Abstract
The purpose of this study was to determine predictors of hemodialysis access patency after drug-coated balloon angioplasty (DCBA) in patients with arteriovenous fistula (AVF). The clinical and imaging data of patients with hemodialysis access dysfunction treated with drug-coated balloon (DCB) in our hospital from January 2020 to January 2024 were analyzed retrospectively, the patency of hemodialysis access was followed up. The length of the DCB is 4 cm. Kaplan-Meier analysis was performed for determination of primary patency and secondary patency in this population. Univariate and multivariate Cox proportional hazards regression analyses were performed to identify predictors of primary patency after DCBA. A total of 173 hemodialysis patients treated with DCB were included in the study. The median survival time of primary and secondary patency were 443 and 1035 days, and the primary patency rates at 6, 12, 18, 24, 30 and 36 months were 85.9%, 64.1%, 34.1%, 21.3%, 12.0% and 6.0%, respectively. The secondary patency rates at 6, 12, 18, 24, 30 and 36 months were 98.8%, 93.8%, 89.8%, 81.9%, 76.1% and 48.6%, respectively. Multivariate analysis using Cox proportional hazard regression models showed that lesion length>4 cm(p=0.002), tandem stenosis(p=0.007) and thrombosis (p < 0.001) were independent risk factors for primary patency after DCBA in patients with AVF. However, lesion length (p=0.021), residual stenosis (p=0.022), and thrombosis (p=0.018) were the independent predictors of primary patency in patients with single lesions.Lesion length>4 cm, tandem stenosis and thrombosis were found to be predictors of primary patency after using 4 cm length DCB. However, in patients with single lesions, lesion length, residual stenosis, and thrombosis serve as independent predictors of primary patency.
Similar content being viewed by others
Introduction
Hemodialysis is one of the kidney replacement treatments for patients with acute and chronic renal failure. With the increasing prevalence of end-stage renal disease (ESRD), more and more patients with ESRD need to undergo hemodialysis. Therefore, hemodialysis access is the lifeline for these patients to survive1,2.Compared with arteriovenous graft and tunnel-cuffed catheter (TCC), arteriovenous fistula (AVF) has longer life, lower incidence of complications and better long-term patency, so it is regarded as the first choice for long-term hemodialysis access3,4,5. However, there is no absolute ideal type of hemodialysis access. Vascular injury during hemodialysis access establishment, vascular injury due to repeated vascular puncture, venous arterialization, fibrosis due to increased shear force in the thin-walled outflow tract vein, and turbulence can lead to dysfunction of hemodialysis access6,7. Vascular access complications have become a common expected problem in hemodialysis patients. How to maintain functional vascular access is still a major problem faced by patients undergoing hemodialysis8.
Percutaneous transluminal angioplasty (PTA) has become the standard treatment for the restrictive stenosis of hemodialysis access. Because of its relatively simple surgical advantages, it can usually achieve initial patency successfully9,10. When the balloon dilates, the intima and media are forcibly torn, and the damaged endothelial cells and vascular smooth muscle cells release growth factors to repair the damaged vascular wall structure, which will eventually lead to intima hyperplasia and restenosis of the target lesion, resulting in dysfunction of hemodialysis access. Therefore, repeated intervention is required to maintain patency11,12. Paclitaxel is known for its ability to inhibit the proliferation and migration of smooth muscle cells and fibroblasts, thereby effectively suppressing neointimal hyperplasia and restenosis in blood vessels13,14. In comparison to rapamycin, paclitaxel-coated balloons have seen broader application15. Paclitaxel drug-coated balloon (DCB) can deliver paclitaxel to the blood vessel wall during dilation, and then can effectively inhibit smooth muscle cell proliferation, migration and extracellular matrix formation by stabilizing microtubules, preventing mitosis, and inhibiting cell DNA synthesis, which in turn reduces restenosis of target diseases16. Studies have shown that the patency rate of paclitaxel drug-eluting balloon angioplasty in hemodialysis stenosis is significantly longer than that of conventional balloon angioplasty (CBA)17. In the IN. PACT AV Access Study, which encompassed 330 cases, results demonstrated a significant difference in target lesion primary patency (TLPP) between DCBs and plain balloons (PB) at 6 and 12 months, with DCBs exhibiting superior performance18. Conversely, the Lutonix AV Randomized Trial of Paclitaxel Coated Balloons, which involved 285 patients, found no significant difference in TLPP between DCBs and PBs at 6 and 12 months19. The reasons for these inconsistent studies may be related to balloon specifications, lumen preparation, drug loss, lesion nature, lesion ___location, etc. However, there are few reports on the risk factors of relapse in hemodialysis access after the use of paclitaxel drug balloon.
This study retrospectively analyzed the clinical data of DCB in the treatment of hemodialysis access dysfunction and followed up on the patency of the hemodialysis access. The DCB utilized in this study comprises a lipophilic matrix of magnesium stearate, which is incorporated with paclitaxel at a density of 3.3 µg/mm². The objective was to analyze the factors related to vascular patency after DCBA in hemodialysis.
Materials and methods
Study participants and characteristics
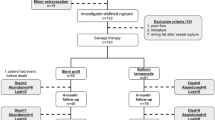
This study was approved by the Ethics Committee of The Affiliated Suzhou Hospital of Nanjing Medical University. The clinical data of 173 patients with AVF dysfunction in our hospital from January 2020 to January 2024 were analyzed retrospectively. Include: Sex, Age, Hypertension, Diabetes, Hyperlipidemia, Left/Right hand, Forearm/upper arm, Thrombus, Smoking, Antiplatelet, Tandem stenosis, Occlusion, Hemodialysis time, Artery diameter, Reference vessel diameter, Lesion length, Preoperative target lesion diameter, Preoperative lumen loss, Preoperative stenosis rate, Postoperative target lesion diameter, Postoperative lumen loss, Residual stenosis, Technical success/Technical failure. The imaging data were all measured on digital subtraction angiography (DSA), and the stenosis rate was calculated by the ratio of the diameter of the narrow blood vessel measured by DSA to the diameter of the normal blood vessel. Through telephone follow-up or retrieval of case data, the patency of the hemodialysis access of each patient after the operation was obtained.
Definition
Technical success was defined according to the SIR reporting guidelines as<30% residual stenosis following PTA with full effacement of the angioplasty balloon. Clinical success was resumption of dialysis for at least one session. Primary patency was defined as the interval from the initial PTA until the repeat PTA, vascular access failure, or study end, whichever occurred first. Secondary patency was defined as the interval from the initial PTA until the abandonment of the vascular access due to any cause, regardless of the number of subsequent PTA. These definitions are based on the 2003 reporting standards of the American Society of Interventional Radiology20. Simple stenosis: defined as only one type of stenosis, such as type I stenosis, type II stenosis, type III stenosis and type IV stenosis. Tandem stenosis: defined as two or more types of stenosis. When there was tandem stenosis, DCB only dealt with the lesions that caused the dysfunction of the hemodialysis access.
Inclusion criteria
Age between 18 and 80 years; At least one successful hemodialysis; Clinical evidence of significant hemodynamic stenosis, ultrasound or angiography confirmed stenosis ≥ 50%; Patients who cannot maintain hemodialysis, such as insufficient blood flow, difficulty in venipuncture, decreased thrill, and increased venous pressure.
Exclusion criteria
The presence of pregnancy, active malignancy, and known hypersensitivity to iodine contrast agent or lidocaine, sepsis or active infection, history of stent placement in target lesions, past or present history of using open surgery to repair arteriovenous fistula, central vein stenosis, target lesion aneurysm formation, lost follow-up patient.
Surgical procedure
After anesthesia with 1% lidocaine, a short sheath (Terumo, Japan) was successfully inserted by percutaneous puncture under the guidance of ultrasound, and heparin was given intravenously according to body weight. Then the whole hemodialysis access angiography is performed to determine the position of the stenosis target. The selection of the balloon refers to the diameter of normal blood vessels around the target lesion, which is the same as or 1 mm larger than the reference blood vessels. The balloon filled until the narrow segment of the waist disappeared. The diameter of the DCB (Acotec, China) is equal to or 1 mm larger than the diameter of the last expanded conventional balloon to maintain normal contact with the blood vessel wall. Cover the target lesion with a 4 cm length of DCB and maintain it at the recommended standard pressure for 3 min. Finally, the entire hemodialysis access was radiographed to rule out any direct complications as well as potential lesions.
Statistical analysis
All statistical analyses were performed using IBM SPSS statistical software V.26.0 for Windows (IBM Corp, Armonk, New York). Categorical variables are expressed as the number (N) and percentage, Percentages are rounded up to the nearest whole number. while continuous variables are expressed as the mean and SD. Univariate and multivariate Cox proportional hazards regression analyses were performed to examine post-DCBA patency. Results of the regression analyses are presented as the HR with corresponding 95% CI and p value. Target lesion primary patency curves were calculated using the Kaplan-Meier method and were compared using the log-rank test. All P values were two tailed, and P < 0.05 were considered statistically significant.
Results
Participant demographic and clinical characteristics
A total of 173 hemodialysis patients were included in this study. The average age of patients was 63.1 ± 12.3 years, and 90(52.0%) were male, with an average hemodialysis time of 7.2 ± 4.6 years. There were 123 (71.7%) cases in the left hand, 125 (72.3%) cases in the forearm. There were 42(24.3%) cases with technical failure,112(64.7%) cases with thrombosis, 107(61.8%) cases with tandem stenosis, and 65(37.6%) cases with occlusion. The mean artery diameter was 4.0 ± 1.4 mm, the mean reference vein diameter was 5.5 ± 1.0 mm, and the mean lesion length was 4.0 ± 1.7 cm. The stenosis rate of the target lesion was 82.8 ± 16.3% before treatment with conventional balloon, and the residual stenosis was 23.5 ± 11.8% after treatment with DCB. The demographic and clinical characteristics of all patients were shown in Table 1.
Primary patency and secondary patency
The median survival time of primary and secondary patency were 443 and 1035 days, and the primary patency rates at 6, 12, 18, 24, 30 and 36 months were 85.9%, 64.1%, 34.1%, 21.3%, 12.0% and 6.0%, respectively (Fig. 1). The secondary patency rates at 6, 12, 18, 24, 30 and 36 months were 98.8%, 93.8%, 89.8%, 81.9%, 76.1% and 48.6%, respectively (Fig. 2).
Predictors of patency
Univariate and multivariate analysis of independent risk factors associated with primary access patency was performed using Cox proportional hazard regression model. The results revealed that Per 1-cm increase in lesion length (HR: 1.19, 95% CI: 1.07, 1.33) was associated with a 19% higher risk of hemodialysis access dysfunction. Additionally, the analysis revealed that patients with tandem stenosis (HR: 1.84, 95% CI: 1.18, 2.88) had a significantly higher risk of hemodialysis access dysfunction compared to those with simple stenosis. Furthermore, compared to patients without thrombosis, patients with thrombosis (HR: 2.27, 95% CI: 1.48, 3.49) had a significantly higher risk of hemodialysis access dysfunction. Therefore, lesion length, tandem stenosis, and thrombosis were the independent predictors of primary patency after using 4 cm length DCB (Table 2). The subgroup analysis of different lesion lengths showed that the primary patency rate of patients with length > 4 cm was lower, and it was significant. Kaplan-Meier survival curve for each risk factor is shown in the Fig. 3.
Predictors of patency in patients with single lesions
To further investigate the application effect of DCB in patients with single lesions of 2 centimeters or smaller, we further excluded patients with tandem lesions. Subsequently, Cox proportional hazards regression models were used to conduct univariate and multivariate analyses on independent risk factors associated with primary patency. The results revealed that lesion length (HR: 1.43, 95% CI: 1.06, 1.93), residual stenosis (HR: 1.38, 95% CI: 1.05, 1.65), and thrombosis (HR: 3.33, 95% CI: 1.22, 9.05) were the independent predictors of primary patency in patients with single lesions (Table 3).
Discussion
As far as we know, this is the first article to discuss the risk factors of recurrence of DCBA in hemodialysis patients. This study retrospectively analyzed the clinical data of patients with hemodialysis access dysfunction in our hospital, the research results show that the median survival time of primary and secondary patency were 443 and 1035 days, and the primary patency rates at 6, 12, 18, 24, 30 and 36 months were 85.9%, 64.1%, 34.1%, 21.3%, 12.0% and 6.0%, respectively. The secondary patency rates at 6, 12, 18, 24, 30 and 36 months were 98.8%, 93.8%, 89.8%, 81.9%, 76.1% and 48.6%, respectively. The result shows that lesion length>4 cm, tandem stenosis and thrombosis were independent risk factors for primary patency after DCBA for hemodialysis access dysfunction. However, in patients with single lesions, lesion length, residual stenosis, and thrombosis serve as independent predictors of primary patency.
Vascular access is one of the most important factors affecting the quality of life and longevity of patients receiving hemodialysis for end-stage renal disease, and PTA is the preferred surgical method for dysfunctional vascular access21,22. Because PTA is more minimally invasive than surgery, it can significantly reduce surgical time, reduce invasive operations, and can open blood vessels in the shortest time so that patients can perform hemodialysis as early as possible23,24. Although PTA has many advantages, the primary patency rate is still poor and requires repeated intervention on the hemodialysis access, which increases the pain and burden of the patient. In order to improve the long-term patency rate of dialysis access, many methods have been tried, including metal bare stent implantation, coated stent implantation, cut balloon angioplasty and high-pressure balloon angioplasty, etc., but the effect is not very satisfactory, so new treatment methods are urgently needed to improve the long-term patency rate of dialysis access25,26,27.DCB is a combination of balloon forming technology and drug elution technology, and paclitaxel drugs that inhibit cell proliferation are attached to the surface of balloon to inhibit intimal proliferation. Professor Scheller of Germany first published the results of animal experiments on the effective inhibition of in-stent restenosis of coronary artery by paclitaxel in 2003, and his team completed the first study on the treatment of in-stent restenosis in humans in 200428,29 Subsequently, DCB began to be used in the treatment of various diseases, including hemodialysis access30,31,32.The randomized trial of paclitaxel DCB in the treatment of arteriovenous fistula stenosis recruited 207 subjects from 23 research centers, and then conducted a randomized control of high-pressure balloon and paclitaxel DCB. The results of 2-year study showed that paclitaxel DCB was effective in the treatment of arteriovenous fistula stenosis, and the long-term patency rate was higher19. The randomized trial of PACT AV Access DCB for the treatment of arteriovenous fistula dysfunction recruited 330 patients through 29 international research centers. The same high-pressure balloon was used for blood vessel preparation. The results showed that DCB was superior to PTA in target lesion primary patency (TLPP) and access primary patency (ACPP), and there was no difference in 3-year mortality33. Ian and Chenyu’s meta-analysis study included 1113 and 1752 patients with hemodialysis access dysfunction, respectively. Based on the primary patency rates at 6 and 12 months, DCB is a better choice than CB for the treatment of hemodialysis access stenosis34,35. In summary, a large number of studies have shown that DCBA can improve the long-term patency of hemodialysis access compared with PTA. However, there is no research report on the factors of recurrence of hemodialysis access after DCBA.
This study shows that lesion length>4 cm, tandem stenosis and thrombosis are independent risk factors for Hemodialysis access dysfunction after DCBA. Previous studies have found that the length of stenosis and multiple stenosis are closely related to the patency of post-PTA hemodialysis access, and longer lesion length and tandem stenosis are important predictors of post-PTA hemodialysis access dysfunction36,37,38. However, in the presence of multiple lesions, the definition of lesion length is variable and can be divided into the length of a single lesion and the cumulative length of multiple lesions, which is reported in this study as the cumulative length. This study showed that the presence of lesion length and tandem stenosis increased the risk of restenosis after DCB treatment of hemodialysis access dysfunction. Further stratified analysis showed that the probability of recurrence was significantly increased when lesion length > 4 cm. The length of the DCB used in this study was 4 cm. When combined with tandem stenosis or lesion length > 4 cm, considering the economic cost, it is impossible to use DCB to cover all the lesions. Generally, only one DCB is used to treat the target lesions that cause the dysfunction of the hemodialysis access, so the lesions that have been treated with CB but not DCB may be the cause of recurrence. This study found that thrombosis can significantly increase the risk of restenosis after DCB treatment of hemodialysis access dysfunction. Thrombosis begins to be organized at 2 weeks, and begins to connect with the blood vessel wall. With the extension of time, the removal of thrombus will gradually become more difficult, so this part of the thrombus will adhere to the blood vessel wall and cannot be removed39. This part of the old thrombus will affect the release of paclitaxel, and the residual thrombus will weaken the effect of DCB. However, when further analyzing the application effect of DCB in patients with single lesions of 2 centimeters or smaller. The results showed that lesion length, residual stenosis, and thrombus formation were independent predictors of primary patency in patients with a single lesion. This suggests that in the treatment of single lesion patients with 4 cm length DCB, longer lesion length and thrombus formation reduce the efficacy of DCB. At the same time, more thorough vascular preparation should be carried out in this specific group to reduce residual stenosis and maintain better DCB treatment outcomes.
According to literature reports, the reported results of hemodialysis age and patency after PTA intervention are inconsistent, and this study did not find a correlation between hemodialysis age and patency after DCB treatment of hemodialysis access obstruction40,41. This study shows that Preoperative stenosis rate, Reference vessel diameter and Postoperative stenosis rate are irrelevant to the patency results after DCBA. The reason may be that the stenosis rate is closely related to the result of Reference vessel diameter. Stenosis or vasodilation near the target vascular lesion can also affect the size of the Reference vessel diameter, which in turn affects the stenosis rate. In this study, the vast majority of patients are well prepared for blood vessels, so that the Postoperative stenosis rate of most patients is less than 30%, achieving technical success, so there is no difference in the postoperative patency rate of hemodialysis access treated with DCB. As far as we know, this study represents a breakthrough analysis to explore the risk factors of postoperative recurrence of DCBA in hemodialysis patients.
However, our research still has some limitations. Firstly, this is a single-center retrospective study, not a prospective study. Secondly, in the whole process of our research, it was not completed entirely by one chief surgeon, but by three experienced surgeons. Small differences caused by the personal experience and skills of the chief surgeon cannot be ruled out. Thirdly, in this study, there are no clear criteria for when to perform PTA again and abandon vascular access, because there are many factors to be considered, including the level of the surgeon, the patient’s self-perception, and taking into account the patient’s age, the patient’s economic situation, the remaining resources of hemodialysis vascular access, the relative risks and benefits of re-PTA and newly established surgical access, so there may be a choice bias. Fourthly, the puncture method, hemodialysis flow and laboratory examination during hemodialysis may have a certain impact on the results, which are not included in this study. In future research, we will strive to address these limitations. Fifthly, this study is constrained by its retrospective, single-center design and a relatively small sample size, which may limit the generalizability of the findings. To enhance the robustness of these results, it is essential to conduct future multicenter prospective studies with larger cohorts. Finally, this study is confined to the outcomes associated with DCB of 4 cm in length, and as such, and these findings may not be generalizable. At the same time, our study appears to be the first to report a recurrence risk factor analysis in hemodialysis patients using DCB.
Conclusion
This study found that lesion length > 4 cm, tandem stenosis and thrombus were predictive factors of primary patency after using 4 cm length DCB. However, in patients with single lesions, lesion length, residual stenosis, and thrombosis serve as independent predictors of primary patency. For patients with the above risk factors, we should strengthen their monitoring to avoid serious adverse events of hemodialysis access dysfunction as far as possible.
Data availability
All data related to this study can be obtained upon reasonable request from the correspondent.
References
Hill, N. R. et al. Global prevalence of chronic kidney Disease - A systematic review and Meta-Analysis[J]. PLoS One. 11 (7), e0158765 (2016).
Global and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017[J] Lancet, 395(10225):709–733. (2020).
Allon, M., Al-Balas, A., Young, C. J. & Cutter, G. R. Lee teffects of a more selective arteriovenous fistula strategy on vascular access Outcomes[J]. J. Am. Soc. Nephrol. 34 (9), 1589–1600 (2023).
Al-Balas, A., Lee, T., Young, C. J., Kepes, J. A. & Barker-Finkel, J. Allon MThe clinical and economic effect of vascular access selection in patients initiating Hemodialysis with a Catheter[J]. J. Am. Soc. Nephrol. 28 (12), 3679–3687 (2017).
Hicks, C. W., Wang, P., Kernodle, A., Lum, Y. W. & Black, J. H. 3 Makary maassessment of use of arteriovenous graft vs arteriovenous fistula for First-time permanent Hemodialysis. Access[J] JAMA Surg. 154 (9), 844–851 (2019).
Northrup, H., He, Y., Le, H., Berceli, S. A. & Cheung, A. K. Shiu YTDifferential hemodynamics between arteriovenous fistulas with or without intervention before successful use[J]. Front. Cardiovasc. Med., 9(1001267. (2022).
Northrup, H. et al. Analysis of Geometric and Hemodynamic Profiles in Rat Arteriovenous Fistula Following PDE5A Inhibition[J].Front Bioeng Biotechnol, 9(779043. (2021).
Riella, M. C. Roy-Chaudhury pvascular access in haemodialysis: strengthening the achilles’ heel[J]. Nat. Rev. Nephrol. 9 (6), 348–357 (2013).
Kim, J., Kwon, Y., Choi, T. W. & Won JHManagement Immature Arteriovenous Fistulas[J] Cardiovasc. Intervent Radiol., 46(9):1125–1135. (2023).
Masud, A., Costanzo, E. J. & Zuckerman, R. Asif athe complications of vascular access in Hemodialysis[J]. Semin Thromb. Hemost. 44 (1), 57–59 (2018).
Zhu, Z. R. et al. Predictors of primary patency after percutaneous balloon angioplasty for stenosis of Brescia-Cimino Hemodialysis arteriovenous fistula[J]. Br. J. Radiol. 93 (1109), 20190505 (2020).
Ming, Z., Li, W., Ding, W. & Yuan, R. Li XThe efficacy of percutaneous transluminal angioplasty treatment for the patients with arteriovenous fistula dysfunction[J]. Int. Angiol. 35 (2), 163–169 (2016).
Wöhrle JDrug-coated. Balloons for coronary and peripheral interventional procedures[J]. Curr. Cardiol. Rep. 14 (5), 635–641 (2012).
Loh, J. P. Waksman RPaclitaxel drug-coated balloons: a review of current status and emerging applications in native coronary artery de Novo lesions[J]. JACC Cardiovasc. Interv. 5 (10), 1001–1012 (2012).
Wessely, R. & Schömig, A. Kastrati asirolimus and Paclitaxel on polymer-based drug-eluting stents: similar but different[J]. J. Am. Coll. Cardiol. 47 (4), 708–714 (2006).
Han, A., Park, T., Kim, H. J., Min, S. & Ha, J. Min skeditor’s Choice - Paclitaxel coated balloon angioplasty vs. Plain balloon angioplasty for haemodialysis arteriovenous access stenosis: A systematic review and a time to event Meta-Analysis of randomised controlled Trials[J]. Eur. J. Vasc Endovasc Surg. 62 (4), 597–609 (2021).
Chen, X., Liu, Y., Wang, J., Zhao, J. & Singh, N. Zhang WWA systematic review and meta-analysis of the risk of death and patency after application of paclitaxel-coated balloons in the Hemodialysis access[J]. J. Vasc Surg. 72 (6), 2186–2196e2183 (2020).
Lookstein, R. A. et al. Drug-Coated balloons for dysfunctional Dialysis arteriovenous Fistulas[J]. N Engl. J. Med. 383 (8), 733–742 (2020).
Trerotola, S. O. & Saad, T. F. Roy-Chaudhury PThe Lutonix AV randomized trial of Paclitaxel-Coated balloons in arteriovenous fistula stenosis: 2-Year results and subgroup Analysis[J]. J. Vasc Interv Radiol. 31 (1), 1–14e15 (2020).
Gray, R. J., Sacks, D. & Martin, L. G. Trerotola soreporting standards for percutaneous interventions in dialysis access[J]. J. Vasc Interv Radiol. 14 (9 Pt 2), S433–442 (2003).
Lok, C. E., Huber, T. S. & Orchanian-Cheff, A. Rajan DKArteriovenous access for Hemodialysis. Review[J] Jama. 331 (15), 1307–1317 (2024).
Schmidli, J. et al. (eds) ‘s Choice - Vascular Access: 2018 Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS)[J].Eur J Vasc Endovasc Surg, 55(6):757–818. (2018).
Yu, H. & Chi, Y. Wang BThe efficacy of percutaneous transluminal angioplasty and arteriovenous fistula reconstruction for immature arteriovenous fistula[J]. BMC Nephrol. 24 (1), 304 (2023).
Luo, F., Huang, C., Yao, G. & Zhou, J. Lu XComparison of percutaneous transluminal angioplasty and surgical revision after intraoperative dilatation with biliary tract probes for arteriovenous fistula stenosis at juxta-anastomosis[J]. Vascular, 17085381221140179. (2022).
Polkinghorne, K. R. et al. KHA-CARI guideline: vascular access - central venous catheters, arteriovenous fistulae and arteriovenous grafts[J]. Nephrol. (Carlton). 18 (11), 701–705 (2013).
Agarwal, S. K. et al. Comparison of cutting balloon angioplasty and percutaneous balloon angioplasty of arteriovenous fistula stenosis: A Meta-Analysis and systematic review of randomized clinical Trials[J]. J. Interv Cardiol. 28 (3), 288–295 (2015).
Chen, X., Zhang, C. & Wang, J. Luo tcomparative efficacy and safety of four common balloon angioplasty techniques for an arteriovenous fistula or graft stenosis: a systematic review and network meta-analysis of randomized controlled trials[J]. Ann. Transl Med. 11 (6), 246 (2023).
Scheller, B., Speck, U., Schmitt, A. & Böhm, M. Nickenig gaddition of Paclitaxel to contrast media prevents restenosis after coronary stent implantation[J]. J. Am. Coll. Cardiol. 42 (8), 1415–1420 (2003).
Scheller, B., Speck, U., Abramjuk, C., Bernhardt, U. & Böhm, M. Nickenig GPaclitaxel balloon coating, a novel method for prevention and therapy of restenosis[J]. Circulation 110 (7), 810–814 (2004).
Rittger, H. et al. Angiographic patterns of drug-eluting stent restenosis after treatment with drug-coated balloon versus balloon angioplasty: late lumen loss subgroup analyses of the PEPCAD-DES study[J]. Catheter Cardiovasc. Interv. 88 (4), 529–534 (2016).
Rittger, H. et al. Long-Term outcomes after treatment with a Paclitaxel-Coated balloon versus balloon angioplasty: insights from the PEPCAD-DES study (Treatment of Drug-eluting stent [DES] In-Stent restenosis with sequent please Paclitaxel-Coated percutaneous transluminal coronary angioplasty [PTCA] Catheter)[J].JACC Cardiovasc Interv, 8(13):1695–1700. (2015).
Trerotola, S. O. & Roy-Chaudhury, P. Saad TFDrug-Coated balloon angioplasty in failing arteriovenous fistulas: more data. Less Clarity[J] Am. J. Kidney Dis. 78 (1), 13–15 (2021).
Lookstein, R. et al. IN.PACT AV Access Randomized Trial of Drug-Coated Balloons for Dysfunctional Arteriovenous Fistulae: Clinical Outcomes through 36 Months[J].J Vasc Interv Radiol, 34(12):2093–2102.e2097. (2023).
Irani, F. G. et al. Hemodialysis arteriovenous fistula and graft stenoses: randomized trial comparing Drug-eluting balloon angioplasty with. Conventional Angioplasty[J] Radiol. 289 (1), 238–247 (2018).
Yan Wee, I. J. et al. A systematic review and meta-analysis of drug-coated balloon versus conventional balloon angioplasty for dialysis access stenosis[J]. J. Vasc Surg. 70 (3), 970–979e973 (2019).
Aktas, A., Bozkurt, A. & Aktas, B. Kirbas ipercutaneous transluminal balloon angioplasty in stenosis of native Hemodialysis arteriovenous fistulas: technical success and analysis of factors affecting postprocedural fistula patency[J]. Diagn. Interv Radiol. 21 (2), 160–166 (2015).
Miyamoto, K. et al. Analysis of factors for post-percutaneous transluminal angioplasty primary patency rate in Hemodialysis vascular access[J]. J. Vasc Access. 21 (6), 892–899 (2020).
Romann, A., Beaulieu, M. C., Rhéaume, P., Clement, J. & Sidhu, R. Kiaii MRisk factors associated with arteriovenous fistula failure after first radiologic intervention[J]. J. Vasc Access. 17 (2), 167–174 (2016).
Berg SObstructive sleep apnoea syndrome. Curr. status[J] Clin. Respir J., 2(4):197–201. (2008).
Kim, S. M. et al. Factors affecting patency following successful percutaneous intervention for dysfunctional Hemodialysis vascular Access[J]. Ann. Vasc Surg. 47, 54–61 (2018).
Zheng, Q. et al. Predictors associated with early and late restenosis of arteriovenous fistulas and grafts after percutaneous transluminal angiography[J]. Ann. Transl Med. 9 (2), 132 (2021).
Funding
This work was supported by the Jiangsu Medical Association Interventional Medicine Phase III Special Fund Project (SYH-3201140-0089).
Author information
Authors and Affiliations
Contributions
GH conceived and designed the study and wrote the main manuscript text. GH, YT, and DZ analyzed the data. JX and JZ conducted the literature search and prepared figures. GH, YT, and DZ performed the manuscript review. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huo, G., Xue, J., Zheng, J. et al. Factors associated with patency following drug-coated balloon angioplasty of hemodialysis access. Sci Rep 15, 19375 (2025). https://doi.org/10.1038/s41598-025-05133-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-05133-7