Abstract
Pathogen reduction technologies using chemicals and or UV light have been demonstrated to improve the safety of ex vivo platelets from infectious diseases. However, UV light exposure also may affect the treated products, depending on wavelength and exposure. Alternatively, visible spectra 405 nm violet-blue light has broad-spectrum microbicidal activity. Here we tested the effect of 405 nm light on Treponema pallidum, the bacterium that causes syphilis. We contaminated platelets stored in plasma with two treponemal concentrations (low and high titers) and treated an aliquot with 270 J/cm2 dose (irradiance = 15 mW/cm2) of 405 nm light while another aliquot remained untreated. Next, we inoculated intradermally an aliquot of both samples into rabbits. Rabbits inoculated with untreated samples developed syphilis while animals inoculated with light-treated samples did not. Thus, inactivation was demonstrated to the limit of detection of the bioassay. We estimated > 2 log10 and > 4 log10 reduction in the low and high dose studies, respectively. These results provide proof-of-concept that 405 nm light is effective in reducing syphilis risk in ex vivo platelets.
Similar content being viewed by others
Introduction
The spirochete bacterium Treponema pallidum subsp. pallidum is the causative agent of syphilis, a disease known under many names since the Middle Ages1,2. Syphilis is primarily transmitted by sexual contact; it is highly invasive and presents with multifaceted manifestations during chronic stages3,4. Syphilis is easily treatable with antibiotics such as penicillin although its diagnosis and management can be challenging due to the difficulty in interpreting serological diagnostic test results and evaluation of the response to therapy. In the U.S., cases of syphilis have increased in the past 10 years among females, with a concomitant increase in cases of congenital syphilis, and in males, primarily in men who have sex with men5. This resurgence of syphilis in high-risk populations is alarming not only in itself but also because of its potential spread to low-risk populations like blood donors. This scenario has been of particular concern to the blood transfusion community since syphilis can be transmitted by blood transfusion6. New studies in the U.S. and elsewhere have investigated how the increase of syphilis cases has impacted syphilis risk in current blood donations. The results showed a correlation between the country’s syphilis epidemic and the rise of syphilis positivity in blood donors7,8,9. However, this increase has not resulted in new cases of transfusion-transmission syphilis, and this is due to the effective risk mitigation measures such as, donor screening questionnaire and universal syphilis testing of donated blood that have been in place for more than 70 years10. In addition, the conventional practice of refrigerated storage of whole blood provides some additional level of reduction of Treponema pallidum, although not as effective and rapid as previously reported11,12. Testing all whole blood donations for multiple pathogens, including Treponema pallidum, has protected the blood supply, and maintained the safety of blood transfusions. However, this strategy has also resulted in an ever-expanding list of emerging or reemerging pathogens to be tested and in some cases mandated tests are based on regional or temporal risks. Implementation of these complex testing scenarios has increased costs and challenges to the blood industry13.
Platelets are the second most transfused blood component as their therapeutic use has grown over the years14,15. Platelet transfusion safety is of particular concern because this component is stored at room temperature which supports growth of bacterial contamination. A meta-analysis using published data from studies encompassing multiple countries and preparation methods of platelets estimated an overall contamination rate of 1:2000 units as assessed by primary culture16. These results aligned with CDC’s active and passive surveillance data17. To mitigate transmission risks of bacterial infections, each platelet unit is assayed using bacterial culture or rapid tests18,19. Bacterial culture methods test an aliquot of the platelet unit using optimized conditions for bacterial growth20. Those tests are highly sensitive and their main limitations are that detection of low bacterial contamination could require up to 3 days of incubation and certain bacteria do not grow to detectable levels21. As an alternative or complementary to detection, bacteria contaminating platelets and plasma can be inactivated or reduced using pathogen reduction technologies (PRTs)22. Among available PRTs is Cerus INTERCEPT Blood System that utilizes amotosalen (S-59) and long-wavelength ultraviolet (UV-A) light to cross-link DNA and RNA in a variety of bacteria, viruses, and parasites23,24,25. Another system called Mirasol Pathogen Reduction Technology System from Terumo uses riboflavin and UV-A/B light to block pathogens’ replication26,27. UV-C light alone used in THERAFLEX, Macopharma to successfully inactivate multiple pathogens28. These technologies were demonstrated effective against a wide range of blood-borne pathogens in ex vivo plasma and platelets, but post-treatment recovery and quality of platelets is technology-dependent, in some studies suboptimal outcome and recovery were reported29. To overcome the challenge that hemoglobin absorbs UV-light, alternative PRT compounds have been developed, for example, amustalin (S-303) has shown some promising results with RBCs in two phase III clinical trials30. Another viable option for light-based pathogen inactivation is violet-blue 405 nm visible light31. Small scale studies demonstrated that violet-blue light treatment of ex vivo platelets and plasma had mild to no effect on platelets function and recovery32,33 and on plasma proteins34. Importantly, this treatment does not require added photosensitive agents. The established mechanism of inactivation is based on the generation of reactive oxygen species (ROS) within the cellular microbe induced by the photoexcitation of endogenous porphyrin molecules35,36. In the case of viruses, it is speculated that flavins and flavin derivatives in the surrounding media contribute to the ROS induction36. Induction of ROS in turn induces formation of nonspecific oxidative damage and microbial death33,34. This microbicidal method has been tested in the laboratory and proven effective against bacteria, viruses and parasites suspended in either plasma or platelets under experimental conditions35,37,38,39,40. We report here 405 nm light inactivation of Treponema pallidum spiked in human platelets resuspended in plasma using rabbit bioassays to assay treponemal infectivity.
Results
405 nm light inactivation of Treponema pallidum
To assess whether 405 nm light inactivated Treponema pallidum bacteria spiked in ex vivo human platelets, we conducted three independent studies using platelets from three donors. In Studies 1 and 2, we spiked platelets with final 5 × 105 treponemes(treps)/ml (low titer) and in Study 3, the final spike was 5 × 107 treps/ml (high titer). In each study, we assayed three samples: the initial time point (T0) obtained before starting inactivation, after 5 h (270 J/cm2) exposure to 405 nm light with shaking (T5-Inactivated), and after 5 h shaking but no light exposure (T5-Control). The light dose was selected based previous studies demonstrating its effectiveness against different blood pathogens spiked in plasma and in platelets35,37,38,39,40. We measured treponemal infectivity using intradermal inoculations in rabbits. Each sample was serially diluted, and each dilution was inoculated at two adjacent sites (left and right) on the shaved back of four rabbits. At the end of the study, we scored each site as positive or negative for syphilis as shown in Supplementary Tables S1 and S2. These tables also report the estimated number of treponemes inoculated per site based on darkfield count of the treponemal stock and a schematic of the injected sites’ ___location in a rabbit. The results for Studies 1 and 2 are in Table 1. All sites inoculated with 10–1 dilution of T0, and T5-Control samples developed lesions consistent with syphilis infection (positive) and the breakpoints were between 10–2 and 10–3 dilutions. Higher dilutions of the inoculum resulted in no infections (negative). T5-Control samples (Studies 1 and 2) had very similar titers at 103.4 ID50/ml and 103.5 ID50/ml while we observed a small difference in the titers of T0 samples (103.3 ID50/ml versus 103.6 ID50/ml). In contrast, all sites inoculated with samples exposed to 405 nm light were syphilis negative (T5-Inactivated). To enhance the sensitivity of the assay, we increased the number of sites injected with the highest concentration of inactivated sample (T5-Inactivated) (10–1) from eight to 16 in Study 1 and 24 in Study 2. Assuming the worst case, we estimated the titers to be < 101.5 ID50/ml for T5-Inactivated samples in both studies. This means that the method reduced infectivity to below the limit of detection of the bioassay or > 2 log10 (> 99%).
We repeated the study with 100-fold higher final treponemal concentration of 5 × 107 treps/ml (Study 3). Table 2 and Supplementary Table S3 report the results for Study 3. The calculated titers of samples T0 and T5-Control were 106.2 ID50/ml and 105.5 ID50/ml, respectively. A relatively small drop in titer of T5-Control compared to the initial titer was also observed in Study 2 and in similar studies with Leishmania donovani parasite35. Rabbits inoculated with T5-Inactivated sample developed no skin lesions and were serologically negative with treponemal and nontreponemal tests. As above, assuming the worst case, we calculated the titer to be < 101.5 ID50/ml and estimated infectivity reduction to below the limit of detection of animal assay or > 4 log10 (> 99.99%).
Syphilis serology
In addition to scoring skin lesions, we tested rabbit sera during the study for the presence of treponemal and nontreponemal antibodies. All rabbits inoculated with untreated samples (T0 and T5-Control) had syphilis-positive serology results usually three weeks post inoculation while all rabbits inoculated with inactivated materials remained serologically negative two months post injection. To further investigate those results, we tested sera from nonreactive rabbits at 1:2 dilution, instead of 1:40 the recommended dilution, and confirmed their negative status. In contrast, sera from serologically reactive rabbits were positive up to dilution 1:2048. These results demonstrated high sensitivity of the serological test with rabbit sera and confirmed lack of seroconversion of rabbits injected with treated samples.
Investigation of inoculated sites in rabbit G130
In Study 2, three of the 24 sites inoculated with 10–1 dilution of T5-Inactivated sample showed indurations that persisted to the end of the study but appeared different from the syphilitic lesions. All three sites were in rabbit G130 and are marked in red in Supplementary Table S2. The initial assessment of these three sites was inconclusive. Although rabbit G130 never seroconverted, we were uncertain about the final assignment of those three sites and decided to investigate them further. To this goal, we biopsied all inoculated sites in rabbit G130 and as a control we also examined corresponding tissues from rabbit G135, a syphilis infected animal. We processed the tissues from the left sites for histology and the tissues from the right sites for detection of treponemal DNA. We also conducted similar analyses with popliteal lymph nodes known to harbor treponemes in infected animals.
Histopathological analysis of skin tissues
Hematoxylin and eosin staining of skin from sites inoculated with T5-Control dilutions 10–1 and 10–2 in rabbit G135 (positive control) showed skin damage exhibiting similar patterns of host response. Supplementary Fig. S1 A-D shows representative staining of tissue at site dilution 10–1. Histopathologic finding included full thickness epithelial necrosis, lymphoplasmacytic to granulomatous dermatitis, edema, and vascular endothelial hypertrophy (Supplementary Fig. S1 A-C) and uncommonly lymphoplamacytic to granulomatous myositis (Supplementary Fig. S1 D). We also observed mild follicular atrophy in tissues from dilutions 10–3, 10–4 and 10–5 with dermal edema and vascular endothelial hypertrophy like those reported in Supplementary Fig. S1C, but those sites showed no or mild inflammation. To rule out a hypersensitivity response in skin samples with edema and vascular endothelial cell hypertrophy as sole findings, we stained sections of skin with Giemsa to identify mast cells. No mast cells were observed. We also stained selected tissues with Warthin-Starry, a silver stain known to detect treponemes. Few treponemes were detected in the necrotic epithelium at the infected sites of rabbit G135 (Supplementary Fig. S4). Histological evaluation of sites in rabbit G130 inoculated with T5-Inactivated dilution 10–3 displayed epithelium with no evident necrosis or tissue damage (representative example in Supplementary Fig. S2). Supplementary Fig. S3 shows staining of tissue from the inconclusive site (rabbit G130, dilution 10–1) indicating mild epithelial hyperplasia and mild to moderate dermal edema and occasional hair follicle rupture with inflammation (furunculosis). Those observations were not consistent with syphilitic lesions and could represent an unrelated hypersensitivity response (edema) and injection associated hair follicle rupture and inflammation. Hematoxylin and eosin staining of popliteal lymph nodes of rabbit G130 showed no evident inflammation or bacteria.
Detection of treponemal DNA in skin and lymph node tissues
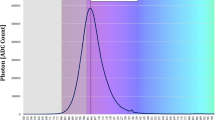
Next, we analyzed the skin biopsies of rabbits G130 and G135 for treponemal DNA using nested PCR. The results in the Fig. 1 (panel A) show the presence of DNA isolated from skin of rabbit G135 at sites injected with T5-Control sample dilutions 10–1 to 10–4. The DNA method was very sensitive and detected the lowest dose injected estimated to have contained 50 organisms at the time of inoculation. Samples with high concentration of treponemal DNA showed a top band corresponding to the product from the first DNA amplification. Importantly, we detected no treponemal DNA at the site in rabbit G135 inoculated with heat-inactivated (HI) treponemes. This result ruled out non-specific reactivity of PCR with rabbit tissue or human platelets (the dilution vehicle). All sites injected with inactivated samples produced no treponemal DNA bands (Fig. 1, panel A, G130 lanes -1 to -3). These results strongly indicated that the indurations at the inconclusive sites were not caused by live treponemes but, likely, by an unexpected host’s reactivity or hypersensitivity to other components of the inoculum. Additionally, our results were consistent with earlier reports showing persistent DNA (at least 60 days post inoculation) at infected sites and absent at sites injected with inactivated treponemes41. DNA extracted from rabbit G135 lymph node showed treponemal PCR signal (Fig. 1, panel B) while no DNA was detected in lymph nodes from all rabbits, including G130, inoculated with inactivated material (G129, G130, G131, G132). Collectively, the results from histology and nucleic acid tests decisively ruled out treponemal infectivity at the three inconclusive sites and confirmed the four rabbits were syphilis-free.
Detection of treponemal DNA in biopsy tissues. Agar gel of nested PCR products of second round of the process for skin biopsies of rabbits in Study 2 (A) and popliteal lymph nodes of rabbits in Study 2 (B) and Study 3 (C). (A) PCR products of skin from rabbit G130 inoculated with T5-Inactivated sample serially diluted from 10–1 to 10–3; G135 inoculated with T5-Control sample diluted from 10–1 to 10–4. (B) PCR products of lymph nodes from rabbits G129, G130, G131, G132 inoculated with T5-Inactivated sample and rabbit G135 inoculated with T5-Control sample. (C) PCR products of lymph nodes from rabbits G153, G154, G155, G156 inoculated with T5-Inactivated sample and rabbit G135 inoculated with T5-Control sample. HI = Heat inactivated; TP = Treponema pallidum.
In Study 3, we injected an estimated 21 million treponemes per rabbit. In previously published studies, similarly high levels of heat-inactivated bacteria inoculated intradermally into rabbits resulted in the generation of anti-treponemal antibodies, although this reactivity was delayed and weaker than that elicited by live bacteria inoculations42,43. Although none of the rabbits inoculated with T5-Inactivated sample seroconverted, we decided to conduct further tests to ensure no cases of syphilis infections were overlooked. We analyzed DNA from popliteal lymph nodes of rabbits inoculated with T5-Inactivated (G153, G154, G155, G156). The results confirmed no treponemal DNA in lymph nodes of serologically negative rabbits (Fig. 1, panel C). From these data, we concluded that none of the rabbits inoculated with light-inactivated treponemes had been infected.
Discussion
Technologies to reduce or inactivate pathogens in blood have been developed and used to address residual risk of bacterial contamination of blood and are viewed as a proactive option to improve safety of blood transfusion. Bacterial contamination of platelets is particularly concerning because of room temperature storage of this blood component. We used an upcoming and promising method of pathogen inactivation that applies violet-blue 405 nm visible light to inactivate the microorganism spiked in plasma or platelets. This technology was tested extensively with multiple pathogens under experimental laboratory conditions. Studies using metabolomics analysis of platelets showed no negative impact of 405 nm light on platelet membrane integrity and platelet aggregation activity33. Furthermore, exposure to violet-blue light for 1 h with cumulative 360 Jcm-2 demonstrated four to five log10 reduction of several transfusion-relevant gram-positive and gram-negative bacteria spiked in human plasma34,37 with no significant finding in a metabolomics study34,44,45. These data support 405 nm light-based pathogen inactivation technology as a promising novel tool for safe and effective treatment of human ex vivo platelets and plasma.
Here we investigated the same technology against the bacterium Treponema pallidum spiked in human platelets at two concentrations, 105.7 and 107.7 treps/ml. Different from other bacteria, Treponema pallidum cannot be propagated in bacterial culture media and for many years this bacterium was considered unculturable. Recently, investigators have improved on earlier attempts and demonstrated that Treponema pallidum can be successively propagated and maintained on rabbit epithelial cell (Sf1EP) under low oxygen and other specific growth conditions46,47. However, the gold-standard for assaying infectivity of Treponema pallidum remains the propagation of the organism in an animal host, usually rabbit testis. To assess inactivation of Treponema pallidum, we needed to quantitate the bacteria before and after treatment. Treponema pallidum enumeration requires darkfield microscopy which lacks sensitivity and is unsuitable to quantify the microorganisms diluted in platelets. The conventional method to titer a Treponema pallidum suspension is to serially dilute the sample, inject intratesticularly each dilution into a group of rabbits and monitor rabbits for seroconversion. This method requires large numbers of animals. We titered Treponema pallidum samples using an alternative approach where each dilution series was injected intradermally into rabbits. This method produced an independent bacterial titration in each rabbit, reduced the number of animals needed and provided a quantitative statistical measurement of infectivity titers. One challenge of this approach was that in a few cases, such as with rabbit G130, determining the final site scores required additional investigations.
Another consideration is the sensitivity of intradermal injections and how it compares to that of the conventional testicular inoculations. We found no published studies that directly compared the two methods using the same materials. Using our data from titration of T0 samples, we estimated 50% infectious dose (ID50) 2500 and 1260 organisms per site in Studies 1 and 2, respectively (low titer stock) and 315 organisms per site in Study 3 (high titer stock). In all cases, our ID50 values were higher than 1–10 organisms/site previously reported for in vitro cultured Treponema pallidum organisms46. Human platelets could have caused this difference or our treponeme stocks, especially that with low titer, might have lost some activity after long-term storage. It is also likely that freshly prepared cultured treponemes were more infectious than our thawed organisms. We are investigating those possible scenarios. However, it should be noted that infectivity log10 reduction was calculated as the difference of the two titers in log10 and thus, it was independent from the number of treponemes in the sample. We also could not find reports of full serial dilution titrations of treponemal stocks using the intratesticular route. Here we could use data from Lin et al.24 showing that 100 organisms per rabbit resulted in an attach rate of 11/16 (68%) and propose that ID50 dose for testicular inoculations is < 100 organisms. Thus, from these limited literature data, the two inoculation modalities have sensitivities in the same order of magnitude although this conclusion should be confirmed with direct measurements.
Rabbits inoculated with light-inactivated samples either from low or high titer studies developed no syphilitic lesions and had no seroreactivity when assayed with treponemal and nontreponemal tests. These results are consistent with our in-house data for rabbits inoculated with heat-inactivated treponemes. Interestingly, bacterial DNA was not present at sites injected with as much as 5 million inactivated treponemes confirming previously reported results that dead treponemes are cleared within days39 possibly by macrophages [4, and Supplementary Fig. S3] or other mechanisms. In contrast, bacterial DNA was detected in all sites injected with T5-Control sample, even at sites with no lesions indicating that PCR was more sensitive than skin reactivity.
Violet-blue 405 nm light inactivated Treponema pallidum to undetectable levels by animal bioassays corresponding to > 2 log10 and > 4 log10 infectivity reduction depending on the input dose. Although treponemal load in donated blood is not known, it is likely that of the two conditions tested, the low concentration is closer to the level of contamination in the blood of a syphilis asymptomatic donor. It should be noted that our studies do not demonstrate sterility of the treated platelets since only a small portion of the total volume was assayed and a few treponemes could have survived the light-treatment and persist after 7 days storage11. However, unlike conventional bacteria that can grow in platelets48, treponemes do not propagate in platelets. Cerus Intercept Blood System technology showed reduction of spiked treponemes by > 5.9 log10 in plasma25 and ~ 7 log10 in platelets24. Our data trends are consistent with those results with two caveats: our starting titers were lower than those used in Cerus’ studies, which limited the number of log10 reduction that we could demonstrate and secondly, we injected 0.1 ml of sample per site compared to 1 ml inoculated into testes in Cerus’ study24,25. This tenfold difference in volume is in part responsible for the difference in log10 reduction between the studies.
In conclusion, these studies conducted using small volumes of platelets provided proof-of concept that 405 nm violet-blue light successfully inactivated Treponema pallidum spiked in human platelets to levels that would offer improvement in transfusion safety. Although not demonstrated in these studies, we anticipate the bactericidal effect of 405 nm violet-blue light on Treponema pallidum in platelets is extended also to plasma matrix, based on published data demonstrating the technology was equally effective in inactivating pathogens in both blood components34,38,39,49.
Materials and methods
Animals
All animal experiments were conducted at the Food and Drug Administration White Oak Campus, Silver Spring, Maryland with prior approval of the FDA White Oak Institutional Animal Care and Use Committee and conformed to the Guide for the Care and Use of Laboratory Animals published by the U.S. National Institutes of Health (NIH). (Animals study ASP#2022–09, LG as principal investigator.) New Zealand white rabbits (Charles River Laboratories, Saint Constant, Canada) weighing 3–4 kg with nonreactive syphilis test were used. Animals were housed individually in a room with temperature set at 16–18 °C. For intratesticular inoculations, rabbits were anesthetized with Ketamine (10 mg/kg) and Dexmedetomidine (0.025 mg/kg) injected intramuscularly followed by isoflurane (1–2%), as needed. For intradermal inoculations, rabbits were sedated with Midazolam at doses between 0.5mg/kg to 1.5 mg/kg injected intramuscularly supplemented with isoflurane, as needed. Rabbits were euthanized by intravenous or intracardiac injections of 1.5 ml of Pentobarbital solution (Euthasol, Virbac, St Louis, MO) while under deep anesthesia induced by Ketamine (50 mg/kg) and Dexmedetomidine (0.05 mg/kg) injected intramuscularly.
Treponemal stocks
We propagated Treponema pallidum, Nichols strain, into naïve rabbits by intratesticular inoculations of 1 ml of treponemal stock using established protocols50. We monitored rabbits daily for orchitis and tested sera every 3–4 days with a treponemal test, Serodia T. pallidum (TP)-particle agglutination (PA) assay (Fujirebio, Malvern, PA), and a nontreponemal test, ASI rapid plasma reagin (RPR) assay (Arlington Scientific Inc., Springville, UT), according to manufacturers’ instructions. At peak orchitis, we euthanized the rabbits and collected testes aseptically. We extracted treponemes from testes in harvest medium (50% normal rabbit serum and 50% saline) for 10–15 min with shaking50. Next, we removed an aliquot for counting treponemes by darkfield microscopy using Nexcelom disposable slides, mixed the rest of the suspension with sterile glycerol (15–20% final concentration), aliquoted, and stored frozen as treponemal glycerol stock.
Violet-blue 405 nm light inactivation of Treponema pallidum
We obtained fresh apheresis platelets collected in plasma from volunteer donors in the Research Donor Program, NIH, Bethesda, Maryland and used the day after collection. This study involving human subjects’ protocol was approved by FDA Research Involving Human Subjects Committee (RIHSC, Exemption Approval #11-036B). All methods were carried out in accordance with the relevant guidelines and regulations. Informed consent from all subjects were obtained as per National Institutes of Health, USA. We conducted three independent inactivation studies with two concentrations of Treponema pallidum bacteria (low and high titers) spiked in ex vivo human platelets. In the two low titer studies 1 and 2, we spiked 20 ml of human platelets with treponemal glycerol stock (1:10) for a final spike concentration of 5 × 105 treponemes/ml (105.7 treps/ml) and mixed gently. We removed an aliquot, performed serial dilution and intradermally inoculated the sample into rabbits within one hour of preparation (T0). We split the rest of the sample into four T-25 flasks (~ 4.5 ml/each), wrapped two flasks in aluminum foil to protect from light (negative control) and placed all four flasks in the 405 nm light treatment in a close cabinet31. The light source was composed of narrowband 405 nm LED arrays (FWHM∼20 nm; LED Engin, CA, USA) with appropriate thermal management and powered by LED drivers (MeanWell, Taiwan). The light source was held at 14 cm above the samples. Light exposure to 405 nm violet-blue light was for 5 h to achieve a light dose of 270 J/cm2 (irradiance = 15 mW/cm2) at room temperature and with mild agitation. Next, we pooled samples from the two exposed flasks (T5-Inactivated) and the two control flasks (T5-Control), removed an aliquot for testing, performed serial dilutions and inoculated intradermally into rabbits within one hour of preparation. In the high titer spike study, we conducted the same inactivation experiment using a treponemal stock with a titer of 5 × 108 treps/ml at a final spike concentration of 5 × 107 treps/ml (107.7 treps/ml) (Study 3).
Rabbit inoculations
We shaved rabbits on the back the day before inoculation, marked the sites of inoculations and kept the area shaven throughout the study. Using human platelets as the diluent, we serially diluted the three samples produced in each study (T0, T5-Inactivated and T5-Control) and immediately injected rabbits intradermally with 0.1 ml of sample per site. Each dilution was inoculated in duplicate into two adjacent sites (left and right)46 and typically we inoculated 5 dilutions except when otherwise noted. Each dilution series was inoculated into four rabbits resulting in a total of eight sites per dilution as indicated in the Tables in Supplementary Information. However, anticipating inactivation of the organisms by exposure to 405 nm light, instead of eight sites we inoculated T5-Inactivated at dilution 10–1 in 16 or 24 sites thus, increasing the probability of detecting at least one positive site. As negative controls, we inoculated platelets alone or treponemal stock heat-inactivated for 30 min at 56 °C and then diluted tenfold in platelets. For the duration of the study, we collected sera weekly and tested with Serodia TP-PA test and RPR ASI test.
We monitored rabbits and injected sites three times a week and reported the appearance of the lesions according to pre-defined scoring system. Typically, injected sites showed initial and transient erythema as a response to the intradermal injections. At sites injected with live treponemes, we observed persistent erythema that changed into induration or papule and progressed to open lesions measuring up to 20 mm and ulcers at sites inoculated with high titer samples. Changes in the appearance and size of the lesions occurred for 5–6 weeks post inoculation and we continued monitoring the rabbits for a total of 8 weeks.
Tissue biopsies and histological evaluation
Sixty days post inoculation we euthanized rabbits inoculated with T5-Inactivated and T5-Control from Study 2. We excised approximately 80–100 mg of skin at the inoculated sites using 4 mm diameter disposable biopsy punchers with plunger (Integra LifeSciences, Mansfield, MA). We analyzed skin and popliteal lymph node tissues from rabbit G130 injected with dilutions of T5-Inactivated and G135 rabbit similarly injected with dilutions of T5-Control. We collected the tissue on the left in 10% formalin for histology and froze the matching tissue from the right site for treponemal DNA detection. We collected popliteal lymph nodes from the same rabbits for histological examination and treponemal DNA detection. Fixed tissues were cut and stained using hematoxylin and eosin (H&E) to reveal morphological changes in the skin tissue and Giemsa to examine mast cells (American Histolabs, Inc, Gaithersburg, Maryland). Selected tissues were stained with Warthin-Starry for detection of spirochetes at the injection sites (Histology Consultation Services, Inc, Everson, Washington).
Treponemal PCR of skin tissues and popliteal lymph nodes
We performed nested PCR on DNA isolated from skin and lymph nodes of G130 and control animals from Study 2. Similarly, we excised popliteal lymph nodes from rabbits injected with T5-Inactivated in Study 3 and processed the tissues for treponemal DNA detection. We isolated total DNA from tissues using Quick-DNA Midiprep Plus Kit (Zymo Research, Irvine, CA) according to the vendor’s instructions. Nested PCR targeting the polA gene was performed initially with inner PolA1 (sense: 5′ -TGCGCGTGTGCGAATGGTGTGGTC-3′ and anti-sense: 5′ -CACAGTGCTCAAAAACGCCTGCACG-3′) in a total volume of 50 μl. Each reaction consisted of 10 μl of DNA, 40 μl of PCR master mix 36 µl AmpliTaq Gold 360 Master Mix (Thermo Fisher Scientific, Waltham, MA) and 2 µl of each primer. In the second round of PCR, 5 μl of the first reaction product was used in a total volume of 50 μl of reaction mixture with PolA2 the sense primer 5′-GGATTGCATCCGCACGATAC-3′ and the anti-sense primer 5′-CAGCAGATGCAGATACCCCA-3′51. DNA isolated from 100 μl of Treponema pallidum glycerol stock using QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) served as positive control for nested PCR.
Statistical analysis
We scored each site as reactive (positive) or nonreactive (negative), we combined the results for all rabbits inoculated with the same sample (usually four rabbits) and based on the ratio reactive/nonreactive sites as a function of sample dilution, we calculated the ID50 per volume inoculated (0.1 ml) using the Reed-Muench method52, adjusted the titer to 1 ml of inoculum and reported it as ID50/ml. In the cases of T5-Inactivated for which all sites were negative, we assumed the worse-case where tenfold higher concentration would have resulted in all sites being reactive. Log10 reduction was calculated as the difference in log10 titers of the untreated (T5-Inactivated) and treated (T5-Control) samples.
Data availability
All data generated during this study are available upon request to the corresponding author. We report here the data that support the findings of this study and its Supplementary Information files.
References
Arora, N. et al. Origin of modern syphilis and emergence of a pandemic Treponema pallidum cluster. Nat. Microbiol. 2, 16245 (2016).
Giacani, L. & Lukehart, S. A. The endemic treponematoses. Clin. Microbiol. Rev. 27, 89–115 (2014).
Peeling, R. W. et al. Syphilis. Nat. Rev. Dis. Primers 3, 17073 (2017).
Lafond, R. E. & Lukehart, S. A. Biological basis for syphilis. Clin. Microbiol. Rev. 19, 29–49 (2006).
Center for Disease Control and Prevention. Sexually Transmitted Disease Surveillance, 2022. Available from: https://www.cdc.gov/std/statistics/2022/overview.htm#Syphilis.
Chambers, R. W., Foley, H. T. & Schmidt, P. J. Transmission of syphilis by fresh blood components. Transfusion 9, 32–34 (1969).
Conti, G. et al. US Transfusion-Transmissible Infections Monitoring System (TTIMS). Syphilis seroprevalence and incidence in US blood donors from 2020 to 2022. Transfusion 64, 325–333 (2024).
O’Brien, S. F. et al. Monitoring syphilis serology in blood donors: Is there utility as a surrogate marker of early transfusion transmissible infection behavioral risk?. Transfusion 63, 1195–1203 (2023).
UK Health Security Agency and NHS Blood and Transplant. Safe supplies 2021: FAIRer donor selection. Accessed April 15, 2024. Available from: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/27793/annual-review-with-a4-infographics-final-accessible-features-v3.pdf
Guidance for Industry: Recommendations for Screening, Testing and Management of Blood Donors and Blood and Blood Components Based on Screening Tests for Syphilis. December 2020. Available from: https://www.fda.gov/media/85283/download
Tamrakar, P. et al. Effect of storage on survival of infectious Treponema pallidum spiked in whole blood and platelets. Transfusion 61, 3181–3189 (2021).
D’aes, T. et al. Does cold storage of blood before transfusion prevent the transmission of syphilis? A systematic review and meta-analysis. Vox Sang. 119, 219–231 (2024).
Klein, H. G., Hrouda, J. C. & Epstein, J. S. Crisis in the sustainability of the U.S. blood system. N. Engl. J. Med. 377, 1485–1488 (2017).
Schiffer, C. A. et al. Platelet transfusion for patients with cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 36, 283–299 (2018).
Lee, R. H., Kasthuri, R. S. & Bergmeier, W. Platelet transfusion for patients with platelets dysfunction: Effectiveness, mechanisms, and unanswered questions. Curr. Opin. Hematol. 27, 378–385 (2020).
White, S. K., Schmidt, R. L., Walker, B. S. & Metcalf, R. A. Bacterial contamination rate of platelet components by primary culture: A systematic review and meta-analysis. Transfusion 60, 986–996 (2020).
Kracalik, I. et al. Posttransfusion sepsis attributable to bacterial contamination in platelet collection set manufacturing facility, United States. Emerg. Infect Dis. 29, 1979–1989 (2023).
Schmidt, M., Ramirez-Arcos, S., Stiller, L. & McDonald, C. ISBT Transfusion-Transmitted Infectious Diseases Working Party, Subgroup on Bacteria. Current status of rapid bacterial detection methods for platelet components: A 20-year review by the ISBT Transfusion-Transmitted Infectious Diseases Working Party Subgroup on Bacteria. Vox Sang. 117, 983–988 (2022).
Kamel, H., Ramirez-Arcos, S. & McDonald, C. ISBT Transfusion-Transmitted Infectious Disease Bacterial Working Party Bacterial Subgroup. The international experience of bacterial screen testing of platelet components with automated microbial detection systems: An update. Vox Sang. 117, 647–655 (2022).
Störmer, M. & Vollmer, T. Diagnostic methods for platelet bacteria screening: current status and developments. Transfus. Med. Hemother. 41, 19–27 (2014).
Levy, J. H., Neal, M. D. & Herman, J. H. Bacterial contamination of platelets for transfusion: Strategies for prevention. Crit. Care 22, 271 (2018).
Cloutier, M. & De Korte, D. ISBT Transfusion-Transmitted Infectious Diseases Working Party, Subgroup on Bacteria. Residual risks of bacterial contamination for pathogen-reduced platelet components. Vox Sang. 117, 879–886 (2022).
Lanteri, M. C. et al. Inactivation of a broad spectrum of viruses and parasites by photochemical treatment of plasma and platelets using amotosalen and ultraviolet A light. Transfusion 60, 1319–1331 (2020).
Lin, L. et al. Photochemical treatment of platelet concentrates with amotosalen and long-wavelength ultraviolet light inactivates a broad spectrum of pathogenic bacteria. Transfusion 44, 1496–1504 (2004).
Singh, Y. et al. Photochemical treatment of plasma with amotosalen and long-wavelength ultraviolet light inactivates pathogens while retaining coagulation function. Transfusion 46, 1168–1177 (2006).
Goodrich, R. P., Gilmour, D., Hovenga, N. & Keil, S. D. A laboratory comparison of pathogen reduction technology treatment and culture of platelet products for addressing bacterial contamination concerns. Transfusion 49, 1205–1216 (2009).
Kwon, S. Y. et al. Pathogen inactivation efficacy of Mirasol PRT System and Intercept Blood System for non-leucoreduced platelet-rich plasma-derived platelets suspended in plasma. Vox Sang. 107, 254–260 (2014).
Gravemann, U., Handke, W., Müller, T. H. & Seltsam, A. Bacterial inactivation of platelet concentrates with the THERAFLEX UV-Platelets pathogen inactivation. Transfusion 59, 1324–1332 (2019).
Marks, P. & Verdun, N. Toward universal pathogen reduction of the blood supply (Conference Report, p. 3002). Transfusion 59, 3026–3028 (2019).
Brixner, V. et al. Red blood cells treated with the amustaline (S-303) pathogen reduction system: A transfusion study in cardiac surgery. Transfusion 58, 905–916 (2018).
Atreya, C., Maclean, M., Anderson, J. G. & MacGregor, S. J. (2024). Inactivation of pathogens in ex vivo blood products in storage bags using visible light. (Patent No. US Patent 11,951,217).
Maclean, M. et al. Non-ionizing 405 nm light as a potential bactericidal technology for platelet safety: Evaluation of in vitro bacterial inactivation and in vivo platelet recovery in severe combined immunodeficient mice. Front Med. (Lausanne). 6, 331 (2020).
Sun, J. et al. Metabolomics evaluation of the photochemical impact of violet blue light (405 nm) on ex vivo platelet concentrates. Metabolomics 19, 88 (2023).
Stewart, C. F. et al. Violet-blue 405-nm Light-based photoinactivation for pathogen reduction of human plasma provides broad antibacterial efficacy without visible degradation of plasma proteins. Photochem. Photobiol. 98, 504–512 (2022).
Kaldhone, P. R. et al. The preclinical validation of 405 nm light parasiticidal efficacy on Leishmania donovani in ex vivo platelets in a Rag2(-/-) mouse model. Microorganisms 12, 280 (2024).
Haridas, D. & Atreya, C. D. The microbicidal potential of visible blue light in clinical medicine and public health. Front. Med. Lausanne 9, 905606 (2022).
Maclean, M., MacGregor, S. J., Anderson, J. G. & Woolsey, G. Inactivation of bacterial pathogens following exposure to light from a 405-nanometer light-emitting diode array. Appl. Environ. Microbiol. 75, 1932–1937 (2009).
Jankowska, K. I. et al. Complete inactivation of blood borne pathogen Trypanosoma cruzi in stored human platelet concentrates and plasma treated with 405 nm violet-blue light. Front Med. (Lausanne) 7, 617373 (2020).
Ragupathy, V. et al. Visible 405 nm violet-blue light successfully inactivates HIV-1 in human plasma. Pathogens 11, 778 (2022).
Jackson, J. W. et al. 405 nm violet-blue light inactivates hepatitis C cell culture virus (HCVcc) in ex vivo human platelet concentrates and plasma. Sci. Rep. 14, 31540 (2024).
Wicher, K. et al. Identification of persistent infection in experimental syphilis by PCR. Infect. Immun. 66, 2509–2513 (1998).
Turner, T. B. & Hollander, D. H. Biology of the treponematoses. Monogr. Ser. World Health Organ. 35, 3–266 (1957).
Gao, K. et al. Origin of nontreponemal antibodies during Treponema pallidum infection: Evidence from a rabbit model. J. Infect. Dis. 218, 835–843 (2018).
Jackson, J. W. et al. Human platelet concentrates treated with microbicidal 405 nm light retain hemostasis activity. J. Photochem. Photobiol. B 255, 112922 (2024).
Stewart, C. F. et al. Microbial reduction of prebagged human plasma using 405 nm light and its effects on coagulation factors. AMB Express 14, 66 (2024).
Edmondson, D. G., Hu, B. & Norris, S. J. Long-term in vitro culture of the Syphilis Spirochete Treponema pallidum subsp. pallidum. MBio 9, e01153-e1218 (2018).
Fieldsteel, A. H., Cox, D. L. & Moeckli, R. A. Cultivation of virulent Treponema pallidum in tissue culture. Infect Immun. 32, 908–915 (1981).
McDonald, C. P., Bearne, J., Aplin, K. & Sawicka, D. Assessing the inactivation capabilities of two commercially available platelet component pathogen inactivation systems: effectiveness at end of shelf life. Vox Sang. 116, 416–424 (2021).
Maclean, M., Anderson, J. G., MacGregor, S. J., White, T. & Atreya, C. D. A New proof of concept in bacterial reduction: Antimicrobial action of violet-blue light (405 nm) in ex vivo stored plasma. J. Blood Transfus. 2016, 2920514 (2016).
Lukehart, S. A. & Marra, C. M. Isolation and laboratory maintenance of Treponema pallidum. Curr. Protoc. Microbiol. Chapter 12: Unit 12A.1 (2007).
Wang, C. et al. Sensitive detection of Treponema pallidum DNA from the whole blood of patients with syphilis by the nested PCR assay. Emerg. Microbes Infect. 7, 83 (2018).
Reed, L. J. & Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 27, 493–497 (1938).
Acknowledgements
We would like to thank the technical staff in the FDA White Oak vivarium for the care provided to our animals and Dr. Damaris Ruth Molano for her assistance and support in the inoculations of animals. We are particularly indebted to Drs. Norris and Edmondson, University of Texas, Houston for their generous gift of a Treponema pallidum stock Nichols stain and for sharing their extensive knowledge of syphilis in rabbits. We also thank our laboratory coworkers for their support and, in particular we are grateful to Temisan Otubu for her early contributions to this project. Finally, we are thankful to our FDA colleagues who helped with procuring fresh human platelets for these studies and all the volunteers who donated blood for this research. This study was also supported, in part, by a Postgraduate Research Fellowship Award to P.K. from the Oakridge Institute for Science and Education (ORISE) through an interagency agreement between the U.S. Department of Energy and the U.S. Food and Drug Administration.
Funding
This research was funded by intramural grants from the U.S. Food and Drug Administration.
Author information
Authors and Affiliations
Contributions
O.Y., T. P., P.K., J. J. performed the experiments; D. R. analyzed histopathology slides; C. A., C. S., J. A., S. M., M. M. developed the violet-blue light inactivation technology used in this work and other contributions include insightful comments to improve the manuscript; L.G., C. A. designed the experiments and drafted the manuscript. All authors have read and agreed to this version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors declare no competing interests. C.S., J.A., S.M., M.M. and C.A. are the inventors of the violet-blue 405 nm light technology (Atreya et al. US Patent No. 11,951,217B2).
Ethics approval
The study was conducted in accordance with ARRIVE guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yakovleva, O., Pilant, T., Kaldhone, P. et al. 405 nm light microbicidal efficacy on Treponema pallidum spiked in ex vivo human platelets. Sci Rep 15, 19893 (2025). https://doi.org/10.1038/s41598-025-03230-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03230-1