Abstract
To establish and validate a novel prognostic model to predict outcomes for intermediate hepatocellular carcinoma (HCC) patients undergoing transarterial chemoembolization (TACE). Clinical data from intermediate-stage HCC patients who underwent TACE between January 2007 and December 2020 were retrospectively analyzed. Patients were divided into a training cohort and a validation cohort. Univariate and multivariate analyses identified risk factors associated with overall survival (OS), leading to the development of a predictive model. The model’s accuracy, consistency, and clinical utility were validated both internally and externally and compared with the Albumin–Bilirubin (ALBI) grading, Platelet–Albumin–Bilirubin (PALBI) grading, Child-Pugh grading, mChild-Pugh grading, and the Model for End-Stage Liver Disease (MELD). A total of 737 intermediate-stage HCC patients were included, with 481 in the training cohort and 256 in the validation cohort. Multivariate analysis identified maximum tumor diameter, tumor number, prealbumin, and total bilirubin as independent factors for OS. A prealbumin–bilirubin (PABI) predictive model was developed. The PABI model’s concordance indices (C-index) in the training and validation cohorts were 0.730 (95% CI 0.701–0.759) and 0.706 (95% CI 0.661–0.751), respectively. The area under the curve (AUC) values at 6, 12, 18, and 24 months in both cohorts were above 0.7. Among the six models, the PABI model had the highest C-index (0.713) and the lowest Akaike information criterion (AIC) value (5897.814) and the best performance in clinical decision curve analysis, suggesting better predictive performance and potential clinical utility. The PABI nomogram model appears to accurately predict survival in intermediate-stage HCC patients treated with TACE, providing clinicians with a valuable tool for candidate selection and prognosis stratification.
Similar content being viewed by others
Introduction
Liver cancer is the sixth most common malignancy globally and ranks third in terms of mortality1. The incidence of liver cancer shows significant geographical variation, with nearly half of new cases occurring in China, where 90% are hepatocellular carcinoma (HCC)1. Epidemiological data indicate that HCC ranks fourth in incidence and second in mortality in China2. Due to the insidious onset of HCC, 70–80% of patients are diagnosed at an intermediate or advanced stage, resulting in poor overall prognosis.
According to the Barcelona Clinic Liver Cancer (BCLC) guidelines3, transarterial chemoembolization (TACE) is recommended as the first-line treatment for intermediate-stage HCC patients who are unsuitable for liver transplantation, have good portal vein flow, low tumor burden, and adequate liver function. However, most HCC patients in China have chronic hepatitis B-related cirrhosis, leading to poor liver reserve function. TACE, while treating tumors, can damage normal liver tissue and impair liver function4,5. Therefore, accurately assessing liver reserve capacity and post-TACE liver damage is crucial for selecting the optimal TACE candidates and prolonging postoperative survival, necessitating the development of precise prognostic models to predict therapeutic outcomes.
While tumor-related factors have traditionally been considered key determinants of prognosis, recent evidence suggests that liver function plays an equally, if not more, critical role in influencing TACE outcomes6,7. This is particularly relevant in the BCLC-B patient population, where liver function can significantly affect the ability to tolerate and respond to TACE.
In our previous work, we developed a comprehensive prognostic model that included a wide array of variables, such as tumor characteristics and general patient factors8. Although this model demonstrated strong predictive performance, its complexity and the inclusion of multiple tumor-related factors made it less practical for routine clinical use, particularly in settings where detailed tumor assessments may not be readily available.
This study aims to establish and validate a novel prognostic model by focusing more on liver function indicators, which are critical determinants of TACE efficacy. By narrowing our scope to include only BCLC stage B patients and simplifying the model to include easily obtainable blood indicators, we seek to enhance the clinical applicability of our findings.
Materials and methods
Study population and case selection
This retrospective study included and analyzed intermediate-stage HCC patients who received conventional TACE (cTACE) as first-line therapy between January 2007 and December 2020 at six centers: the First Affiliated Hospital of Soochow University, Wuxi People’s Hospital, Changzhou No.1 People’s Hospital, Changzhou No.2 People’s Hospital, Nantong First People’s Hospital, and Nantong Tumor Hospital. All included HCC patients were unsuitable for liver resection (LR) or radiofrequency ablation (RFA), and were not candidates for liver transplantation (LT). Treatment decisions were made through discussions by a multidisciplinary team (including interventional radiologists and surgeons). Inclusion criteria were: (1) age 18–75 years; (2) clinical or pathological diagnosis of HCC, with clinical staging of BCLC stage B before treatment; (3) no prior treatments for HCC (transplantation, surgical resection, ablation, TACE, systemic therapy). Exclusion criteria were: (1) other types of malignancies; (2) absolute contraindications for TACE; (3) severe cardiac, cerebral, pulmonary, or renal diseases; (4) missing follow-up data. Patients from the First Affiliated Hospital of Soochow University, Wuxi People’s Hospital, Changzhou No.1 People’s Hospital, and Changzhou No.2 People’s Hospital were included in the training cohort, while patients from Nantong First People’s Hospital and Nantong Tumor Hospital were included in the validation cohort. All methods were carried out in accordance with relevant guidelines and regulations. This study was approved by the Ethics Committee of the First Affiliated Hospital of Soochow University and was conducted in strict accordance with the principles of the Declaration of Helsinki.
Methods and strategies for treatment
TACE procedures were tailored to the patient’s tumor burden, liver function, and physical condition utilizing cTACE techniques. All cTACE procedures were performed by two experienced interventional radiologists via the femoral artery under local anesthesia following the fundamental principles of cTACE, including: (1) superselective catheterization of tumor-feeding arteries using microcatheters; (2) emulsion preparation of lipiodol mixed with doxorubicin (10–40 mg) and oxaliplatin (100–150 mg); (3) embolization endpoints defined as blood flow reduction and contrast clearance ≥ 5 cardiac cycles; (4) embolic agents: gelatin sponge or polyvinyl alcohol (PVA) particles were uniformly used across centers. Specificlly, after percutaneous local anesthesia, a catheter was advanced through the femoral artery to the superior mesenteric artery for indirect portography to assess portal vein patency. Subsequently, the catheter was positioned in the hepatic artery for angiography to evaluate the tumor-feeding arteries. A microcatheter (Progreat, Terumo, Japan or Renegade, Boston Scientific, USA) was then superselectively placed in the proximal tumor-feeding vessels. A lipiodol emulsion was prepared, typically using 10–40 mg of doxorubicin (Pfizer, USA) and 100–150 mg of oxaliplatin (Jiangsu Hengrui Medicine Co., Ltd., China) mixed with lipiodol (Ultra-Fluid, 10 ml/vial, Guerbet, France). The emulsion was slowly injected into the tumor-feeding arteries via the microcatheter, with the specific volume determined based on the patient’s tumor characteristics and liver function, generally not exceeding 20 ml. Additional embolization was performed using an appropriate amount of gelatin sponge particles (Ailikang Medicine Technology Co., Ltd., China) or PVA particles (Ailikang Medicine Technology Co., Ltd., China) until the embolization endpoint was reached. Hepatic arteriography was repeated to ensure complete embolization of the tumor-feeding arteries.
Follow-up and evaluation
On the third day after TACE, patients underwent follow-up complete blood count, liver, kidney, and electrolyte laboratory tests. Subsequent follow-up visits were scheduled at 4–6 weeks post-procedure and then at regular intervals (every 2–3 months) for up to two years, followed by biannual visits. Each follow-up visit included comprehensive laboratory tests and imaging examinations [enhanced computed tomography (CT) or magnetic resonance (MRI)] to monitor tumor response and liver function.
The need for additional TACE treatments was based on on-demand principle, according to tumor progression, residual viable tumor on imaging, or elevated tumor markers. In cases of poor condition or unsuitability for further TACE, systemic therapy or best supportive care (BSC) was provided. Adverse events were monitored throughout the follow-up period.
Follow-up continued until December 31, 2021. The primary endpoint was overall survival (OS), defined as the time from the first TACE treatment to death. For patients still alive at the end of the follow-up period, the endpoint was set as the follow-up cutoff date.
Statistical analysis
Continuous variables were presented as mean ± standard deviation, and categorical variables as frequencies and percentages. Baseline characteristics between the training and validation cohorts were compared using t-tests for continuous variables and χ2 or Fisher’s exact tests for categorical variables. For non-normally distributed data, the Mann-Whitney U test was used. Kaplan–Meier curve was used to calculate median OS, and comparison was performed by log-rank test. Univariate and multivariate Cox regression analyses identified risk factors for OS. Variables with P < 0.05 in the univariate analysis were included in multivariate analysis. Variables with P < 0.05 in the multivariate Cox regression analysis were considered independent risk factors for OS. Statistical analyses were performed using SPSS version 26 (IBM, Armonk, NY), with P-values < 0.05 considered statistically significant.
Construction and validation of the predictive model
Independent risk factors for OS identified through multivariate Cox analysis were used to construct the predictive model using the rms package in R. The model’s accuracy was evaluated by calculating the concordance index (C-index) and plotting time-dependent receiver operating characteristic (ROC) curves with area under the curve (AUC) values at various time points. Model consistency was assessed using Akaike information criterion (AIC) values, and clinical utility was evaluated through decision curve analysis (DCA).
The new model was compared with Albumin–Bilirubin (ALBI), Platelet–Albumin–Bilirubin (PALBI), Child-Pugh, mChild-Pugh, and Model for End-Stage Liver Disease (MELD) grading system in whole sample to determine its predictive power and practical application.
Results
Patients clinical characteristics
A total of 737 intermediate-stage HCC patients treated with cTACE as first-line therapy were included, with 481 in the training cohort and 256 in the validation cohort. No significant differences were found between cohorts in most baseline clinical characteristics, except for liver cirrhosis, ALBI grade, prealbumin, albumin, and total bilirubin (TBIL). (Table 1).
Survival outcomes
By the end of the follow-up period, the median follow-up time for the training cohort was 34.2 months (95% CI 32.0-44.9 months), and 19.8 months (95% CI 18.6–22.8 months) for the validation cohort. In the training cohort, 404 patients had died, and 77 were alive, with a median OS (mOS) of 17.7 months (95% CI 16.7–18.6 months). In the validation cohort, 163 patients had died, and 93 were alive, with a mOS of 16.2 months (95% CI 12.1–19.1 months) (Figure S1).
Cox regression analysis in the training cohort
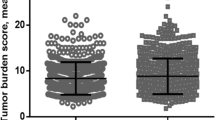
The variables included in the univariate and multivariate Cox regression analyses were selected based on a combination of clinical experience, established clinical guidelines, and published research. Univariate analysis identified ascites, maximum tumor diameter, tumor number, alpha-fetoprotein (AFP), aspartate aminotransferase (AST), prealbumin, albumin, TBIL, (prothrombin time) PT, and lymphocytes as significant factors for OS (P < 0.05). Multivariate analysis determined that maximum tumor diameter, tumor number, prealbumin, and TBIL were independent factors for OS (P < 0.05) (Table 2).
Construction of the predictive nomogram
Based on the results of the multivariate Cox analysis, two readily available laboratory indicators, prealbumin and TBIL, were incorporated for multivariate Cox proportional hazards analysis. The hazard ratios (HR) for prealbumin and TBIL were 0.985 and 1.056, respectively (Table S1), indicating that prealbumin was a protective factor and TBIL was a risk factor for mortality. The prealbumin–bilirubin (PABI) predictive model was constructed based on these hazard ratios and visualized as a nomogram (Fig. 1). Patients were categorized into high-risk and low-risk groups based on their predictive model scores, with Kaplan-Meier curves plotted for both groups(Figure S2). Log-rank test showed a significant difference between the OS of high-risk and low-risk groups [14.6 (95%CI 11.8–17.9) months vs. 20.7 (95%CI 15.1–24.0) months, P < 0.001].
Preliminary validation of the PABI predictive model
Internal and external validation showed that the PABI model’s C-index to be 0.730 (95% CI 0.701–0.759) for the training cohort and 0.706 (95% CI 0.661–0.751) for the validation cohort, indicating good accuracy. The bootstrap method was used to perform 1,000 random samples with replacement in both training and validation cohort, and the time-dependent concordance index curve remained around 0.7 (Figure S3), demonstrating the model’s stability. Time-dependent ROC curves at 6, 12, 18, and 24 months showed AUC values above 0.7, indicating good accuracy at all time points (Fig. 2). Calibration curves at 6, 12, 18, and 24 months showed a high degree of agreement between predicted and observed outcomes (Fig. 3). DCA at 6, 12, 18, and 24 months showed no intersection between the actual and dashed lines, indicating strong clinical applicability (Fig. 4).
Model comparison
The PABI model had the highest C-index (0.713) and the lowest AIC value (5897.814) (Table 3), indicating higher accuracy and consistency among the six models studied. It also showed higher AUC values (Table 3) and stronger clinical applicability at all time points (Fig. 5).
Discussion
Given the heterogeneity among intermediate-stage HCC patients, not all individuals benefit equally from TACE. Identifying appropriate predictive factors and establishing accurate prognostic models can better assist clinicians in selecting potential beneficiaries of TACE treatment. This study found that preoperative serum prealbumin, serum total bilirubin, maximum tumor diameter, and number of tumors are independent factors affecting the survival of intermediate-stage HCC patients treated with TACE. In order to provide a more accessible and practical tool, we developed a nomogram model, PABI, using preoperative serum prealbumin and serum TBIL these two easily obtainable blood indicators. Internal and external validations showed that this PABI model had high predictive accuracy (AUC values > 0.75) at 6, 12, 18, and 24 months, satisfactory calibration, and strong clinical applicability.
Prealbumin as a prognostic marker
Serum prealbumin, also known as transthyretin (TTR), has a shorter half-life (1.9 days) compared to albumin (21 days)9. This makes it less likely to be rapidly replenished through intravenous infusion in clinical settings, allowing it to more sensitively reflect the liver’s synthetic and reserve functions. Several studies have linked low prealbumin levels with postoperative complications in various tumors10,11. Recent research indicates that malnutrition is a significant prognostic factor for HCC patients12. However, due to the pathophysiological issues of cirrhosis leading to hypoalbuminemia, some researchers argue that albumin is unsuitable for predicting HCC prognosis. They found that serum prealbumin could serve as a novel prognostic biomarker for HCC patients13. A meta-analysis by Qiao et al. found that low serum prealbumin levels were adverse prognostic factors for OS and recurrence-free survival (RFS) in HCC patients14. Another multicenter study in China demonstrated that preoperative serum prealbumin levels could predict recurrence and mortality in HCC patients undergoing hepatectomy15. Wen et al. stratified Child-Pugh grade A patients based on prealbumin levels, resulting in an improved Child-Pugh classification that better predicted outcomes for HCC patients undergoing radical resection16. Additionally, our previous study mentioned above identified prealbumin as the only blood marker with an independent impact on survival outcomes in patients with unresectable HCC undergoing TACE (> 170 mg/L vs. ≤170 mg/L, HR = 0.71, 95% CI 0.56–0.91, P = 0.006)8. This reinforces the critical role of prealbumin in prognostic models for HCC patients treated with TACE. Despite the limited research in this area, our findings underscore the importance of incorporating prealbumin into predictive models for survival outcomes in these patients.
Role of total bilirubin
Total bilirubin, the sum of indirect and direct bilirubin, often shows abnormal levels in hepatic cell damage or biliary obstruction. High serum total bilirubin levels have been associated with increased mortality in cancer cachexia patients. Numerous studies have used serum total bilirubin as a predictive factor in various prognostic models17. Some researchers argue that direct bilirubin is a better predictor than total bilirubin for patient prognosis18,19. Young et al. found that direct bilirubin had a stronger predictive ability for complications and overall survival in TACE-treated patients compared to total bilirubin (AIC = 941.19 vs. 1000.51 for OS; AIC = 352.22 vs. 357.42 for postoperative complications)20. Another study on cirrhotic patients found that direct bilirubin had a higher AUC value for predicting six-month mortality, leading to the development of the DB-MELD model, which showed improved predictive ability21. However, our study only analyzed total bilirubin and did not collect data on direct bilirubin, warranting further research on its prognostic application in TACE-treated intermediate-stage HCC patients.
Comparison with other models
Child-Pugh classification is widely used for assessing liver function but has limitations due to its subjective criteria. Similar to Liu et al.'s findings22, our study showed that Child-Pugh classification had a relatively lower C-index (0.525) and higher AIC value (6101.260), with lower AUC values at 6, 12, 18, and 24 months, indicating weak predictive ability for TACE-treated HCC patients.
Wen et al. improved the Child-Pugh classification by excluding subjective criteria like ‘hepatic encephalopathy’ and ‘ascites’ and incorporating prealbumin, an independent risk factor for HCC prognosis post-surgery, leading to the mChild-Pugh classification16. However, compared to the PABI model, the mChild-Pugh classification had a lower C-index (0.593 vs. 0.713) and higher AIC value (6081.955 vs. 2897.814), with AUC values decreasing over time, indicating that mChild-Pugh classification was less effective for early prognosis prediction in TACE-treated HCC patients. The main reason might be that the mChild-Pugh classification was designed for predicting outcomes in early-stage HCC patients undergoing surgical resection, who generally have less severe albumin depletion compared to intermediate-stage HCC patients undergoing TACE.
Since the introduction of the ALBI score in 2014, its ability to assess liver function and stratify prognosis in HCC patients has been validated in multiple studies23,24. However, the ALBI grading has limitations. Firstly, the calculation of the ALBI score is relatively complex, making it difficult to quickly grade liver function in HCC patients in clinical practice. Secondly, preoperative short-term interventions such as blood transfusion or intravenous human albumin supplementation can increase serum albumin levels in HCC patients, affecting the accuracy of liver function assessment based on the ALBI score25.
The PALBI classification, developed by Roayaie et al. by incorporating platelet count into the ALBI grade to account for portal hypertension26, showed contradictory roles of platelets in HCC progression. Platelets can promote HCC tumor growth through secretion of serotonin, vascular endothelial growth factor (VEGF), and platelet-derived growth factor (PDGF) and can enhance angiogenesis and metastasis27,28. However, due to factors like portal hypertension, cirrhotic and HCC patients often have low platelet counts, which could lead to poor prognosis29. Despite this, PALBI classification had lower C-index and higher AIC values compared to the PABI model, and platelets were not an independent prognostic factor for TACE-treated HCC patients in our multivariate analysis. Pang et al. found that PALBI was effective in distinguishing survival in HCC patients without thrombocytopenia but not in those with thrombocytopenia30. This may explain why PALBI classification had weaker predictive ability compared to the PABI model in our study.
The MELD score, developed by Malinchoc et al. in 2000 to predict liver reserve and postoperative mortality in cirrhotic patients undergoing transjugular intrahepatic portoystemic shunt (TIPS)31, is less reliable for predicting HCC prognosis since not all HCC patients have cirrhosis32. In our study, half of the patients did not have cirrhosis, and ‘creatinine’ and ‘INR’, included in the MELD calculation, were not strong prognostic factors for TACE-treated HCC patients. Consequently, MELD had the lowest C-index (0.500) and highest AIC value (6115.499), with poor AUC values at all time points.
Our study focused on OS rather than PFS because OS is based on death events, while PFS is based on tumor assessments. We were more concerned with postoperative survival rather than tumor response. In summary, the PABI model outperformed existing models in predicting survival in intermediate-stage HCC patients undergoing TACE, highlighting its potential for clinical application. While the PABI model provides an objective prognostic foundation, its clinical value lies in synergistic use with standard staging systems and clinician judgment. Threshold-free interpretation avoids oversimplification, while serial measurements enable dynamic risk assessment—a critical advantage in managing this heterogeneous patient population.
Limitations
First, the sample size was relatively small, leading to uneven distribution among different liver function grades. Second, as a retrospective study, it was subject to selection bias and other limitations. Third, the model was specifically applicable to intermediate-stage HCC patients undergoing TACE and may not be suitable for those receiving combined treatments or in early stages. Furthermore, the impact of post-TACE therapies on survival could not be fully stratified due to their variability. Future studies should prospectively record and standardize subsequent treatments to refine prognostic models.’
Future directions
Although the PABI model performed consistently across eras, its applicability to patients treated with newer TACE technologies or combination therapies requires validation in contemporary cohorts. Future studies should include more HCC patient data for further model analysis and improvement. Additionally, the combination with imaging biomarkers (e.g., CT/MRI radiomics) may further improve stratification, particularly for heterogeneous tumors. More liver function classifications should be included for comparison, analysis, and improvement. Finally, the model should be validated in more external centers to evaluate its generalizability.
Conclusion
In conclusion, the PABI model developed in this study provides a superior predictive tool for assessing survival in intermediate-stage HCC patients undergoing TACE. By incorporating readily available and reliable clinical indicators, the PABI model outperforms existing liver function assessment models, demonstrating higher accuracy, better calibration, and stronger clinical utility. This model offers significant potential for improving patient selection and individualized treatment planning, ultimately enhancing clinical outcomes. Further validation in diverse patient cohorts and clinical settings is warranted to confirm its generalizability and robustness.
Data availability
All data applied in this study are presented in this article. Further enquiries can be directed to the corresponding authors.
Abbreviations
- TACE:
-
Transarterial chemoembolization
- cTACE:
-
Conventional transarterial chemoembolization
- HCC:
-
Hepatocellular carcinoma
- BCLC:
-
Barcelona clinic liver cancer
- ALBI:
-
Albumin–Bilirubin
- CR:
-
Complete response
- PR:
-
Partial response
- SD:
-
Stable disease
- PD:
-
Progressive disease
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- ORR:
-
Objective response rate
- DCR:
-
Disease control rate
- AEs:
-
Adverse events
- C-index:
-
concordance index
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- AIC:
-
Akaike information criterion
- DCA:
-
Decision curve analysis
- CT:
-
Computed tomography
- MR:
-
Magnetic resonance
- mRECIST:
-
Modified response evaluation criteria in solid tumors
- ECOG:
-
Eastern cooperative oncology group
- DEB-TACE:
-
Drug-eluting bead transarterial chemoembolization
- AFP:
-
Alpha-fetoprotein
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- TBIL:
-
Total bilirubin
- PT:
-
Prothrombin time
- WBC:
-
White blood cell
- HR:
-
Hazard ratio
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74 (3), 229–263 (2024).
Zheng, R. S. et al. [Cancer incidence and mortality in China, 2022]. Zhonghua Zhong Liu Za Zhi. 46 (3), 221–231 (2024).
Reig, M. et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 76 (3), 681–693 (2022).
Lu, W. et al. A comparative study of damage to liver function after TACE with use of low-dose versus conventional-dose of anticancer drugs in hepatocellular carcinoma. Hepatogastroenterology 54 (77), 1499–1502 (2007).
Xiang, H. et al. Comparison of liver function and safety in hepatocellular cancer patients treated with DEB-TACE and cTACE: A multi-center, retrospective cohort study. Transl Cancer Res. 8 (5), 1950–1964 (2019).
Eltawil, K. M., Berry, R., Abdolell, M. & Molinari, M. Quality of life and survival analysis of patients undergoing transarterial chemoembolization for primary hepatic malignancies: A prospective cohort study. HPB (Oxford). 14 (5), 341–350 (2012).
Labeur, T. A., Takkenberg, R. B., Klumpen, H. J. & van Delden, O. M. Reason of discontinuation after transarterial chemoembolization influences survival in patients with hepatocellular carcinoma. Cardiovasc. Intervent Radiol. 42 (2), 230–238 (2019).
Xu, L. et al. Development and validation of a prognostic model for transarterial chemoembolization in unresectable hepatocellular carcinoma based on preoperative serum prealbumin. J. Hepatocell Carcinoma. 10, 2239–2250 (2023).
Ingenbleek, Y. & Young, V. Transthyretin (prealbumin) in health and disease: Nutritional implications. Annu. Rev. Nutr. 14, 495–533 (1994).
Song, S. et al. Low preoperative serum prealbumin levels and risk of postoperative complications after transsphenoidal surgery in nonfunctioning pituitary adenoma. Neurosurg. Focus. 53 (6), E6 (2022).
Zhou, J. et al. Role of prealbumin as a powerful and simple index for predicting postoperative complications after gastric cancer surgery. Ann. Surg. Oncol. 24 (2), 510–517 (2017).
Schutte, K. et al. Malnutrition is a prognostic factor in patients with hepatocellular carcinoma (HCC). Clin. Nutr. 34 (6), 1122–1127 (2015).
Shimura, T. et al. Clinical significance of serum transthyretin level in patients with hepatocellular carcinoma. ANZ J. Surg. 88 (12), 1328–1332 (2018).
Qiao, W. et al. Prognostic value of prealbumin in liver cancer: A systematic review and meta-analysis. Nutr. Cancer. 72 (6), 909–916 (2020).
Li, J. D. et al. Association between preoperative prealbumin level and postoperative mortality and morbidity after hepatic resection for hepatocellular carcinoma: A multicenter study from a HBV-endemic area. Am. J. Surg. 221 (5), 1024–1032 (2021).
Wen, X. et al. Integration of prealbumin into Child-Pugh classification improves prognosis predicting accuracy in HCC patients considering curative surgery. J. Clin. Transl Hepatol. 6 (4), 377–384 (2018).
Li, X. R. et al. Association of serum total bilirubin with survival outcomes in patients with cancer cachexia: A prospective, multicenter cohort study. Nutrition 102, 111711 (2022).
Yokoyama, Y. et al. Predictive power of prothrombin time and serum total bilirubin for postoperative mortality after major hepatectomy with extrahepatic bile duct resection. Surgery 155 (3), 504–511 (2014).
Jia, Z. et al. The prognostic value of serum bilirubin in colorectal cancer patients with surgical resection. Int. J. Biol. Markers. 36 (2), 825645024 (2021).
Young, S., Sanghvi, T., Lake, J. J., Rubin, N. & Golzarian, J. Predicting post-transarterial chemoembolization outcomes: A comparison of direct and total bilirubin serums levels. Diagn. Interv Imaging. 101 (6), 355–364 (2020).
Lee, H. A. et al. Direct bilirubin is more valuable than total bilirubin for predicting prognosis in patients with liver cirrhosis. Gut Liver. 15 (4), 599–605 (2021).
Liu, Y. et al. Comparison of modified Child-pugh (MCP), Albumin-bilirubin (ALBI), and Child-pugh (CP) score for predicting of survival in hepatocellular carcinoma patients treated with transcatheter arterial chemoembolization. Bull. Cancer. 108 (10), 931–939 (2021).
Johnson, P. J. et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade. J. Clin. Oncol. 33 (6), 550–558 (2015).
Toyoda, H. & Johnson, P. J. The ALBI score: From liver function in patients with HCC to a general measure of liver function. JHEP Rep. 4 (10), 100557 (2022).
Devoto, G. et al. Prealbumin serum concentrations as a useful tool in the assessment of malnutrition in hospitalized patients. Clin. Chem. 52 (12), 2281–2285 (2006).
Roayaie, S. et al. PALBI - An objective score based on platelets, albumin & bilirubin stratifies HCC patients undergoing resection & ablation better than child’s classification. Hepatology 62, 631A–632A (2015).
Zuo, X. et al. 5-hydroxytryptamine receptor 1D aggravates hepatocellular carcinoma progression through FoxO6 in AKT-dependent and independent manners. Hepatology 69 (5), 2031–2047 (2019).
Carr, B. I. et al. Platelet extracts induce growth, migration and invasion in human hepatocellular carcinoma in vitro. BMC Cancer. 14, 43 (2014).
Liu, P. H. et al. Thrombocytosis is associated with worse survival in patients with hepatocellular carcinoma. Liver Int. 40 (10), 2522–2534 (2020).
Pang, Q. et al. The significance of platelet-albumin-bilirubin (PALBI) grade in hepatocellular carcinoma patients stratified according to platelet count. Cancer Manag Res. 12, 12811–12822 (2020).
Malinchoc, M. et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31 (4), 864–871 (2000).
Ho, S. Y. et al. Prognostic performance of ten liver function models in patients with hepatocellular carcinoma undergoing radiofrequency ablation. Sci. Rep. 8 (1), 843 (2018).
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Contributions
N.J. performed the data analysis and wrote the manuscript. Y.Z. performed the data analysis. S.Z. performed the data curation and validation. B.Z. provided resources. J.Y., W.L., Y.Y. and M.L. supervised the project. J.S., Z.L. and X.Z. reviewed and edited the manuscript. C.N. conceptualized the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Ethics approval
This study is a retrospective analysis utilizing clinical data from the hospital’s medical records system. No patient images, radiological data, or personally identifiable information were used in the study. Therefore, based on the nature of the research, the need to obtain the informed consent was waived by the Ethics Committee of the First Affiliated Hospital of Soochow University.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiang, N., Zhan, Y., Zhang, S. et al. Development and validation of a prealbumin–bilirubin model for prognostic prediction in intermediate hepatocellular carcinoma undergoing transarterial chemoembolization. Sci Rep 15, 18147 (2025). https://doi.org/10.1038/s41598-025-02960-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02960-6