Abstract
This study aimed to investigate the change of peri-implant bone mass after touch-controlled, minimally invasive implantation in the mandibular first molar region by cone-beam computed tomography (CBCT). A retrospective study was conducted, involving 60 implants in the mandibular first molar region. Touch-controlled, minimally invasive implantation was performed, and healing abutments were installed after surgery. CBCT scans were obtained at four time points: on the day of surgery (T0) and at 1 month (T1) and 6 months (T2) after surgery. Implant retention, as well as horizontal and vertical bone absorption, both bucco-lingually and in the proximal and distal regions, was measured at each time point. The implant retention at T2 was 100%. Bone resorption was observed at the proximal and distal sites of the implant as early as at T1, with more noticeable resorption at T2. Compared with T1, there was a significant increase in bone resorption, and the resorption amount tended to stabilize by T2. Horizontal bone resorption was not evident. Briefly, following touch-controlled, minimally invasive implantation of mandibular first molars, peri-implant vertical bone resorption was observed in the proximal, distal, and bucco-lingual regions, while horizontal bone resorption was not apparent. These findings provide valuable guidance for implant clinicians in selecting optimal surgical techniques.
Similar content being viewed by others
Introduction
Bone integration, which is also known as osseointegration, plays a pivotal role in the long-term success of oral implants. Once successful osseointegration occurs and the implant is subjected to occlusal forces, bone remodeling typically takes place. Within the first year after implant placement, the marginal bone undergoes horizontal and vertical changes due to functional loading. Moreover, various clinical procedures, implant accessories, and patient-related factors can contribute to implant failure or marginal bone loss1. To deem the implant treatment successful, it is imperative that a peri-implant bone loss of less than 2 mm is observed within the first year, and less than 0.2 mm is observed in subsequent years2.
In practice, tooth extraction results in substantial alveolar bone loss. This bone loss encompasses both horizontal dimensions on the bucco-lingual side, as well as a reduction in alveolar bone height3,4. Within the initial 3 months following tooth extraction, the buccal bone experiences 20–30% absorption3. Immediate implantation can mitigate alveolar bone resorption but it also heightens the risk of implant failure. Conversely, delayed implantation reduces the likelihood of implant failure, as it allows ample time for alveolar bone remodeling5. The stability of a molar area implant predominantly relies on the specific implant site and the quality and quantity of the available bone.
The loss of a mandibular first molar is a prevalent oral disease. The utilization of minimally invasive dental implant technology has emerged as a rapidly advancing trend in oral medical technology6,7,8,9. Compared with conventional dental implant surgery, minimally invasive dental implants present several advantages over peri-implant soft and hard tissues. This technique minimizes surgical trauma, diminishes duration of operation, and mitigates postoperative alveolar bone resorption around the implant. Simultaneously, it mitigates the risk of infection, alleviates patient discomfort, and reduces postsurgical edema, rendering it more favorable and acceptable to patients6,7,8,9,10. Furthermore, minimally invasive dental implants can effectively diminish, reduce, or prevent the occurrence of intraoperative patient complications, thereby extending the applicability of this technology in implant surgery.
Prior to performing minimally invasive implantation, cone-beam computed tomography (CBCT) should be utilized to acquire imaging data for the assessment and documentation of alveolar ridge bone condition, patient bone mass and bone density, and other relevant factors; this ensures optimal implantation8. The modified technique for minimally invasive implantation involves employing a precise circular incision, thereby enhancing the visibility of the alveolar bone surface. This improvement aids in achieving a better seal around the implant’s neck and promotes the formation of the implant cuff, thereby facilitating early postoperative healing. Moreover, this technique creates favorable conditions for subsequent denture fixation11. Overall, the use of minimally invasive dental implants has generally exhibited favorable clinical outcomes in the restoration of mandibular first molar loss, significantly enhancing the treatment experience for patients12.
However, after implantation, marginal bone resorption ensues around the implant; this is a crucial determinant of long-term implant stability. The longevity of implant-supported dentures becomes jeopardized owing to bone resorption occurring at the periphery of the implant13. Within the initial year subsequent to implant placement, the adjacent bone tissue may experience an approximate loss of 1.5 mm, and bone loss during the non-loading phase exhibits a significant correlation with the efficacy of implant restoration14.
As a crucial diagnostic tool, CBCT is employed for guiding implant choice and assessing bone density prior to implant surgery. Moreover, it allows for the observation of bone integration and implant-related bone resorption during and after surgery, while also facilitating the evaluation of the implant’s proximity to vital anatomical structures within the surrounding region8,15,16,17. Consequently, CBCT has evolved into an indispensable imaging modality in the field of oral implantology.
Currently, there is a lack of definitive data elucidating peri-implant bone resorption following the minimally invasive implantation of mandibular first molar implants in the presence of a healing abutment. In light of this, the objective of this investigation was to employ CBCT to quantify the alterations in bone density surrounding the implant following touch-controlled, minimally invasive implantation of the mandibular first molar, coupled with the placement of a healing abutment postoperatively. The results of this study will assist clinicians in making more accurate determinations regarding surgical method and in enhancing the efficacy of implant restoration.
Materials and methods
Research design
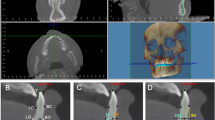
In this retrospective study conducted at the Affiliated Hospital of Chifeng University in Inner Mongolia, China, from June 2022 to December 2023, we examined 54 patients who had undergone a touch-controlled, minimally invasive implantation procedure for mandibular first molars. Postoperatively, healing abutments were installed to facilitate recovery. The bone density surrounding the implants was meticulously assessed both vertically and horizontally on the day of surgery, as well as at 1, and 6 months after the procedure, to monitor the changes in bone mass around the implant site. An accomplished dental implant specialist meticulously documented the indicators of peri-implant bone loss throughout the study. A detailed diagram of the study design is provided in Fig. 1.
Study population
The inclusion criteria were as follows: (1) age ≥ 18 years; (2) implants placed using touch-controlled, minimally invasive non-flap surgery for mandibular first molar replacement, without significant bone defects, and with a healing abutment installed postoperatively; (3) no significant peri-implant inflammation observed after implantation; (4) the presence of healthy adjacent teeth; and (5) CBCT scans obtained at our hospital before surgery, immediately after surgery, and at 1, and 6 months postoperatively. The exclusion criteria were as follows: (1) Adjacent teeth at the implant site have deformities. (2) moderate-to-severe periodontitis or progressive periodontitis; (3) heavy smoking (≥ 10 cigarettes per day); and (4) oral mucosal fibrosis.All subjects and/or their legal guardians have signed informed consent statements.
Materials and equipment
Datsing planting system produced by Beijing Daqing Biological Co., Ltd. CBCT (Newtom VGi made in Italy), the measurement tool is the CBCT software NNT (Version 9.0, QR, Italy).
Research method
CBCT scanning
Seat projection was employed during the acquisition of CBCT in all subjects undergoing implant procedures. The scanning parameters were as follows: X-ray tube voltage of 110 kV; tube current of 20 mA; focus size of 0.5 × 0.5 mm; pulse exposure; and an effective exposure time of 6 s. Subsequently, axial, sagittal, and coronal images of the alveolar bone in the edentulous region of the mandibular first molar were reconstructed from the acquired scanning data. Notably, each image acquisition is performed by the same radiologist in accordance with uniform standards.
Time observation point and data measurement
Observation time points were the day after surgery (T0), 1 month after surgery (T1),and 6 months after surgery (T3).
Measurement methods
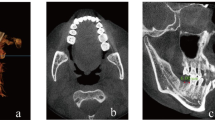
The CBCT images underwent axial-plane adjustments to ensure that the vertical reference line precisely bisects the implant in the bucco-lingual direction. The coronal view of the image was then adjusted to align with the long axis of the implant parallel to the vertical reference line. Subsequently, the image was magnified to the maximum extent within the measurement window to ensure accurate measurements.
The measurement of the proximal and distal parameters of the implant is illustrated in Fig. 2. The vertical height of the mesial bone surrounding the implant was defined as the vertical distance between points B1 and C1. Similarly, the vertical height of the distal bone was measured as the vertical distance between points B2 and C2.
(A) longitudinal axis of the implant, (B) implant’s shoulder line, which is perpendicular to the longitudinal axis A of the implant (B1: located at the apex of the implant on the buccal side, B2: located at the apex of the implant on the lingual side) C: superior line of the proximal–distal bone plate, perpendicular to the longitudinal axis A of the implant (C1: situated at the apex of the mesial bone plate, C2: situated at the apex of the distal bone plate).
Bucco-lingual assessment of the implant was conducted to determine the vertical dimensions of the surrounding bone, as illustrated in Fig. 3. The buccal bone plate’s height was measured as the vertical distance between points B1 and D1, while the lingual bone plate’s height was determined as the vertical distance between points B2 and D2.
The horizontal parameters of bone around the implant were measured as shown in Fig. 4.
The E(0, 1, 3) : Reference line at mm from shoulder line (B) (0, 1, 3), perpendicular to implant major axis A. E1(0, 1, 3) : The distance from the intersection of the buccal bone wall surface of the implant and the mm line E(0, 1, 3) to the surface of the implant, perpendicular to the major axis A of the implant. E2(0, 1, 3) : The distance from the intersections of the bone wall of the lingual side of the implant and the mm lines of E(0, 1, 3) to the surface of the implant, perpendicular to the major axis A of the implant.
Evaluation of marginal bone loss
CBCT imaging was conducted at four distinct time points, namely at T0, T1 and T2. The NNT (Version 9.0, QR, Italy) image processing software was utilized for analysis and measurement. The vertical distance between the highest point of contact between the implant and bone and the uppermost edge of the implant shoulder was measured as a reference point, with separate measurements taken on the proximal–distal and buccal sides. The MBL was calculated as the vertical distance between two points at T0 minus the vertical distance between the same two points at each subsequent visit. The length of the implant was also recorded in case adjustment was necessary. A negative difference indicated marginal bone increase, while a positive difference signified marginal bone absorption.
Evaluation of implant success
The following criteria determined the success of implantation.
-
1.
The esthetic outcome of the restored implant was commendable.
-
2.
Gingivitis could be effectively managed without any implant-related infections.
-
3.
There was no evident harm to the adjacent dental-supporting tissues.
-
4.
The masticatory efficiency exceeded 70%.
-
5.
The implant demonstrated satisfactory clinical inactivity while effectively supporting and retaining denture functions.
-
6.
Vertical bone resorption did not surpass one-third of the length of the implanted portion, as confirmed by standard radiographs. Transverse bone absorption was also limited to one-third, and the implant remained stable.
-
7.
There were no sustained complications such as damage, pain, numbness, paresthesia, or other adverse symptoms after implantation, and the patient reported overall good well-being.
Statistical analysis
SPSS 22.0 software (version 22.0, SPSS Inc., Chicago, IL, USA) was used for statistical analysis of all data. Quantitative data were presented as the mean ± standard deviation (\({\overline{\text{x}}} \pm {\text{s}}\)), Comparisons between groups were conducted using the independent t-test, with a significance level set at α = 0.05.
Results
Descriptives and implant success rate
The demographic characteristics of the 54 patients are presented in Table 1. At the 6-month follow-up (3 months after prosthesis placement), CBCT assessment revealed the absence of any persistent radiolucent area surrounding the implant, as well as the absence of implant loosening, displacement, or detachment. The implant success rate was, remarkably, 100%.
Marginal bone loss (MBL)
Bone resorption at the proximal and distal sites of the implant manifested at T1, and further increased at T2, showing significant increase compared with T1 (P < 0.05). as indicated in Table 2.
The marginal bone absorption of the bucco-lingual site of the implant appeared at T1 and increased at all observation points, there were statistically significant differences in the marginal bone absorption between the time points (P < 0.05), and the bone absorption tended to be stable at T2, as shown in Table 3.
The horizontal bone absorption at the bucco-lingual site of the implant showed no significant marginal bone absorption at any of the observation time points, and there was no statistically significant difference in the bone absorption amount among the groups (P > 0.05), as shown in Table 4.
Discussion
At present, incision and flap surgery represents the primary surgical approach utilized by implantologists around the world. The alveolar bone receives its blood supply from three primary sources, namely mucoperiosteal vessels, the vascular plexus of the periodontal ligament, and intracellular cancellous vessels. Upon tooth loss, the vascular plexus of the periodontal ligament diminishes, leaving the tooth blood supply primarily reliant on the other two sources. Consequently, performing an incision and flap procedure may result in inadequate blood supply to the mucoperiosteal vessels, thereby necessitating a reliance on the blood vessels within the cancellous bone itself to sustain blood flow to the alveolar bone. Notably, cortical bone relies solely on the blood vessels housed within the cancellous bone, implying that bone absorption may occur to some extent during treatment18. Hence, incision and flap surgery requires the incision and subsequent elevation of the mucoperiosteal flap, leading to alterations in periosteal blood flow. Following implant placement, periosteal reconstruction occurs around the implant, inducing varying degrees of bone injury19,20. Furthermore, incision and flap surgery may result in heightened bleeding, an extended duration of operation, and postoperative complications such as pain and swelling, thereby causing discomfort for patients. Moreover, these factors may impede the esthetic outcome of the implantation procedure and increase the psychological burden on patients21.
With the continuous advancement of dental implantology, a trend towards minimally invasive and simplified procedures has emerged. Alongside advancements in implant surface treatment technology and modern medical imaging, the future direction of oral implantology lies in the implementation of minimally invasive implantation techniques, specifically the touch-controlled non-flap approach. The notion of flapless implantation was initially introduced by Kan et al.22, and subsequent basic studies and clinical observations23,24,25 have provided a theoretical foundation for flapless implantation, confirming its clinical feasibility and advantages. In recent years, the introduction of CBCT has enhanced dentists’ comprehension of oral and maxillofacial tissue anatomy, consequently augmenting their cognitive abilities and operational skills in the realm of minimally invasive implantation26,27,28.
CBCT is extensively utilized in the diagnosis and treatment of various conditions within the fields of alveolar surgery, maxillofacial surgery, implantology, orthodontics, orthognathology, and endodontics. The distinctive attributes of CBCT, including its three-dimensional (3D) imaging capabilities and multidirectional imaging, play a significant role in its ability to assess numerous aspects of oral health, including the relationship between impacted wisdom teeth and the inferior alveolar neural tube, the localization of impacted teeth, mandibular angle morphology, hyoid morphology, the condition of the temporomandibular joint, and the state of the pterygopalatine canal29,30,31. Notably, CBCT has proven immensely valuable in preoperative implant surgery planning and postoperative assessment of implant retention15,16,17. The 3D images obtained through CBCT enable thorough examination of the jaw bone structure, and the construction of 3D images using volumetric data facilitates the detailed observation of virtual implantation procedures. Prior to surgery, a comprehensive understanding of the alveolar bone shape, tooth root orientation, and alveolar fossa dimensions can be obtained in three dimensions. This enables the preoperative determination of implant placement direction, specifications, and the required amount of bone grafting in the defect area. Furthermore, CBCT allows for examination of postoperative bone resorption around the implant32. CB CT is a novel product in CT technology. By using conical beam X-rays and the circular rotation scanning method to obtain two-dimensional image data and three-dimensional digital reconstruction, it is capable of conducting various angle scans, such as tangent, oblique, and side incisions. The internal conditions of the mouth can be observed from different perspectives and face to face, enabling small structures like bone trabeculae and periodontal membranes to be clearly displayed without being influenced by surrounding structures33.
The 60 mandibular first molars of 54 patients in this cohort underwent preoperative CBCT examination and subsequent touch-controlled, minimally invasive implantation. Healing abutments were subsequently installed. Postoperative assessments were conducted on the day of surgery, as well as at 1 month and 6 months after surgery to evaluate the changes in peri-implant bone mass. The results revealed bone resorption at the proximal and distal and bucco-lingual sites of the implant within 1 month after surgery, which became more prominent at 6 months. However, bone resorption volume stabilized at 6 months, with only minimal vertical bone absorption observed on the bucco-lingual aspect. This finding supports the occurrence of marginal bone resorption around the implant following implantation1,13. Notably, Cardaropoli et al. reported vertical bone absorption exceeding 0.7 mm after 1 year of implant loading32, which significantly exceeds the levels observed in our study. It is important to highlight that the study by Cardaropoli et al. relied on parallel apical radiography for measurements, thereby precluding the observation of bucco-lingual bone plates via CBCT, which could have contributed to the differences in measurement outcomes.
The present study also revealed that horizontal bone resorption of the proximal, distal, and bucco-lingual aspects of the mandibular first molar implant was not prominent, which may be attributed to the thickness of the bucco-lingual bone plate of the implant. Following the loss of the mandibular first molar, there is minimal bone absorption in this region within a short duration, resulting in there being ample bone on both the buccal and lingual sides of the implant. It has been demonstrated that thicker bone plates can mitigate mechanical stimulation around the implant, alter the surrounding strain state, and reduce strain energy density, thereby minimizing bone resorption33. A comprehensive clinical study conducted by Spray et al. indicated that when the bone plate thickness reached 1.8 mm, the extent of bone absorption significantly decreased, while a decrease in the bone plate thickness led to an increase in bone absorption34. Therefore, when implanting the mandibular first molar, ensuring the stability of the bucco-lingual bone plate can be achieved by maintaining sufficient bone thickness on both the buccal and lingual sides35,36.
However, the duration of observation in our study was limited, necessitating a longer observation period to ascertain the potential stabilization of bone resorption following touch-controlled, minimally invasive implantation following the extraction of the mandibular first molar. The retrospective nature of the study design limited the ability to control for potential confounders and introduced the risk of selection bias. Due to the lack of a control group, such as the traditional flap surgery group, it is difficult to determine the true impact of minimally invasive techniques on peri-implant bone absorption. Additionally, artifacts represent a significant impediment to the diagnostic integrity of CBCT images37. Metal artifacts in CBCT primarily arise from beam hardening phenomena induced by high-density metallic materials, which can compromise the accuracy of evaluations and diagnoses made by dental practitioners38.
In future studies, we will try our best to control bias while adding control group to reflect the superiority of minimally invasive planting technology. To mitigate the occurrence of metal artifacts in CBCT imaging, dental professionals and radiologic technologists can implement strategies such as optimizing equipment settings, avoiding the use of materials with high density and atomic numbers, and employing other effective techniques. With advancing implantation technologies and increasing patient awareness, it is anticipated that an increasing number of patients will undergo touch-controlled, minimally invasive implantation surgery in the foreseeable future.
Conclusion
In this study, after the extraction of the mandibular first molar, a touch-controlled, minimally invasive implantation procedure was performed. Following the placement of the healing abutment, a certain degree of vertical bone resorption was observed in the proximal–distal and bucco-lingual regions surrounding the implant. However, the extent of bone resorption was minimal. These findings hold significant implications for implant clinicians in determining optimal implant surgical method and serve as valuable reference for enhancing the efficacy of implantation treatment.
Data availability
All data generated or analysed during this study are included in this published article.
References
Dereci, Ö. et al. Effects of implant-related variables on the marginal bone loss around dental implants. Quintessence. Int. 51(2), 118–126. https://doi.org/10.3290/j.qi.a43864 (2020).
Albrektsson, T., Zarb, G., Worthington, P. & Eriksson, A. R. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int. J. Oral. Maxillofac. Implants. 1(1), 11–25 (1986).
Schropp, L., Wenzel, A., Kostopoulos, L. & Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics. Restor. Dent. 23(4), 313–323 (2003).
Covani, U., Ricci, M., Bozzolo, G., Mangano, F., Zini, A. & Barone, A. Analysis of the pattern of the alveolar ridge remodelling following single tooth extraction. J. Clin. Oral. Implants. Res. 22 (8), 820–825. https://doi.org/10.1111/j.1600-0501.2010.02060.x (2011)
Hossein Bassir, S., El Kholy, K., Chia-Yu, Chen., Kyu, H. L. & Giuseppe, I. Share Outcome of early dental implant placement versus other dental implant placement protocols: A systematic review and meta-analysis. J. Periodontol. 90(5), 493–506. 10.1002/ JPER.18–0338 (2019).
Wenchao, L., Ning, R., Wei, Zu., Yuan, T. & Senhao, Li. Effects of Minimally Invasive Circumcision Implantation on Implant Stability and Alveolar Crest Bone Resorption in Patients with Dentition Defect. Boletín. De. Malariologíay. Salud. Ambiental. 59 (4), 152–157. (2019).
Romandini, M., Ruales-Carrera, E., Sadilina, S., Hämmerle, C. H. F. & Sanz, M. Minimal invasiveness at dental implant placement: A systematic review with meta-analyses on flapless fully guided surgery. Periodontol.2000.91(1), 89–112. https://doi.org/10.1111/prd.12440 (2023).
Laverty, D. P., Buglass, J. & Patel, A. Flapless dental implant surgery and use of cone beam computer tomography guided surgery. Br. Dent. J. 224(8), 601–611. https://doi.org/10.1038/sj.bdj.2018.268 (2018).
Bagde, H. et al. Healing of Peri-Implant Tissue following Flapless Implant Surgery. J. Pharm. Bioallied. Sci. 15(2), S1139–S1141. https://doi.org/10.4103/jpbs.jpbs_189_23 (2023).
Singh, N. et al. Clinical outcomes of flap versus flapless immediately loaded single dental implants in the mandibular posterior region: One-year follow-up results from a randomized controlled trial. J. Prosthet. Dent. 128(2), 167–173. https://doi.org/10.1016/j.prosdent.2020.08.035 (2022).
Lahoti, K., Dandekar, S., Gade, J. & Agrawal, M. Comparative evaluation of crestal bone level by flapless and flap techniques for implant placement: Systematic review and meta-analysis. J. Indian. Prosthodont. Soc. 21(4), 328–338. https://doi.org/10.4103/jips.jips_208_21 (2021).
Rao, W. & Benzi, R. Single mandibular first molar implants with flapless guided surgery and immediate function: preliminary clinical and radiographic results of a prospective study. J. Prosthet. Dent. 97(6), S3–S14. https://doi.org/10.1016/S0022-3913(07)60003-1 (2007).
Galindo-Moreno, P. et al. Early marginal bone loss around dental implants to define success in implant dentistry: A retrospective study. Clin. Implant. Dent. Relat. Res. 24(5), 630–642. https://doi.org/10.1111/cid.13122 (2022).
Barboza, E. P., Caúla, A. L. & Carvalho, W. R. Crestal bone loss around submerged and exposed unloaded dental implants: a radiographic and microbiological descriptive study. Implant. Dent. 11(2), 162–169. https://doi.org/10.1097/00008505-200204000-00018 (2002).
Rashsuren, O. et al. CBCT Evaluation of Cortical Bone Thickness for Orthodontic Mini-Screw. Cent. Asian. J. Med. Sci. 7, 277–284 (2021).
Song, D. et al. Diagnostic accuracy of CBCT versus intraoral imaging for assessment of peri-implant bone defects. BMC. Med. Imaging. 21(1), 23. https://doi.org/10.1186/s12880-021-00557-9 (2021).
Feng, L., Chen, H., Chen, Z., Chen, Y. & Gu, X. Associations between cortical bone-to-implant contact and microstructure derived from CBCT and implant primary stability. Clin. Oral. Implants. Res. 34(3), 243–253. https://doi.org/10.1111/clr.14037 (2023).
Campelo, L. D. & Camara, J. R. D. Flapless implant surgery: a 10- year clinical retrospective analysis. Int. J. Oral. Maxillofac. Implants. 17(2), 271–276 (2002).
Hermann, J. S., Cochran, D. L., Nummikoski, P. V. & Buser, D. Crestal bone changes around titanium implants.A radiographic evaluation of unloaded nonsubmerged and submerged implants in the canine mandible. J. Periodontol. 68(11), 1117–1130. 10.1902 /jop. 1997.68.11.1117 (1997).
Alzahrani, M. et al. Failure Rate of Dental Implants in the Esthetic Zone: A Systematic Review and Meta-Analysis. Cureus. 16(7), e65506. https://doi.org/10.7759/cureus.65506 (2024).
Froum, S. J. et al. Survival rate of one-piece dental implants placed with a flapless or flap protocol–a randomized, controlled study: 12-month results. Int. J. Periodontics. Restorative. Dent. 31(6), 591–601 (2011).
Kan, J. Y., Rungeharassaeng, K. & Ojano, M. Flapless anterior implant surgery:a surgical and pmsthodontic rational. Pract. Periodonties. Aestliet. Dent. 12(5), 467–474 (2000).
Kolerman, R. et al. Esthetic Assessment of Implants Placed into Fresh Extraction Sockets for Single-Tooth Replace ments Using a Flapless Approach. Clin. Implant. Dent. Relat. Res. 19(2), 351–364. https://doi.org/10.1111/cid.12458 (2017).
Stoupel, J., Lee, C. T., Glick, J., Sanz-Miralles, E. & Chiuzan, C. Papapanou, P, N. Immediate implant placement and provisionalization in the aesthetic zone using a flapless or a flap-involving approach: a randomized controlled trial. J. Clin. Periodontol. 43(12), 1171–1179. https://doi.org/10.1111/jcpe.12610 (2016).
Wang, F., Huang, W., Zhang, Z., Wang, H., Monje, A. & Wu, Y. Minimally invasive flapless vs. flapped approach for single implant placement: a 2-year randomized controlled clinical trial. Clin. Oral. Implants. Res. 22(2), 1–14. https://doi.org/10.1111/clr.12875 (2016).
Fürhauser, R. et al. Esthetics of Flapless Single-Tooth Implants in the Anterior Maxilla Using Guided Surgery: Association of Three-Dimensional Accuracy and Pink Esthetic Score. Clin. Implant. Dent. Relat. Res. 17(2), e427–e433. https://doi.org/10.1111/cid.12264 (2015).
Adrià, J. G., Albert, G. B., Octavi, C. F., Rui, F. & Eduard, V. C. Accuracy assessment of dynamic computer-aided implant placement: a systematic review and meta-analysis. Clin. Oral. Investig. 25(5), 2479–2494. https://doi.org/10.1007/s00784-021-03833-8 (2021).
Wenchao, Li. et al. Clinical Application of the Anterior Maxilla AtraumaticImmediate Implant by Cone Beam Computer Tomography.Science. Discovery. 4(2), 61–64. (2016).
Pimkhaokham, A., Jiaranuchart, S., Kaboosaya, B., Arunjaroensuk, S., Subbalekha, K. & Mattheos, N. Can computer-assisted implant surgery improve clinical outcomes and reduce the frequency and intensity of complications in implant dentistry? A critical review. Periodontol. 2000. 90(1), 197–223. https://doi.org/10.1111/prd.12458 (2022).
Krishankumar, L., Sayali, D., Jaykumar, G. & Megha. A. Comparative evaluation of crestal bone level by flapless and flap techniques for implant placement: Systematic review and meta-analysis. J. Indian. Prosthodont. Soc. 21(4), 328–338. https://doi.org/10.4103/jips.jips_208_21 (2021).
Lemos, C. A. A. et al. Comparison between flapless and open-flap implant placement: a systematic review and meta-analysis. Int. J. Oral. Maxillofac. Surg. 49(9), 1220–1231. https://doi.org/10.1016/j.ijom.2018.04.002 (2020).
Jacobs, R., Vranckx, M., Vanderstuyft, T., Quirynen, M. & Salmon, B. CBCT vs other imaging modalities to assess peri-implant bone and diagnose complications: a systematic review. Eur. J. Oral. Implantol. 11(1), 77–92 (2018).
Karl, M., Buder, T., Krafft, T. & Grobecker-Karl, T. Reliability of clinical techniques for evaluating alveolar bone quality and primary implant stability. Quintessence. Int. 50(5), 388–393. https://doi.org/10.3290/j.qi.a42297 (2019).
Cardaropoli, G. & Lekholm, U. J. L. Tissue alterations at implant-supported single-tooth replacements: a 1-year prospective clinical study. Clin. Oral. Implants. Res. 17(2), 165–171. https://doi.org/10.1111/j.1600-0501.2005.01210.x (2006).
Zheng, K. et al. Effects of buccal thickness augmentation on bone remodeling after maxillary anterior implantation. Biomech. Model. Mechanobiol. 19(1), 133–145. https://doi.org/10.1007/s10237-019-01200-x (2020).
Spray, J. R., Black, C. G., Morris, H. F. & Ochi, S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann. Periodontol. 5(1), 119–128. https://doi.org/10.1902/annals.2000.5.1.119 (2000).
Pinto, M. G. O. et al. Influence of exposure parameters on the detection of simulated root fractures in the presence of various intracanal materials. Int. Endod. J. 50(6), 586–594. https://doi.org/10.1111/iej.12655 (2017).
de Rezende Barbosa, G. L., Sousa Melo, S. L., Alencar, P. N., Nascimento, M. C. & Almeida, S. M. Performance of an artefact reduction algorithm in the diagnosis of in vitro vertical root fracture in four different root filling conditions on CBCT images. Int. Endod. J. 49(5): 500–508. https:// https://doi.org/10.1111/iej.12477 (2016).
Funding
This work was supported to the Program for Young Talents of Science and Technology in Universities of Inner Mongolia Autonomous Region (Grant NO. NJYT 23064), the First-class Scientific Research Fund Project of Stomatology School of Chifeng University (Grant NO. KQYXYYLXK 202101), and the Chifeng University Affiliated Hospital research project (Grant NO. FSYY2022-20).
Author information
Authors and Affiliations
Contributions
Wenchao Li and Yuan Tian. contributed to the conception and design of this study; Ning Ruan, Weize Han and Senhao Li. contributed to data acquisition; Senhao li and Xinxin Zhang contributed to the interpretation of data/results; Haoyang Yu performed the data analyses; Wenchao Li, Yuan Tian, Senhao li, and Yu Xie drafted and revised themanuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study has been approved by the Clinical Research Ethics Committee of the Affiliated Hospital of Chifeng University of Inner Mongolia, China (fsyy202149). All methods were carried out in accordance with relevant guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, W., Ruan, N., Tian, Y. et al. Short-term cone beam CT study on bone mass changes post touch-controlled minimally invasive mandibular molar implant. Sci Rep 15, 10923 (2025). https://doi.org/10.1038/s41598-024-84209-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84209-2