding the surgeon to stop the robot if the deviation was out of range. Surgeons were tasked with dragging the robotic arm out of the mouth, changing the drill in sequence, stopping the procedure in case of intraoperative complications using a foot pedal, and deciding on alternative treatment plans based on each situation. When the drilling tip reaches the preset depth, the system will send a signal to the robotic arm to automatically stop drilling and exit the hole. After the preparation of the implant cavities, the dental implants were inserted automatically by the robotic arm or by free hand according to the insertion torque (Fig. 2). For immediate implant placement, guided bone regeneration (GBR) surgery was applied by the surgeon when the jumping gap at the implant site was > 2 mm. Finally, the surgeon closed the incision in a tension-free manner using a 4–0 absorbable suture and removed the positioning marker (Fig. 2). Psychological care was also essential throughout this process. Namely, the tensions and fears of patients were relieved through conversation or by providing stress balls. Each patient’s vital signs were also monitored during this process.
Postoperatively, surgeons or surgical assistants were required to provide detailed postoperative instructions. Patients were instructed to eat, but to avoid hot or hard food 2 h after surgery, to rinse their mouths with chlorhexidine 0.12% for 2 weeks, and take antibiotics (375 mg of cefaclor, 375 mg each time, twice a day, 0.5 g of tinidazole, 0.5 g each time, twice a day) and painkillers (60 mg of loxoprofen sodium, 60 mg each time, three times a day) for 3 days. Local intermittent ice compresses were applied to the surgical area within 48 h, and local hot compress or physical therapy was performed 48 h later. In addition, the patients needed to return to remove sutures after 10 ~ 14 days. Surgical assistants were required to clean and disinfect surfaces of the robotic system and to reposition it. Namely, the robotic arm was cleaned and disinfected twice using the alcohol wipes, and returned to its original position, and powered down. The number of use times and the status of the robotic system was recorded in detail. When cleaning the accessories in the robotic tool kit, it was necessary to completely detach each part of a tool, and to clean it under flowing water to remove any visible contamination. However, the handpiece could not be washed or soaked in water. The correct way to clean the handpiece was to connect the dental implant machine to a water pipe which washed it bidirectionally for 20 s at a time, to disinfect it with an alcohol wipe, and to inject oil for maintenance. Finally, the handpiece and other robotic accessories were placed correctly in the tool kit and sterilized together with conventional surgical instruments.
Postoperative imaging and accuracy assessment
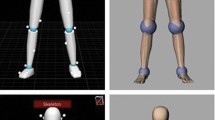
Patients were required to undergo a postoperative CBCT examination using preoperative scanning parameters. The postoperative CBCT and preoperative CBCT data were imported into the robotic surgical navigation software (RemeDent, Beijing, China), and the preoperative and postoperative CBCT were roughly aligned by selecting at least four pairs of different points on the patient’s preoperative and postoperative 3D-reconstructed dentition. They were then accurately aligned by highlighting an area of the same part of the dentition on the preoperative and postoperative CBCT. Finally, the alignment accuracy was judged by observing the colour distribution (blue indicated a good fit, with an accuracy of 0–0.1 mm). After alignment was completed, the software automatically extracted the postoperative implant contour by threshold segmentation and comparison with the implant data, and compared it to the virtually planned implant to calculate the deviations. An accuracy report was then generated (Fig. 2). As indicated in Fig. 3, the coronal (global, lateral, vertical) , apical (global, lateral, vertical), and angular deviations were measured by comparing the preoperative planned position with the achieved implant position after surgery.
Statistical analysis
The resulting data was analysed using the SPSS 29.0 software (SPSS Inc., Chicago, USA). Measurement data are presented as descriptive statistics (mean, standard deviation, median, interquartile range, minimums, maximums and 95% confidence interval). The normality of the data distributions was evaluated using the Shapiro–Wilk test and the equality of variance was checked using the Levene’s test. When analysing the effect of implant timeline, implant region and implant diameter on implant accuracy, two independent samples t-tests were used to compare differences between the variables if the distribution was normal and variances were equal. If the data was non-normally distributed, the Mann–Whitney U test was used. When analysing the effect of implant length on implant accuracy, one-way ANOVA was used if the distribution was normal and variances were equal. If the data were not normally distributed, the Kruskal–Wallis test was used. P < 0.05 indicated that the differences were statistically significant.
Sample size calculation
Sample size calculations were based on the global coronal, global apical, and angle deviations of the implant as reported in a recent in vivo study, where the means and standard deviations for the rCAIS group were 0.68 ± 0.36 mm, 0.69 ± 0.36 mm, and 1.37° ± 0.92°, respectively, while those for the dCAIS group were 1.25 ± 0.54 mm, 1.39 ± 0.52 mm, and 4.09° ± 1.79°, respectively43. Minimum sample size calculations were performed using PASS 15.0 (Power Analysis and Sample Size Software version 15.0, NCSS, LLC) for two independent mean comparisons (t-tests) with a significance level (α) of 0.05 and a power (1 − β) of 0.8. The results indicated that the minimum numbers of total samples needed for the global coronal, global apical and angular deviations were 32, 20 and 16 implants, respectively. Therefore, a sample size of 44 implants was considered sufficient to explore the performance of the robotic systems with a standard operation procedure in partially edentulous patients.
Results
All of the implant surgeries using robotic systems with a standard operation procedure were successfully completed. No complications or adverse events occurred. Table 1 shows information of patients and the distribution of implants. A total of 30 partially edentate participants (18 males, 12 females) with 44 implants were included in this study, with an average age of 45.1 (ranging from 19 to 70) years. Anterior areas were defined as the incisor to canine areas, and posterior areas were defined as the premolars to molar areas. Operation procedures were conducted in three parts: adequate preoperative preparation, intraoperative supervision and skilled handling of the robotic system, and careful postoperative care and correct disinfection of robotic accessories.
The median (25th-75th percentile) global coronal deviation, global apical deviation, and angular deviation were 0.62 mm (0.46–1.00), 0.62 mm (0.49–1.01) and 1.16 (0.69–1.69) °, respectively(Table 2). The maximum global coronal, apical and angular deviations were 2.96 mm, 3.19 mm, and 12.67°, respectively (Table 2). The jaw was a factor in the lateral coronal deviation, vertical coronal deviation and vertical apical deviation (P < 0.05), but the effect of the implant regions (anterior, posterior) on the accuracy of the robotic system was not significant(P > 0.05) (Table 3, Fig. 4). Both lateral coronal and apical deviations were greater for immediate implant placements than those for delayed implant placements (P < 0.05, Table 4, Fig. 5). Implant dimensions significantly affected the apical deviation (P < 0.05). The global apical deviation increased significantly when the implant diameter was greater than 4.5 mm and the length was greater than 10 mm (Table 5, Fig. 6, Fig. 7).
Discussion
A robotic system combines the advantages of both the real-time feedback from dynamic navigation and the physical constraints of static guides, which is an alternative to guide implant placement50. In clinical practice, a virtual plan can be directly transferred to the surgical site without the introduction of errors that result from transferring plans to a static guide and then to patients. This approach can also mitigate errors caused by the hand tremors or fatigue of surgeons, thereby maximizing the consistency, reproducibility, and reliability of the operation51. Due to the introduction of dental implant robots, the workload of surgeons and surgical assistants has been reduced. In the future, implant surgeries are likely to be completed automatically without surgeons and surgical assistants, and the role of the surgeon will change to a supervision role to ensure the safety of the operations. Nonetheless, the demand for proficient surgeons and surgical assistants will not be decreased. In addition to mastering traditional surgical knowledge and skills, surgeons and their assistants should be familiar with robotic implant surgery procedures. Therefore, in this study, a standardized and uniform operation procedure for robotic implant surgery was developed and the sources of error and influencing factors were summarized and analysed in order to improve surgical efficiency and reduce implant deviations caused by improper practice by surgeons and their assistants.
The results of this study demonstrated that all implant robotic surgeries using a standardized operation procedure were successfully completed without complications or adverse events. This indicates that the uniformity and standardization of surgical procedures were beneficial to the successful implementation of robotic implant surgery. Based on a total of 30 cases of implant robotic surgeries included in this study, several recommendations can be made. Firstly, it is necessary to communicate with patients preoperatively to obtain their consent for the use of robotic systems and to alleviate their worries and concerns. This is particularly important in surgeries relying on robotics. Secondly, surgical assistants should also master the use of navigation software and make prompt surgical step adjustments to improve surgical efficiency. Finally, it is necessary for surgeons and surgical assistants to be capable of dealing with the common malfunctions of robotic systems. Other protocols like freehand implantation, sCAIS, or dCAIS can be used as an alternative if the robot malfunctions. If the latter occurs, the causes and solutions should be documented in detail. Regular inspection and maintenance of the robotic system may reduce the likelihood of intraoperative malfunctions.
The implant position and angle deviation results of the current study were in line with previous clinical studies2,27,35,42. Yang et al. 35 used the same robotic system and they reported coronal, apical, and angular deviations of 0.74 mm, 0.73 mm, and 1.11◦, respectively. A study by Chen et al.27 reported that the implant deviations of a semi-active robotic system in the entry point, exit point, and angle were 0.53 mm, 0.53 mm, and 2.81°, respectively. A case series by Qiao et al.46 reported that the implant deviations of a semi-active robotic system were 0.54 mm, 0.54 mm, and 0.79°, respectively. A retrospective study using an active robotic system reported 0.43 mm , 0.56 mm, and 1.48° for coronal, apical, and angular deviations42. Bolding et al. 2 reported deviations of 1.04 mm, 0.95 mm and 2.56°for Yomi, a passive robotic system. Another study using a passive robotic system reported deviations of 1.23 mm, 1.40 mm and 3.0°47. Based on these findings, active and semi-active robotic systems seem to be more accurate than passive robots, but further clinical studies are required to validate these findings. The results of the current study are also similar to two recent systematic reviews and meta-analyses on robotic implant accuracy. The systematic review and meta-analysis by Yang et al.33 showed that the average global coronal, global apical, and angular deviations of rCAIS in the clinical studies were 0.6 mm, 0.7 mm, and 1.6°, respectively. The systematic review and meta-analysis by Wu et al. 52 reported that the platform, apex, and angular deviations were 0.68 mm, 0.67 mm, and 1.69°, respectively. The robotic implant deviations reported in this study were also lower than those of dynamic navigation and static guides, especially in terms of angular deviation. Recent systematic reviews have reported that the linear and angular deviations of both static guides53,54,55 and dynamic navigation56,57,58 were more than 1 mm and 3°, respectively. This may be due to the use of high-quality CBCT data in this study, which reduces systematic errors in the registration and calibration of the robotic system. The use of robotic systems also avoids errors associated with the fabrication and placement of guides, as well as human errors due to fatigue and hand tremors40.
However, large incidental errors in this study cannot be ignored. The most likely reasons for these are as follows. Firstly, the undiscovered loosening of a positioning marker may significantly affect the accuracy of the robotic system. The fixed marker may become loose when subjected to force. The loosening of the marker affects the accurate positioning of the handpiece and drill, resulting in the accumulating of errors 59. Therefore, it is recommended that the marker is fixed to the teeth with a concave and self-curing resin is used to fill the gap between teeth and the slot. Next, a large deviation can occur if the patient suddenly moves or closes their mouths, and the robotic arm is not adjusted accordingly 27,60. Lastly, similar to freehand surgery, there is a risk of the drill side-slipping with rCAIS, especially when placing an implant on an uneven bone surface such as during immediate implant placements 35,46,47. In the present study, we observed an extremely high angular deviation value. This occurred in a case of immediate implant placement in the posterior mandible. There were several reasons for this high angular deviation. First, the patient had an insufficient mouth opening. In this patient, we initially planned to place a Straumann implant, but due to the patient’s limited mouth opening and the very far posterior implant site (37, Federation Dentaire International system, FDI), the drills of the Straumann system were too long. Thus, the robotic arm was unable to enter the patient’s mouth to prepare the cavity after several attempts. Therefore, we changed the surgical plan to the Nobel PMC implant system, which has different lengths of drills in the tool kit. We chose the shortest drills (28 mm) for implant bed preparation. The second reason was due to manual implant placement. After the osteotomy preparation was completed, it was difficult to place the implant with the robotic arm due to the inadequate mouth opening of the patient, as the implant increased in length when it was attached to a carrier. Therefore, we ended up placing the implant free-hand. Third, side-slip of the drill may have also contributed to some errors. The bone in the posterior fresh extraction socket was asymmetric, which can easily lead to side slipping of the drill. Thus, this case also had a large lateral coronal and apical deviations of 1.03 mm and 2.72 mm, respectively. Fourth, bone grafting may also result in a slight inclination of the implant angle. Given that the extraction socket was large, most of the implant was exposed in the socket after placement, and the implant was only retained by a small amount of alveolar bone at the apex. This caused the implant to tilt in a certain direction due to the extrusion of the bone graft and filling instruments during bone grafting. For global coronal deviation, we observed a maximum value of 2.96 mm. This occurred in a patient with an implant site of 46 (FDI). The deviation was mainly due to an inaccurate placement depth. Because the bone quality of the mandible was dense, the implant could not be inserted in place due to the high torque. The implant was ultimately placed manually, resulting in the actual implant position being more coronal than the planned position, with a vertical deviation of -2.95 mm. In addition, the maximum global apical deviation of 3.19 mm occurred in another patient with an implant site of 17 (FDI). Because the occlusal space was insufficient in the posterior area in this case, the robot was unable to perform drilling after positioning the site. Ultimately, the surgeon switched to freehand osteotomy preparation and implantation. This resulted in the actual implant position being more buccal than the planned position, with a lateral apical deviation of 3.18 mm. The above special scenarios demonstrate that the application of the robotic system in the posterior region is still limited. The following two factors should be considered when utilizing an implant robot in the posterior region in the clinical setting. The first is the patient’s mouth opening. A limited mouth opening will result in insufficient working space in the posterior region, and the robotic arm may not be able to drill and place the implant. Accordingly, the flexibility of these robots requires improvement3,26. The second factor is the bone structure. Both dense bone quality and uneven bone morphology can contribute to the error. As the tactile perception of the robot is still not as sensitive as the “hand feel” of a surgeon with multiple years of implant experience, if the robotic arm does not sufficiently lift during drilling when encountering dense bone, bone burns may occur, or the implant cannot be inserted. The tactile sensation and temperature sensation functions are also issues that require urgent improvement for dental implant robots26. Accordingly, a sufficient safety zone should be provided when using a robotic system to place implants.
Several researchers have reported that the apical deviations of static guides and dynamic navigation are higher than the coronal deviations53,57,61. However, the global coronal and global apical deviations were identical in our study. As there was no fulcrum in the tool path under the guidance of the robotic system, amplification of apical deviations was not observed in the present study2. Moreover, the possible correlations between the implant regions (maxilla, mandible, anterior, posterior) and deviations of the implant position were investigated. The results were similar to the studies of Jia et al.42 and Chen et al.27, which showed no significant differences in the 3D platform, apex, and axial deviations. However, when comparing the implant accuracy in the maxilla and mandible, we found that the lateral coronal deviation in the maxilla was statistically larger than that in the mandible, this is because the maxilla is susceptible to interferences from the buccal muscle and adjacent teeth, especially if the mouth opening is limited27. Moreover, the vertical coronal and apical deviations in the maxilla were statistically smaller than those in the mandible. This may be because the bone density in the mandible is denser and therefore it is difficult to insert implants here due to excessive torque, resulting in a larger vertical deviation2. When comparing the implant accuracy between immediate and delayed implant placement, the results showed that both the lateral coronal and apical deviations of immediate implant placement were greater than those of delayed implant placement. This may be because the bone surface of the fresh extraction socket was uneven and the drill tended to slide along the bone surface, especially when it encountered the hard palatal bone wall in the anterior region. This would have resulted in greater lateral deviation7,38. However, the sample size for immediate implant placements in this study was insufficient to make firm conclusions.
The effect of the implant dimensions on implant accuracy was also analysed in this study. The results showed that the length and diameter of the implant significantly affected the apical deviation. The global apical deviation of implants with diameters of 4.0–4.5 mm was significantly smaller than those with a diameter above 4.5 mm. An in vitro study by Thu Linn et al.62 also reported that the apical deviation of implants with a diameter of 5 mm was significantly greater than that of implants with a diameter of 3.5 mm. Moreover, similar to the present study, another study found that the implant length was also a contributing factor in apical deviations42. This indicates that the performance of the dental implant robot in the preparation of wider and deeper implant cavities still needs to be improved. However, a study by Chen et al.27 reported no statistically significant difference between implants of different dimensions. Therefore, more clinical studies with large sample sizes are needed to clarify the effect of the implant dimensions on implant accuracy.
The present study also has several limitations that should be noted. First, the sample size in this study was limited. In particular, there was an insufficient number of cases of immediate implantation which may have impacted the results. Therefore, the results of this study should be interpreted with caution. The accuracy of dental implant robots applied in complex clinical scenarios requires further exploration in large-sized samples. Second, this study was a retrospective, exploratory study without a comparison group. More controlled clinical studies are needed to verify the influence of the operator’s experience and proficiency in the surgical procedure on the safety, accuracy, and surgical duration of robotic surgery. In addition, the implant accuracy, surgical duration, long-term implant success, and related complications of implant robots should be compared with freehand, static guides, and dynamic navigation. Third, in accordance with the inclusion and exclusion criteria, we objectively assessed the patients’ local bone volume and general health. However, there was a lack of criteria for assessing the patients’ status of psychological preparation and anxiety. The patient’s psychological condition and cooperation can also have an impact on the outcome. In the future, the popularization of dental implant robots should be strengthened to eliminate patients’ prejudices. Further, a standardized scale should be used to assess patient anxiety before surgery to reduce human errors. Finally, the patients involved in this study were all partially edentulous, and therefore, a well-established, uniform robotic implant surgical procedure for completely edentulous patients still requires future development.
Conclusion
These results indicate that rCAIS based on a standard operation procedure is safe and accurate in partially edentulous patients. However, there remains a need to optimize robotic systems to simplify the workflow and improve their ability to recognize and respond to complex bone structures. Further clinical studies should also focus on comparing the long-term implant success rate and related complications of rCAIS with traditional approaches.
Data availability
Data is available on request from the authors.
References
Sun, T. M., Lee, H. E. & Lan, T. H. The influence of dental experience on a dental implant navigation system. BMC Oral Health 19, 222. https://doi.org/10.1186/s12903-019-0914-2 (2019).
Bolding, S. L. & Reebye, U. N. Accuracy of haptic robotic guidance of dental implant surgery for completely edentulous arches. J. Prosthet. Dent. 128, 639–647. https://doi.org/10.1016/j.prosdent.2020.12.048 (2022).
Khaohoen, A. et al. Accuracy of implant placement with computer-aided static, dynamic, and robot-assisted surgery: a systematic review and meta-analysis of clinical trials. BMC Oral Health 24, 359. https://doi.org/10.1186/s12903-024-04033-y (2024).
Chen, Y. W. et al. Computer-assisted surgery in medical and dental applications. Expert Rev. Med. Devices 18, 669–696. https://doi.org/10.1080/17434440.2021.1886075 (2021).
Bi, X. Q. & Zhao, F. R. [Application of artificial intelligence in stomatology treatment and nursing]. Hua xi kou qiang yi xue za zhi = Huaxi kouqiang yixue zazhi = West China journal of stomatology 36, 452–456, https://doi.org/10.7518/hxkq.2018.04.018 (2018).
Jia, S., Wang, G., Zhao, Y. & Wang, X. Autonomous robotic system for the assisted immediate placement of a maxillary anterior implant: A clinical report. J. Prosthet. Dent. https://doi.org/10.1016/j.prosdent.2024.02.030 (2024).
Chen, J. et al. Accuracy of immediate dental implant placement with task-autonomous robotic system and navigation system: An in vitro study. Clin. Oral Implant Res. https://doi.org/10.1111/clr.14104 (2023).
Chackartchi, T., Romanos, G. E., Parkanyi, L., Schwarz, F. & Sculean, A. Reducing errors in guided implant surgery to optimize treatment outcomes. Periodontology 2000(88), 64–72. https://doi.org/10.1111/prd.12411 (2022).
Sarhan, M. M., Ibrahim, E. A., Ezzelarab, S. & Marei, M. K. Navigating the future of guided dental implantology: A scoping review. The international journal of medical robotics + Computer Assisted Surgery. MRCAS 20, e2627, https://doi.org/10.1002/rcs.2627 (2024).
Bover-Ramos, F., Viña-Almunia, J., Cervera-Ballester, J., Peñarrocha-Diago, M. & García-Mira, B. Accuracy of Implant Placement with Computer-Guided Surgery: A Systematic Review and Meta-Analysis Comparing Cadaver, Clinical, and In Vitro Studies. Int. J. Oral Maxillofacial Implants 33, 101–115. https://doi.org/10.11607/jomi.5556 (2018).
Pomares-Puig, C., Sánchez-Garcés, M. A. & Jorba-García, A. Dynamic and static computer assisted implant surgery for completely edentulous patients. A proof of a concept. J. Dentistry https://doi.org/10.1016/j.jdent.2023.104443 (2023).
Yotpibulwong, T. et al. Accuracy of implant placement with a combined use of static and dynamic computer-assisted implant surgery in single tooth space: A randomized controlled trial. Clin. Oral Implants Res. 34, 330–341. https://doi.org/10.1111/clr.14043 (2023).
Block, M. S., Emery, R. W., Lank, K. & Ryan, J. Implant Placement Accuracy Using Dynamic Navigation. Int. J. Oral Maxillofacial Implants 32, 92–99. https://doi.org/10.11607/jomi.5004 (2017).
Wu, D. et al. Accuracy of dynamic navigation compared to static surgical guide for dental implant placement. Int. J. Implant Dentistry 6, 78. https://doi.org/10.1186/s40729-020-00272-0 (2020).
Feng, Y., Su, Z., Mo, A. & Yang, X. Comparison of the accuracy of immediate implant placement using static and dynamic computer-assisted implant system in the esthetic zone of the maxilla: a prospective study. Int. J. Implant Dentistry 8, 65. https://doi.org/10.1186/s40729-022-00464-w (2022).
Yimarj, P. et al. Comparison of the accuracy of implant position for two-implants supported fixed dental prosthesis using static and dynamic computer-assisted implant surgery: A randomized controlled clinical trial. Clin. Implant Dentistry Related Res. 22, 672–678. https://doi.org/10.1111/cid.12949 (2020).
Moon, S. Y., Lee, K. R., Kim, S. G. & Son, M. K. Clinical problems of computer-guided implant surgery. Maxillofacial Plastic Reconstruct. Surgery 38, 15. https://doi.org/10.1186/s40902-016-0063-3 (2016).
Block, M. S. & Emery, R. W. Static or Dynamic Navigation for Implant Placement-Choosing the Method of Guidance. J. Oral Maxillofacial Surg. 74, 269–277. https://doi.org/10.1016/j.joms.2015.09.022 (2016).
Wang, J., Ge, Y., Mühlemann, S., Pan, S. & Jung, R. E. The accuracy of dynamic computer assisted implant surgery in fully edentulous jaws: A retrospective case series. Clinical oral implants research 34, 1278–1288. https://doi.org/10.1111/clr.14168 (2023).
Jaemsuwan, S. et al. Comparison of the accuracy of implant position among freehand implant placement, static and dynamic computer-assisted implant surgery in fully edentulous patients: a non-randomized prospective study. Int. J. Oral Maxillofacial Surg. 52, 264–271. https://doi.org/10.1016/j.ijom.2022.05.009 (2023).
Pozzi, A., Hansson, L., Carosi, P. & Arcuri, L. Dynamic navigation guided surgery and prosthetics for immediate loading of complete-arch restoration. Journal of esthetic and restorative dentistry : official publication of the American Academy of Esthetic Dentistry, [et al.] 33, 224–236, https://doi.org/10.1111/jerd.12710 (2021).
Somogyi-Ganss, E., Holmes, H. I. & Jokstad, A. Accuracy of a novel prototype dynamic computer-assisted surgery system. Clin. Oral Implants Res. 26, 882–890. https://doi.org/10.1111/clr.12414 (2015).
Kivovics, M., Takács, A., Pénzes, D., Németh, O. & Mijiritsky, E. Accuracy of dental implant placement using augmented reality-based navigation, static computer assisted implant surgery, and the free-hand method: An in vitro study. J. Dentistry https://doi.org/10.1016/j.jdent.2022.104070 (2022).
Spille, J. et al. Learning Curve and Comparison of Dynamic Implant Placement Accuracy Using a Navigation System in Young Professionals. Dentistry J. https://doi.org/10.3390/dj10100187 (2022).
Casap, N., Nadel, S., Tarazi, E. & Weiss, E. I. Evaluation of a navigation system for dental implantation as a tool to train novice dental practitioners. J. Oral Maxillofacial Surg. 69, 2548–2556. https://doi.org/10.1016/j.joms.2011.04.026 (2011).
Liu, C. et al. The evolution of robotics: research and application progress of dental implant robotic systems. Int. J. Oral Sci. 16, 28. https://doi.org/10.1038/s41368-024-00296-x (2024).
Chen, W. et al. Accuracy of dental implant placement with a robotic system in partially edentulous patients: A prospective, single-arm clinical trial. Clin. Oral Implants Res. 34, 707–718. https://doi.org/10.1111/clr.14083 (2023).
Sin, M. et al. Development of a Real-Time 6-DOF Motion-Tracking System for Robotic Computer-Assisted Implant Surgery. Sensors (Basel, Switzerland), https://doi.org/10.3390/s23052450 (2023).
Li, C. et al. Autonomous robotic surgery for zygomatic implant placement and immediately loaded implant-supported full-arch prosthesis: a preliminary research. Int. J. Implant Dentistry 9, 12. https://doi.org/10.1186/s40729-023-00474-2 (2023).
Wu, Y., Wang, F., Fan, S. & Chow, J. K. Robotics in Dental Implantology. Oral Maxillofacial Surg. Clin. North Am. 31, 513–518. https://doi.org/10.1016/j.coms.2019.03.013 (2019).
Liu, L., Watanabe, M. & Ichikawa, T. Robotics in Dentistry: A Narrative Review. Dentistry J. https://doi.org/10.3390/dj11030062 (2023).
Xu, Z. et al. Accuracy and efficiency of robotic dental implant surgery with different human-robot interactions: An in vitro study. J. Dentistry https://doi.org/10.1016/j.jdent.2023.104642 (2023).
Yang, J. & Li, H. Accuracy assessment of robot-assisted implant surgery in dentistry: A systematic review and meta-analysis. J. Prosthetic Dent. 132(747), e741-747.e715. https://doi.org/10.1016/j.prosdent.2023.12.003 (2024).
Zhou, W. K. et al. Clinical and in vitro application of robotic computer-assisted implant surgery: a scoping review. Int. J. Oral Maxillofacial Surg. https://doi.org/10.1016/j.ijom.2024.09.006 (2024).
Yang, S. et al. Accuracy of autonomous robotic surgery for single-tooth implant placement: A case series. J. Dentistry https://doi.org/10.1016/j.jdent.2023.104451 (2023).
Cao, Z. et al. Pilot study of a surgical robot system for zygomatic implant placement. Med. Eng. Physics 75, 72–78. https://doi.org/10.1016/j.medengphy.2019.07.020 (2020).
Deng, H. et al. Semi-autonomous two-stage dental robotic technique for zygomatic implants: An in vitro study. J. Dentistry https://doi.org/10.1016/j.jdent.2023.104687 (2023).
Zhao, N. et al. Accuracy analysis of robotic-assisted immediate implant placement: A retrospective case series. J. Dentistry https://doi.org/10.1016/j.jdent.2024.105035 (2024).
Li, J. et al. Accuracy of immediate anterior implantation using static and robotic computer-assisted implant surgery: A retrospective study. J. Dentistry https://doi.org/10.1016/j.jdent.2024.105218 (2024).
Wang, M. et al. Accuracy of an autonomous dental implant robotic system in partial edentulism: A pilot clinical study. Clin. Oral Investig. 28, 385. https://doi.org/10.1007/s00784-024-05780-6 (2024).
Wu, Y., Zou, S., Lv, P. & Wang, X. Accuracy of an autonomous dental implant robotic system in dental implant surgery. J. Prosthetic Dentistry https://doi.org/10.1016/j.prosdent.2024.07.020 (2024).
Jia, S., Wang, G., Zhao, Y. & Wang, X. Accuracy of an autonomous dental implant robotic system versus static guide-assisted implant surgery: A retrospective clinical study. J. Prosthetic Dentistry https://doi.org/10.1016/j.prosdent.2023.04.027 (2023).
Zhang, S. et al. Accuracy of implant placement via dynamic navigation and autonomous robotic computer-assisted implant surgery methods: A retrospective study. Clin. Oral Implants Res. 35, 220–229. https://doi.org/10.1111/clr.14216 (2024).
Mozer, P. S. & Guentsch, A. An in vitro analysis of the accuracy of static and robot-assisted implant surgery. Clinical Oral Implants Res. 35, 487–497. https://doi.org/10.1111/clr.14233 (2024).
Li, Z., Xie, R., Bai, S. & Zhao, Y. Implant placement with an autonomous dental implant robot: A clinical report. J. Prosthetic Dentistry https://doi.org/10.1016/j.prosdent.2023.02.014 (2023).
Qiao, S. C., Wu, X. Y., Shi, J. Y., Tonetti, M. S. & Lai, H. C. Accuracy and safety of a haptic operated and machine vision controlled collaborative robot for dental implant placement: A translational study. Clin. Oral Implants Res. 34, 839–849. https://doi.org/10.1111/clr.14112 (2023).
Shi, J. Y. et al. Improved positional accuracy of dental implant placement using a haptic and machine-vision-controlled collaborative surgery robot: A pilot randomized controlled trial. J. Clin. Periodontol. 51, 24–32. https://doi.org/10.1111/jcpe.13893 (2024).
Tao, B. et al. The accuracy of a novel image-guided hybrid robotic system for dental implant placement: An in vitro study. The international journal of medical robotics + computer assisted surgery, MRCAS 19, e2452, https://doi.org/10.1002/rcs.2452 (2023).
Zhao, Y. et al. Effect of the number and distribution of fiducial markers on the accuracy of robot-guided implant surgery in edentulous mandibular arches: An in vitro study. J. Dentistry https://doi.org/10.1016/j.jdent.2023.104529 (2023).
Rawal, S., Tillery, D. E., Jr. & Brewer, P. Robotic-Assisted Prosthetically Driven Planning and Immediate Placement of a Dental Implant. Compendium of continuing education in dentistry (Jamesburg, N.J. : 1995) 41, 26–30; quiz 31 (2020).
Sun, X. et al. Automated dental implantation using image-guided robotics: registration results. Int. J. Computer Assisted Radiol. Surg. 6, 627–634. https://doi.org/10.1007/s11548-010-0543-3 (2011).
Wu, X. Y., Shi, J. Y., Qiao, S. C., Tonetti, M. S. & Lai, H. C. Accuracy of robotic surgery for dental implant placement: A systematic review and meta-analysis. Clin. Oral Implants Res. 35, 598–608. https://doi.org/10.1111/clr.14255 (2024).
Tahmaseb, A., Wu, V., Wismeijer, D., Coucke, W. & Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implants Res. 29(Suppl 16), 416–435. https://doi.org/10.1111/clr.13346 (2018).
Eftekhar Ashtiani, R., Ghasemi, Z., Nami, M., Mighani, F. & Namdari, M. Accuracy of static digital surgical guides for dental implants based on the guide system: A systematic review. J. Stomatol. Oral Maxillofac. Surg. 122, 600–607. https://doi.org/10.1016/j.jormas.2020.10.010 (2021).
Aghaloo, T., Hadaya, D., Schoenbaum, T. R., Pratt, L. & Favagehi, M. Guided and Navigation Implant Surgery: A Systematic Review. Int. J. Oral Maxillofacial Implants 38, 7–15. https://doi.org/10.11607/jomi.10465 (2023).
Yu, X., Tao, B., Wang, F. & Wu, Y. Accuracy assessment of dynamic navigation during implant placement: A systematic review and meta-analysis of clinical studies in the last 10 years. J. Dent. https://doi.org/10.1016/j.jdent.2023.104567 (2023).
Wei, S. M. et al. Accuracy of dynamic navigation in implant surgery: A systematic review and meta-analysis. Clin. Oral Implants Res. 32, 383–393. https://doi.org/10.1111/clr.13719 (2021).
Jorba-García, A., González-Barnadas, A., Camps-Font, O., Figueiredo, R. & Valmaseda-Castellón, E. Accuracy assessment of dynamic computer-aided implant placement: a systematic review and meta-analysis. Clin. Oral Investig. 25, 2479–2494. https://doi.org/10.1007/s00784-021-03833-8 (2021).
Tao, B. et al. Accuracy of dental implant surgery using dynamic navigation and robotic systems: An in vitro study. J. Dent. https://doi.org/10.1016/j.jdent.2022.104170 (2022).
Cheng, K. J. et al. Accuracy of dental implant surgery with robotic position feedback and registration algorithm: An in-vitro study. Comput. Biol. Med. https://doi.org/10.1016/j.compbiomed.2020.104153 (2021).
D’Haese, J., Van De Velde, T., Elaut, L. & De Bruyn, H. A prospective study on the accuracy of mucosally supported stereolithographic surgical guides in fully edentulous maxillae. Clin. Implant Den. Related Res. 14, 293–303. https://doi.org/10.1111/j.1708-8208.2009.00255.x (2012).
Linn, T. Y. et al. Accuracy of implant site preparation in robotic navigated dental implant surgery. Clin. Implant Den. Related Res. 25, 881–891. https://doi.org/10.1111/cid.13224 (2023).
Acknowledgements
The authors would like to express their gratitude to the excellent technical assistance of Xiongqian Wang from Beijing Baihui Weikang Technology Co., Ltd.
Funding
This work was sponsored by Fujian provincial health technology project (2022GGA040) and Startup Fund for scientific research, Fujian Medical University (Grant No. 2023QH2017). Program of Undergraduate Education and Teaching, Fujian Medical University (Project No: J24013).
Author information
Authors and Affiliations
Contributions
Yitian Liu: Writing—Original Draft, Writing—Review & Editing, Validation, Formal analysis. Qingqing Zheng: Writing—Original Draft, Methodology, Investigation, Date curation. Zonghe Xu: Funding acquisition, Investigation, Date curation. Yanjun Lin: Validation, Formal analysis. Sihui Zhang: Funding acquisition. Dong Wu: Conceptualization, Supervision, Resources, Writing—Review & Editing. Wenxiu Huang: Methodology. Jiang Chen: Resources, Supervision. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was conducted in full accordance with the World Medical Association Declaration of Helsinki and was approved by the Biomedical Research Ethics Committee of Stomatology Hospital of Fujian Medical University (Ref. [2022] NO.59). Written informed consent was obtained from all participants.
Consent to publication
Written informed consent was obtained from all participants to publish their information and images in an online open access publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Y., Zheng, Q., Xu, Z. et al. Accuracy and operation procedure of robotic computer-aided implant surgery. Sci Rep 15, 307 (2025). https://doi.org/10.1038/s41598-024-83997-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-83997-x