Abstract
This study aimed to evaluate the clinical application of different myopia correction methods in the prevention and control of myopia in adolescents. A total of 145 myopic adolescents aged 8 to 15 years were included, and their eyes were divided into four groups based on the treatment modality: wearing Defocus Incorporated Multiple Segments (DIMS) spectacle lenses alone (Group A), orthokeratology (OK) lenses alone (Group B), DIMS spectacle lenses combined with racemic anisodamine eye drops (Group C), and OK lenses combined with racemic anisodamine eye drops (Group D). The primary outcomes, including axial length and refractive error (expressed as spherical equivalent refraction, SER), were measured at baseline and at the 12-month follow-up. The clinical effects of each group were compared. The results showed significant differences in myopia progression across the groups, with Group D showing the least axial elongation. OK lenses were more effective than DIMS spectacle lenses in controlling myopia progression, and the combination of racemic anisodamine eye drops further enhanced the correction effect. This study provides important clinical evidence for myopia control interventions in adolescents.
Similar content being viewed by others
Introduction
Myopia, a common refractive error, is characterized by blurred distance vision while near objects remain clear1. Its pathogenesis is typically associated with excessive axial elongation, particularly during childhood and adolescence2. This process is influenced by various factors, including genetics, environment and lifestyle habits such as prolonged near work3. The rising prevalence of myopia worldwide has become a significant concern, with projections estimating that the global number of myopia cases will reach 2.5 billion by the end of this century4. In China, approximately 90% of adolescents are affected by myopia, making it the country with the largest number of myopia cases globally5. High myopia can lead to retinal deformation, which significantly increases the risk of severe complications such as retinal detachment, glaucoma, and cataracts6. Therefore, timely prevention and control of myopia in adolescents are of critical importance.
Among the various myopia control methods, orthokeratology (OK) lenses have gained significant attention as a non-surgical intervention7,8. OK lenses are rigid contact lenses worn overnight, which apply gentle pressure to the cornea through a reverse geometric design, temporarily reshaping the central corneal curvature. This results in clear vision during the day without the need for glasses9. More importantly, OK lenses induce a “myopic defocus” effect in the peripheral retina, focusing peripheral light in front of the retina, thereby inhibiting axial elongation and effectively slowing the progression of myopia. This design is considered one of the key factors contributing to the significant effect of OK lenses in myopia control10,11. Unlike OK lenses, Defocus Incorporated Multiple Segments (DIMS) spectacle lenses create a defocus effect in the peripheral area primarily through lens design, without altering the shape of the eye12. The optical effect is entirely achieved through the design of the lenses, making them suitable for daily wear. DIMS lenses are easy to wear and require minimal lens care, whereas OK lenses demand a higher level of hygiene and care to reduce the risk of infection13.
In addition, pharmacological interventions have been introduced into the field of myopia control. For example, low-concentration atropine eye drops help control myopia progression by relaxing the ciliary muscle and reducing accommodative load14. Studies have shown that, among European children and adolescents, both DIMS lenses and 0.01% atropine eye drops significantly reduce axial elongation, with the combined use of the two showing the most pronounced effect15. This highlights the efficacy of combining optical and pharmacological interventions in myopia control. Racemic anisodamine, as also an anticholinergic agent, has certain pharmacological effects; however, while anticholinergic drugs have demonstrated efficacy in some ophthalmic applications16, there is currently insufficient clinical evidence to confirm their effectiveness in treating and alleviating myopia.
Given the differences in design and application between OK lenses and DIMS spectacle lenses in myopia control, further investigation into their potential differences in controlling myopia progression is of significant importance. This study aims to systematically evaluate the effectiveness of OK lenses and DIMS lenses, both individually and in combination with racemic anisodamine eye drops, in controlling myopia progression in adolescents, providing evidence for safe and effective clinical strategies in myopia prevention and control.
Subjects and methods
Subjects
Clinical data were collected from 145 adolescents (280 eyes) diagnosed with myopia who attended the Department of Ophthalmology of the First Affiliated Hospital of ChongQing Medical and Pharmaceutical College from July 2022 to October 2023. The participants were divided into four groups based on the myopia correction treatment modalities: Group A: wearing DIMS spectacle lenses alone (35 participants, 70 eyes). Group B: OK lenses alone (38 participants, 72 eyes). Group C: DIMS spectacle lenses combined with racemic anisodamine eye drops (35 participants, 70 eyes). Group D: OK lenses combined with racemic anisodamine eye drops (37 participants, 68 eyes). The study was approved by the Ethics Committee of the First Hospital Affiliated with Chongqing Higher School of Medicine, and written informed consent was obtained from all participants and their guardians.
Inclusion and exclusion criteria
The inclusion criteria were as follows: adolescents who underwent comprehensive ocular assessments, including evaluation of the anterior segment, unaided visual acuity, cycloplegic refraction, corneal topography, ocular axial length measurement, corneal endothelial microscopy, fundus examination, and an overall assessment to determine eligibility for the treatment modalities. The specific criteria were: (a) Age between 8 and 15 years; (b) Children diagnosed with pure myopia with a corrected visual acuity of at least 5.0 in at least one eye; (c) A mean spherical equivalent refraction (SER) between − 1.00 D and − 6.00 D, with regular astigmatism no greater than − 1.50 D; (d) No history of ocular or systemic diseases; (e) No prior use of interventions for myopia control, including hard contact lenses, multifocal soft contact lenses, low-concentration atropine, or specialized frame lenses other than mono-focal glasses. Participants in the OK lenses groups (Group B and D) were also required to possess the necessary skills for lens use and care, including the ability to independently or with parental assistance wear, remove, clean, rinse, and store the lenses.
Participants were excluded if they presented with any of the following: (a) Ophthalmological conditions other than refractive error (e.g., ptosis, amblyopia, strabismus, congenital cataracts, glaucoma, retinal disorders); (b) A family history of genetic myopia; (c) A prior history of ocular surgery; (d) Presence of systemic diseases affecting vision or visual function; (e) Severe mental illness and cognitive dysfunction.
Data collection and follow-up
Basic information (name, sex, and age) and myopia-related ocular biological parameters were collected, including: visual acuity, axial length, corneal curvature, and SER.
Participants were followed up at 3, 6, and 12 months after the baseline visit. At each follow-up visit, axial length and SER were re-measured to assess changes over time.
Instrumentation and measurements
Ocular axial length were measured using an ophthalmic optical biometer (IOL Master 500, Carl Zeiss Meditec, Germany). Each measurement was repeated at least five times per eye, and the mean value was recorded. Refraction error was assessed using a Nidek ARK-1 computerized keratometer after pharmacological dilation of the pupil. Compound tropicamide eye drops (Medrol) were instilled, and optometry was performed 30 min after full ciliary muscle paralysis and pupil dilation (pupil diameter > 6 mm). Measurements were repeated three times per eye, and the mean value was calculated. Refractive error was expressed as the SER, calculated as: SER = spherical power + (1/2 × cylindrical power).
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows (version 26.0). For continuous data, the Shapiro-Wilk test was used to assess normality. Data with a normal distribution were expressed as mean ± standard deviation (SD). Group comparisons were performed using the independent samples t-test for two groups and one-way analysis of variance (ANOVA) for multiple groups. Non-normally distributed data were analyzed using the Mann-Whitney U test. Categorical variables were expressed as n (%), and group comparisons of sex and age distribution were performed using the chi-square test. A P-value of < 0.05 was considered statistically significant.
Results
Baseline characteristics
Table 1 presents the baseline characteristics of four patient groups undergoing different myopia correction methods. No statistically significant differences were observed among the groups in terms of sex, age, SER, corneal curvature, or ocular axis length (P > 0.05), indicating that the baseline parameters were comparable across the adolescent myopia correction groups.
Comparison of different myopia control methods on axial elongation
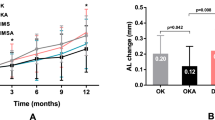
When comparing the effects of four myopia control methods on axial elongation, there were no significant differences in axial length between the four groups at baseline (P > 0.05). The axial lengths during the follow-up period are shown in Table 2. At 3 months post-treatment, the axial elongation in Group B (OK lens group) was significantly less than that in Group A (DIMS lens group) (P < 0.01). At 6 months post-treatment, in addition to the aforementioned difference, the combination of racemic anisodamine eye drops were significantly more effective in controlling axial elongation compared to the use of DIMS lenses or OK lenses alone (P < 0.01). At the 12-month follow-up, significant differences in axial elongation were observed among the four groups, with Group D (OK lenses combined with racemic anisodamine eye drops) showing the least axial elongation (Table 3).
Comparison of spherical equivalent refractive changes
In the baseline, 3-month, 6-month, and 12-month follow-ups, there were no significant differences in the SER between Group A and Group C (DIMS spectacle lens combined with racemic anisodamine eye drops) (P > 0.05) (Table 4). However, at the 12-month follow-up, a significant difference in the change of SER was observed between the two groups (P < 0.01), with Group C showing a smaller change than Group A. This indicates that the combination of racemic anisodamine eye drops with DIMS spectacle lenses is more effective in controlling myopia progression compared to wearing DIMS spectacle lenses alone (Table 5).
Discussion
This study evaluated the effectiveness of different myopia correction methods in adolescent patients. The results indicated that the use of OK lenses alone was more effective than wearing DIMS spectacle lenses, with the combination of OK lenses and racemic anisodamine eye drops showing the most significant effect in controlling myopia progression. These findings provide important evidence for the development of more effective clinical strategies for myopia prevention and control.
The pathogenesis of myopia is complex. Studies have shown that myopia is not caused by retinal blur, but rather by interference with the eye’s refractive system due to prolonged use of negative lenses (such as myopic glasses) or near work, leading to excessive axial elongation17,18. Negative lenses and near work increase the accommodative load on the eye, gradually altering the ocular shape, ultimately resulting in the onset and progression of myopia19. Both OK lenses and DIMS spectacle lenses are based on the principle of “peripheral myopic defocus” to control myopia progression. This mechanism involves creating myopic defocus in the peripheral retina (focusing light in front of the retina), sending signals to the eye to inhibit axial elongation and thereby slowing myopia progression20. OK lenses work by applying mild pressure to the cornea during overnight wear, reshaping the cornea to flatten the central area and induce myopic defocus in the peripheral region, allowing for clear vision during the day without the need for glasses21. In contrast, DIMS spectacle lenses achieve the myopic defocus effect in the peripheral retina through optical design, without altering the shape of the cornea22. Our study compared the efficacy of OK lenses and DIMS spectacle lenses in controlling myopia progression. After 12 months of patient follow-up, we observed that while both methods effectively slowed myopia progression, OK lenses demonstrated superior performance in controlling axial elongation.
Additionally, pharmacological intervention plays a critical role in myopia prevention and control. Tang et al.23 investigated the long-term efficacy of two combined treatments: low-dose atropine with OK lenses and low-dose atropine with DIMS lenses in Chinese children and adolescents. The results demonstrated that the atropine-OK combination showed superior efficacy in slowing ocular axial elongation and myopia progression. Both combined approaches outperformed monotherapy with low-dose atropine or optical correction alone, emphasizing the clinical value of combination therapies for long-term myopia management. Atropine, a muscarinic cholinergic receptor antagonist24, has been extensively studied and widely applied in myopia control. Low-concentration atropine is associated with relatively fewer side effects25. Racemic anisodamine, also an anticholinergic agent, is widely used in China for the treatment of various conditions, including septic shock and organophosphorus poisoning26,27. The drug exerts its effects by blocking muscarinic cholinergic receptors, resulting in smooth muscle relaxation, improved microcirculation, and antispasmodic properties28. Although research on the ophthalmic applications of racemic anisodamine is limited, its antispasmodic and microcirculation-enhancing properties may hold potential for the ophthalmic treatments. In our study, the treatment group combining racemic anisodamine eye drops with DIMS lenses demonstrated superior control over axial elongation and increases in SER compared to group treated with DIMS lense alone. Furthermore, the combination of OK lenses and racemic anisodamine eye drops showed significantly greater efficacy in controlling ocular axial elongation compared to the combination of DIMS lenses and racemic anisodamine eye drops.
This study has several limitations. First, the observation period was only 12 months, which is relatively short and insufficient to fully assess the long-term effects of different treatments on myopia progression. Second, the relatively small sample size may limit the generalizability of the findings. Third, as a retrospective study, it was not possible to strictly control participants’ daily wearing times and behavioral habits, which could have introduced potential biases in the results. Furthermore, this study included data from both eyes of each subject in the analysis. Future research should adopt an approach that analyzes only one eye per subject to better address the issue of sample duplication. Lastly, the study did not include a high myopia group, which could have provided insights into the efficacy of the treatments in individuals with more severe myopia. Future prospective, large-scale studies are needed to further validate its efficacy and safety.
Conclusion
This study compared the effectiveness of OK lenses, DIMS spectacle lenses, and their respective combinations with racemic anisodamine eye drops in controlling myopia progression in adolescents. The results demonstrated that OK lenses were more effective than DIMS lenses in slowing axial elongation, and the addition of racemic anisodamine eye drops further enhanced the myopia control effect. These findings provide valuable insights for the clinical application of myopia prevention and control strategies.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Baird, P. N. et al. Myopia. Nat. Rev. Dis. Primers. 6(1), 99. https://doi.org/10.1038/s41572-020-00231-4 (2020).
Du, R. et al. Continued increase of axial length and its risk factors in adults with high myopia. JAMA Ophthalmol. 139(10), 1096–1103. https://doi.org/10.1001/jamaophthalmol.2021.3303 (2021).
Biswas, S., Kareh, E. & Qureshi, A. The influence of the environment and lifestyle on myopia. J. Physiol. Anthropol. 43(1), 7. https://doi.org/10.1186/s40101-024-00354-7 (2024).
Tao, L. et al. Correlation between increase of axial length and height growth in Chinese school-age children. Front. Public. Health. 9, 817882. https://doi.org/10.3389/fpubh.2021.817882 (2021).
Chang, L. C., Sun, C. C. & Liao, L. L. Compliance with orthokeratology care among parents of young children in Taiwan. Cont. Lens Anterior Eye. 44(5), 101427. https://doi.org/10.1016/j.clae.2021.02.013 (2021).
Li, H. F. & Mo, J. Myopia and risk factors among Chinese adolescents. Mod. Prev. Med. 48(14), 2552–2557 (2021).
Hiraoka, T. Myopia control with orthokeratology: A review. Eye Contact Lens. 48(3), 100–104. https://doi.org/10.1097/ICL.0000000000000867 (2022).
Zhu, Q. et al. Retardation of myopia progression by multifocal soft contact lenses. Int. J. Med. Sci. 16(2), 198–202. https://doi.org/10.7150/ijms.30118 (2019).
Bullimore, M. A. & Johnson, L. A. Overnight orthokeratology. Cont. Lens Anterior Eye. 43(4), 322–332. https://doi.org/10.1016/j.clae.2020.03.018 (2020).
Banerjee, S. & Horton, J. Lenses and spectacles to prevent myopia worsening in children. CADTH Health Technology Review.
Gardner, D. J., Walline, J. J. & Mutti, D. O. Choroidal thickness and peripheral myopic defocus during orthokeratology. Optometry Vis. Sci. Official Publication Am. Acad. Optometry. 92(5), 579–588. https://doi.org/10.1097/OPX.0000000000000573 (2015).
Chun, R. K. M. et al. Defocus incorporated multiple segments (DIMS) spectacle lenses increase the choroidal thickness: A two-year randomized clinical trial. Eye Vis. (Lond). 10(1), 39. https://doi.org/10.1186/s40662-023-00356-z (2023).
Lee, C. Y. et al. Comparison of myopic control between orthokeratology contact lenses and defocus incorporated multiple segments spectacle lenses. Int. J. Med. Sci. 21(7), 1329–1336. https://doi.org/10.7150/ijms.93643 (2024).
Frcsedin, J. C. Y. F. et al. Low-concentration atropine for myopia progression (LAMP) study: A randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% Atropine Eye drops in Myopia Control—ScienceDirect. Ophthalmology 126(1), 113–124 (2019).
Nucci, P. et al. A comparison of myopia control in European children and adolescents with defocus incorporated multiple segments (DIMS) spectacles, atropine, and combined DIMS/atropine. PLoS One. 18(2), e0281816. https://doi.org/10.1371/journal.pone.0281816 (2023).
Wang, B. et al. Anisodamine affects the pigmentation, mineral density, craniofacial area, and eye development in zebrafish embryos. J. Appl. Toxicol. 5(6), 42 (2022).
Koomson, N. Y. et al. Relationship between reduced accommodative lag and myopia progression. Optom. Vis. Sci. 93(7), 683–691. https://doi.org/10.1097/OPX.0000000000000867 (2016).
Bowrey, H. E. et al. The effect of spectacle lenses containing peripheral defocus on refractive error and horizontal eye shape in the guinea pig. Invest. Ophthalmol. Vis. Sci. 58(5), 2705–2714. https://doi.org/10.1167/iovs.16-20240 (2017).
Medina, A. The cause of myopia development and progression: Theory, evidence, and treatment. Surv. Ophthalmol. 67(2), 488–509. https://doi.org/10.1016/j.survophthal.2021.06.005 (2022).
Lu, W. et al. Different efficacy in myopia control: Comparison between orthokeratology and defocus-incorporated multiple segment lenses. Contact lens Anterior eye: J. Br. Contact Lens Association. 47(2), 102122. https://doi.org/10.1016/j.clae.2024.102122 (2024).
Hiraoka, T. Myopia control with Orthokeratology: A review. Eye Contact lens (2021).
Lam, C. S. Y. et al. Long-term myopia control effect and safety in children wearing DIMS spectacle lenses for 6 years. Sci. Rep. 13(1), 5475. https://doi.org/10.1038/s41598-023-32700-7 (2023).
Tang, T. et al. Comparison of the long-term effects of atropine in combination with orthokeratology and defocus incorporated multiple segment lenses for myopia control in Chinese children and adolescents. Eye 38(9), 1660–1667. https://doi.org/10.1038/s41433-024-02987-5 (2024).
Thomson, K. et al. The role of the serotonergic system in atropine’s anti-myopic effects. Biomed. Pharmacother. 167, 115542. https://doi.org/10.1016/j.biopha.2023.115542 (2023).
Chia, A., Lu, Q. S. & Tan, D. Five-year clinical trial on atropine for the treatment of myopia 2: Myopia control with atropine 0.01% eyedrops. Ophthalmology 123(2), 391–399. https://doi.org/10.1016/j.ophtha.2015.07.004 (2016).
Zhao, T. et al. Beneficial effects of anisodamine in shock involved cholinergic anti-inflammatory pathway. Front. Pharmacol. 2, 23. https://doi.org/10.3389/fphar.2011.00023 (2011).
Eisenkraft, A. & Falk, A. Possible role for anisodamine in organophosphate poisoning. Br. J. Pharmacol. 173(11), 1719–1727. https://doi.org/10.1111/bph.13486 (2016).
Zhang, Y. et al. Update on the sources, pharmacokinetics, pharmacological action, and clinical application of anisodamine. Biomed. Pharmacother. 161, 114522. https://doi.org/10.1016/j.biopha.2023.11452 (2023).
Funding
2021 Chongqing Nanan District Science and Health Joint Medical Research Project (2021-13).
Author information
Authors and Affiliations
Contributions
Conceptualization, Yi Deng and Wen-Jing Ran; methodology, Yi Deng; software, Yi Deng; validation, Jie Gao, and Yu Mei; formal analysis, Yi Deng; investigation, Yi Deng; resources, Yi Deng; data curation, Yi Deng; writing—original draft preparation, Yi Deng; writing—review and editing, Yi Deng and Wen-Jing Ran; visualization, Yi Deng; supervision, Jie Gao, and Yu Mei; project administration, Wen-Jing Ran; funding acquisition, Wen-Jing Ran. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the First Hospital Affiliated to Chongqing Higher School of Medicine and conducted in accordance with the Declaration of Helsinki and clinical practice guidelines. We briefed all participants in detail on the sample collection process, and informed consent to participate was obtained from the parents or legal guardians of any participant under the age of 16, all participants provided written informed consent following the declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Deng, Y., Gao, J., Mei, Y. et al. Effects of racemic anisodamine in combination with orthokeratology and defocus incorporated multiple segment spectacle lenses for myopia control in adolescents. Sci Rep 15, 8781 (2025). https://doi.org/10.1038/s41598-024-84914-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84914-y