Abstract
Healthcare workers frequently encounter demanding schedules, shift work, and significant psychological stressors, all of which can contribute to gastrointestinal disturbances and sleep irregularities. Although research has established that stress and shift work are independent risk factors for gastrointestinal discomfort and insomnia, the direct link between these two conditions in healthcare workers remains insufficiently explored. In this cross-sectional study, we recruited 372 healthcare workers from 6 public hospitals in Quanzhou via an online survey. Gastrointestinal and insomnia symptoms were measured using the Gastrointestinal Symptom Rating Scale (GSRS) and the Insomnia Severity Index (ISI), respectively, and analyzed via univariate and multivariate logistic regression models. Overall, 40.6% of participants reported insomnia symptoms. The GSRS total score was positively associated with insomnia both before (OR 1.18, 95% CI 1.12–1.25) and after adjustment for confounders including age, gender, anxiety, depression, somatization, and weekly night shift count (adjusted OR 1.07, 95% CI 1.00–1.15). These findings underscore a significant relationship between gastrointestinal symptoms and insomnia among healthcare workers, highlighting the need for targeted interventions to improve both GI health and sleep quality, thereby enhancing work efficiency and the overall quality of patient care.
Similar content being viewed by others
Introduction
Insomnia is a prevalent health issue characterized by difficulty initiating or maintaining sleep or early-morning awakening, accompanied by dissatisfaction with sleep quantity or quality and clinically significant daytime impairment, which can severely impact an individual’s daily functioning and overall quality of life1. Chronic sleep problems may also increase the risk of cardiovascular disease, metabolic syndrome, and cognitive decline2. Healthcare workers are frequently exposed to prolonged work hours, rotating shifts, and heightened psychological stress, placing them at increased risk for sleep disturbances3. Evidence-based data suggest a high prevalence of insomnia symptoms among healthcare professionals, with several meta-analyses and large-scale studies indicating that approximately 36.1–43.7% of healthcare workers report clinically significant insomnia symptoms4,5. Such impaired sleep can adversely impact cognitive functioning, decision-making, and overall job performance, ultimately affecting patient safety and care quality6.
In parallel, gastrointestinal (GI) symptoms, which include abdominal pain, bloating, and altered bowel habits, are also prevalent among healthcare workers. The prevalence of these symptoms often exceeds the rates observed in the general population7. Studies have reported that up to 31–48% of healthcare workers may experience frequent GI complaints, potentially linked to irregular meal patterns, limited time for breaks, high psychological demands, and disruption of circadian rhythms due to shift work8. These GI symptoms not only reduce quality of life but may also compromise the ability to deliver optimal patient care9.
While substantial research has documented the association between poor sleep and GI symptoms in the general population10, evidence specifically targeting healthcare workers remains limited. A few studies have hinted at this relationship in certain subgroups, such as nurses, but most have not systematically accounted for relevant confounders, including anxiety, depression, and shift work frequency. These factors are known to be common and impactful in high-stress medical environments9,11. Moreover, previous investigations often focused on either insomnia or GI disturbances independently, rather than examining their concurrent interplay in this occupational cohort12. Given the prevalence of gastrointestinal symptoms and insomnia among healthcare workers and their known correlation in the general population, this study aims to explore the relationship between gastrointestinal symptoms and insomnia in healthcare workers.
Materials and methods
This study received formal approval from the Medical Ethics Committee of Quanzhou City First Hospital, approval number: 2023[185]. All methods were carried out in accordance with the Declaration of Helsinki and relevant guidelines and regulations. Written informed consent was obtained from all participants.
Study design and participants
This cross-sectional study was conducted from August 25 to November 30, 2023. We used a convenience sampling approach to recruit healthcare workers from 6 public hospitals in Quanzhou. For the purposes of this study, “healthcare workers” included doctors (both clinical physicians and those working in medical technology departments), nurses, and other allied health professionals. The complete questionnaire is provided in Supplementary Materials. Inclusion criteria: (1) Healthcare worker; (2) Age between 18 and 65, no gender restrictions. Exclusion criteria: (1) History of gastrointestinal malignancy; (2) History of gastrointestinal surgery (excluding colorectal polypectomy); (3) Evidence of peptic ulcer or erosive esophagitis within the last six months on endoscopy; (4) Chronic pancreatitis, inflammatory bowel disease, or bowel obstruction; (5) Severe organ damage and complications (such as cirrhosis, uremia) and severe cardiovascular, respiratory, or endocrine disease; (6) History of malignancy in other systems or organs; (7) Autoimmune diseases such as systemic lupus erythematosus and ankylosing spondylitis; (8) Long-term use of sleeping pills, anti-anxiety, or antidepressant medication; (9) Pregnant or breastfeeding women.
Data were collected via an online platform, Wenjuanxing (https://www.wjx.cn), which is widely used for academic and clinical research in China13. The questionnaire for this study was hosted at: https://www.wjx.cn/vm/wvkZGfj.aspx. The study team collaborated with the administrative offices of the participating hospitals to disseminate the survey link and/or a Quick Response (QR) code to eligible individuals through departmental email lists, hospital intranet portals, and dedicated WeChat groups. Upon accessing the online link or QR code, participants were presented with an introductory page outlining the study objectives, confidentiality statements, and an electronic consent form. Only those who confirmed consent were directed to the main questionnaire. All participants completed the questionnaire using their mobile phones or personal computers. Duplicate submissions were minimized by restricting each participant’s unique survey link/QR code access.
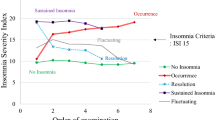
Assessment of insomnia
The Insomnia Severity Index (ISI) is used to assess the severity of insomnia symptoms. This scale consists of seven items, each evaluating the severity and impact of insomnia symptoms on daily life over the past two weeks. Each item is rated from 0 (no problem) to 4 (very severe problem). The total score ranges from 0 to 28, with higher scores indicating more severe insomnia symptoms. In accordance with the original ISI validation studies, scores are conventionally stratified as follows: normal (0–7), sub-threshold insomnia (8–14), moderate insomnia (15–21), and severe insomnia (22–28)14. For the present study, and consistent with the recommendation for community samples in the 2023 European Insomnia Guideline15, we defined insomnia for primary analyses as ISI ≥ 10.
Assessment of gastrointestinal symptoms
The Gastrointestinal Symptom Rating Scale (GSRS) is commonly used to evaluate the severity of symptoms in patients with functional gastrointestinal disorders (e.g., functional dyspepsia, irritable bowel syndrome). The GSRS, developed by Svedlund et al. in 1988, assesses multiple aspects of gastrointestinal symptoms, including reflux, abdominal pain, bloating, constipation, and diarrhea. Designed as a self-assessment scale, it allows patients to evaluate the severity of their symptoms based on recent experiences16. A higher GSRS score indicates more severe gastrointestinal symptoms. Details on how the GSRS is calculated are provided in the Supplementary Materials.
Covariates
Covariates considered in this study included age, gender, marriage, body mass index (BMI), education, monthly salary, smoking status, drinking status, weekly night shift count, comorbidity, family history of cancer, profession, department, unhealthy diet, weekly exercise frequency, anxiety, depression, and somatic symptom disorder. BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2). Smoking was defined as a habit of smoking more than one cigarette daily. Drinking was defined as a habit of drinking alcohol more than once a week17. Comorbidity were defined as having hypertension, diabetes, or heart disease. An unhealthy diet was defined as frequently consuming barbecued or fried foods (≥ 1 time/week) or preferring salty flavors; otherwise, it was considered a healthy diet. Anxiety was defined as a total score of ≥ 5 on the Generalized Anxiety Disorder Scale (GAD-7). This scale consists of seven items to assess the frequency of anxiety symptoms over the past two weeks. Each item is rated from 0 (never) to 3 (almost every day), and the total score ranges from 0 to 21, with higher scores indicating more severe functional impairment due to anxiety. Scores of 5–9 and ≥ 10 represent mild and moderate-to-severe anxiety symptoms, respectively18. Depression was defined as a total score of ≥ 5 on the Patient Health Questionnaire-9 (PHQ-9)19. The scale assesses the degree of depressive symptoms experienced over the past two weeks, with each item rated from 0 (never) to 3 (almost every day). The total score ranges from 0 to 27, with higher scores indicating more severe depressive symptoms. Prior literature indicates scores of 5–9 represent mild depressive symptoms, and scores ≥ 10 represent moderate-to-severe depressive symptoms20. Somatic symptom disorder (SSD) was defined as a total score of ≥ 30 on the Self-reported Somatic Symptom Scale-China (SSS-CN)21. In clinical practice, SSD can be divided into mild, moderate, and severe levels based on scale scores: mild (30–39 points), moderate (40–59 points), and severe (over 60 points).
Statistical analysis
The sample size was calculated using G*Power software (Version 3.1.9.7, Heinrich-Heine-Universität Düsseldorf, Germany) based on logistic regression. A minimum of 221 participants was required to achieve 80% statistical power (α = 0.05) to detect an odds ratio of 1.5 for the association between gastrointestinal symptoms and insomnia22. The calculation assumed a baseline probability of 0.4 for the insomnia at the mean value of the GSRS score and an increase to 0.5 with one standard deviation increase in the independent variable, accounting for an R-squared of 0.1. The achieved power was 79.8%. All analyses were conducted using R statistical software (version 4.2.1; http://www.R-project.org, The R Foundation) and Free Statistics software (version 1.9; Beijing, China, http://www.clinicalscientists.cn/freestatistics)23. Continuous variables were expressed as mean ± standard deviation (SD) for normally distributed data or as median (interquartile range) for skewed data. Categorical variables were described as counts (percentages). Between-group differences were compared using the independent samples t-test, chi-square test, and Mann–Whitney U test, as appropriate. The relationship between gastrointestinal symptoms and insomnia was analyzed using univariate and multivariate logistic regression. The covariates included in the model were determined based on clinical expertise, univariate screening results (P-value < 0.05), or whether they led to a change in the effect estimate > 10%. Interactions between subgroups were examined through likelihood ratio tests. A P-value < 0.05 was considered statistically significant.
Results
Baseline characteristics of the study population
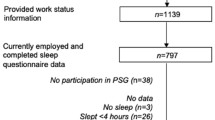
The online survey recruited 380 participants. After excluding three participants who met the exclusion criteria, two who were missing GSRS data, and three who were missing covariate data (age, smoking status, and drinking status), 372 participants were included in our analysis (Fig. 1). Table 1 presents the clinical characteristics of the study population based on insomnia symptoms. The participants had an average age of 37.8 ± 8.0 years, and 159 (42.7%) were male. At baseline, participants with insomnia symptoms had more weekly night shifts count, higher rates of anxiety, depression, and SSD, and nurses were more prone to insomnia than doctors.
Effect of gastrointestinal symptoms on the risk of insomnia in healthcare workers
Univariate analysis revealed that the weekly night shifts count, education, profession, anxiety, depression, SSD, and GSRS total score were associated with insomnia risk (Table 2). The results of the multivariate logistic regression analysis are shown in Table 3. In the unadjusted model, the GSRS total score was positively correlated with insomnia risk (OR 1.18; 95% CI 1.12–1.25). In Model 1, after adjusting for age and gender, the results remained consistent (OR 1.18; 95% CI 1.12–1.25). Model 2, which adjusted for variables in Model 1 as well as anxiety, depression, SSD, and weekly night shift count (these confounders were selected based on their association with the outcomes of interest or a change in effect estimate of more than 10%), still showed a positive correlation (OR 1.10; 95% CI 1.03–1.16). Model 3, which adjusted for the variables in Model 2 plus marriage, BMI, education, monthly salary, smoking status, drinking status, comorbidity, family history of cancer, profession, department, unhealthy diet, and weekly exercise Frequency, still demonstrated a positive correlation (OR 1.07; 95% CI 1.00–1.15).
Subgroup analysis
In this study, we performed stratified analyses and interaction tests to determine whether the association between the GSRS total score and insomnia incidence was consistent across several subgroups. When stratified by age, gender, anxiety, depression, SSD, and profession, a consistent positive correlation was observed, and no significant interactions were found in any subgroup (Fig. 2). This indicates that the impact of gastrointestinal symptoms on insomnia outcomes is stable and not influenced by changes in covariates.
Subgroup analyses for the association of GSRS total score and insomnia. GSRS Gastrointestinal Symptom Rating Scale, SSD somatic symptom disorder. Adjusted for gender, age, BMI, marriage, education, profession, department, hospital grade, monthly salary, comorbidity, smoking status, drinking status, unhealth diet, weekly night shift count, weekly exercise frequency, anxiety, depression, SSD.
Discussion
This study examined the association between gastrointestinal symptoms and insomnia among healthcare workers and found a significant positive correlation between the two. That is, an increase in the severity of gastrointestinal symptoms was associated with a higher risk of insomnia. This finding complements existing literature on the relationship between gastrointestinal symptoms and insomnia in both general and specific populations while providing new insights into this relationship in the unique occupational group of healthcare workers.
Association between gastrointestinal symptoms and insomnia
A growing body of research has consistently highlighted the co-occurrence of GI symptoms and sleep disturbances in both community and occupational settings. For example, Gastrointestinal distress has been positively correlated with sleep disturbances, with pain, discomfort, and nocturnal gastrointestinal events potentially disrupting sleep continuity24. Additionally, One study examined the combined effects of psychological stress and insufficient sleep on GI function, revealing that elevated stress markers and reduced sleep duration significantly predicted GI complaints among office workers25. Although this study did not specifically target healthcare professionals, the high-pressure work environment and irregular schedules it described mirror those experienced by clinical staff, implying a similar pathophysiological trajectory in which stress-induced autonomic dysregulation could potentiate GI dysfunction and sleep impairment.
Notably, other investigations have identified specific disorders, such as irritable bowel syndrome (IBS), as being significantly intertwined with both insomnia and nonrestorative sleep26. One plausible mechanism is that inflammatory and nociceptive processes associated with IBS can heighten nocturnal arousal, leading to frequent awakenings and unrefreshing sleep. Conversely, chronic insufficient sleep may worsen GI symptoms by amplifying systemic inflammation and stress hormone levels, thus perpetuating a “vicious cycle” of exacerbated GI distress and cumulative sleep loss27. Taken collectively, these studies reinforce the notion that GI symptoms and sleep disturbances are linked by shared biopsychosocial factors, including autonomic dysfunction, heightened nociception, maladaptive coping mechanisms, and anxiety. They also underscore the need to move beyond viewing GI disturbances and insomnia as isolated conditions and instead regard them as mutually reinforcing domains, particularly in occupations (such as healthcare) where stress and irregular schedules further amplify this bidirectional interaction.
The uniqueness of gastrointestinal symptoms and insomnia in healthcare workers
In contrast, studies focusing on healthcare workers are relatively scarce. Our findings align with a study of South Korean nurses, which found that long working hours and night shifts could lead to poor sleep quality and digestive system problems among nurses11. Moreover, due to their high-stress work environment and irregular working hours, healthcare workers are more prone to gastrointestinal symptoms like indigestion and stomach pain, further exacerbating insomnia28. This underscores that the relationship between gastrointestinal symptoms and insomnia may differ in healthcare workers compared to the general population, especially given the role of work-related stress and lifestyle factors.
Furthermore, the persistent mental stress and emotional burden faced by healthcare workers may also be a key factor. Stress and emotional issues are common triggers of gastrointestinal symptoms and major contributors to insomnia. Our univariate analysis showed that anxiety, depression, and SSD were associated with insomnia risk. Previous research demonstrated that short sleep duration and poor sleep quality significantly affected the mental health of military healthcare workers29. Another study revealed that sleep disorders are closely related to the mental health issues of healthcare workers, particularly during the COVID-19 pandemic, where healthcare workers with sleep disorders had 3.74 times the risk of psychological problems compared to those without sleep disorders30. When facing gastrointestinal symptoms and insomnia, healthcare workers may need to emphasize stress management and emotional regulation due to the unique nature of their occupational stress.
This study focused on doctors and nurses, revealing that 48.7% of nurses experienced insomnia compared to 37.1% of doctors, which aligns with prior evidence indicating that rotating shift schedules contribute to disturbed sleep and poor recovery4. Additionally, nurses exhibited significantly higher GSRS scores. These findings underscore the greater health challenges nurses face in high-intensity, shift-based work environments. Frequent night shifts disrupt circadian rhythms and reduce sleep quality, leading to gastrointestinal dysfunction. Moreover, the high-stress clinical environment, characterized by long hours and heavy workloads, further exacerbates these symptoms among nurses31. In contrast, while doctors also endure high stress and long working hours, they typically have fewer shifts and concentrate more on diagnosis and decision-making, which may help mitigate some insomnia and gastrointestinal issues. Nevertheless, emergencies and extended hours continue to pose significant health risks for doctors32. Furthermore, the predominantly female nurse population contributes to these disparities, as research indicates that females are more susceptible to insomnia and gastrointestinal symptoms33.
Exploring the mechanisms of gastrointestinal symptoms and insomnia
While this study did not directly investigate the biopsychosocial mechanisms between gastrointestinal symptoms and insomnia, our findings align with existing literature regarding the gut-brain axis and the impact of stress responses on sleep. The possible mechanisms include: (1) Gut-Brain Axis and Neuroimmune Modulation: Emerging research emphasizes the pivotal role of the gut-brain axis, a bidirectional communication network involving the enteric nervous system, central nervous system, and gut microbiota, in maintaining the homeostasis of both GI and sleep functions34. Alterations in gut microbial composition can trigger neuroimmune responses, leading to increased production of proinflammatory cytokines and changes in neurotransmitter availability (e.g., serotonin, gamma-aminobutyric acid)35. These mediators not only modulate local GI motility and sensation but may also disrupt sleep architecture and circadian regulation. Furthermore, chronic low-grade inflammation has been implicated in both GI disorders (e.g., irritable bowel syndrome) and insomnia, underscoring a shared inflammatory pathophysiology that heightens perceived pain or discomfort, disrupts autonomic balance, and ultimately degrades sleep quality36. (2) Psychosocial Stress and hypothalamic–pituitary–adrenal (HPA) Axis Dysregulation: Healthcare workers, particularly those in high-acuity clinical environments, frequently encounter prolonged work-related stressors such as demanding schedules, critical patient care, and emotional labor37. This chronic stress can upregulate the HPA axis, leading to elevated cortisol levels that persist well beyond the work shift38. Elevated cortisol and sustained sympathetic hyperarousal are known to impair the restorative aspects of sleep, resulting in difficulty initiating and maintaining sleep, fragmented sleep cycles, and nonrestorative sleep39. Concurrently, these hormonal and autonomic shifts may compromise GI motility and increase visceral hypersensitivity, exacerbating symptoms such as pain, bloating, and reflux. Over time, this cyclical pattern of stress-related GI distress and sleep disruption can reinforce maladaptive behaviors, such as the use of stimulants, unhealthy dietary patterns, and insufficient relaxation. These behaviors further exacerbate both insomnia and GI dysfunction40. (3) Circadian Rhythm Disruption and Gastrointestinal Dysregulation: Irregular work hours and night shifts are hallmarks of many healthcare professions. Such schedules can dramatically disturb circadian rhythms by misaligning an individual’s internal clock with environmental light–dark cycles41. Circadian misalignment influences melatonin secretion, core body temperature rhythms, and peripheral clock gene expression in tissues including the GI tract42. Under normal conditions, circadian regulation helps synchronize GI motility, digestive enzyme secretion, and nutrient absorption with feeding times. However, night shift work disrupts these processes, precipitating erratic GI activity and potentially leading to symptoms such as constipation, diarrhea, and reflux. Meanwhile, the misalignment also impairs sleep initiation and maintenance, creating a dual burden on the individual43. (4) Psychological and Behavioral Components: In addition to biologically mediated mechanisms, psychological factors such as anxiety, depression, and somatization can intensify the association between insomnia and GI symptoms. Individuals with heightened anxiety or depressive symptoms often exhibit increased attentional bias toward bodily sensations, perceiving GI discomfort or pain more intensely44. This can precipitate a cycle in which nighttime ruminations about work stress or physical discomfort amplify pre-sleep arousal and worsen insomnia, in turn fueling further GI distress the following day45. Over extended periods, negative affect and poor sleep quality can lower stress tolerance, further accelerating the dysregulation of both GI and sleep systems46.
Limitations and future research directions
This study has several limitations. First, we employed convenience sampling through hospital e-mail lists, intranet notices, and WeChat groups. Although this approach facilitated rapid, anonymous recruitment, the sampling frame was indeterminate and a precise response rate could not be calculated, which may limit the representativeness of the findings. Second, the cross-sectional design precludes any inference of causality. Third, reliance on self-reported questionnaires may introduce recall and social-desirability biases. Fourth, the study was conducted in a single geographic region, so it may not capture variations in work environments and stressors experienced by healthcare professionals elsewhere. Future studies should adopt probability-based, multi-centre longitudinal designs to clarify causal relationships and to further elucidate the biopsychosocial mechanisms linking gastrointestinal symptoms and insomnia—particularly in high-stress clinical settings.
Conclusion
This study found a significant positive correlation between gastrointestinal symptoms and insomnia among healthcare workers. This finding highlights the health challenges healthcare workers face, particularly the close link between gastrointestinal health and sleep quality in high-stress work environments.
Data availability
Datasets can be obtained from the corresponding author upon reasonable request.
References
Perlis, M. L. et al. Insomnia. Lancet 400, 1047–1060 (2022).
Lechat, B. et al. The association of co-morbid insomnia and sleep apnea with prevalent cardiovascular disease and incident cardiovascular events. J. Sleep Res. 31, e13563 (2022).
Thun, E. et al. Trajectories of sleepiness and insomnia symptoms in Norwegian nurses with and without night work and rotational work. Chronobiol. Int. 33, 480–489 (2016).
Zhang, C. et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front. Psychiatry 11, 306 (2020).
Mahmud, S., Hossain, S., Muyeed, A., Islam, M. M. & Mohsin, Md. The global prevalence of depression, anxiety, stress, and insomnia and its changes among health professionals during COVID-19 pandemic: A rapid systematic review and meta-analysis. Heliyon 7, e07393 (2021).
Leso, V. et al. Impact of shift work and long working hours on worker cognitive functions: current evidence and future research needs. IJERPH 18, 6540 (2021).
Zhang, Y. et al. The prevalence of functional gastrointestinal disorders related symptoms and the association with working place among healthcare workers who were in the fighting against COVID-19 in regional China. Front. Public Health 10, 1048935 (2022).
Nojkov, B., Rubenstein, J. H., Chey, W. D. & Hoogerwerf, W. A. The impact of rotating shift work on the prevalence of irritable bowel syndrome in nurses. Am. J. Gastroenterol. 105, 842–847 (2010).
Zhen, Lu. & W., Ann Gwee, K., Yu Ho, K.,. Functional bowel disorders in rotating shift nurses may be related to sleep disturbances. Eur. J. Gastroenterol. Hepatol. 18, 623–627 (2006).
Zhao, W. et al. Sleep quality of functional gastrointestinal disorder patients in class-three hospitals: a cross-sectional study in Tianjin, China. BioMed. Res. Int. 2018, 1–5 (2018).
Hwang, S.-K., Lee, Y.-J., Cho, M.-E., Kim, B.-K. & Yoon, Y.-I. Factors associated with gastrointestinal symptoms among rotating shift nurses in South Korea: a cross-sectional study. IJERPH 19, 9795 (2022).
Pappa, S. et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 88, 901–907 (2020).
Su, Z. et al. Acute and long COVID-19 symptoms and associated factors in the omicron-dominant period: a nationwide survey via the online platform Wenjuanxing in China. BMC Public Health 24, 2086 (2024).
Bastien, C. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2, 297–307 (2001).
Riemann, D. et al. The European Insomnia Guideline: An update on the diagnosis and treatment of insomnia 2023. J. Sleep Res. 32, e14035 (2023).
Svedlund, J., Sjödin, I. & Dotevall, G. GSRS-a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig. Dis. Sci. 33, 129–134 (1988).
Takeoka, A. et al. Psychological effects of Helicobacter pylori-associated atrophic gastritis in patients under 50 years: A cross-sectional study. Helicobacter 22, e12445 (2017).
Plummer, F., Manea, L., Trepel, D. & McMillan, D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry 39, 24–31 (2016).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9 validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613 (2001).
Glazer, K., Rootes-Murdy, K., Van Wert, M., Mondimore, F. & Zandi, P. The utility of PHQ-9 and CGI-S in measurement-based care for predicting suicidal ideation and behaviors. J. Affect. Disord. 266, 766–771 (2020).
Jiang, M. et al. Identifying and measuring the severity of somatic symptom disorder using the Self-reported Somatic Symptom Scale-China (SSS-CN): a research protocol for a diagnostic study. BMJ Open 9, e024290 (2019).
Hsieh, F. Y., Bloch, D. A. & Larsen, M. D. A simple method of sample size calculation for linear and. logistic regression. Stat. Med. 17, 1623–1634 (1998).
Yang, Q. et al. Association between preadmission metformin use and outcomes in intensive care unit patients with sepsis and type 2 diabetes: a cohort study. Front. Med. 8, 640785 (2021).
Tu, Q., Heitkemper, M. M., Jarrett, M. E., Buchanan, D. T. Sleep disturbances in irritable bowel syndrome: a systematic review. Neurogastroenterol. Motil. 29, (2017).
Clevers, E., Lutin, E., Cornelis, J. & Van Oudenhove, L. Gastrointestinal symptoms in office workers are predicted by psychological distress and short sleep duration. J. Psychosom. Res. 138, 110230 (2020).
Grover, M. et al. Psychological, physical, and sleep comorbidities and functional impairment in irritable bowel syndrome: Results from a national survey of US adults. PLoS ONE 16, e0245323 (2021).
Hao, G. et al. Sleep quality and disease activity in patients with inflammatory bowel disease: a systematic review and meta-analysis. Sleep Med. 75, 301–308 (2020).
Roman, P. et al. Influence of shift work on the health of nursing professionals. JPM 13, 627 (2023).
Pan, X. et al. Prevalence of mental health problems and associated risk factors among military healthcare workers in specialized COVID ‐19 hospitals in Wuhan, China: A cross‐sectional survey. Asia-Pac. Psychiatry. 14, (2022).
Liu, Y. et al. Association between sleep disturbance and mental health of healthcare workers: A systematic review and meta-analysis. Front. Psychiatry 13, 919176 (2022).
Gander, P. et al. Fatigue and nurses’ work patterns: An online questionnaire survey. Int. J. Nurs. Stud. 98, 67–74 (2019).
Kotze, K., van der Westhuizen, H.-M., van Loggerenberg, E., Jawitz, F. & Ehrlich, R. Doctors’ extended shifts as risk to practitioner and patient: South Africa as a case study. IJERPH 17, 5853 (2020).
Marta, O. F. D. et al. Gender differences in the relationships between sleep disturbances and academic performance among nursing students: A cross-sectional study. Nurse Educ. Today 85, 104270 (2020).
Mayer, E. A., Nance, K. & Chen, S. The gut-brain axis. Annu. Rev. Med. 73, 439–453 (2022).
Lin, C.-H. et al. Altered gut microbiota and inflammatory cytokine responses in patients with Parkinson’s disease. J. Neuroinflamm. 16, 129 (2019).
Xia, L. et al. Relationships between a range of inflammatory biomarkers and subjective sleep quality in chronic insomnia patients: a clinical study. NSS 13, 1419–1428 (2021).
Mrs, S. B. Impact of prolonged working hours, work stress and fatigue among Nurses. IJFMR 5, 2553 (2023).
Miyama, H. et al. Association of chronotypes and sleep disturbance with perceived job stressors and stress response: a covariance structure analysis. NDT 16, 1997–2005 (2020).
Cohn, A. Y. et al. Effects of sleep fragmentation and estradiol decline on cortisol in a human experimental model of menopause. J. Clin. Endocrinol. Metab. 108, e1347–e1357 (2023).
Jiang, Y., Greenwood-Van Meerveld, B., Johnson, A. C., Travagli, R. A. Role of estrogen and stress on the brain-gut axis. Am. J. Physiol.-Gastrointest. Liver Physiol. 317, G203–G209 (2019).
Skene, D. J. et al. Separation of circadian- and behavior-driven metabolite rhythms in humans provides a window on peripheral oscillators and metabolism. Proc. Natl. Acad. Sci. U.S.A. 115, 7825–7830 (2018).
Resuehr, D. et al. Shift work disrupts circadian regulation of the transcriptome in hospital nurses. J. Biol. Rhythms 34, 167–177 (2019).
Rogers, A. E. et al. Shiftwork, functional bowel symptoms, and the microbiome. PeerJ 9, e11406 (2021).
Yanartaş, Ö. et al. Depression and anxiety have unique contributions to somatic complaints in depression, irritable bowel syndrome and inflammatory bowel diseases. Psychiatry Clin. Psychopharmacol. 29, 418–426 (2019).
Melo, J. M. et al. Work-related rumination and worry at bedtime are associated with worse sleep indicators in schoolteachers: a study based on actigraphy and sleep diaries. Sleep Med. 80, 113–117 (2021).
Topan, R. et al. Poor subjective sleep quality predicts symptoms in irritable bowel syndrome using the experience sampling method. Am. J. Gastroenterol. 119, 155–164 (2024).
Acknowledgements
Firstly, we thank the Free Statistics team for providing technical assistance and valuable tools for data analysis and visualization. We also extend our gratitude to the Zotero team. Their reference management tool greatly simplified the collection and organization of my literature, making the management of references more efficient and standardized. Lastly, we thank the Obsidian team. Their note-taking software provided an efficient platform for my research notes, idea recording, and material organization, significantly improving my work efficiency.
Funding
This study was supported by China Scholarship Council (Grant no. 201906070289), Startup Fund for Scientific Research, Fujian Medical University (Grant no. 2022QH1268). The funders had no role in the study design, analysis, decision to publish, nor preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
X.L., Y.H. and X.L. participated in the design of research schemes, extracted, and analyzed the data, and wrote the main manuscript text. C.L. and Y.H. collected the data. Y.Z., P.C. and B.X. participated in the design of research schemes. Y.W. reviewed the manuscript. All authors contributed to the article and approved the submitted version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
This study was approved by the Medical Ethics Committee of Quanzhou City First Hospital (Approval No. 2023[185]). All procedures were conducted in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments, as well as all relevant guidelines and regulations. Written informed consent was obtained from every participant prior to enrolment in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, X., Huang, Y., Wang, Y. et al. Association between gastrointestinal symptoms and insomnia among healthcare workers: a cross-sectional study. Sci Rep 15, 19572 (2025). https://doi.org/10.1038/s41598-025-05079-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-05079-w