Abstract
The genus Schistosoma causes a schistosomiasis which is one of the neglected tropical diseases that pose a major threat to public health in East Africa. Praziquantel (PZQ) is the first line drug to treat human schistosomiasis. However, there is scarcity of pooled and summarized data on PZQ efficacy to policymakers. Articles were searched from PubMed, Google Scholar, Web of Science, and Scopus databases. In total, 87 published articles were retrieved. Only studies conducted in English that reported the efficacy of PZQ against Schistosoma mansoni, regardless of the year, and studies with more than fifty positive cases were included in the present study. Excel software was used to extract the name of the authors, the total sample size, number of cured participants, the study area, and the year of publication. The pooled efficacy of PZQ against S. mansoni was analyzed using CMA Version 2.2 software. A total of 21 studies fulfilled the inclusion criteria for the present systematic review and meta-analysis. The overall pooled efficacy of PZQ was 85.0% (95% CI: 80.0-89.0%) against S. mansoni. In subgroup analysis, the efficacy of PZQ against S. mansoni was 90.4% in Ethiopia, 71.2% in Kenya, 97.9% in Rwanda, 75.4% in Tanzania, and 68.4% in Uganda. Its heterogeneity was high (I2 = 94.8), and the there is no publication bias between studies. The overall effectiveness of PZQ against S. mansoni in East Africa is doubtful. Therefore, repeated doses should be advocated.
Similar content being viewed by others
Introduction
The genus Schistosoma are also called blood flukes, or trematode worms, which cause both acute and chronic schistosomiasis1. Transmission occurs when skin-piercing cercariae which is present in the infected freshwater bodies gets an access to enter to the human body. Individuals of all ages are susceptible to infection when bathing, swimming, or wading in tainted freshwater2.
Schistosomiasis is common in tropical and subtropical regions, particularly among impoverished populations lacking access to clean drinking water and proper sanitation1. According to current estimates, 11,792 people worldwide pass away from schistosomiasis each year1. In Africa, where incidence rates of the disease can surpass 50% in local communities, schistosomiasis accounts for an estimated 85% of all cases worldwide. Schistosoma mansoni is widespread throughout Africa2.
The parasite eggs in stool are identified under a microscope to make the diagnosis. For populations living in endemic areas, sensitive, and quick point-of-care tests are required for the identification of worm antigens in serum or eggs in excreta. Because egg shedding in travelers and those who have never had schistosomiasis may not be consistent, serologic tests are helpful in diagnosing light infections2,3.
It is estimated that Africa is home to at least 90% of people with schistosomiasis who require treatment1. The recommended and first line treatment for all types of schistosomiasis is PZQ1. It works best against adult parasite forms together with strong host’s immune system. Even though a single course of treatment is typically curative, repeat treatment may be necessary after 2–4 weeks to maximize success, especially in patients with mild infections, since the immune response may be weaker in these cases2. Concerns about potential drug resistance have been raised due to the use of a single medication to treat a disease with such a high burden, particularly in endemic areas4. According to McManus, Dunne3, PZQ is safe and effective against adult worms of all six Schistosoma species that infect humans. However, it does not prevent reinfection, and the establishment of drug resistance is a significant problem.
PZQ is extremely effective against a variety of trematodes, including all schistosome species, and has no structural kinship with the other anthelminthics. Children older than four years old are administered the medication in a single dose of 40 mg/kg5. The WHO states that the cure rate and egg reduction rate are used to evaluate PZQ’s effectiveness against Schistosoma species.
PZQ treatment produced normal cure rates (78 ± 88%) for individuals from the area temporarily living in an urban area without transmission, with re-treatment after three weeks for those from the area who were not cured6. In Ethiopia, S. mansoni infections had a pooled cure rate of 89.2% with 40 mg/kg PZQ. Similarly, among individuals infected with S. mansoni, the mean rates of egg reduction at 40 mg/kg PZQ were 90.2%7. Using the geometric mean of the egg count and the arithmetic mean, the egg reduction rate was 87.95% and 99.85%, respectively8. PZQ pooled cure rate was determined to be 86.65%8.
Ethiopian children infected with S. mansoni reacted favorably to the standard PZQ dosage, and PZQ overall cure rates were greater in Amhara regional state than in Oromia regional state. In the regional states of Oromia and Amhara, the pooled cure rates were 84.79% and 88.58%, respectively8. In addition to mass drug administration, schistosomiasis can be prevented by avoiding bathing, swimming, wading, or other contact with freshwater in disease-endemic areas. There is currently no vaccine or medication available to prevent illness2.
Generally, many studies evaluating the efficacy of PZQ against S. mansoni infection have been conducted across various regions. However, there has been limited systematic review or meta-analysis performed specifically within the East African region. Therefore, the present systematic review and meta-analysis aimed to determine the efficacy of PZQ against S. mansoni infection in East African countries.
Materials and methods
Criteria for inclusion and exclusion of studies
Studies reporting the efficacy of PZQ against S. mansoni, conducted in English, and in any year, examining the efficacy of PZQ between 14 and 21 days after treatment5, conducted with single dose of PZQ, and reporting more than 50 positive cases were included in the current study. However, studies that were reviews, duplicated, extended analyses from an earlier study, incomplete, or used additional anthelminthic drugs like artemisinin, pyrimethamine, or oxamniquine against S. mansoni were excluded.
Search strategy
The PubMed, Google Scholar, Web of Science, and Scopus databases were searched for articles written in English and containing the keywords: ‘’Schistosoma mansoni’’ AND ‘’World,’’ ‘’Efficacy’’ AND ‘‘Praziquantel,’’ ‘’Praziquantel’’ AND ‘‘Schistosoma mansoni,’’ ‘’Anthelminthic drug’ AND ‘’Schistosoma mansoni,’’ AND ‘‘Praziquantel’’ combined with ‘Schistosoma mansoni.’’from June 2024 to September 2024.
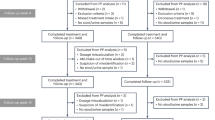
The electronic data search for the studies was conducted on published papers until September 2024. Identification, screening, checking eligibility, and inclusion of the relevant literature were done following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)9 (Fig. 1). Articles were first screened to remove duplicates by reading titles and abstracts, and were initially excluded if they did not specifically refer to S. mansoni or if they were review articles. Finally, the articles were further screened by reading the full text and were excluded if they did not investigate the efficacy of PZQ against S. mansoni. The final retrieved papers were evaluated by the first and the second authors.
Method of data extraction and analysis
The data extraction method was developed by MS and reviewed by TH, DD, KG, LZ and DM. The data extraction method consisted of the name of authors, year of publication, study region, sample size taking the drug, number of cured after 14 days, name of parasite involved. The following information was extracted from the accepted studies: author, publication year, study area, total sample size, number of cured, parasite involved, which was based on the cure rate. The extracted data was analyzed using meta-analysis. The meta-analysis was also performed using Comprehensive Meta-Analysis (CMA) software version 2.2 (Biostat Inc., Englewood, NJ, USA). The efficacy of PZQ against S. mansoni was calculated using a random-effects model at a 95% confidence interval (CI). Heterogeneity between studies were assessed using the Cochran (Q)-value, p-value, inverse variance index (I2) test, and visual inspection of the funnel plot. I2-values lower than 25%, between 25% and 50%, and above 50% were regarded as low, moderate, and high heterogeneity, respectively10. For all tests, the level of statistical significance was set at p < 0.05.
Data quality assessment
The cure rate (CR) of a single dose of PZQ for the treatment of S. mansoni was the main result of this review and meta-analysis. Using Jaded scoring standards, the three reviewers independently evaluated the caliber of the searched studies that were part of the review11. The three investigators jointly rechecked the quality score and had a discussion to settle any discrepancies once it had been cross-checked.
Result
Articles selected for the study
A total of 87 studies were identified. Sixty-seven studies were screened and recorded after duplicates were removed. Twenty-one studies were deemed eligible after a full document assessment. Finally, the total number of articles incorporated into the final systematic review and meta-analysis was 21 for S. mansoni.
Characteristics of the eligible studies
Mostly, the distribution of studies on the efficacy of PZQ against S. mansoni in East Africa was high in Ethiopia and low in Rwanda. The studies were from only five countries: Ethiopia (11, or 52.4%), Tanzania (4, or 19.1%), Uganda (3, or 14.3%), Kenya (2, or 9.5%), and Rwanda (1, or 4.8%) (Table 1).
The efficacy of PZQ againstSchistosoma mansoni
A total of 4889 positive cases of S. mansoni were included in the eligible studies in East Africa. The efficacy of PZQ against S. mansoni ranged from 61.8 to 99.1%. Its pooled efficacy against S. mansoni was 85.0% (95% CI: 80.0–89.0%) (Fig. 2).
Subgroup analysis of PZQ efficacy studies againstS. mansoniby country
The efficacy of PZQ against S. mansoni was highest in Rwanda at 97.9% (95% CI: 94.5-99.2%), followed by Ethiopia at 90.4% (95% CI: 88.9-93.0%), in Tanzania at 75.4% (95% CI: 62.9-84.7%), in Kenya at 71.2% (95% CI: 58.8-80.4%), and the least was in Uganda at 68.4% (95% CI: 48.2-83.5%) in descending order (Fig. 3).
Subgroup analysis of PZQ efficacy studies against S. mansoni by study year
The efficacy of PZQ against S. mansoni across study years was highest 91.4% from 2016 to 2023 years followed by 77.0% from 2008 to 2015 years, and 72.3% from 2000 to 2007 (Fig. 4).
Heterogeneity among studies reviewed for PZQ efficacy againstS. mansoni
The 21 articles reviewed for PZQ efficacy against S. mansoni were highly heterogeneous (I2 = 94.8; P < 0.001 (Table 2).
Publication bias among studies reviewed for PZQ against S. mansoni in East Africa
The studies were distributed symmetrically around the combined effect size, indicating the absence of publication bias. The dot-like structure represents the number of studies, the middle line represents the estimated value, and the diagonal lines represent the 95% confidence limits around the summary efficacy estimate (Fig. 5).
Discussion
The neglected tropical disease schistosomiasis, which is primarily found in sub-Saharan Africa but also occurs in portions of the Middle East, South America, and Southeast Asia, is brought on by parasitic flatworms of the genus Schistosoma. Praziquantel, an anti-schistosome medication, is effective and safe against adult parasites of all Schistosoma species that infect people; however, it does not stop reinfection, and drug resistance is a persistent worry33. In the present study, the pooled efficacy of PZQ against S. mansoni was 85.0% (95% CI: 80.1-88.9%) in East Africa. According to WHO guideline, it was doubtful efficacious5. The current finding is in line with the review result previously reported in school children 86.6% in Ethiopia8. In this review, the cure rate (CR) was 85.0% better than previously reported review34 was70% that indicates that low CR and egg reduction rate (ERR) could be improved by higher PZQ treatment doses. However, this result slightly lower than the previously reported reviews of infected individuals in Ethiopia 89.2% (95% CI: 85.4–93.1)7. In contrast, the other reviews showed that PZQ had high efficacy4. The difference in efficacy might be due to the difference period of assessment, the stage of the parasite present in the host, immune status of the participants, ubiquitous nature of the parasite, the extreme resistance of its egg to harsh environments, age group, brand of drug, infection intensity, nature of study population, sample size, and brand of the drug used.
The efficacy of PZQ against S. mansoni in Rwanda was highly efficacious than others East Africa country (97.9% (95% CI: 94.5-98.2%)) which is satisfactory based on to the WHO guideline. This review result is higher than the previous review results reported 89.2%7, 86.6%8, and 70%35 in different areas. Similarly, to Rwanda, the efficacy of PZQ against S. mansoni in Ethiopia was highly efficacious (90.4% (95% CI: 88.9- 93.0%)) than others East Africa country with in the satisfactory range. This result similar with the studies conducted in Australia33. However, this review result is higher than reviews findings 89.2%7, 86.6%8, and 70% reported earlier35. This efficacy difference might be due to variations in baseline infection intensity, nature of study population, sample size, and brand of the drug used.
In the subgroup analysis, the efficacy of PZQ against S. mansoni in Tanzania and Kenya were 75.5% (95% CI: 63.4- 84.6%) and 71.2% (95% CI: 59.8- 80.4%), which are doubtful efficacious against S. mansoni based on the WHO guideline. This findings are lower than the previous reviews results reported 89.2%7, and 86.6%8. However, these reviews are higher than the previous review findings reported 70%35. This difference might be due to variations in the infection intensity, nature of study population, sample size, and brand of the drug used.
In the current review, the efficacy of PZQ against S. mansoni in Uganda was 68.4% (95% CI: 48.2- 83.5%) which is a reduced efficacious against S. mansoni based on WHO guide line. This review finding is lower than the reviews reports 89.2%7, 86.6%8, and the 70%35 obtained previously. The difference in efficacy might be due to the difference period of assessment, the stage of the parasite present in the host, immune status of the participants, age group, brand of drug, infection intensity, nature of study population, sample size, and brand of the drug used.
In the present review, the efficacy of PZQ against S. mansoni from 2000 to 2007 and 2008–2015 years against S. mansoni were 72.3% and 77.1%, respectively according to WHO guide line. This finding is lower than previous review reports 89.2%7, 86.6%8. However, it is higher than the reviews reported 70%35. In contrast, the efficacy of PZQ against S. mansoni from 2016 to 2023 years, was 91.4%, which is satisfactory efficacious against S. mansoni. This finding is higher than previous review reports 89.2%7, 86.6%8, and 70%35. The duration of assessment between the initial doses and the follow-up, the stage at which the parasite present in the host, the participants’ immune status, age group, and drug brand, the nature of the study population, sample size, and drug brand, might be the contribute factors for the differences in efficacy.
The heterogeneity among studies reviewed for PZQ efficacy against S. mansoni was I2 = 94.8%, P < 0.001, indicating that there was a significant difference between the investigations were high. We conducted the source of heterogeneity by considering region of study, nature of study participants, year of study, and S. mansoni species. All these did not contribute to the observed heterogeneity. Other conditions such as sample size, infection intensity, and specific intervention time and area might contribute to the observed heterogeneity across studies. The result is in line with the study conducted previously in Ethiopia7. Publication bias among studies reviewed for PZQ efficacy against S. mansoni, the funnel plot used in this investigation proved effective. The equitable distribution of the studies into the plot’s median alignment suggests that there was no publication bias among the studies.
By giving deworming medication to all susceptible groups in a designated area to lessen the burden of infection, this study may be implicated. Coordinating and communicating regularly can help with case referrals, treatment follow-up, and the distribution of health education resources. Encourage the incorporation of intestinal parasite prevention strategies into national health programs and provide sufficient resources for their execution. This will guarantee the viability of deworming initiatives and facilitate their inclusion into the current healthcare systems.
Conclusion and recommendations
In East Africa, the efficacy of PZQ against S. mansoni infection is decreases from the standard. PZQ is found to be highly efficient against S. mansoni in Ethiopia and Rwanda, but less effective against S. mansoni in Kenya, Tanzania, and Uganda based on the WHO cut off value Therefore, utilizing re-doses PZQ and periodic efficacy evaluation might be important in East African countries like Ethiopia and Rwanda. The effectiveness of PZQ against S. mansoni will require more research in Tanzania and Kenya. For S. mansoni, an alternate medication should be looked for in Uganda. Encourage the inclusion of intestinal parasite control methods in national health policies and provide sufficient money for their implementation when formulating policy. This will guarantee the viability of deworming initiatives and facilitate their inclusion into current healthcare systems.
Limitations
This meta-analysis, which also examined the PZQ effectiveness studies, produced a pooled cure rate. However, it has a number of limitations. To begin, the studies that comprised this meta-analysis did not include a control group or individuals receiving a placebo during the intervention period. Because of this, it is impossible to compute relative risk or the risk ratio (RR). Consequently, the risk ratio has to be replaced by the cure rate. Second, one unique parasitological method (Kato-Katz) was used in the studies that matched the criteria for this meta-analysis. The sensitivity and specificity of these methods may affect the findings of PZQ efficacy. Lastly, not all of the papers that met the requirements for our study revealed PZQ’s drawbacks. Last but not least, the published papers on the effectiveness of PZQ against S. mansoni were only available in English and were based on a small database.
Data availability
Data will available freely online and Bahir Dar University database (https://www.researchgate.net/institution/Bahir_Dar_University), and Debre Tabor University ResearchGate (https://www.researchgate.net/institution/Debre_Tabor_University).
References
WHO, Schistosmiasis & Accessed on March 30 (2024). https://www.who.int/news-room/fact-sheets/detail/schistosomiasis
CDC & Schistosomiasis Accessed on March 30, (2023). https://www.cdc.gov/schistosomiasis/index.html
McManus, D. P. et al. Nat. Rev. Dis. Primers ;4(1):13. (2018).
Kabuyaya, M., Chimbari, M. J. & Mukaratirwa, S. Efficacy of praziquantel treatment regimens in pre-school and school aged children infected with schistosomiasis in sub-saharan Africa: a systematic review. Infect. Dis. Poverty. 7 (1), 1–7 (2018).
WHO. Assessing the efficacy of anthelminthic drugs against schistosomiasis and soil-transmitted helminthiases: Geneva: World Health Organization. : 1–13. 2013 [ (2013).
Gryseels, B. et al. Are poor responses to praziquantel for the treatment of Schistosoma mansoni infections in Senegal due to resistance? An overview of the evidence. Trop. Med. Int. Health. 6 (11), 864–873 (2001).
Hailegebriel, T., Nibret, E. & Munshea, A. Efficacy of praziquantel for the treatment of human schistosomiasis in Ethiopia: a systematic review and meta-analysis. J. Trop. Med. 2021, 1–12 (2021).
Bisetegn, H. & Erkihun, Y. Efficacy of praziquantel treatment for Schistosoma mansoni infection among children in Ethiopia: a systematic review and metaanalysis. Int. J. Immunol. 8 (4), 61–69 (2020).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. ;10.1136/bmj.n71:n71. (2021).
Ioannidis, J. P., Patsopoulos, N. A. & Evangelou, E. Uncertainty in heterogeneity estimates in meta-analyses. Br. Med. J. 335 (7626), 914–916 (2007).
Jadad, A. R. M. R. et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control clin trials. 17: 1–12. (1996).
Bajiro, M. et al. Prevalence of Schistosoma mansoni infection and the therapeutic efficacy of praziquantel among school children in Manna District, Jimma Zone, Southwest Ethiopia. Parasit. Vectors. 9 (1), 560 (2016).
Berhanu, M. S., Atnafie, S. A., Ali, T. E., Chekol, A. A. & Kebede, H. B. Efficacy of praziquantel treatment and Schistosoma mansoni infection among primary school children in Kemisse town, Northeast Ethiopia. Ethiop. J. Health Sci. 32 (3), 631–640 (2022).
Dejenie, T., Asmelash, T. & Abdelkadir, M. Efficacy of praziquantel in treating Schistosoma mansoni infected school children in Tumuga and Waja, north Ethiopia. Momona Ethiop j sci. ;2(2). (2010).
Ejigu, K., Hailu, T. & Alemu, M. Efficacy of mebendazole and praziquantel against soil-transmitted helminths and Schistosoma mansoni infections among schoolchildren in Northwest Ethiopia. Biomed. Res. Int. 2021, 6682418 (2021).
Gebreyesus, T. D. et al. Efficacy and safety of praziquantel preventive chemotherapy in Schistosoma mansoni infected school children in southern Ethiopia: a prospective cohort study. Front. Pharmacol. 14, 968106 (2023).
Samuel, H. L. G. & Zeleke, M. Prevalence of Schistosoma mansoni and effectiveness of praziquantel in school children in Finchaa Valley, Ethiopia. J. Parasitol. Vector Biol. 4 (3), 25–30 (2012).
Hailu, T. et al. Efficacy of single dose albendazole and praziquantel drugs among helminth-infected school children at Rural Bahir Dar, northwest Ethiopia. Trop. Doct. 48 (4), 270–272 (2018).
Reta, B. & Erko, B. Efficacy and side effects of praziquantel in the treatment for Schistosoma mansoni infection in school children in Senbete Town, northeastern Ethiopia. Trop. Med. Int. Health. 18 (11), 1338–1343 (2013).
Tadele, T. et al. Efficacy and safety of praziquantel treatment against Schistosoma mansoni infection among pre-school age children in southern Ethiopia. Trop. Med. Health. 51 (1), 72 (2023).
Tesfie, A. et al. Praziquantel is an effective drug for the treatment of Schistosoma mansoni infection among school-aged children in Northwest Ethiopia. Trop. Med. Int. Health. 48 (1), 1–8 (2020).
Woldegerima, E., Bayih, A. G., Tegegne, Y., Aemero, M. & Jejaw Zeleke, A. Prevalence and reinfection rates of Schistosoma mansoni and praziquantel efficacy against the parasite among primary school children in Sanja Town, Northwest Ethiopia. J. Parasitol. Res. 2019, 3697216 (2019).
Obonyo, C. O., Muok, E. M. & Mwinzi, P. N. Efficacy of artesunate with sulfalene plus pyrimethamine versus praziquantel for treatment of Schistosoma mansoni in Kenyan children: an open-label randomised controlled trial. Lancet Infect. Dis. 10 (9), 603–611 (2010).
Thiongo, F., Mbugua, G., Ouma, J. & Sturrock, R. Efficacy of oxamniquine and praziquantel in school children from two Schistosoma mansoni endemic areas. East. Afr. Med. J. 79 (1), 29–33 (2002).
Kabatende, J. et al. Efficacy of single-dose praziquantel for the treatment of Schistosoma mansoni infections among school children in Rwanda. Pathogens ;12(9). (2023).
Mazigo, H. D., Dunne, D. W., Kinung’hi, S. M. & Nuwaha, F. Praziquantel efficacy against Schistosoma mansoni among HIV-1 infected and uninfected adults living in fishing villages along Lake Victoria, Northwest Tanzania. Infect. Dis. Poverty. 3 (1), 47 (2014).
Mnkugwe, R. H., Minzi, O. S., Kinung’hi, S. M., Kamuhabwa, A. A. & Aklillu, E. Efficacy and safety of praziquantel for treatment of Schistosoma mansoni infection among school children in Tanzania. Pathogens ;9(1). (2019).
Munisi, D. Z., Buza, J., Mpolya, E. A., Angelo, T. & Kinung’hi, S. M. The efficacy of single-dose versus double-dose praziquantel treatments on Schistosoma mansoni infections: its implication on undernutrition and anaemia among primary schoolchildren in two on-shore communities, northwestern Tanzania. Biomed Res Int. ;2017. (2017).
Olliaro, P. L. et al. A multicentre randomized controlled trial of the efficacy and safety of single-dose praziquantel at 40 mg/kg vs. 60 mg/kg for treating intestinal schistosomiasis in the Philippines, Mauritania, Tanzania and Brazil. PLoS Negl. Trop. Dis. 5 (6), e1165 (2011).
Kabatereine, N. et al. Efficacy and side effects of praziquantel treatment in a highly endemicSchistosoma mansoni focus at Lake Albert, Uganda. Trans. R Soc. Trop. Med. Hyg. 97 (5), 599–603 (2003).
Nalugwa, A., Nuwaha, F., Tukahebwa, E. M. & Olsen, A. Single versus double dose praziquantel comparison on efficacy and Schistosoma mansoni re-infection in preschool-age children in Uganda: a randomized controlled trial. PLoS Negl. Trop. Dis. 9 (5), e0003796 (2015).
Tukahebwa, E. M., Vennervald, B. J., Nuwaha, F., Kabatereine, N. B. & Magnussen, P. Comparative efficacy of one versus two doses of praziquantel on cure rate of Schistosoma mansoni infection and re-infection in Mayuge District, Uganda. Trans. R Soc. Trop. Med. Hyg. 107 (6), 397–404 (2013).
McManus, D. P. The Search for a Schistosomiasis Vaccine: Australia’s Contribution. Vaccines (Basel) ;9(8). (2021).
Fukushige, M., Chase-Topping, M., Woolhouse, M. E. & Mutapi, F. Efficacy of praziquantel has been maintained over four decades (from 1977 to 2018): a systematic review and meta-analysis of factors influence its efficacy. PLoS Negl. Trop. Dis. 15 (3), e0009189 (2021).
Liu, R., Dong, H. F., Guo, Y., Zhao, Q. P. & Jiang, M. S. Efficacy of praziquantel and artemisinin derivatives for the treatment and prevention of human schistosomiasis: a systematic review and meta-analysis. Parasit. Vectors. 4, 201 (2011).
Acknowledgements
We would like to acknowledge Debre Tabor and Bahir Dar university for internet and materials support to complete this work.
Funding
The budget for the review was covered by authors.
Author information
Authors and Affiliations
Contributions
MS-Developed the conception of the review, designed the methodology, participated in data collection, manuscript drafting and data analysis and approved the final manuscript. TH- Participated in designing and editing and finally approved the manuscript. DD, KG, LZ and DM-Participated in data collection, analyzing, editing and finally approved the final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sisay, M., Hailu, T., Damtie, D. et al. Efficacy of single dose praziquantel against Schistosoma mansoni in East Africa: a systematic review and meta-analysis. Sci Rep 15, 4642 (2025). https://doi.org/10.1038/s41598-024-84621-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84621-8