Abstract
The principal aim of this study was to present a novel approach to manipulative repositioning for the management of anterior shoulder dislocation. This was evaluated in comparison with the established repositioning method to ascertain its clinical efficacy. Seventy-six patients with anterior dislocation of the shoulder joint were randomly assigned to one of two groups. Each group underwent reducing using either Tang’s method or Hippocrates’ method, respectively. The patients were then monitored for six months. The researchers analyzed and compared the general condition, reduction time, reduction success rate, VAS score, and ASES score of the patients in the two groups. No statistically significant difference was observed in the general condition of the patients prior to the reduction between the two groups. The mean reduction time for the Tang’s method group (70.9 ± 11.88) was found to be significantly shorter than that observed for the Hippocrates method group (411.6 ± 50.41). The reduction success rate was significantly higher in the Tang’s method group (100.00%) than in the Hippocrates method group (80.56%). No statistically significant difference was observed in VAS scores between the two groups prior to the reduction. However, the Tang’s method group demonstrated superior outcomes compared to the Hippocrates method group during and following the reduction. No statistically significant difference was observed in ASES scores between the two groups prior to the reduction. However, at one, three, and six months post-reduction, the Tang’s method group exhibited significantly superior outcomes compared to the Hippocrates method group. The Tang’s method is a safe and effective method of reducing for anterior dislocation of the shoulder. It is significantly superior to the traditional Hippocrates method.
Similar content being viewed by others
Introduction
External violence has the potential to cause dislocation of various joints in the human body. Among these, shoulder dislocation is the most common, with an estimated incidence rate of 25.62 to 25.97 per 100,000 persons per year1,2. Among shoulder dislocations, anterior shoulder dislocation is the most prevalent. A review of relevant studies indicates that anterior shoulder dislocation accounts for over 90% of all shoulder dislocations3,4. The shoulder joint is characterised by a distinctive structural configuration, comprising a sizable humeral head and a relatively shallow glenoid fossa. This is encased in a loose capsule, which impairs stability and renders the joint susceptible to dislocation in response to a sudden, high-energy impact5,6. The majority of patients present with clinical manifestations including shoulder swelling and pain, accompanied by limitations in limb movement7. Additionally, they exhibit a square shoulder deformity, as well as shoulder joint emptiness. The affected side of the inner elbow is unable to be tightly pressed against the chest wall, and the upper limb is unable to be carried on the shoulder8. In the absence of complex fractures and serious soft tissue injuries, the primary treatment method for shoulder dislocation is manipulation9. However, there are numerous techniques for reducing the shoulder, and regardless of the reduction method employed, the objective is to “return to the original position"10. The most common reduction method is the Hippocrates method. However, this traditional and classic method has many shortcomings, including a long reduction time, a painful process, and a low success rate11. The objective is to restore the normal anatomical structure of the shoulder in a simple, safe and expeditious manner, while simultaneously relieving the patient’s discomfort and enhancing functionality. We have devised a novel approach to treating anterior dislocation of the shoulder joint, drawing upon a range of established techniques for repositioning the joint. Our method, which we have designated Tang’s method, builds upon the strengths of existing techniques while addressing their limitations. The Tang’s technique is an efficacious method of reducing pain and improving shoulder function in patients. To further assess the clinical efficacy of this reduction method, we conducted a prospective study comparing it to the traditional Hippocrates method.
Methods
Case information
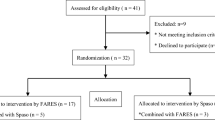
Patients with anterior dislocation of the shoulder admitted to the outpatient and emergency clinic of Suzhou Hospital of Anhui Medical University from February 2021 to February 2023 were randomly assigned to one of two groups (A and B) using a double-blind approach. A random number is generated for each patient using a computer program, with the number representing group A if it is odd and group B if it is even. Group A was reduced using the Tang’s method, while group B was reduced using the Hippocrates method. All patients were informed of the nature of the study and provided written informed consent. A total of 76 patients were included in this study. The study was approved by the Ethics Committee of Cebu Hospital of Anhui Medical University (Ethical Review Comment No.: C2021010). All patients were informed about the study and signed an informed consent form. The research was performed in accordance with the Declaration of Helsinki.
Inclusion and exclusion criteria
Inclusion criteria: (1) A clear history of trauma; (2) Shoulder swelling and pain with activity limitation; (3) A sensation of emptiness is experienced in the shoulder joint; (4) A positive Dugas test; (5) An X-ray examination to confirm diagnosis.
Exclusion criteria: (1) Individuals with serious cardiovascular and cerebrovascular diseases, as well as those with associated complications; (2) Mental anomalies that prevent cooperation with repositioning of patients; (3) The patient presented with a complex injury pattern, including multiple fractures and severe soft tissue injuries that necessitated surgical intervention.
Reduction methods
Following diagnosis, patients who met the inclusion criteria for the study and consented to participate were randomly assigned to one of two study groups using a computerized randomization process. Neither the patients nor the surgeons were privy to the specifics of the dislocation treatment plan until the patients provided their informed consent. The procedure of shoulder reduction was carried out by the same physician for all patients.
Tang’s method: To illustrate, consider the case of a right shoulder dislocation. The patient is positioned on the side of the examination bed, while the operator stands on the same side as the patient’s injured limb. The affected limb is extended at the elbow. The operator’s left knee is firmly pressed against the affected limb’s armpit, the left hand is placed on the affected limb’s shoulder, and the right hand holds the affected limb’s wrist and applies traction as needed. Then, the operator slowly rotates and abducts the affected limb while the knee gradually pushes upward against the armpit, and the head of the humerus is slipped into the glenoid of the joint, indicating that the reduction has been successful. A subsequent examination should be conducted to ascertain whether the Dugas sign has undergone a reversal from positive to negative. The aforementioned reduction process is illustrated in Fig. 1A–C.
Hippocrates method: the patient lies supine, the operator stands on the affected side of the bed, the heel of the same side is placed in the patient’s axilla against the chest wall, both hands hold the affected limb in the outer booth for freehand traction, and the heel is pressed against the axilla as a counter-traction force. In the case of a left shoulder dislocation, the operator utilizes the left foot. Conversely, when a right shoulder dislocation occurs, the right foot is employed. It is essential that the traction be continuous and that the force be even. Following the application of traction for a designated period, the shoulder muscles will gradually relax. At this juncture, the upper limb will undergo an internal retraction and internal rotation, allowing the head of the humerus to slide into the scapula through the breach of the joint capsule in front. This process is accompanied by a popping and rattling sound, which serves as an indicator of successful reduction. Subsequently, the Dugas sign will be reassessed, and a change from positive to negative should be noted. The reduction process is illustrated in Fig. 1D–F.
In cases where manual reduction was unsuccessful, the patients were reduced under anesthesia. A subsequent radiographic examination was performed on all patients who had undergone reducing to confirm the efficacy of the procedure. Figure 2 illustrates the radiographs obtained prior to and following the dislocation of the shoulder joint.
Post-reduction processing
Following a successful reduction, the affected shoulder is suspended and fixed with a forearm sling in the position of internal rotation for a period of 2–3 weeks. During this period of fixation with the forearm sling, active wrist and hand functional exercises are carried out. Rehabilitation exercises were conducted on the affected shoulder at designated intervals following the cessation of immobilization, with the objective of facilitating the recovery of shoulder joint function. Furthermore, the same investigator conducted periodic follow-up visits with the patients.
Evaluation indicators
The success rate of reduction, the time required for reducing, the visual analog scale (VAS) scores obtained before, during, and after reducing, and the American Shoulder and Elbow Surgeons (ASES) scores of the shoulder joints before and one month, three months, and six months after reducing were documented for both groups.
Statistical methods
All data analysis and graphical production for this study were conducted using GraphPad Prism 9.4.1 software. The quantitative data were subjected to one-way ANOVA analysis, while the qualitative data were analysed using the X² test. The repeated measures data were analysed using two-way ANOVA. P < 0.05 was deemed to indicate a statistically significant difference.
Results
A total of 76 patients were included in the study, comprising 39 males and 37 females with an age range of 18 to 80 years. The statistical results of the basic information of each group before reset are presented in Table 1. The analysis revealed no statistically significant difference in the general conditions of the patients in the two groups.
The statistical results pertaining to the reduction time and reduction success rate of the two reduction methods are presented in Table 2. The mean reduction time was 70.9 ± 11.88 s for the Tang’s method and 411.6 ± 50.41 s for the Hippocrates method, indicating a statistically significant difference between the two methods (Fig. 3A). The time required for reducing can influence the patient’s treatment experience. Rapid reduction has the potential to significantly lessen the patient’s discomfort, suggesting that Tang’s method may offer a more comfortable treatment experience compared to Hippocrates’ method. Furthermore, the success rates of the two maneuvers were calculated, yielding 40/40 (100.00%) for Tang’s method and 29/36 (80.56%) for Hippocrates’ method. The difference between the two was statistically significant (Fig. 3B). These findings suggest that Tang’s method outperforms the conventional Hippocrates method in terms of reduction success rate.
To more accurately assess the efficacy of Tang’s method for treating shoulder dislocation, we recorded the patients’ shoulder VAS scores at three distinct time points: before, during, and after the reduction procedure. Additionally, we conducted regular follow-ups for a period of six months to document the patients’ ASES scores for the affected shoulder joint. The results of the VAS and ASES scores for patients in both groups are presented in Table 3. No statistically significant difference was observed in VAS scores between the two groups of patients pre-reduction. However, the VAS scores of patients in the Tang’s group were significantly lower than those of patients in the Hippocrates group intra-reduction and post-reduction (Fig. 4A–C). This indicates that the Tang’s reduction method is more gentle, which helps to minimize secondary injuries due to repositioning. There was no statistically significant difference in the ASES scores of the shoulder joints between the two groups pre-reduction. However, the patients in the Tang’s group exhibited superior outcomes compared to the Hippocrates group at the one-month, three-month, and six-month follow-up periods following reduction (Fig. 4D–F). This indicates that Tang’s method of reduction for anterior dislocation of the shoulder joint is more conducive to patient recovery. The aforementioned results indicate that Tang’s method is a practical and effective approach for the treatment of anterior dislocation of the shoulder joint.
Discussion
The shoulder joint is the most mobile joint in the human body, and therefore the most prone to dislocation. Indeed, shoulder dislocation accounts for approximately 50% of all dislocation of large joints in the human body12,13. In addition to the joint capsule, the shoulder joint is surrounded by a number of muscle groups, including the deltoid and pectoralis major, as well as a multitude of ligaments14. These structures serve to stabilise the joint. Despite the presence of a substantial amount of soft tissue between the glenoid of the scapula and the head of the humerus, the glenoid is relatively small and shallow, while the head of the humerus is large and rounded. This configuration renders the shoulder joint highly instable15. The tissues situated beneath the anterior aspect of the shoulder joint are characterised by reduced tensile strength, while the joint capsule displays a relatively lax structure. Consequently, the likelihood of a shoulder dislocation occurring when an external force is applied is increased. Shoulder dislocation has a significant impact on patients’ quality of life due to the severe pain associated with the condition16. Therefore, it is crucial to perform reduction procedures as soon as possible to restore the normal anatomical structure and prevent the potential for muscle, nerve, and blood vessel injuries caused by prolonged dislocation of the humeral head8,17,18. There are numerous traditional methods of reducing dislocated shoulders, with the most commonly used techniques in clinical settings including the Matsen, Hippocrates, Kocher, Stimson, and Milch methods19,20. Irrespective of the method employed, its underlying principle can be distilled into three fundamental principles: lever mechanics, traction mechanics, and gravity mechanics13,21. Each of these methods has certain inherent limitations. The Matsen and Hippocrates methods are associated with an increased risk of brachial plexus injuries, humeral trunk or neck fractures, and other complications. The Kocher method has been linked to an elevated incidence of humeral trunk and neck fractures, joint capsule and vascular injuries. The Stimson method often necessitates the application of a considerable degree of force, which can be uncomfortable and painful for the patient in the absence of anaesthetic intervention. The application of traction may result in an increased risk of muscle spasm22,23. The Milch method is comparatively safe and free of complications when compared to the aforementioned techniques. However, its success rate is 69.23%, with the modified Milch method demonstrating an improved success rate24.
Manipulation represents the primary method of treatment for shoulder dislocation25. Based on the principles of traditional manipulation and a synthesis of anatomical and biological characteristics, we have devised a new technique, the knee-to-elbow extension, external rotation, and abduction manipulation. The fundamental principle underlying this technique is as follows: Appropriate traction exerted by the extended elbow’s external rotation and adduction relaxes the damaged muscle groups surrounding the shoulder joint and the joint capsule fissure, thereby facilitating the unlocking of the embedded biceps tendon. Subsequently, the knee joint of the operator serves as the fulcrum, while the upper limb functions as the arm of the force, facilitating the displacement of the head of the humerus in the anterior and inferior regions of the glenoid articular surface. Given the absence of responsive ligaments and muscles in these areas, a relatively minimal force can achieve the reduction of the head of the humerus26. It is imperative to consider the patient’s age and bone quality prior to reduction. The simple lever principle reduction method is contraindicated for elderly osteoporotic patients, as it may potentially result in medically induced fractures27. In this study, none of the patients who underwent reducing using the Tang’s method experienced a medically induced fracture. This method effectively utilizes lever and traction mechanics. As the operator does not need to exert a significant force during the reduction, the pulling effect of the adductor muscle group and the blocking effect of the biceps muscle can be reduced, thereby enabling a reduction that is comparable to that under anesthesia.
Tang’s method offers several advantages. Primarily, it can be performed by a single individual, which reduces the need for anaesthesia and other medical interventions. Additionally, the procedure is relatively straightforward, with a short reduction time and a high success rate. Furthermore, it causes minimal discomfort and fewer complications, resulting in less damage to surrounding tissues. Finally, the method allows for good joint mobility after reduction, which often leads to satisfactory functional recovery.
The rapid, safe, and effective reduction for patients is a common objective among orthopedic surgeons. The limitations of this empirical study are as follows: (1) The sample size is relatively small, which may introduce some bias into the results; (2) There is a lack of long-term efficacy evaluation. In the near future, we will conduct a multi-faceted study in conjunction with several orthopedic centers in our region to collect a large sample of cases, with the aim of further confirming the clinical value of Tang’s reduction method.
In conclusion, Tang’s method of treating anterior dislocation of the shoulder joint is a simple and straightforward technique that can be easily performed to avoid secondary injury. It has been demonstrated to be highly effective in reducing dislocation, and its clinical efficacy and safety have been established. Furthermore, this method has been shown to facilitate functional recovery of the shoulder joint, making it a valuable addition to the clinical toolkit for managing this condition. Further studies will be conducted to identify additional effective methods to enhance the success rate of reduction.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Szyluk, K. et al. Shoulder dislocation incidence and risk factors-rural vs urban populations of Poland. Int. J. Environ. Res. Public. Health. https://doi.org/10.3390/ijerph191911857 (2022).
Nazzal, E. M. et al. First-time traumatic anterior shoulder dislocation: current concepts. J. ISAKOS. 8, 101–107. https://doi.org/10.1016/j.jisako.2023.01.002 (2023).
Kroner, K., Lind, T. & Jensen, J. The epidemiology of shoulder dislocations. Arch. Orthop. Trauma. Surg. 108, 288–290. https://doi.org/10.1007/BF00932317 (1989).
Goth, A. P. et al. Traumatic anterior shoulder dislocation: epidemiology, diagnosis, and treatment. Dtsch. Arztebl Int. https://doi.org/10.3238/arztebl.m2024.0254 (2025).
Lv, H. et al. National incidence of joint dislocation in China: a retrospective survey of 512,187 individuals. Chin. Med. J. (Engl). 135, 1742–1749. https://doi.org/10.1097/CM9.0000000000002253 (2022).
Luckenbill, D. B. et al. Biomechanical evaluation of recurrent dissociation of modular humeral prostheses. Bioengineering (Basel). https://doi.org/10.3390/bioengineering9020076 (2022).
Kearney, R. S. et al. Acute rehabilitation following traumatic anterior shoulder dislocation (ARTISAN): pragmatic, multicentre, randomised controlled trial. BMJ 384, e076925. https://doi.org/10.1136/bmj-2023-076925 (2024).
Atef, A., El-Tantawy, A., Gad, H. & Hefeda, M. Prevalence of associated injuries after anterior shoulder dislocation: a prospective study. Int. Orthop. 40, 519–524. https://doi.org/10.1007/s00264-015-2862-z (2016).
Gonai, S., Miyoshi, T., da Silva Lopes, K. & Gilmour, S. An umbrella review of systematic reviews and meta-analyses for assessment and treatment of acute shoulder dislocation. Am. J. Emerg. Med. 87, 16–27. https://doi.org/10.1016/j.ajem.2024.09.060 (2025).
Hawkins, R. J. & Belle, R. M. Posterior instability of the shoulder. Instr Course Lect. 38, 211–215 (1989).
Bose, S., Ambade, R., Bhartiya, Y. & Velagala, V. R. Applications of latissimus dorsi grafts in reverse shoulder arthroplasty. Cureus 15, e48469. https://doi.org/10.7759/cureus.48469 (2023).
Hutyra, C. A., Smiley, S., Taylor, D. C., Orlando, L. A. & Mather, R. C. 3rd. Efficacy of a Preference-Based decision tool on treatment decisions for a First-Time anterior shoulder dislocation: A randomized controlled trial of At-Risk patients. Med. Decis. Mak. 39, 253–263. https://doi.org/10.1177/0272989X19832915 (2019).
Dong, H., Jenner, E. A. & Theivendran, K. Closed reduction techniques for acute anterior shoulder dislocation: a systematic review and meta-analysis. Eur. J. Trauma. Emerg. Surg. 47, 407–421. https://doi.org/10.1007/s00068-020-01427-9 (2021).
Kibler, W. B., Sciascia, A. D. & Grantham, W. J. The shoulder joint complex in the throwing motion. J. Shoulder Elb. Surg. 33, 443–449. https://doi.org/10.1016/j.jse.2023.06.031 (2024).
Iannotti, J. P., Gabriel, J. P., Schneck, S. L., Evans, B. G. & Misra, S. The normal glenohumeral relationships. An anatomical study of one hundred and Forty shoulders. J. Bone Joint Surg. Am. 74, 491–500 (1992).
Damani, A. et al. Imaging for patients presenting with a painful shoulder. Br. J. Hosp. Med. (Lond). 84, 1–10. https://doi.org/10.12968/hmed.2023.0058 (2023).
Braun, C. & McRobert, C. J. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database Syst. Rev. 5, CD004962. https://doi.org/10.1002/14651858.CD004962.pub4 (2019).
Guler, O. et al. Comparison of four different reduction methods for anterior dislocation of the shoulder. J. Orthop. Surg. Res. https://doi.org/10.1186/s13018-015-0226-4 (2015).
Sayegh, F. E. et al. Reduction of acute anterior dislocations: a prospective randomized study comparing a new technique with the hippocratic and Kocher methods. J. Bone Joint Surg. Am. 91, 2775–2782. https://doi.org/10.2106/JBJS.H.01434 (2009).
Eachempati, K. K., Dua, A., Malhotra, R., Bhan, S. & Bera, J. R. The external rotation method for reduction of acute anterior dislocations and fracture-dislocations of the shoulder. J. Bone Joint Surg. Am. 86, 2431–2434. https://doi.org/10.2106/00004623-200411000-00011 (2004).
Fennelly, J. T. et al. A systematic review of pre-hospital shoulder reduction techniques for anterior shoulder dislocation and the effect on patient return to function. Chin. J. Traumatol. 23, 295–301. https://doi.org/10.1016/j.cjtee.2020.08.003 (2020).
Amar, E. et al. Milch versus Stimson technique for nonsedated reduction of anterior shoulder dislocation: a prospective randomized trial and analysis of factors affecting success. J. Shoulder Elb. Surg. 21, 1443–1449. https://doi.org/10.1016/j.jse.2012.01.004 (2012).
Risan, H. K., Serhan, F. M. & Al-Azzawi, A. A. Management of a typical experiment in engineering and science. AIP Conf. Proc. 2864 (2024). https://doi.org/10.1063/5.0186079
Sapkota, K., Shrestha, B., Onta, P. R. & Thapa, P. Comparison between external rotation method and Milch method for reduction of acute anterior dislocation of shoulder. J. Clin. Diagn. Res. 9, RC01–03. https://doi.org/10.7860/JCDR/2015/11850.5738 (2015).
Hayashi, M. et al. Success rate of anterior shoulder dislocation reduction by emergency physicians: a retrospective cohort study. Acute Med. Surg. 9, e751. https://doi.org/10.1002/ams2.751 (2022).
Arrillaga, B. et al. Human shoulder anatomy: new ultrasound, anatomical, and microscopic perspectives. Anat. Sci. Int. 99, 290–304. https://doi.org/10.1007/s12565-024-00775-5 (2024).
Pan, X. et al. Iatrogenic fracture during shoulder dislocation reduction: characteristics, management and outcomes. Eur. J. Med. Res. 26, 73. https://doi.org/10.1186/s40001-021-00545-3 (2021).
Author information
Authors and Affiliations
Contributions
P.Y. and R.T. were major contributors to writing the manuscript. P.Y. and Y.Z. collected patient data. L.L. and S.R. supported the statistical analysis. M.T. designed the work, interpreted the data and wrote the paper. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
All subjects and/or their legal guardian(s) gave informed consent for publication of identifying information/images in an online open-access publication.
Tables.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yuan, P., Tang, R., Zhou, Y. et al. Tang’s method is an effective new treatment for anterior shoulder dislocation. Sci Rep 15, 17705 (2025). https://doi.org/10.1038/s41598-025-03097-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03097-2