Abstract
Spinal fusion has shown satisfactory efficacy in the treatment of adult patients with low-grade isthmic spondylolisthesis (LGIS), however, the efficacy of direct repair (DR) for LGIS has not been established, and there is as yet a few reports on it. To assess the clinical efficacy of DR with the pedicle screw-rod-hook (PSRH) fixation and transforaminal lumbar interbody fusion (TLIF) in adult patients with symptomatic LGIS. A total of 140 adult patients with LGIS were enrolled from April 2009 to December 2018, of whom, 69 cases underwent DR using the PSRH system and 71 cases underwent TLIF, with clinical efficacy evaluated comparatively using clinical and radiological assessments. The patients in both groups showed satisfactory pain relief efficacy and improvement in lumbar spine function. Bone fusion rate was 97.10% in the DR group vs. 100% in the TLIF group. The range of motion (ROM) of the surgical segment was significantly decreased from 13.72 ± 6.73 preoperatively to 11.60 ± 9.70 at the final follow-up (FFU) in the DR group and lost in the TLIF group, however, that of the upper intervertebral space (UIS) in each group or between groups before and after operation did not differ significantly. Both DR and TLIF are effective for adult patients with LGIS. As compared with TLIF, DR is more effective in preserving the ROM of the operative segment yet with less impact on adjacent segments.
Similar content being viewed by others
Introduction
Spondylolysis is defined as a defect in pars interarticularis of lumbar vertebra1. Approximately 39–82% cases of spondylolysis progress to spondylolisthesis2,3. Isthmic spondylolisthesis (IS) is the anterior translation of one lumbar vertebra relative to the next caudal segment due to pars interarticularis defect4. IS occurs in 3.7–8% of the general adult population4, and approximately 60% of the adult lysis cases present low-grade (Meyerding5 grade I/II) isthmic spondylolisthesis6 (LGIS). Low back pain (LBP) is the most common clinical symptom. The patients with no response to nonsurgical treatment for ≥ 6-months or those with progressive worsening of symptoms or neurologic deficit may benefit from surgical management with direct repair (DR) or spinal fusion7,8.
The spinal fusion was found to be associated with satisfactory pain relief, and improved lumbar spine function, a high fusion rate, which thus is widely used to treat patients with LGIS9,10,11,12. However, fusion surgery may lead to a loss of the surgical segment motion, potentially causing spinal stiffness and an increased incidence of adjacent segment disk degeneration (ASD). DR may be a better option because it contributes to normal anatomy and preserves the motion of the affected segment13. The DR techniques, including Buck’s method14, Nicol and Scott transverse steel wire15,16, Morscher hook-screw17, pedicle screw-rod-hook (PSRH) fixation18, pedicle screw with a U-shaped or V-shaped rod7, mainly used for the treatment of lumbar spondylolysis showed satisfactory efficacy19,20 but rarely used exclusively for LGIS19,21,22,23. There are as yet few comparative studies on the efficacy of interbody fusion and DR24,25. The results of Schlenzka et al.25,26 showed that the fusion group did significantly better at the mean follow-up of 14.8 years than in Scott’s wiring group by compared with posterolateral segmental fusion without instrumentation in patients with IS and LGIS. The Scott’s wiring technique showed little efficacy in reducing the slipped vertebral body and the isthmic defect area, thus affecting spondylolysis fusion and the long-term efficacy. DR using the PSHR system showed satisfactory clinical efficacy for lumbar spondylolysis and for LGIS in a small number of cases7,27. Whether DR using the PSHR system is more safe and effective than lumbar interbody fusion in patients with LGIS remains unknown. The aim of this study is to evaluate the clinical efficacy of DR using PSRH system versus transforaminal lumbar interbody fusion (TLIF) in adult patients with LGIS.
Materials and methods
Ethics statement
This retrospective study was approved by the Institutional Review Board of the Third Affiliated Hospital of Chongqing Medical University (Approval No. KY22039) and conducted in accordance with the Declaration of Helsinki. Due to the retrospective nature of the study, the Institutional Review Board of the Third Affiliated Hospital of Chongqing Medical University waived the need of obtaining informed consent’ in the manuscript.
Patient population
The included patients should meet the inclusion criteria including symptomatic single-segment low-grade (Meyerding grade I/II) bilateral IS, lack of response to conservative treatment for at least 6 months, disabling LBP with or without radiating pain in lower extremities or neurological deficit, and follow-up of at least 2 years were included. Those patients with severe osteoporosis, scoliosis, fractures, infection, tumors, previous lumbar surgery, and psychological disorders were excluded from this study.
Between April 2009 and December 2018 in our department, a total of 140 patients with LGIS meeting the inclusion criteria were included in our study, with 69 cases undergoing DR with the PSRH system and 71 patients undergoing TLIF. Detailed information for each group is shown in Table 1. The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions. The patients without radicular pain (but possibly radiating pain down to the thighs) and neurological deficit, and their intervertebral disc degeneration was evaluated at ≤ Grade 3 by Pfirrmann’s classification28 with the discal height of above two-thirds of its normal height were assigned to receive DR, otherwise to receive TLIF.
Preoperative management
Preoperative radiological assessments included radiography for examination of isthmic defect, vertebral slip, 3-dimensional reconstruction computed tomography (CT) for examination of the pars defect and pedicle size, excluding lumbar intervertebral disc herniation, spinal stenosis, and magnetic resonance imaging (MRI) for assessing the level of disc degeneration by the Pfirrmann grading systems28, foraminal stenosis, and nerve root compression.
Surgical technique
A posterior midline longitudinal incision was made under general anesthesia. Through the Wiltse intermuscular approach29, the following structures were exposed bilaterally: the pars interarticularis, laminas, base of the transverse processes, and screw entry points (positioned at the mammillary process, corresponding to the junction of the proximal third of the transverse process and the lateral margin of the superior articular facet in the lumbar spine).
Direct repair (DR) protocol
In the DR group, under direct visualization, the local soft tissue, the fibrocartilaginous tissue and sclerotic bone edges within the pars interarticularis defect were curetted until punctuate bleeding from cancellous bone was observed. Autogenous cancellous bone graft was harvested through the same midline fascial incision via a subcutaneous tunneling downward to the posterosuperior iliac crest, where a 3 × 1 cm cortical window was created using a 4-mm osteotome for cortical opening followed by a curved curette, with preservation of the inner cortical table. The bone window was reapproximated and secured using #2 Ethibond sutures in a horizontal mattress pattern through 1.2-mm drill holes at the cortical margins. Bilateral long-tailed pedicle screws (length determined by preoperative CT measurements) were inserted into the lytic vertebra, targeting the pedicle axis under fluoroscopic guidance. Reduction technique: A lamina hook was precisely anchored to the inferior edge of the pathologic lamina. The pre-bent titanium rod was primarily secured to the hook assembly, with subsequent gradual cantilever reduction achieved through sequential tightening between the screw’s extended tabs and rod construct. Fusion: The isthmic defect was reduced through final compression and locking between the laminar hooks and pedicle screws along the titanium rod. Decortication of the lamina and pars surfaces was performed using a high-speed burr. Harvested cancellous bone was grafted over the decorticated bilateral pars defects and laminae. The surgical incision was closed in a layered manner after subfascial drainage placement, with subsequent approximation of subcutaneous tissue followed by skin closure.
In the TLIF group, after exposure of laminas and the bilateral facet joints at each level of the spinal segment to be fused, a standard TLIF procedure was used to perform decompression, reduction, fusion, and pedicle screw fixation30.
Postoperative care
The patients were allowed to walk with a brace for 3 months to limit extension and torsion movements and do proper functional exercise. All enrolled patients underwent a systematic follow-up protocol comprising both clinical evaluations and radiological assessments. The initial postoperative evaluation was conducted within the first 72 h postoperatively, followed by comprehensive follow-up assessments at 3, 6, 12, 18, and 24 months after surgical intervention. Subsequent annual evaluations were maintained thereafter. Regarding imaging surveillance, computed tomography (CT) scans were systematically obtained at 6-month intervals during the critical bone remodeling phase (specifically at 6, 12, and 18 months post-operation) until radiographic confirmation of bone healing was achieved. For longitudinal assessment of intervertebral disc remodeling and early detection of degenerative changes, serial MRI evaluations were performed using T2-weighted sequences at biennial intervals (2, 4, 6, 8, and 10 years postoperatively). This protocol specifically targeted morphological integrity, nuclear hydration status, and adjacent segment degeneration, with particular attention to recurrent herniation and annular fibrosis formation.
Evaluation criteria
Clinical outcome assessments
The clinical outcomes were measured using the Visual Analog Scale (VAS) of LBP and lower extremity pain, the Oswestry Disability Index (ODI) of the functional outcome, and the Prolo score of the functional and economic statutes31. The length of the operation time, the amount of blood loss, and surgical complications were assessed.
Radiological assessments
The radiologic outcomes32 (Fig. 1) included disc height (DH), slip distance (SD), slipping percentage (SP), slip angle (SA), upper intervertebral space angle (UISA), lumbar lordosis (LL), the range of motion of the surgical intervertebral space (ROMSIS) and upper intervertebral space (ROMUIS) and the isthmic and intervertebral union.
Points a, d, e and f represent the front and rear edges of the upper endplate of S1 and the lower endplate of L5, respectively. Line segments da, gh, jk are lines paralleling to the upper endplates of S1, L5 and L1, respectively, and segments ef and ih are lines paralleling to the lower endplates of L5 and L4, respectively. Lines gh and ih intersect at point h to form ∠β. Perpendicular lines were drawn from point e and f to the line segment da with intersection of points d′ and b, respectively. Point d and point d′ coincide with each other. Point c is corresponds to the trailing edge of the lower endplate of L5 on S1. da and ef are respectively extended lines and they intersect at point o, forming ∠α.
DH = 1/2(de + bf), SD = ca, SP = ca/da*100%, SA = ∠doe = ∠α, UISA = ∠ghi = ∠β, LL = The angle formed by the lines da and jk.
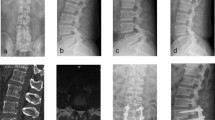
Bone fusion was evaluated based on axial and sagittal CT images33 (Fig. 2 G and H). MRI scan was performed for evaluating the intervertebral disc degeneration using the Pfirrmann grading system28 both before the operation and at the final follow‐up (FFU).
A 48-year-old female patient with LGIS of the L4 underwent direct pars repair using a PSRH system. (A–D) Show the preoperative X-rays of the lumbar spine in anteroposterior, sagittal, and hyperextension and flexion, suggesting LGIS of the L4 plus isthmic defect. The slipping percentage of L4 is 20.99%. The height and range of motion (ROM) of the L4–5 intervertebral disc is 10.55 mm and 25.8°, respectively. (E, F) Are the postoperative x-ray findings, showing that the isthmic defect has been repaired by PSRH system, and the lumbar 4 spondylolisthesis has been reset. Radiograms (G and H) are CT scans of the lumbar spine on the 6th postoperative month, showing bone fusion for the bilateral isthmic defect. (I–L) Are the x-ray findings at 24 months before and after the removal of internal fixation following the first operation. The slipping percentage of L4 is 10.31%. The disc height and ROM of L4–5 is 9.5 mm and 14.9°, respectively, and the ROM of the upper segment is 10°.
Statistical analysis
All statistical analyses were performed with the use of SPSS version 26.0 statistical software (SPSS, Inc., Chicago, IL, USA). The measurement data in normal distribution but disconformity to the median ± interquartile range were expressed as the mean ± standard deviation. Repeated-measures ANOVA was used for the comparison within each group or between groups at three time points, and the data that were not normally distributed were corrected by the Mauchly test of sphericity. For data that were not normally distributed, the comparison within each group was made using the Wilcoxon matched-pairs signed rank test and that between groups using Mann–Whitney U test. Comparison of the categorical data between groups was performed using the chi-square test, and that of the ordered categorical data using the rank-sum test. Values of P < 0.05 were considered statistically significant.
Results
Clinical assessments
Both cohorts maintained complete follow-up compliance (DR: 54.4 ± 11.8 vs. TLIF: 53.4 ± 7.6 months) with no attrition. Intergroup comparison confirmed equivalent observation periods (P = 0.518) in this retrospective matched study. The general data of the patients are summarized in Table 1. The baselines of the two groups were not uniform. The VAS and ODI scores are shown in Table 2. The modified Prolo score indicating the ability to restart work and leisure activities was evaluated as “Excellent” in 64 patients (92.75%) and “Good” in 5 patients (7.25%) in the DR group, as compared with “Excellent” in 64 patients (90.14%) and “Good” in 7 patients (9.86%) in the TLIF group at the FFU. Poor outcome was noted in none.
Radiological assessments
Radiographic findings and slip reduction assessments are shown in Table 3 and Table 4. Successful bone fusion was achieved in 67 cases (97.10%) for the DR group and 71 cases (100%) for the TLIF group. Typical cases are shown in Fig. 2. The assessments of intervertebral disc degeneration are presented in Table 5. The disc signal intensity at the surgical segment and the upper adjacent segment in the DR group and that at the upper adjacent segment in the TLIF group decreased significantly at FFU compared with before the operation (P = 0.000 < 0.05).
Complications
Operative complications are shown in Table 6. Implant failure or donor site complications occurred in none of the patients for both groups. In the DR group, of the total 5 cases with complications, one internal fixation-related LBP case presented healing of the isthmus at the onset of a symptom of LBP, with symptom relieved after removal of the internal fixation; of the 2 nonunion cases, 1 case received reoperation, and 1 received follow-up observation alone. In the TLIF group, 6 (8.45%) had complications, however, they all recovered after being given corresponding treatments including debridement, anti-infection, and open drainage among others.
Discussion
LBP is a major public health issue throughout the world, leading to a high burden steadily from 1990 to 201934. IS, predominantly LGIS6, is a common cause of LBP4. Surgery should be considered when conservative treatment fails.
Spinal fusion
Spinal fusion has been widely accepted as the treatment of symptomatic LGIS12. PLIF, TLIF, PLF, ALIF, and 360° circumferential fusion have resulted in satisfactory pain relief and a high bone fusion rate yet few complications in patients with LGIS9,10,11. In our study, the TLIF group showed significant improvements in LBP and lumbar function after the operation and the spondylolisthesis reduction and maintenance, and a higher intervertebral fusion rate (100%) than those reported in other similar studies (TLIF, 93–94%)35,36. However, some researchers believe that fusion surgery may lead to ASD and increase the risk of reoperation37,38. Kim et al.37 reported that the prevalence of radiologic versus clinical adjacent segment diseases in L4–L5 IS patients undergoing single-level interbody fusion was 72.2% and 15.9%, respectively. The incidence of ASD after L4–L5 fusion requiring reoperation was 25.2%39. The TLIF group in our study showed increases in the range of motion (ROM) and angle of the upper intervertebral space, and aggravation in radiologic ASD at the FFU as compared with before the operation. The aggravation of ASD might be attributed to the altered kinematics of the adjacent segments following fusion and redistribution of the mobility toward relative hypermobility in the adjacent levels40. Spinal fusion is associated with increased ASD but not associated with clinical outcome41. At the FFU, recurrence of pain or impaired lumbar spine function occurred in none of the patients in our study.
The advantage of DR is that it helps maintain the motion of the operative segment yet with little effect on the adjacent segment13. DR used for the treatment of spondylolysis has demonstrated satisfactory results20,40,42,43. However, the efficacy of DR in patients with LGIS remains unclear.
Feasibility of DR using the PSRH system for LGIS
In 1968, Kimura44 reported the first bone graft without internal fixation to directly repair the pars interarticularis. Since then, many DR techniques developed rapidly and contribute to improved surgical success rates in spondylolysis. However, for the LGIS patients, accurate screw placement for the Buck method was the main technical difficulty due to the slippage. In the Buck, Scott, and Morscher method, the reduction of the slipped vertebral body is difficult due to poor reduction force, and the internal fixation has a high risk of loosening and breakage, leading to a low bone fusion rate of the pars7,25,40. PSRH system is biomechanical excellent in terms of intervertebral flexion and extension stiffness or intervertebral torsional stiffness in the current several surgical methods45,46,47. The pedicle screw-based DR was associated with a low frequency of screw pullout because they provide firm fixation in three columns7.
Therefore, the PSRH system has a good biomechanical basis in the treatment of LGIS. The satisfactory efficacy of DR with the PSRH system has been reported in the treatment of spondylolysis, including a small number of LGIS cases40. In our study, both surgical cohorts demonstrated clinically meaningful improvements exceeding established MCID thresholds48. In the DR group, lumbar VAS scores decreased from 6 to 1, while TLIF patients showed reduction from 5 to 1, both surpassing the 2.1-point MCID benchmark for surgical interventions. Parallel functional improvements were observed in ODI outcomes, with DR patients achieving a 40% reduction (50% → 10%) and TLIF patients a 42% decrease (52% → 10%), exceeding the 14.9-point MCID threshold for disability index. These outcomes confirm that both techniques enabled clinically significant pain mitigation and functional restoration.
Effects of DR on the surgical segment
As we all know, DR can preserve the ROM of the operative segment. Patients in the DR group showed satisfactory activity of the operative segment at the FFU, although its activity significantly decreased from 13.72 ± 6.73 preoperatively to 11.60 ± 9.70. Fan et al.45 reported that following the performance of TSRH’s Hook plus screw fixation, modified Scott’s fixation, screw–rod construct, and Buck’s fixation at the L4-L5, the flexion–extension of the operative segment retained a ROM of about 10.5 degrees. Schlenzka et al.25 reported a decrease in the ROM of the operated segment from 13.2° preoperatively to 9.9° at the FFU in spondylolysis and LGIS by DR using Scott’s technique. Li et al.49 reported that the range of motion of the surgical segment in the PSVPH group decreased from 13.44 ± 3.99° preoperatively to 7.12 ± 1.79° at the final follow-up. The ROM of the surgical segment in our study was better than that reported above.
Currently, there is limited literature reporting the reoperation rates of stabilized segments following direct repair surgery, with most cases involving reoperations due to postoperative wound infections or non-union of the isthmus49,50. In our study, the height and slip angle of the intervertebral disc on the involved segment at the FFU showed no significant change in the DR group but the grade of disc degeneration was higher than that before surgery, which might be attributed to the natural degeneration of the intervertebral disc. After DR surgery, the posterior lumbar column unloads a small portion of the compressive stress of the anterior-middle column of the lumbar spine51, but the preoperative degenerated intervertebral disc was not restored, and the anterior-middle column still bearing most of the compressive stress, therefore, intervertebral disc degeneration might progress. However, signs of disc degeneration were not correlated to pain or patient outcomes. At the FFU, the patients with disc signal modification achieved satisfactory pain relief and regained a high quality of life.
Influence of DR on adjacent segments and lumbar curvature
The results of ASD assessments were to some extent unexpected. The DR group at the FFU showed insignificant changes in UISA, ROMUIS, and LL as compared with before the operation, but higher grades of intervertebral disc degeneration than that before the operation. Li et al.49 reported that in the PSVPH group, the ROM of the adjacent segment increased from 3.27 ± 1.22° preoperatively to 3.40 ± 0.92° at the final follow-up, with an occurrence rate of ASD of 12% (3/25) in patients treated for lumbar spondylolysis. Schlenzka et al.25 also found a similar phenomenon in the higher grades of adjacent disc degeneration at the FFU than that before the operation, while not proposing any related mechanism. At the final follow-up in the DR group, none of the patients exhibited clinical symptoms or required reoperation due to degeneration of adjacent segments. The changes observed in the adjacent segments on MRI may be attributed to a natural degeneration process, which warrants clarification in future studies.
Efficacy of two surgical methods in spondylolisthesis reduction and bone fusion
The purpose of lumbar interbody fusion surgery for patients with lumbar spinal stenosis resulting from LGIS is primarily focused on decompression rather than reduction 12. On the contrary, satisfactory reduction is very important for DR surgery. In the DR group, reduction of the slip was significantly improved and the bone fusion rate was 96.86%, which was even higher than those reported in some spondylolysis studies (52%-91%)33,40,42,49. Zayan et al.50 reported that the fusion rate for pars repair surgery utilizing pedicle screws and laminar hooks was 86.4% in a study involving 22 patients with symptomatic lumbar spondylolysis. PSRH system is associated with satisfactory reduction and maintenance of the slip, a reduction in the defect area of the isthmus, and the creation of a favorable environment for bone fusion. Preoperatively, the degree of spondylolisthesis in the TLIF group was more severe than that in the DR group. However, the reduction rate, loss rate, and bone fusion rate in the TLIF group are better than those in the DR group and those reported by many other similar studies11,52.
Overall, DR surgery not only provides effective pain relief and improves lumbar function but also preserves the ROM of stabilized segments without increasing degeneration in adjacent segments, thereby enhancing patients’ quality of life. It is anticipated that it will demonstrate even better performance in the field of non-fusion lumbar surgery in the future.
There are several limitations to this study. First, this is a retrospective study, and the baseline characteristics of the two groups were not well-balanced, reducing comparability. Second, the sample size was relatively small, which may limit the statistical power and generalizability of the findings. The reliability of our results needs further validation through prospective, multicenter studies with larger sample sizes and longer follow-up periods using similar techniques.
Conclusion
Both DR and TLIF showed satisfactory clinical efficacy for adult patients with LGIS. DR is better than TLIF in preserving the ROM of the operative segment yet with less impact on adjacent segments.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Berger, R. G. & Doyle, S. M. Spondylolysis 2019 update. Curr. Opin. Pediatr. 31, 61–68. https://doi.org/10.1097/mop.0000000000000706 (2019).
Fujii, K., Katoh, S., Sairyo, K., Ikata, T. & Yasui, N. Union of defects in the pars interarticularis of the lumbar spine in children and adolescents. The radiological outcome after conservative treatment. J. Bone Jt. Surg. 86, 225–231. https://doi.org/10.1302/0301-620x.86b2.14339 (2004).
Beutler, W. J. et al. The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Spine 28, 1027–1035. https://doi.org/10.1097/01.Brs.0000061992.98108.A0 (2003).
Kreiner, D. S. et al. Guideline summary review: An evidence-based clinical guideline for the diagnosis and treatment of adult isthmic spondylolisthesis. Spine J. Off. J. N. Am. Spine Soc. 16, 1478–1485. https://doi.org/10.1016/j.spinee.2016.08.034 (2016).
Meyerding, H. Spondylolisthesis; surgical fusion of lumbosacral portion of spinal column and interarticular facets; use of autogenous bone grafts for relief of disabling backache. J. Int. Coll. Surg. 26, 566–591 (1956).
Sakai, T., Sairyo, K., Takao, S., Nishitani, H. & Yasui, N. Incidence of lumbar spondylolysis in the general population in Japan based on multidetector computed tomography scans from two thousand subjects. Spine 34, 2346–2350. https://doi.org/10.1097/BRS.0b013e3181b4abbe (2009).
Mohammed, N. et al. A comparison of the techniques of direct pars interarticularis repairs for spondylolysis and low-grade spondylolisthesis: A meta-analysis. Neurosurg. Focus 44, E10. https://doi.org/10.3171/2017.11.Focus17581 (2018).
Noorian, S., Sorensen, K. & Cho, W. A systematic review of clinical outcomes in surgical treatment of adult isthmic spondylolisthesis. Spine J. Off. J. N. Am. Spine Soc. 18, 1441–1454. https://doi.org/10.1016/j.spinee.2018.04.022 (2018).
Burkus, J. K., Gornet, M. F., Schuler, T. C., Kleeman, T. J. & Zdeblick, T. A. Six-year outcomes of anterior lumbar interbody arthrodesis with use of interbody fusion cages and recombinant human bone morphogenetic protein-2. J. Bone Jt. Surg. 91, 1181–1189. https://doi.org/10.2106/jbjs.G.01485 (2009).
Khan, J. M. et al. Patients with predominantly back pain at the time of lumbar fusion for low-grade spondylolisthesis experience similar clinical improvement to patients with predominantly leg pain: mid-term results. Spine J. Off .J. N. Am. Spine Soc. 20, 276–282. https://doi.org/10.1016/j.spinee.2019.09.021 (2020).
Jones, T. R. & Rao, R. D. Adult isthmic spondylolisthesis. J. Am. Acad. Orthop. Surg. 17, 609–617. https://doi.org/10.5435/00124635-200910000-00003 (2009).
Tsirikos, A. I. & Garrido, E. G. Spondylolysis and spondylolisthesis in children and adolescents. J. Bone Jt. Surg. 92, 751–759. https://doi.org/10.1302/0301-620x.92b6.23014 (2010).
Gao, Y. et al. Surgical reduction and direct repair using pedicle screw-rod-hook fixation in adult patients with low-grade isthmic spondylolisthesis. Pain Res. Manag. 1–7, 2022. https://doi.org/10.1155/2022/8410519 (2022).
Buck, J. E. Direct repair of the defect in spondylolisthesis. Preliminary report. J. Bone Jt. Surg. 52, 432–437 (1970).
Scott, J. The Edinburgh repair of isthmic (Group II) spondylolysis. J. Bone Jt. Surg. Br. 69, 491 (1987).
Nicol, R. O. & Scott, J. H. Lytic spondylolysis. Repair by wiring. Spine 11, 1027–1030. https://doi.org/10.1097/00007632-198612000-00011 (1986).
Morscher, E., Gerber, B. & Fasel, J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Arch. Orthop. Trauma Surg. 103, 175–178. https://doi.org/10.1007/BF00435550 (1984).
Tokuhashi, Y. & Matsuzaki, H. Repair of defects in spondylolysis by segmental pedicular screw hook fixation. A preliminary report. Spine 21, 2041–2045. https://doi.org/10.1097/00007632-199609010-00023 (1996).
Karatas, A. F. et al. Comparison of direct pars repair techniques of spondylolysis in pediatric and adolescent patients: Pars compression screw versus pedicle screw-rod-hook. Clin. Spine Surg. 29, 272–280. https://doi.org/10.1097/BSD.0b013e318277cb7d (2016).
Ghobrial, G. M., Crandall, K. M., Lau, A., Williams, S. K. & Levi, A. D. Minimally invasive direct pars repair with cannulated screws and recombinant human bone morphogenetic protein: Case series and review of the literature. Neurosurg. Focus 43, E6. https://doi.org/10.3171/2017.5.Focus17153 (2017).
Shin, M. H., Ryu, K. S., Rathi, N. K. & Park, C. K. Direct pars repair surgery using two different surgical methods: Pedicle screw with universal hook system and direct pars screw fixation in symptomatic lumbar spondylosis patients. J. Korean Neurosurg. Soc. 51, 14–19. https://doi.org/10.3340/jkns.2012.51.1.14 (2012).
Kakiuchi, M. Repair of the defect in spondylolysis. Durable fixation with pedicle screws and laminar hooks. J. Bone Jt. Surg. 79, 818–825. https://doi.org/10.2106/00004623-199706000-00003 (1997).
Raudenbush, B. L., Chambers, R. C., Silverstein, M. P. & Goodwin, R. C. Indirect pars repair for pediatric isthmic spondylolysis: A case series. J. Spine Surg. (Hong Kong) 3, 387–391. https://doi.org/10.21037/jss.2017.08.08 (2017).
Westacott, D. J. & Cooke, S. J. Functional outcome following direct repair or intervertebral fusion for adolescent spondylolysis: A systematic review. J. Pediatr. Orthop. B 21, 596–601. https://doi.org/10.1097/BPB.0b013e328355393d (2012).
Schlenzka, D. et al. Direct repair for treatment of symptomatic spondylolysis and low-grade isthmic spondylolisthesis in young patients: No benefit in comparison to segmental fusion after a mean follow-up of 14.8 years. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deformity Soc. Eur. Sect. Cerv. Spine Res. Soc. 15, 1437–1447. https://doi.org/10.1007/s00586-006-0072-5 (2006).
Schlenzka, D., Seitsalo, S., Poussa, M. & Osterman, K. Operative treatment of symptomatic lumbar spondylolysis and mild isthmic spondylolisthesis in young patients: Direct repair of the defect or segmental spinal fusion?. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 2, 104–112. https://doi.org/10.1007/bf00302712 (1993).
Kumar, N. et al. Is there a place for surgical repair in adults with spondylolysis or grade-I spondylolisthesis-a systematic review and treatment algorithm. Spine J. Off. J. N. Am. Spine Soc. 21, 1268–1285. https://doi.org/10.1016/j.spinee.2021.03.011 (2021).
Pfirrmann, C. W., Metzdorf, A., Zanetti, M., Hodler, J. & Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26, 1873–1878. https://doi.org/10.1097/00007632-200109010-00011 (2001).
Wiltse, L. L., Bateman, J. G., Hutchinson, R. H. & Nelson, W. E. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J. Bone Jt. Surg. 50, 919–926 (1968).
Amin, B. Y., Tu, T. H. & Mummaneni, P. V. Mini-open transforaminal lumbar interbody fusion. Neurosurgical focus 35, Video 2. https://doi.org/10.3171/2013.V2.FOCUS13187 (2013).
Pavlovcic, V. Surgical treatment of spondylolysis and spondylolisthesis with a hook screw. Int. Orthop. 18, 6–9. https://doi.org/10.1007/bf00180169 (1994).
Hanson, D. S., Bridwell, K. H., Rhee, J. M. & Lenke, L. G. Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine 27, 2026–2029. https://doi.org/10.1097/00007632-200209150-00011 (2002).
Lee, G. W., Lee, S. M., Ahn, M. W., Kim, H. J. & Yeom, J. S. Comparison of surgical treatment with direct repair versus conservative treatment in young patients with spondylolysis: A prospective, comparative, clinical trial. Spine J. Off. J. N. Am. Spine Soc. 15, 1545–1553. https://doi.org/10.1016/j.spinee.2015.02.019 (2015).
Chen, S. et al. Global, regional and national burden of low back pain 1990–2019: A systematic analysis of the Global Burden of Disease study 2019. J. Orthop. Transl. https://doi.org/10.1016/j.jot.2021.07.005 (2021).
Lauber, S., Schulte, T. L., Liljenqvist, U., Halm, H. & Hackenberg, L. Clinical and radiologic 2–4-year results of transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Spine 31, 1693–1698. https://doi.org/10.1097/01.brs.0000224530.08481.4e (2006).
Abou-Madawi, A. M., Ali, S. H. & Abdelmonem, A. M. Local autograft versus iliac crest bone graft PSF-augmented TLIF in low-grade isthmic and degenerative lumbar spondylolisthesis. Glob. Spine J. 12, 70–78. https://doi.org/10.1177/2192568220946319 (2022).
Kim, K. H. et al. Adjacent segment disease after interbody fusion and pedicle screw fixations for isolated L4–L5 spondylolisthesis: A minimum five-year follow-up. Spine 35, 625–634. https://doi.org/10.1097/BRS.0b013e3181bb8168 (2010).
Yamasaki, K. et al. Risk factors of adjacent segment disease after transforaminal inter-body fusion for degenerative lumbar disease. Spine 42, E86-e92. https://doi.org/10.1097/brs.0000000000001728 (2017).
Maragkos, G. A., Atesok, K. & Papavassiliou, E. Prognostic factors for adjacent segment disease after L4–L5 lumbar fusion. Neurosurgery 86, 835–842. https://doi.org/10.1093/neuros/nyz241 (2020).
Debusscher, F. & Troussel, S. Direct repair of defects in lumbar spondylolysis with a new pedicle screw hook fixation: Clinical, functional and Ct-assessed study. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deformity Soc. Eur. Sect. Cerv. Spine Res. Soc. 16, 1650–1658. https://doi.org/10.1007/s00586-007-0392-0 (2007).
Mannion, A. F. et al. ISSLS Prize winner: Long-term follow-up suggests spinal fusion is associated with increased adjacent segment disc degeneration but without influence on clinical outcome: Results of a combined follow-up from 4 randomized controlled trials. Spine 39, 1373–1383. https://doi.org/10.1097/brs.0000000000000437 (2014).
Ishida, K. et al. Spondylolysis repair using a pedicle screw hook or claw-hook system. -a comparison of bone fusion rates. Spine Surg. Relat. Res. 2, 135–139. https://doi.org/10.22603/ssrr.2017-0011 (2018).
Giudici, F., Minoia, L., Archetti, M., Corriero, A. S. & Zagra, A. Long-term results of the direct repair of spondylolisthesis. Eur. Spine J. 20(Suppl 1), S115-120. https://doi.org/10.1007/s00586-011-1759-9 (2011).
Kimura, M. J. S. G. My method of filing the lesion with spongy bone in spondylolysis and spondylolistesis. Seikeigeka Orthop. Surg. 19, 285–296 (1968).
Fan, J., Yu, G. R., Liu, F., Zhao, J. & Zhao, W. D. Direct repair of spondylolysis by TSRH’s hook plus screw fixation and bone grafting: biomechanical study and clinical report. Arch. Orthop. Trauma Surg. 130, 209–215. https://doi.org/10.1007/s00402-009-0897-6 (2010).
Ulibarri, J. A., Anderson, P. A., Escarcega, T., Mann, D. & Noonan, K. J. Biomechanical and clinical evaluation of a novel technique for surgical repair of spondylolysis in adolescents. Spine 31, 2067–2072. https://doi.org/10.1097/01.brs.0000231777.24270.2b (2006).
Deguchi, M., Rapoff, A. J. & Zdeblick, T. A. Biomechanical comparison of spondylolysis fixation techniques. Spine 24, 328–333. https://doi.org/10.1097/00007632-199902150-00004 (1999).
Chung, A. S. et al. Minimum clinically important difference: Current trends in the spine literature. Spine 42, 1096–1105. https://doi.org/10.1097/BRS.0000000000001990 (2017).
Li, Q. et al. Clinical outcomes of isobar TTL system with isthmic bone grafting and pedicle screw-vertebral plate hook with direct repair of defect for lumbar spondylolysis: A matched-pair case control study. Orthop. Surg. 15, 2582–2590. https://doi.org/10.1111/os.13837 (2023).
Zayan, M., Hussien, M. A. & El Zahlawy, H. Pars interarticularis repair using pedicle screws and laminar hooks fixation technique in patients with symptomatic lumbar spondylolysis. SICOT J. 8, 13. https://doi.org/10.1051/sicotj/2022013 (2022).
Inoue, N., Orías, A. A. E. & Segami, K. Biomechanics of the lumbar facet joint. Spine Surg. Relat. Res. 4, 1–7. https://doi.org/10.22603/ssrr.2019-0017 (2020).
Suh, K. T. et al. Posterior lumbar interbody fusion for adult isthmic spondylolisthesis: A comparison of fusion with one or two cages. J. Bone Jt. Surg. Br. Vol. 90, 1352–1356. https://doi.org/10.1302/0301-620x.90b10.21078 (2008).
Acknowledgements
We would like to acknowledge Professor Junying Tian from College of Foreign Languages of Chongqing Medical University for his assistance in proofreading the manuscript.
Author information
Authors and Affiliations
Contributions
Y-J. G. and Q.Z. designed the study and co-ordinated the project. Y-J.G., P.L. and C.Z collated the data and produced the first draft of the manuscript and subsequent revisions.L-C. L.and L.L prepared Figs. 1–2 and L-H.L. and L-C.L. prepared Tables 1–6. Y-J.G. and L-C.L. assisted with participant assessments and collation of data. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gao, Y., Zhao, C., Li, P. et al. Comparative study of direct pars repair versus transforaminal lumbar interbody fusion for low grade isthmic spondylolisthesis: a retrospective analysis. Sci Rep 15, 19560 (2025). https://doi.org/10.1038/s41598-025-03462-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03462-1