Abstract
The six-minute walk test (6MWT) is a convenient method for evaluating functional capacity in daily living. We evaluated the prognostic value of the 6MWT in patients with cardiovascular disease to predict the incidence of MACE. Patients with prevalent cardiovascular diseases were enrolled in the cardiac rehabilitation registry. 6MWT was measured at baseline, and incidences of all-cause death, coronary intervention, admission due to heart failure, and stroke were monitored. Odds ratios (OR) and hazard ratios (HR) for MACE were compared, and cutoff distance of 6MWT according to endpoint diseases were calculated for both common and disease-specific thresholds. A total of 1,374 patients were enrolled, with 105 (7.6%) MACE events. The MACE group walked shorter 6MWT distances (329 ± 110 m) compared to controls (396 ± 114 m, p < 0.001). Each 50-meter increase in 6MWT distance was associated with a lower OR (0.78, p < 0.001) and HR (0.83, p < 0.001) for the MACE. Cutoff distance for MACE was 392 m, with sensitivity of 76% and specificity of 53%. The disease-specific cutoffs provided better classification of individual outcomes for all-cause death, coronary intervention, and stroke. The 6MWT has a prognostic value for predicting MACE in patients with prevalent cardiovascular diseases. Different thresholds should be applied for specific diseases to enhance the predictive accuracy.
Similar content being viewed by others
Introduction
Advances in optimal medical therapies and interventions have made long-term management and secondary prevention increasingly important in patients with cardiovascular disease1,2. Various methods have been proposed to evaluate the risks and prognoses of these patients3,4,5.
Established scoring systems3,4 from large cohorts, such as the Framingham Study, offer intuitive and more precise predictions. However, these approaches require complex baseline information3 including laboratory results, imaging techniques, and the involvement of healthcare professionals. Functional exercise capacity tests are also known to provide comprehensive insights, particularly for patients with cardiopulmonary diseases5,6. Although the cardiopulmonary exercise test (CPET) is accepted as a standard, it may be challenging for some patients with severe conditions because the test requires patients to reach the maximum level of effort5.
The 6-minute walk test (6 MWT) is another method for measuring functional exercise capacity, which closely represents activities of daily living7. Its advantage is that the test is applicable to almost everyone who can walk on a flat surface, and there is no need for special equipment or professional assistance7. Although the 6 MWT differs from the CPET in that it measures submaximal effort and thereby provides only limited information6, studies have shown significant correlations between these tests6,8. Previous studies have explored the prognostic value of the 6 MWT in patients with cardiovascular diseases9,10,11,12. Bittner et al. showed that patients with heart failure (HF) who walked shorter distances had a more than 3-fold higher mortality risk than those who walked longer distances (p = 0.01)9, and Roul et al. proposed that poor prognosis of HF was more evident in patients who walked less than 300 m (p = 0.013)10.
While these studies consistently suggested that greater distances walked in the 6 MWT were associated with better outcomes, many of them focused on mortality as an endpoint in HF patients9,11. In contrast, studies that considered the outcome as a composite of major adverse cardiovascular events (MACE) have shown different results12,13, calling for further research.
In this study, we aimed to evaluate the prognostic value of the 6-minute walk test in patients with known cardiovascular disease for major adverse cardiovascular events and to provide cutoff values of the distance covered in the test for better prognosis of the endpoints.
Results
Clinical characteristics of study participants
A total of 1,374 patients were enrolled in the registry (Table 1), and 105 experienced MACE during the study period of 2015 and 2020. The median ages were 69 and 62 years (p < 0.001), and the proportions of male patients were 78% and 79% in the MACE and control groups (p = 0.910), respectively. In both groups, acute coronary syndrome was the most common primary diagnosis, accounting for more than half of the cases (66% in the MACE group and 71% in the control group, p = 0.239). It was followed by stable angina, which comprised 27% of cases in the MACE group and 20% in the control group (p = 0.092). The proportion of patients with HF were similar in both groups (7% in the MACE group and 6% in the control group, p = 0.806). The median follow-up periods were 686 and 572 days for the MACE and control groups (p = 0.058), respectively, and the median time to an event in the MACE group was 236 days. Among patients with MACEs, the most common event was coronary intervention (60%), and 18 deaths were recorded.
Distance walked in the six-minute walk test at baseline
Patients who experienced any MACE had originally walked a significantly shorter distance in the 6 MWT (328.8 ± 109.7 m) than controls (396.2 ± 114.1 m, p < 0.001, Table 2). The largest difference was observed in patients who died, with a reduction of 137.9 m, followed by stroke patients, with a reduction of 113 m. This difference was statistically significant regardless of the type of MACE.
Correlation and effect size of the six-minute walk test and subsequent major adverse cardiovascular events
Each 50-meter increase in the 6 MWT distance was associated with a lower odds ratio (OR) for MACE, both as a composite and for individual endpoints (Table 3). The OR were particularly low for mortality (0.621, p < 0.001) and stroke (0.673, p = 0.030). When controlled for age, sex, and underlying comorbidities, the negative correlation between the distance walked and composite MACE, as well as for death and coronary intervention, remained robustly significant. However, the correlation between admission due to HF and stroke was no longer significant in the adjusted model.
The decreased risk for patients who walked a greater distance was consistent for composite MACE in both the unadjusted crude (HR = 0.831, p < 0.001) and adjusted models (HR = 0.852, p = 0.001 adjusted for age and sex; HR = 0.857, p = 0.001 adjusted for age, sex, and comorbidities). For individual endpoints, risk reduction was statistically significant only for death in all models, and for coronary intervention in the unadjusted model (Table 3).
Cutoff distances in the six-minute walk test for outcome prediction
The distance to predict any MACE was estimated to be 392 m (Table 4), with a sensitivity of 76% and specificity of 53%. The cut-off was particularly strict for stroke (280 m) and death (320 m), providing higher validity indices. The sensitivity and specificity were 80% and 85% for stroke, and 78% and 75% for death, respectively.
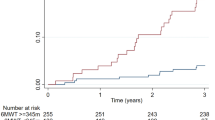
Based on this estimation, the cutoff distance of the composite MACE (392 m) provided the correct classification for all clinical outcomes, except HF admission (Fig. 1, panel a). When disease-specific cutoffs were applied to the corresponding diseases instead of using a common threshold of 392 m, a more reliable classification was observed based on lower log-rank p-values for all endpoints, except HF admission. Although not statistically significant, the better prognostic value of using a disease-specific cutoff could still be inferred in HF admission as well, in that the log-rank chi-square statistic was enhanced from 2.087 to 3.545, and the log-rank p-value was reduced from 0.148 to 0.059.
Kaplan-Meier curves showing classification for individual clinical outcomes when (a) using the cutoff distance of six-minute walk test from composite major adverse cardiovascular outcomes (392 m) as a common threshold, and (b) using the disease-specific cutoff distance (320 m for death, 392 m for coronary intervention, 370 m for heart failure admission, and 280 m for stroke) for corresponding endpoints.
Discussion
This study aimed to evaluate the prognostic value of the 6 MWT in predicting MACE in patients with prevalent cardiovascular disease. Our findings show that the MACE group had significantly shorter baseline 6 MWT distances, particularly among patients who died or had a stroke, than the control group, which did not experience further events. Additionally, the results indicated that the 6 MWT distance was a robust predictor of MACE and all-cause mortality, with greater distances providing protection. The cutoff distance for predicting composite MACE was estimated to be 392 m, with a sensitivity of 75% and a specificity of 53%.
The relationship between 6 MWT results and outcomes in individuals without prevalent cardiovascular diseases and in acute or chronic patients has been suggested in previous studies6,14,15. However, there have been discrepancies in the prediction of individual MACE endpoints6,14. Our study showed a protective effect of the 6 MWT distance not only against death (HR = 0.662, p < 0.001, per 50-meter increase), but also against coronary intervention (HR = 0.879, p = 0.016) when considering the 6 MWT result as a single predictor. However, the statistical significance of the protective effect was lost for coronary intervention in the adjusted hazard models as well as for HF admission and stroke in the adjusted logistic and all hazard models.
Perez de Arenada et al. reported that patients who walked > 300 m on the 6 MWT had a 5.6%p lower incidence of postoperative stroke16. However, the study also showed that based on the Euroscore classification, an established reference for postoperative risk evaluation, the 6 MWT did not have a discriminative value in the low-to medium-risk Euroscore groups (P = 0.34), except in the high-risk group (P = 0.03)16. Another study on patients with previously diagnosed cardiovascular conditions8, similar to our study population, found that traditional risk factors such as age, sex, and comorbidities such as hypertension or diabetes alone could provide approximately 69% predictability for MACE. When the 6 MWT was considered as an additional prognostic factor, the discrimination improvement was 4.1%, which was lower than the 4.8% improvement with the addition of NT-proBNP. These results can be interpreted in two ways: the 6 MWT measures integrated and global function rather than specific disease-related risks7, and the heterogeneity of study populations, such as healthy adults, patients with ischemic heart disease, and patients with heart failure, may possess different baseline risks for MACE prognosis13,17.
The prognostic power of the 6 MWT for MACE varies depending on the specific endpoint disease. Stroke and death exhibited the highest AUC values. Considering that ambulation is a major risk factor for stroke18 and that mortality reflects a general decline in physical function, it is expected that the 6 MWT, which measures the overall functional status in daily living7, will provide better predictions of these outcomes. In contrast, HF has a broad-spectrum pathophysiology and is viewed as a syndrome influenced by various peripheral factors rather than a single disease entity19,20. The complex etiology of HF may dilute the implications of the 6 MWT compared to other risk factors, resulting in a relatively low predictive power.
Similarly, the necessity for different cutoffs for different outcomes should be considered when estimating the prognosis. In studies reporting contrasting results on the prognostic power of the 6 MWT10,21, many commonly used a 6 MWT distance of 300 m as an empirical threshold, regardless of the specific outcomes. However, Yazdanyar et al. reported that the increased HR of shorter 6 MWT distance was only statistically significant at a certain level of quintiles and that the specific quintile showing significance varied by endpoint disease14. For example, the HR for all-cause mortality increased in participants below the third lowest quintile (373 m, Confidence interval of HR: 1.3–2.4), while mortality due to cardiovascular disease and ischemic heart disease increased below the second lowest (338, CI: 1.2–3.4) and only at the lowest quintile (290 m, CI: 1.4–4.8), respectively14. Similarly, the Kaplan-Meier curve in our study showed a more reliable classification for each endpoint when disease-specific cutoffs were applied to the corresponding diseases.
Our study has some limitations. First, the total number of identified MACEs was only 7.6% (105 cases) of the registered patients, resulting in an even smaller number of specific endpoint diseases. This is because of the single-center nature of the study, and some cases might have been undetected if the event had occurred in other hospitals. Findings that were not statistically significant in our study but were suggested otherwise in previous studies, such as HF admission22,23, could be attributed to insufficient statistical power for the same reason. Second, despite our best efforts, there may have been some discrepancies in the exact test protocol, which is crucial for functional capacity tests19,21,24. For example, the length of the test corridor was 26 m, requiring an average of 12 stop-and-turn cycles for the MACE group. However, fewer turns and longer straight distances were closely related to better 6 MWT results25,26. Third, the 6 MWT was performed only once at the baseline. Changes in the distance walked through repeated measures during follow-up may provide a better understanding.
We conclude that, in patients with prevalent cardiovascular diseases, the 6 MWT has prognostic value for predicting subsequent MACE incidence. However, different thresholds must be applied to estimate the risk of specific diseases. The 6 MWT may assist in earlier screening and identification of high-risk outcomes and provide valuable insights for clinical decision-making from a preventive perspective, as well as patient education.
Methods
Study population
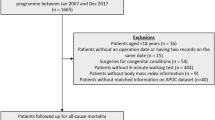
This was a retrospective observational study. Between 2015 and 2020, patients who were admitted to, received outpatient care from, or were referred to the cardiology center at the Korea University Guro Hospital were considered eligible for the study. Among these patients, inclusion criteria required a primary diagnosis of cardiovascular disease, including acute coronary syndrome (e.g., myocardial infarction or unstable angina), stable angina, HF, or peripheral artery disease. Exclusion criteria included patients aged < 20 years, pregnant women, and patients unable to cooperate with the 6 MWT due to conditions such as hemodynamic instability or ambulatory difficulties.
Baseline six-minute walk test
The 6 MWT was performed when the patient was stable enough to complete the procedure, in order to minimize potential biases related to the acute phases of their condition. For admitted patients, the test was conducted either after the completion of their scheduled management and clearance for discharge, or during their first follow-up visit. For outpatients, the test was conducted at the time they were first referred to the clinic. The test was conducted according to the standard protocol7. The patients were instructed by a technician to walk along a designated 26-meter path in a hospital corridor. No walking practice was performed before the test. Patients were instructed to walk as far as possible at their own pace for six minutes. Throughout the test, technicians encouraged the patients every minute using standard phrases. The test was concluded either after six minutes or when the patient chose to stop, and the distance walked to that point was recorded as the baseline 6 MWT distance.
Endpoint presentation
The enrollment to the study registry did not affect the patients’ management for their prevalent cardiovascular condition (e.g., guideline-directed medical therapy for patients with HF). After the termination of the registry, medical records were reviewed to identify MACE, including all-cause death, coronary intervention, and admission due to HF or stroke that occurred between the enrollment to the registry and the end of 2020. Observation time varied for each patient depending on their entry date into the registry and whether they experienced a designated outcome event. If multiple events occurred in the same patient during their follow-up period, only the first event was considered.
Patients who experienced MACE were assigned to the MACE group, whereas those with no identified events by the end of the study were assigned to the control group. For patients in the MACE group, the time from enrollment to the date of the first event was recorded. In the control group, the total observation period was defined as the time from entry into the registry until the last follow-up visit.
Statistical analysis
The distance walked in the 6 MWT was analyzed as the entire MACE as a composite, as well as individual outcomes, such as all-cause death, coronary intervention, admission due to HF, or stroke. The mean distances between the MACE and control groups were compared, and the differences were tested using an independent t-test. To investigate whether the 6 MWT distance influenced the occurrence of MACE, odds ratios (OR) were calculated using logistic regression. Hazard ratios (HR) were calculated using Cox proportional hazards regression to measure and compare the risk of MACE. To distinguish the effect size of the 6 MWT distance more clearly, the distance, measured in meters, was converted to 50-m units for regression analyses. Both regressions were repeated with a crude model considering the 6 MWT distance as a single predictor, as well as with adjusted models controlled for patients’ age and sex or for age, sex, and comorbidities such as hypertension, diabetes, or dyslipidemia. Area under the curve (AUC) analysis was used to estimate the cutoff distances of the 6 MWT, and validity indices, including sensitivity and specificity, were calculated for MACE as a composite as well as for individual endpoint diseases. Kaplan-Meier curves were plotted to examine the difference in classifying the endpoints between using a common threshold of composite MACE and disease-specific cutoffs for the corresponding diseases.
Ethics
This study used previously collected and anonymized data from the registry of patients who underwent the 6 MWT. The overall study design was reviewed by the Institutional Review Board of Korea University Guro Hospital and granted an exemption from additional informed consent (2018GR0295).
Data availability
Informed consent from study participants does not include permission to share data with other researchers or institutions. However, the availability of data can be considered on a case-by-case basis upon request to the corresponding author.
References
Smith, S. C. et al. AHA consensus panel statement. Preventing heart attack and death in patients with coronary disease. The secondary prevention panel. J. Am. Coll. Cardiol. 26, 292 (1995).
LaBresh, K. A., Ellrodt, G., Gliklich, A., Liljestrand, R., Peto, R. & J. & Get with the guidelines for cardiovascular secondary prevention: Pilot results. Arch. Intern. Med. 164, 203–209 (2004).
Cameli, M. et al. Prognosis and risk stratification of patients with advanced heart failure (from PROBE). Am. J. Cardiol. 124, 55–62 (2019).
D’agostino, R. B. et al. Primary and subsequent coronary risk appraisal: New results from the Framingham study. Am. Heart J. 139, 272–281 (2000).
Arena, R. et al. Development of a ventilatory classification system in patients with heart failure. Circulation 115, 2410–2417 (2007).
Guazzi, M., Dickstein, K., Vicenzi, M. & Arena, R. Six-minute walk test and cardiopulmonary exercise testing in patients with chronic heart failure: A comparative analysis on clinical and prognostic insights. Circ. Heart Fail. 2, 549–555 (2009).
Crapo, R. O. et al. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir Crit. Care Med. 166, 111–117 (2002).
Beatty, A. L., Schiller, N. B. & Whooley, M. A. Six-minute walk test as a prognostic tool in stable coronary heart disease: Data from the heart and soul study. Arch. Intern. Med. 172, 1096–1102 (2012).
Bittner, V. et al. Prediction of mortality and morbidity with a 6-minute walk test in patients with left ventricular dysfunction. JAMA J. Am. Med. Assoc. 270, 1702–1707 (1993).
Roul, G., Germain, P. & Bareiss, P. Does the 6-minute walk test predict the prognosis in patients with NYHA class II or III chronic heart failure? Am. Heart J. 136, 449–457 (1998).
Grundtvig, M., Eriksen-Volnes, T., Ørn, S., Slind, E. K. & Gullestad, L. 6 Min walk test is a strong independent predictor of death in outpatients with heart failure. ESC Heart Fail. 7, 2904–2911 (2020).
Coulshed, A., Coulshed, D. & Pathan, F. Systematic review of the use of the 6-minute walk test in measuring and improving prognosis in patients with ischemic heart disease. CJC Open 5, 816–825 (2023).
Cavero-Redondo, I. et al. Accuracy of the 6-minute walk test for assessing functional capacity in patients with heart failure with preserved ejection fraction and other chronic cardiac pathologies: Results of the ExIC-FEp trial and a meta-analysis. Sport Med. Open 10 (2024).
Yazdanyar, A. et al. Association between 6-minute walk test and all-cause mortality, coronary heart disease-specific mortality, and incident coronary heart disease. J. Aging Health 26, 583–599 (2014).
Zielińska, D., Bellwon, J., Rynkiewicz, A. & Elkady, M. A. Prognostic value of the six-minute walk test in heart failure patients undergoing cardiac surgery: A literature review. Rehabil. Res. Pract. 2013, 1–5 (2013).
De Arenaza, D. P. et al. Preoperative 6-minute walk test adds prognostic information to Euroscore in patients undergoing aortic valve replacement. Heart 96, 113–117 (2010).
Rostagno, C. Six-minute walk test: Independent prognostic marker? Heart 96, 97–98 (2010).
Chiu, H. T. et al. Effect of functional status on survival in patients with stroke: Is independent ambulation a key determinant? Arch. Phys. Med. Rehabil. 93, 527–531 (2012).
Sharma, R. & Anker, S. D. The 6-minute walk test and prognosis in chronic heart failure—the available evidence. Eur. Heart J. 22, 445–448 (2001).
Clark, A. L., Poole-Wilson, P. A. & Coats, A. J. Exercise limitation in chronic heart failure: central role of the periphery. J. Am. Coll. Cardiol. 28, 1092–1102 (1996).
Opasich, C. et al. Six-minute walking performance in patients with moderate-to-severe heart failure; is it a useful indicator in clinical practice? Eur. Heart J. 22, 488–496 (2001).
McCabe, N., Butler, J., Dunbar, S. B., Higgins, M. & Reilly, C. Six-minute walk distance predicts 30-day readmission after acute heart failure hospitalization. Hear. Lung J. Acute Crit. Care 46, 287–292 (2017).
Ferreira, J. P. et al. Clinical correlates and outcome associated with changes in 6-minute walking distance in patients with heart failure: Findings from the BIOSTAT-CHF study. Eur. J. Heart Fail. 21, 218–226 (2019).
Guyatt, G. H. et al. Effect of encouragement on walking test performance. Thorax 39, 818–822 (1984).
Sciurba, F. et al. Six-minute walk distance in chronic obstructive pulmonary disease: Reproducibility and effect of walking course layout and length. Am. J. Respir Crit. Care Med. 167, 1522–1527 (2003).
Beekman, E. et al. Course length of 30 metres versus 10 metres has a significant influence on six-minute walk distance in patients with COPD: An experimental crossover study. J. Physiother. 59, 169–176 (2013).
Author information
Authors and Affiliations
Contributions
All authors made more than one substantial contributions to the study and qualify the authorship. Conception and design of the work: S.S., S.L., E.K.; Acquisition of data: S.S., J.J., J.E.L., S.H.P., D.O.K., E.J.P., D.L., J.Y.C., S.L., S.Y.R., J.O.N., C.U.C., J.W.K., S.W.R., C.G.P., E.J.K.; Analysis and interpretation of data: S.S.; Drafting the work: S.S. All authors provided critical review for important intellectual content and approved the final version to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was performed in accordance with the ethical standards of Declaration of Helsinki. The overall study design was reviewed and approved by the Institutional Review Board of Korea University Guro Hospital (2018GR0295).
Consent to participate
All participants were informed of the purpose and process of the walk test at the time of their testing. Informed consent was waived by the institutional review board at the time of data analysis because the study retrospectively used previously obtained and anonymized data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sohn, S., Jeon, J., Lee, J.E. et al. Prognostic value of the six-minute walk test in patients with cardiovascular disease. Sci Rep 15, 20817 (2025). https://doi.org/10.1038/s41598-025-04480-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-04480-9