Abstract
Based on the premise of bounded rationality, this study introduces the value function and decision weight function from prospect theory into the framework of evolutionary game theory to analyze the decision-making process of healthcare institutions, patients, and the government during the vertical integration of electronic health records. The study incorporates factors such as loss aversion, sensitivity to gains and losses, and the degree of awareness and utilization of records, to explain the behavioral tendencies of the three players from the perspective of perceived value. It uses simulations to reveal how factors such as the loss aversion coefficient and sensitivity to perceived value influence the evolutionary outcomes. This research extends the discussion of psychological factors, such as risk attitudes and gain-loss perception, in the context of the vertical integration of electronic health record. The findings indicate that: (1) increasing the initial willingness of all parties to participate is a key factor in encouraging active involvement in the EHR integration process; (2) the value of record awareness and the closeness of medical alliances significantly affect participation behavior, thus accelerating the integration process; (3) factors such as loss aversion, sensitivity to gains and losses, and efficacy loss sensitivity have complex effects on the system’s evolutionary path. Policymakers need to consider the risk perception characteristics of all parties and adjust policies accordingly to promote the stable development of the system.
Similar content being viewed by others
Introduction
With the aging population and the continuous rise in the number of chronic disease patients, the mismatch between the supply and demand for healthcare resources has become increasingly pronounced. The traditional decentralized healthcare information management model can no longer meet the needs of modern healthcare services1. The importance of healthcare consortia within the global healthcare system is becoming increasingly prominent. Their vertical integration enhances the mobility and continuity of patients among different healthcare institutions by promoting the optimal allocation of medical resources. Being the core data support for the operation of healthcare consortia, the vertical integration of electronic health records facilitates the seamless flow of patients’ health information within a consortium. This integration enables efficient collaboration between different healthcare institutions and provides continuous health management support for patients’ cross-institutional care2. Although many countries are currently vigorously promoting the integration of electronic health records, challenges remain, such as inconsistent technical standards, inadequate data privacy protection, and imperfect information-sharing mechanisms3. The cross-institutional sharing of medical information resources often involves multiple stakeholders, and effective integration requires complex negotiations and coordination of interests, aiming to achieve mutually beneficial outcomes for all parties involved4.
Evolutionary game theory is an effective tool for clarifying complex game relationships and the evolution of strategies5 which helps to analyze the process of strategy adjustment and evolution for all parties in dynamic environments. In fields such as public governance6,7,8, information sharing9,10, and resource allocation11 evolutionary game models are widely used to study the strategic interactions and evolutionary patterns in complex systems. Zhu12 et al. constructed a three-party evolutionary game model involving drug manufacturers, third-party drug testing organizations, and government regulators, to analyze rent-seeking problems that may arise during drug production, highlighting potential rent-seeking behavior by manufacturers and testers. Battiston13 and colleagues constructed a three-party evolutionary game model involving government, business, and civil organizations to analyze the evolutionary trajectories of environmental policies. Similarly, He14 et al. addressed the issues of information distortion, false advertising, and difficult supervision in e-commerce supply chains within the context of “live broadcasting +.” They proposed feasible recommendations for the standardized operation of live streaming e-commerce supply chains, considering three scenarios with varying rates of return: low, medium, and high. Hosseini15 et al. applied evolutionary game theory to study the evolutionary strategies of supply chain members for channel coordination and the distribution mechanism of surplus coordination profits, arguing that the share of coordination profits plays a crucial role in evolutionary decision-making. In recent years, increasing scholarly attention has been directed toward the evolutionary game modeling of behavioral compliance and incentive mechanisms, leading to a series of influential studies. For example, Han16 et al. proposed the “committed cooperation model,” which emphasizes the coordination between individual willingness to participate and compliance incentives. The authors highlight that fostering participation is as equally important as enhancing compliance, thereby offering theoretical support for institutional design. In the fields of AI governance and environmental cooperation, researchers have effectively captured the dynamics of multi-party behavioral compliance through the introduction of voluntary commitments, media oversight, and soft law incentives17. Furthermore, Ogbo18 et al. investigated the effects of prior commitment mechanisms on coordination outcomes within multi-agent evolutionary game frameworks, providing methodological insights for analyzing asymmetric strategic interactions. In the area of technology safety regulation, Bova and Balabanova19 integrated media monitoring, audit incentives, and regulatory policies into the evolutionary game framework of AI governance, arguing that in the absence of formal oversight structures, the media can fulfill a “soft regulation” role.
In parallel, recognizing the bounded rationality and cognitive biases of decision-makers, an increasing number of studies have incorporated prospect theory within multi-agent evolutionary game frameworks. This integration offers a more behaviorally grounded and realistic depiction of agents’ decision-making processes and perceptual distortions under uncertainty. By incorporating behavioral assumptions such as loss aversion and risk preference, prospect theory reveals the biases in decision-making under uncertainty20. This can aid in gaining an understanding of participants’ risk and loss aversion behaviors in these decisions and their responses to policy incentives, thereby providing theoretical support for optimizing policy design and fostering multi-agent collaboration21. Zhang22 et al. based on their research prospect theory and mental accounting theory, constructed a collaborative evolutionary game model for shared manufacturing quality, studying quality decision-making under different cost-benefit amortization mechanisms. Wang21 et al. constructed a decentralized multi-agent collaborative three-party evolutionary game model based on digital empowerment theory and prospect theory. In this model, the government builds a platform, while new energy enterprises and academic research institutions collaborate. As noted in prospect theory, behavioral assumptions such as loss aversion and risk preference reveal biases in decision-making under uncertainty20. This understanding supports policy design and promotes multi-agent collaboration.
In summary, while prospect theory and evolutionary game theory have been widely applied in public management and healthcare services, there remains a relative lack of research combining the two to analyze the vertical integration of EHR. Existing research has the following shortcomings: First, it fails to fully account for the heterogeneity of the strategic choices and dynamic evolutionary process among healthcare institutions, patients, and the government, hindering a comprehensive understanding of the transformation of the roles of these parties and their shifting participation intentions. Second, it lacks a systematic analysis of behavioral factors, such as sensitivity to loss aversion, and overlooks the psychological factors influencing strategic decision-making, making it difficult to adapt to the complex, long-term evolutionary processes in reality. In response to the above shortcomings, this paper assumes the limited rationality of the game participants and incorporates the value function from prospect theory, along with the decision-making weight function for perceived profits and losses, loss aversion, and other factors, into the payment matrix of the three-party game for the vertical integration of EHR. It analyzes how the perception of value and risk preferences of the three parties influence the evolution and stability of the system. Additionally, simulations are used to examine how factors such as loss aversion and sensitivity to perceived value impact the evolutionary outcomes, further exploring the tripartite strategic evolution from multiple perspectives.
Based on the above analysis, this paper aims to analyze strategic interactions in the vertical integration of electronic health records. To address this, it develops a three-party evolutionary game model among medical institutions, patients, and the government, incorporating factors such as loss aversion, sensitivity to gains and losses, and perceived value of information. Simulation experiments are performed in parallel to conduct a sensitivity analysis of these factors and explore the impact of loss aversion coefficients, perceived value sensitivity, and other elements on the system’s evolutionary path. This study offers valuable references for policymakers in optimizing the EHR integration strategy, improving multi-party participation willingness, and fostering the stability of the system.
The main contributions of this paper are as follows:
-
(1)
This study constructs a game-theoretic model involving hospitals, patients, and the government to analyze strategic interactions in the vertical integration of electronic health records. The model provides a novel theoretical framework for studying EHR integration. Compared with traditional game models, the evolutionary game approach captures the dynamic evolution and interaction of strategies among players, making it more suitable for capturing complex game dynamics. This approach deepens our understanding of the dynamic relationships among multiple stakeholders in the vertical integration of EHR.
-
(2)
This paper introduces the concept of integration within healthcare alliances and parameters related to the sharing and utilization of EHR, enabling a deeper analysis of how stakeholders coordinate resources, share information, and optimize services during the EHR vertical integration process.
-
(3)
To further investigate the strategic interactions among hospitals, patients, and the government in the vertical integration of EHR, this study incorporates factors such as perceived value, loss aversion, and decision weighting derived from prospect theory into the payment matrix of the three-player game. This approach helps explain stakeholder decision-making under risk and uncertainty, offering insights into how perceptual biases shape decision outcomes.
The remainder of this paper is organized as follows: Sect. 2 develops a multi-agent game model of EHR vertical integration based on prospect theory and conducts a stability analysis. Section 3 assigns values to key parameters in the model for simulation analysis. Section 4 discusses the simulation results. Section 5 presents the conclusions, including key findings, policy recommendations, limitations, and future research directions.
Construction of the evolutionary game model
Description of evolutionary game problem
The vertical integration of electronic health records involves three primary stakeholders: healthcare institutions, patients, and the government, whose interrelationships are illustrated in Fig. 1. As primary providers of healthcare services, healthcare institutions actively participate in the vertical integration of EHR within the healthcare consortium to improve service quality and operational efficiency, enabling seamless sharing and management of diagnostic and treatment information. However, healthcare institutions face several challenges during the integration process, including significant costs, pressures to upgrade technology, and risks related to data security. Moreover, they may choose to passively participate due to trade-offs between risks and resource constraints. Thus, the strategy space for healthcare institutions includes (active participation, passive participation). As recipients of healthcare services and key data contributors in EHR, patients can gain more transparent healthcare services and enhance their health management capabilities by actively engaging in the monitoring and management of their records. However, patients must bear certain time and financial costs in this process and may hesitate to participate due to concerns about data privacy and security. Thus, the strategy space for patients in EHR integration includes (active participation, passive participation). As regulators of healthcare resource distribution, governments aim to improve the efficiency and equity of healthcare services within the healthcare consortium by facilitating EHR integration, thereby enhancing the overall health of society. However, in practice, local governments may face constraints such as budget limitations, uneven resource distribution, and difficulties in building information systems, leading them to either actively support integration or adopt a passive stance. Thus, the strategy set for the government comprises (active participation, passive participation).
Assumptions and parameters
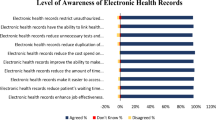
To ensure the scientific soundness and practical applicability of the model settings, the parameters adopted in this study are based on a comprehensive review of national policy documents and prior scholarly research. Specifically, key policy-related parameters, including government subsidies, penalty levels, and incentives for electronic record implementation—are derived from policy guidelines issued by the National Health Commission concerning the development of EHR systems and the establishment of healthcare consortia23. Meanwhile, behavioral cognition variables, such as healthcare institutions’ awareness of EHR24,25 and the degree of integration within healthcare consortia26—are drawn from empirical findings in prior studies.
In addition, considering the complexity of the multi- party strategic evolution process, this study also draws upon recent applications of evolutionary game theory in areas such as environmental governance13 healthcare investment27 and AI safety regulation19. These studies typically incorporate dynamic penalty mechanisms, perceived utility functions, and behavioral adjustment processes under incomplete information—offering valuable theoretical and methodological insights for the design of the patient’s perceived value function and the government’s incentive mechanism within this study.
Building upon these foundations, this paper constructs a three-party evolutionary game model based on prospect theory and introduces the following key assumptions to systematically depict the behavioral logic and strategy evolution processes of each stakeholder.
Hypothesis 1
Each player in the game has two strategic choices: active participation and passive participation. “Active participation” refers to the behavior of actively engaging in the vertical integration of electronic health records, while “passive participation” refers to the behavior of a player passively engaging in this process. The probability that a medical institution chooses “active participation” is denoted by \(\:x\) (\(\:0\le\:x\le\:1\)), and the probability of choosing “passive participation” is \(\:1-x\). Similarly, the probability that a patient chooses “active participation” is denoted as \(\:y\) (\(\:0\le\:y\le\:1\)), and the probability of choosing “passive participation” is \(\:1-y\). Similarly, the probability that the government chooses “active participation” is denoted as \(\:z\) (\(\:0\le\:z\le\:1\)), and the probability of choosing “passive participation” is \(\:1-z\).
Hypothesis 2
The players in the game are healthcare institutions, patients, and the government, all of which are boundedly rational. Consequently, the choice of strategy by these players is primarily based on their perceived value of the strategy’s payoff, rather than the direct gaina or losses associated with the strategy itself28 According to the prospect theory proposed by Tversky and Kahneman, the psychologically perceived value of each player can be quantified using the prospect value \(\:V\), which is jointly determined by the value function \(\:v\left(\varDelta\:{x}_{i}\right)\) and the weight function \(\:w\left(p\right)\)29. By replacing the expected utility function with the prospect value function, and the objective probability with a decision weight function, better reflects the decision-maker’s subjective judgment regarding the event’s gain or loss, as well as the probability of its occurrence during the game process30. \(\:{V}_{i}\) denotes the perceived value of a given strategy for player \(\:i\), which is equal to the sum of the products of the perceived values of \(\:n\) outcomes in the strategy and their corresponding subjective probabilities. Where \(\:\varDelta\:{x}_{i}={x}_{i}-{x}_{0}\), with \(\:{x}_{i}\) representing the \(\:i\)-th outcome of the event, \(\:{x}_{0}\) is the reference point, and \(\:\varDelta\:{x}_{i}\) represents the relative gain or loss of outcome \(\:i\) relative to the reference point \(\:{x}_{0}\).
In the value function \(\:v\left(\varDelta\:{x}_{i}\right)\) (see Eq. (2)), \(\:\varDelta\:{x}_{i}\ge\:0\) indicates a gain in outcome \(\:{x}_{i}\) relative to the reference point \(\:{x}_{0}\), while \(\:\varDelta\:{x}_{i}<0\) denotes a relative loss. Parameters \(\:\alpha\:\) and \(\:\beta\:\) capture the degree of diminishing sensitivity in the value functions for gains and losses, respectively. Larger values of \(\:\alpha\:\) and\(\:\:\beta\:\) indicate a steeper decline in the respective value functions. \(\:\lambda\:\) represents the degree of loss aversion and is typically greater than 1, indicating higher sensitivity to losses than to gains.
In the decision weight function \(\:\pi\:\left({p}_{i}\right)\) (see Eq. (3)), \(\:{p}_{i}\) denotes the objective probability of event iii occurring, and \(\:\sigma\:\) \(\:\left(0<\sigma\:<1\right)\) is the distortion parameter of the function, reflecting the curvature of the decision weight function.
In this paper, we introduce the value function and decision weight function from prospect theory, which reflect the psychological biases influencing decision-making, such as perceived value sensitivity and loss aversion. The reference point is set to \(\:{x}_{0}=0\) to measure the perceived value of objective gains and losses31,32,33,34.
Hypothesis 3
For medical institutions, the baseline operational benefitis denoted as \(\:{K}_{h}\). The actual benefit resulting from their participation in the vertical integration of EHRs depends on the institutions’ awareness and utilization of health records, denoted as \(\:\rho\:\) (where \(\:0\le\:\rho\:\le\:1\)). If the average incremental benefit from active participation in cross-institutional EHR vertical integration is \(\:{M}_{h}\), then the additional benefit for medical institutions’ active participation will be \(\:\rho\:*{\text{M}}_{\text{h}}\), at a cost of \(\:{C}_{h}\). Meanwhile, medical institutionsreceive an incentive subsidy \(\:{R}_{h}\) from the local government. The damage to the overall societal interest caused by medical institutions’ adoption of a negative strategy is denoted as \(\:{D}_{h}\), which is ultimately borne by the patients. When a healthcare provider successfully creates a health record for a patient, itreceive a subsidy \(\:{S}_{h}\) from the government.
Hypothesis 4
For patients, the benefits of active participation in health record integration are closely related to the closeness of the healthcare consortium, \(\:\phi\:\) (where \(\:0\le\:\phi\:\le\:1\)). The higher the closeness within the consortium, the stronger the data-sharing and service synergies between healthcare organizations, allowing patients to receive more comprehensive and convenient healthcare services. It is assumed that when the vertical integration of the EHR system is successfully established, the average unit benefit from patients’ active participation in health record integration is denoted as \(\:{M}_{p}\). Therefore, the ultimate health benefit for patients’ participation in record management is \(\:\phi\:*{M}_{p}\). The cost of filing a complaint arises when a patient perceives that their EHR has not been fully utilized for inter-institutional sharing or has failed to provide the expected medical convenience. This cost is denoted as \(\:{C}_{p}\). Such complaint behavior is not deterministic, but rather a probabilistic event, depending on the patient’s willingness to complain and the perceived likelihood of a successful outcome. If the healthcare organization is negatively involved at this point, it receives an incentive, \(\:{R}_{p}\), from the government. However, no reward is provided for successful complaints when the local government is also passively engaged. The assumption that \(\:V\left({M}_{p}\right)>{R}_{p}\) indicates that patients prefer the ongoing benefits of EHR integration to one- off government rewards obtained through complaints, especially when seeking long-term health management benefits. If patients abandon monitoring, they neither incur costs nor receive government rewards.
Hypothesis 5
The government, acting as the regulatory authority in the evolutionary game, supervises the strategic decisions of all participants. When the government actively promotes the integration of EHRs, it gains benefits, such as social value and public acclaim, denoted as by \(\:{M}_{g}\), while incurring costs represented by \(\:{C}_{g}\).If the local government determines that patient complaints are legitimate or that healthcare institutions fail to take effective action during their active participation in EHR integration, the institutions will be penalized by the local government, with the penalty denoted as \(\:{P}_{h}\).If the healthcare organization’s negative participation results in unsatisfactory EHR integration while the local government is also passively involved, the local government will be held accountable by the higher-level government, represented by \(\:{P}_{g}\).When the healthcare organization actively participates in the integration of information under the influence of policy and achieves positive outcomes, the distinction between the local government’s proactive efforts and its negative response becomes clearer. When the local government is actively engaged in information integration under the policy’s influence and achieves successful outcomes, the distinction between promotion and passivity becomes blurred, and the local government will not be held accountable by higher authorities or face potential penalties such as loss of credibility and reputation35.
Based on the assumptions outlined above, the model parameters are defined, and the symbols of each parameter, along with their respective meanings, are presented in Table 1.
Game benefit matrix
According to prospect theory, there is no deviation between actual utility and perceived value when gains or losses are deterministic. Psychological perceived utility arises only under conditions of uncertainty regarding benefits and costs36. Under normal conditions, the benefits to healthcare organizations, \(\:Kh\), are internal and independent of external factors. Government incentives, \(\:Rh\), and subsidies, \(\:Sh\), provided for their active participation in the integration, as well as the rewards, \(\:Rp\), given for patients’ reports of negative participation, are explicit policy incentives. These incentives are deterministic and guaranteed as long as the participation conditions are satisfied. Similarly, penalties imposedon local governments for failing to promote integration, and on healthcare organizations for passive participation, are policy-mandated and deterministic. The remaining parameters depend on the actual integration outcomes and the level of cooperation among all parties. These parameters are uncertain and susceptible to perceptual bias. Accordingly, the three strategy combinations of healthcare institutions, patients, and local governments, along with the corresponding perception matrices of gains and losses in the evolutionary game, are presented in Table 2.
In Table 2, \(\:\alpha\:\:\)denotes the sensitivity to perceived gain, \(\:\beta\:\:\)denotes the sensitivity to perceived losses, and λ represents the coefficientof loss aversion. \(\:V\left({M}_{h}\right)={\left(\rho\:*{\text{M}}_{\text{h}}\right)}^{\alpha\:}\) represents the perceived benefit gained when healthcare organizations actively participate in EHR construction, where ρ reflects their level of awareness and utilization. \(\:-V\left(-{C}_{h}\right)={\lambda\:\left({\text{C}}_{\text{h}}\right)}^{\beta\:}\) denotes the perceived loss when healthcare organizations actively participate in EHR integration. \(\:V\left({M}_{p}\right)={\left(\phi\:*{\text{M}}_{\text{p}}\right)}^{\alpha\:}\) denotes the perceived value of patients’ active participation in EHR integration. \(\:-V\left(-{C}_{p}\right)={\uppi\:}\left({p}_{0}\right){\lambda\:\left({\text{C}}_{\text{p}}\right)}^{\beta\:}\) represents the perceived cost of monitoring incurred only when the patient files a complaint during the longitudinal integration of EHR. \(\:-V\left(-{D}_{h}\right)={\lambda\:\left({\text{D}}_{\text{h}}\right)}^{\beta\:}\) represents the social loss caused by passive participation of healthcare organizations in the vertical integration of EHR, which is borne by patients. \(\:V\left({M}_{g}\right)={\left({\text{M}}_{\text{g}}\right)}^{\alpha\:}\) represents the perceived benefit generated when the government actively promotes EHR. \(\:-V\left(-{C}_{g}\right)={\lambda\:\left({C}_{g}\right)}^{\beta\:}\) represents the cost incurred by the government during active promotion of EHR integration. \(\:-V\left(-{\text{P}}_{\text{g}}\right)={\lambda\:\left({\text{P}}_{\text{g}}\right)}^{\beta\:}\) represents the penalty imposed by higher-level authorities on local government for passive engagement in EHR integration. In this study, uncertainty in the vertical integration of EHR is assumed to primarily arise from patient complaints. It is further assumed that the decision weights for \(\:V\left({M}_{h}\right)\), \(\:V\left({M}_{g}\right), V\left({M}_{p}\right),-V\left(-{C}_{h}\right),-V\left(-{P}_{h}\right),-V\left(-{D}_{h}\right),-V\left(-{C}_{g}\right),-V\left(-{P}_{g}\right)\) are all equal to 1. The probability of a patient file a complaint is denoted as \(\:{\uppi\:}\left({p}_{0}\right)\).
Analysis of evolutionarily stable strategies for replicator dynamic equations
Stability analysis of medical institutions’ strategies
From Table 2, the expected benefits \(\:{E}_{x}\) and \(\:{E}_{1-x}\) for both active and passive participation of healthcare organizations in the vertical integration of EHRs can be derived, along with the corresponding average expected benefit \(\:\stackrel{-}{{E}_{x}}\), as follows:
This yields the replicator dynamic equation \(\:F\left(x\right)\) for healthcare organizations, along withits first-order derivative with respect to x, \(\:\frac{d\left(F\left(x\right)\right)}{dx}\):
For convenience, let \(\:G\left(z\right)=V\left(-{C}_{h}\right)+{P}_{h}*y+{P}_{h}*z+{R}_{h}*z+V\left({M}_{h}\right)-{P}_{h}*y*z\). It follows that \(\:d\left(G\left(z\right)\right)/dz>0\), indicating that \(\:G\left(z\right)\) is a strictly increasing function.
According to the stability theorem of differential equations, a stable equilibrium requires that the probability \(\:x\) of active participation satisfies \(\:F\left(x\right)=0\) and \(\:d\left(F\left(x\right)\right)/dx<0\). When\(\:{\:G\left({z}_{1}^{*}\right)}_{}=0\), then \(\:{z}_{1}^{*}=\frac{V\left(-{C}_{h}\right)+V\left({M}_{h}\right)+\left({P}_{h}\right)*y}{\left(y-1\right)*{P}_{h}-{R}_{h}}.\:\)From \(\:F\left(x\right)=0\), it is evident that \(\:x=0\) or \(\:x=1\) are both potential equilibrium strategies. When \(\:z>{z}_{1}^{*}\), then \(\:{\left.\frac{d\left(F\left(x\right)\right)}{dx}\right|}_{x=1}<0,{\left.\frac{d\left(F\left(x\right)\right)}{dx}\right|}_{x=0}>0\), \(\:x=1\) is the equilibrium point, and “active participation” is the evolutionary equilibrium strategy. When \(\:z<{z}_{1}^{*}\), then \(\:{\left.\frac{d\left(F\left(x\right)\right)}{dx}\right|}_{x=1}>0,{\left.\frac{d\left(F\left(x\right)\right)}{dx}\right|}_{x=0}<0\), \(\:x=0\) is the equilibrium point, and “passive participation” is the evolutionary equilibrium strategy. The phase diagram of strategy evolutionfor healthcare organizations is presented in Fig. 2. In Fig. 2, H1 denotes the propensity of healthcare organizations to actively participate in the vertical integration of electronic health records, while H2 denotes the propensity to participate passively.
As shown in Fig. 2, the healthcare organization’s strategy choice is influenced by both the strategies of patients and the government. All points along the x-axis cross-section represent stable strategies for the healthcare organization. The evolution in the upper region of the cross-section tends toward \(\:x\:=\:0\), where \(\:V\left({M}_{h}\right)+{R}_{h}*z<-V\left(-{C}_{h}\right)+{P}_{h}*y*z-{P}_{h}*z-{P}_{h}*y\), meaning the benefits and rewards resulting from the government’s active participation are outweighed by its costs and penalties, leading the healthcare organization’s strategy to converge to negative participation. If the total benefits of healthcare organization participation increase and costs decrease, achieving \(\:V\left({M}_{h}\right)+{R}_{h}*z>-V\left(-{C}_{h}\right)+{P}_{h}*y*z-{P}_{h}*z-{P}_{h}*y\), the healthcare organization’s strategy will shift to active participation. The evolution will then tend toward \(\:x\:=\:1\) in the lower region of the cross-section.
Stability analysis of patients’ strategies
From Table 2, the expected benefits \(\:{E}_{y}\) and \(\:{E}_{1-y}\) under both active and passive patient participation in the longitudinal integration of EHRs can be obtained, along with the corresponding average expected benefit \(\:\stackrel{-}{{E}_{y}}\):
This results in the patient’s replicator dynamic equation \(\:F\left(y\right)\) and its first-order derivative with respect \(\:y\), \(\:\frac{d\left(F\left(y\right)\right)}{dy}\), respectively:
For convenience, let \(\:H\left(x\right)={R}_{p}*z+V\left(-{C}_{p}\right)-{R}_{p}*x*z+V\left({M}_{p}\right)*x\)* \(\:{H}_{\left(x\right)}\) is an increasing function, as \(\:d\left(H\left(x\right)\right)/dx>0\).
According to the stability theorem of the differential equation, the probability of the patient chooses to actively participate in the longitudinal integration of the EHR at steady state must satisfy \(\:{F}_{\left(y\right)}=0\) and\(\:d\left(F\left(y\right)\right)/dy<0\). When \(\:{H\left({x}_{1}^{*}\right)}_{}=0\) it can be obtained that \(\:{x}_{1}^{*}=\frac{{R}_{p}+V\left(-{C}_{p}\right)}{{R}_{p}-V\left({M}_{p}\right)}\). From \(\:{F}_{\left(y\right)}=0\) it is clear that \(\:y=0\) or \(\:y=1\) are two stable strategies. When \(\:x>{x}_{1}^{*}\), then \(\:{\left.\frac{d\left(F\left(y\right)\right)}{dy}\right|}_{y=1}<0,{\left.\frac{d\left(F\left(y\right)\right)}{dy}\right|}_{y=0}>0\), \(\:y=1\) is the equilibrium point, and “active participation” is the evolutionary equilibrium strategy. When \(\:x<{x}_{1}^{*}\), then \(\:{\left.\frac{d\left(F\left(y\right)\right)}{dy}\right|}_{y=1}>0,{\left.\frac{d\left(F\left(y\right)\right)}{dy}\right|}_{y=0}<0\), then \(\:y=0\) is the equilibrium point, and “passive participation” is the evolutionary equilibrium strategy. The patient’s strategy evolution phase diagram is shown in Fig. 3. In Fig. 3, P1 denotes the propensity of patients to participate passively in the vertical integration of electronic health records, while P2 denotes the propensity to participate actively.
As shown in Fig. 3, the patient’s strategy choice is influenced by both hospital and government strategies. All points of the cross-section corresponding to y represent stable strategies for healthcare providers. The evolution in the upper region of the cross-section tends toward \(\:y\:=\:0\), where \(\:{R}_{p}*z*\left(1-x\right)+V\left({M}_{p}\right)*x>-V\left(-{C}_{p}\right)\), at which point the perceived benefits and rewards from patient participation exceed the perceived participation costs, and the patient’s stabilizing strategy is to actively participate. If the total benefits of patient participation decrease and the costs increase to the point where \(\:{R}_{p}*z*\left(1-x\right)+V\left({M}_{p}\right)*x<{R}_{p}*x*z-V\left(-{C}_{p}\right)\), the patient’s behavioral strategy will shift to passive participation, corresponding to the region below the cross-section, with the evolution tending toward \(\:y=0\).
Stability analysis of government strategies
From Table 2, the expected returns \(\:{E}_{z}\) and \(\:{E}_{1-z}\) under the two participation attitudes—positive and negative—of local governments in the vertical integration of Electronic Health records, as well as the corresponding average expected return \(\:\stackrel{-}{{E}_{z}}:\)
This leads to the replication dynamic equation \(\:F\left(z\right)\) for local governments, along with its first-order derivative with respect to \(\:z\), \(\:\frac{d\left(F\left(z\right)\right)}{dz}\), respectively.
For convenience, let \(\:J\left(x\right)={P}_{g}+{P}_{h}+V\left({M}_{g}\right)\)+\(V\left(-{C}_{g}\right)\)– \({P}_{g}*x-{P}_{h}*x-{P}_{h}*y-{R}_{h}*x\)+\({P}_{h}*x*y-{R}_{p}*y+{R}_{p}*x*y\). It is evident that \(\:J\left(x\right)\) is a decreasing function, as demonstrated by the fact that\(\:d\left(J\left(x\right)\right)/dx<0\).
According to the stability theorem for differential equations, the probability that the local government will actively participate in the vertical integration of EHR must reach a steady state and satisfy both \(\:F\left(z\right)=0\) and \(\:d\left(F\left(z\right)\right)/dz<0\). When \(\:{J\left({x}_{2}^{*}\right)}_{}=0\), we can derive \(\:{x}_{2}^{*}\) as follows:\(\:{x}_{2}^{*}=\frac{{P}_{g}+{P}_{h}+V\left({M}_{g}\right)+V\left(-{C}_{g}\right)-{P}_{h}*y-{R}_{p}*y}{{P}_{g}+{P}_{h}+{R}_{h}-{P}_{h}*y-{R}_{p}*y}\). From \(\:F\left(z\right)=0\), we can observe that \(\:z=0\) or \(\:z=1\) are two stabilizing strategies. When \(\:x>{x}_{2}^{*}\), then \(\:{\left.\frac{d\left(F\left(z\right)\right)}{dz}\right|}_{z=1}<0,{\left.\frac{d\left(F\left(z\right)\right)}{dz}\right|}_{z=0}>0\), suggesting that \(\:z=1\) is the equilibrium point, and that “active participation” is the evolutionary equilibrium strategy. Conversely, when \(\:x<{x}_{2}^{*}\), we have \(\:{\left.\frac{d\left(F\left(z\right)\right)}{dz}\right|}_{z=1}>0,{\left.\frac{d\left(F\left(z\right)\right)}{dz}\right|}_{x=0}<0\), indicating that \(\:z=0\) is the equilibrium point, and “passive participation” is the evolutionary equilibrium strategy. The evolutionary phase diagram of the local government’s strategy is shown in Fig. 4. As shown in Fig. 4, G1 denotes the propensity of the local government to participate passively in the vertical integration of electronic health records, while G2 denotes the propensity to participate actively.
From Fig. 4, it is clear that the strategy choices of local governments are influenced by the strategies of healthcare organizations and patients. All points within the cross-section correspond to z, which represent stable strategies for the government. The evolution in the inner region of the cross-section tends toward \(\:z=1\). Specifically, if \(\:{P}_{h}+V\left({M}_{g}\right)+{P}_{h}*x*y-{P}_{h}*x\)–\({P}_{h}*y>{P}_{g}*x\)– \(V\left(-{C}_{g}\right)+{R}_{h}*x+{R}_{p}*y\)–\({R}_{p}*x*y-{P}_{g}\) , then the government actively participates, and the benefits of active participation outweigh its costs. However, if the total benefits from active participation decrease and the costs increase, leading to \(\:{P}_{h}+V\left({M}_{g}\right)+{P}_{h}*x*y-{P}_{h}*x-{P}_{h}*y<{P}_{g}*x\)\(-V\left(-{C}_{g}\right)+{R}_{h}*x+{R}_{p}*y-{R}_{p}*x*y-{P}_{g}\), the government’s strategy will shift to passive participation, corresponding to the outer region of the cross-section, with the evolution tending towards \(\:z=0.\)
Equilibrium analysis of the evolutionary system
The conditions required for each party’s individual strategy to achieve local stability have been analyzed above, whereas achieving overall system stability requires the coordinated evolution of medical institutions, patients, and the government. To further explore the overall equilibrium state of the system, a dynamic system of differential equations is constructed for the tripartite evolutionary game model, and all equilibrium points are identified by solving the equations \(\:{F}_{\left(x\right)}=0,{F}_{\left(y\right)}=0,{F}_{\left(z\right)}=0\). After solving, the system yields nine equilibrium points, including eight pure strategy equilibrium points and one mixed strategy equilibrium point, namely, \(\:{E}_{1}\left(\text{0,0},0\right),{E}_{2}\left(\text{1,0},0\right),{E}_{3}\left(\text{0,1},0\right),{E}_{4}\left(\text{0,0},1\right),{E}_{5}\left(\text{1,1},0\right),{E}_{6}\left(\text{1,0},1\right),{E}_{7}\left(\text{0,1},1\right),{E}_{8}\left(\text{1,0},0\right),{E}_{9}\left({x}_{1},1,{z}_{1}\right)\). To further assess the stability of these equilibria, the Jacobian matrix of the replicator dynamic system is derived, which is given in Eq. (13).
In the stability analysis of differential systems, the system’s stability can be assessed by examining the signs of the real components of the eigenvalues at equilibrium points. According to Lyapunov’s first method37 an equilibrium point is asymptotically stable if all eigenvalues of the Jacobian matrix have negative real parts, and it is unstable if at least one eigenvalue has a positive real part. Therefore, prior to analyzing the local stability of strategy combinations, a Jacobian eigenvalue analysis must be conducted for the equilibrium points of the evolutionary game to determine whether they correspond to locally stable fixed points within the replicator dynamic system37. The eigenvalues of each equilibrium point can be derived by sequentially substituting the corresponding strategy combinations into the Jacobian matrix, as presented in Table 3. This table summarizes the eigenvalues and signs of the real parts for each fixed point under different strategy combinations, providing a basis for determining their local stability in the replicator dynamic system.
Given that all parameters are positive and \(\:-V\left(-{C}_{p}\right)={\uppi\:}\left({p}_{0}\right){*\lambda\:\left({\text{C}}_{\text{p}}\right)}^{\beta\:}>0\), there is a non-zero perceived value in the equilibrium solution E₃ (0,1,0), which does not satisfy the stability condition and can be directly excluded. In the context of actively promoting the integration of electronic health record, when healthcare institutions, patients, and the government simultaneously adopt negative strategies, the scenario lacks empirical relevance and is therefore not explored further. Consequently, the pure-strategy equilibrium solution \(\:{E}_{1}\left(\text{0,0},0\right)\) is not analyzed in depth. The stability of equilibrium points \(\:{E}_{2},{E}_{4},{E}_{5},{E}_{6},{E}_{7}\), and \(\:{E}_{8}\) will be discussed in the following section.
At the initial stage of EHR vertical integration, the initial ideal state is \(\:{E}_{8}\left(\text{1,1},1\right)\), where healthcare organizations, patients, and the government are all actively involved. The government incentivizes healthcare providers and patients to participate in the integration through policy support, resource investment, and infrastructure development, aiming to achieve the initial goals of information sharing and healthcare quality improvement. Achieving this initial ideal state requires the following conditions to be met: \(\:-V\left(-{C}_{p}\right)-V\left({M}_{h}\right)<0,{R}_{h}-V\left({M}_{g}\right)-V\left(-{C}_{g}\right)<0,-{P}_{h}-{R}_{h}-V\left(-{C}_{h}\right)-V\left({M}_{h}\right)<0\). These conditions suggest that the perceived benefits of participation for patients should outweigh their costs, and that the government’s incentives and policy support should be sufficiently strong to ensure that healthcare organizations receive a net benefit from the integration process. Satisfying these conditions can motivate all actors to actively participate in the early stages, thus effectively promoting the progress of system integration. As the system matures, however, the government gradually shifts from a facilitating role to a regulatory role, reallocating resources from direct intervention to other priority areas of public health, thus creating an evolutionary pattern of \(\:{E}_{5}\left(\text{1,1},0\right)\). The key parameter driving this shift is a reduction in government incentives, ℎ. As ℎ decreases, the government’s direct engagement in integration diminishes, and more effort is directed toward data security, privacy protection, and standards maintenance. At this stage, \(\:{E}_{5}\left(1,\text{1,0}\right)\) becomes a more reasonable goal, with healthcare providers and patients continuing to actively participate due to the direct benefits of improved healthcare quality, resulting from the optimization of treatment processes and the enhancement of the patient experience. Meanwhile, the government assumes a more passive role, maintaining the essential regulatory responsibilities to ensure the long-term stability of the system. To achieve this final ideal state, the following conditions must hold: \(\:-V\left({M}_{p}\right)-V\left(-{C}_{p}\right)<0,-{P}_{h}-V\left(-{C}_{h}\right)-V\left({M}_{h}\right)<0,V\left({M}_{g}\right)-{R}_{h}+V\left(-{C}_{g}\right)<0,\:\)These conditions indicate that the patients’ spontaneous demand for profile integration is sufficient to drive their participation. Furthermore, healthcare organizations can still benefit and maintain their willingness to participate despite diminishing policy support. The government, in turn, opts for passive participation, focusing solely on basic regulation due to the reduced regulatory benefits. In this scenario, the integration of electronic health record is primarily driven by the demand from medical institutions and patients, while the government’s moderate supervision ensures the standardization and sustainable development of the system. This equilibrium allows the integration to operate stably over the long term, balancing the interests of all parties involved.
For the equilibrium point \(\:{E}_{2}\left(1,\text{0,0}\right)\), when the following conditions are met: \(\:V\left({M}_{p}\right)+V\left(-{C}_{p}\right)<0, -V\left({M}_{h}\right)-V\left(-{C}_{h}\right)<0, V\left({M}_{g}\right)-{R}_{h}+V\left(-{C}_{g}\right)<0,\:\)healthcare organizations choose to actively participate, as the perceived benefits of integration outweigh the costs. However, patients choose to passively participate because the perceived benefits are lower than the costs, and similarly, the government also chooses passive participation due to the higher perceived policy incentives and management costs relative to the benefits of integration. In this scenario, the equilibrium strategy among the three parties is (active participation, passive participation, negative participation). The promotion of EHR integration largely relies on the initiative of healthcare organizations, while patients and the government remainpassive due to the imbalance between costs and benefits. This situation could lead to a slowdown or limited promotion of the integration process. To improve the effectiveness of the integration, it is necessary to enhance service quality to increase patients’ perceived benefits, thereby fostering a higher level of synergistic participation.
For the equilibrium point \(\:{E}_{4}\left(\text{0,0},1\right)\), when the following conditions are met: \(\:{R}_{p}+V\left(-{C}_{p}\right)<0,-{P}_{g}-V\left({M}_{g}\right)-{P}_{h}-V\left(-{C}_{g}\right)<0,{P}_{h}+{R}_{h}+V\left(-{C}_{h}\right)+V\left({M}_{h}\right)<0,\:\)the cost of integration for healthcare organizations exceeds the benefits, leading them to choose passive participation. Similarly, the benefits for patients are insufficient to offset their costs, prompting them to also choose passive participation. In contrast, the government’s social and public health benefits surpass its regulatory costs and policy incentives, encouraging it to actively participate.Under these conditions, the equilibrium strategy is (negative participation, negative participation, active participation), with healthcare organizations and patients opting for negative participation due to the excessive costs and insufficient benefits they face. The government, on the other hand, actively participates due to the significant public health benefits and strong policy incentives.
For the equilibrium point \(\:{E}_{6}\left(1,0,1\right)\), when the following conditions are met: \(\:V\left(-{C}_{p}\right)+V\left({M}_{p}\right)<0,{R}_{h}-V\left({M}_{g}\right)-V\left(-{C}_{g}\right)<0,-{P}_{h}-{R}_{h}-V\left(-{C}_{h}\right)-V\left({M}_{h}\right)<0,\:\)healthcare organizations perceive greater benefits from integration than the associated costs, so they choose to actively participate. However, patients’ benefits are not enough to cover their participation costs, leading them to choose passive participation. Additionally, the government’s regulatory and incentive costs outweigh the perceived public health benefits, so it also chooses passive participation. Under these conditions, the equilibrium strategy is (active participation, passive participation, active participation). The active participation of healthcare providers can promote system development, but the passive participation of both patients and the government constrains the overall integration process, undermining the realization of the full synergistic effect.
For the equilibrium point \(\:{E}_{7}\left(0,1,1\right)\), when the following conditions are satisfied: \(\:-{R}_{p}-V\left(-{C}_{p}\right)<0,{P}_{h}+{R}_{h}+V\left({M}_{h}\right)+V\left(-{C}_{h}\right)<0,{R}_{p}-{P}_{g}-V\left({M}_{g}\right)-V\left(-{C}_{g}\right)<0,\:\)the benefits of integration for healthcare organizations are lower than the costs, prompting them to choose passive participation. In contrast, patients perceive higher benefits from integration than the associated costs, and thus choose positive participation. The government, seeing greater public health benefits than regulatory and incentive costs, chooses to actively participate as well. In this scenario, the equilibrium strategy is (negative participation, active participation, active participation). Healthcare organizations are the key players in EHR integration. If they choose negative participation, the entire system integration process will face significant obstacles.
Simulation
Numerical simulations using MATLAB provide an intuitive means of observing the evolutionary trajectories of strategic choices by stakeholders and to verify the reliability of the model. Based on the ideal evolutionary stable point \(\:{E}_{5}\left(\text{1,1},0\right)\), this study adopts the parameterization approaches adopted by Wei38 et al. and colleagues39. The parameters are set as follows: \(\:Kh=100,Mh=50,Mp=10,Ph=50,Sh=10\), Rh = 20, \(Mg=55,Ch=30,Rp=15\), \(Dh=10,Cg=30,Pg=50,Cp=10\). These values are chosen to ensure that the equilibrium conditions for \(\:{E}_{5}\left(\text{1,1},0\right)\) hold, namely: \(\:V\left(Mp\right)>-V\left(-Cp\right),Ph+V\left(Mh\right)>-V\left(-Ch\right),V\left(Mg\right)<Rh-V(-Cg)\).
For the behavioral parameters derived from prospect theory, including the loss aversion coefficient and the value function parameters, reference is drawn from the work of Tao40 and other related studies. The initial values of the relevant prospect theory parameters are defined as α = β = 0.88, σ = 0.69, and λ = 1.1.
Accordingly, this study analyzes the impact of the initial strategic choices of the three participants on the stability of the evolutionary strategies. Moreover, it examines the effects of the archival awareness parameter (ρ), the healthcare alliance cohesion parameter (φ), the value sensitivity parameters (α and β) for gains and losses, and the loss aversion coefficient (λ) on the system’s evolutionary dynamics.
Impact of initial strategy selection on the stability of game strategies
As shown in Fig. 5, the evolutionary trajectories of behavioral strategies for healthcare institutions, patients, and the government are presented under varying initial participation probabilities of 0.1, 0.3, 0.5, 0.7, and 0.9, with all other parameters held constant. Here, \(\:{x}_{0},{y}_{0}\) and \(\:{z}_{0}\) represent the initial willingness to participate of healthcare institutions, patients, and the government, respectively, in the process of vertical integration of electronic health records.
(A) Evolutionary path of hospital behavioral strategies under different initial participation levels. (B) Evolutionary path of patient behavioral strategies under different initial participation levels. (C) Evolutionary path of government behavioral strategies under different initial participation levels.
Figure 5A shows that as the initial willingness to participate increases, the participation probability of healthcare organizations rises rapidly and eventually stabilizes at a higher level of participation. When the initial willingness is low, the evolutionary path of healthcare organizations is slower, but as the initial willingness increases, the rate of participation accelerates significantly. This suggests that, all else being equal, a higher initial willingness to participate enables healthcare organizations to accelerate their participation probability, thereby becoming more active in the vertical integration of EHRs.
Figure 5B illustrates the evolutionary dynamics of patients’ strategy choices over time. Similar to healthcare organizations, the higher the patients’ initial willingness to participate, the faster their participation rate increases, eventually reaching a steady state of near full participation. Under different initial willingness settings, patients’ evolutionary curves show a gradual increase and stabilization. Overall, patients’ participation decisions are particularly sensitive, and the speed at which patients choose to participate is significantly accelerated as their initial willingness rises. This phenomenon suggests that increasing patients’ initial willingness to participate can more effectively enhance their motivation to engage in EHR integration.
Figure 5C, the government’s strategy evolution path shows characteristics distinct from those of healthcare organizations and patients. Although the government’s willingness to participate differs initially, the overall evolutionary trend is similar, with the willingness to participate eventually stabilizing at a lower level. This indicates that, as the EHR integration system matures, the government may gradually reduce its direct involvement, shifting to a regulatory and guiding role rather than remaining a direct intervener. Therefore, the evolution from “active participation” to “passive participation” reflects a shift in the government’s role, as it increasingly cedes responsibility to healthcare organizations and patients in order to promote the self-operation and sustainable development of the system.
Sensitivity analysis of parameters
Analysis of the impact of archival epistemic value and the closeness of the medical association on evolutionary outcomes
Figure 6 presents the evolutionary paths of the respective behaviors of the three parties when the degree of awareness and utilization of the EHR(\(\:{\uprho\:}\)) and the closeness of the healthcare consortium (\(\:{\upphi\:}\)) are set to 0, 0.2, 0.4, 0.6, and 0.8, while other parameters are held constant.
As shown in Fig. 6 A, the probability of healthcare organization participation increases significantly with both \(\:{\uprho\:}\) and \(\:{\upphi\:}\), and the rate of increase is further amplified. This can be attributed to the fact that higher recognition of EHRs and a stronger healthcare consortium enhance the perceived benefits for healthcare organizations, thereby motivating greater participation in the integration process. The evolutionary trajectory converges toward 1, indicating that under conditions of high awareness and strong collaboration, healthcare organization participation eventually stabilizes.
Figure 6B demonstrates that when \(\:{\uprho\:}\) and \(\:{\upphi\:}\) are 0 or 0.2, healthcare organizations make limited use of their records, and the healthcare consortium lacks synergistic support, resulting in limited patient awareness of the value of EHRs. Under these conditions, patients are less likely to engage actively in the record integration process. However, as \(\:{\uprho\:}\) and \(\:{\upphi\:}\) gradually increase, patients become more inclined to actively participate in the EHR integration process to obtain long-term benefits in health management. The probability of patient participation rises significantly and eventually stabilizes. Moreover, as \(\:{\uprho\:}\) and \(\:{\upphi\:}\) continue to increase, the participation probability rises more rapidly and stabilizes more rapidly, suggesting that high awareness and a collaborative environment can effectively encourage patients’ proactive participation.
As shown in Fig. 6 C, the government’s participation rate initially increases and then decreases as \(\:{\uprho\:}\) and \(\:{\upphi\:}\) rise. In the early stages of integration, the potential value of EHRs has not yet fully been realized, so the government must adopt a more proactive strategy to promote EHR integration and ensure active participation from healthcare organizations and patients. However, as the perceived utility of records and the closeness of the healthcare consortium increase, healthcare organizations and patients become more willing to participate autonomously, and the government’s initial promotional role gradually wanes. At this point, the government’s involvement strategy transitions from direct intervention to a role of support and oversight, optimizing resource allocation and fostering the system’s autonomous operation and sustainable development.
(A) Evolutionary path of hospital behavioral strategies under different values of \(\:{\uprho\:}\:\)and \(\:{\upphi\:}\). (B) Evolutionary path of patient behavioral strategies under different values of \(\:{\uprho\:}\:\)and \(\:{\upphi\:}\). (C) Evolutionary path of government behavioral strategies under different values of \(\:{\uprho\:}\:\)and \(\:{\upphi\:}\).
Impact of profit and loss perceived value sensitivity coefficients on evolutionary outcomes
To further examine the factors influencing system evolution, this study performs a sensitivity analysis on the perceived value sensitivity coefficients α and β, which represent the marginal diminishing sensitivity to gains and losses. Higher values of these coefficients indicate a stronger diminishing marginal sensitivity, reflecting greater sensitivity to either gains or losses41. As illustrated in Fig. 7, the evolutionary trajectories of the three stakeholders are presented under varying values of the gain sensitivity coefficient α (0.22, 0.44, 0.66, 0.88, and 0.99), while all other parameters are held constant.
(A) Impact of the perceived value sensitivity coefficient\(\:\:\alpha\:\) for gains on hospital strategy selection. (B) Impact of the perceived value sensitivity coefficient \(\:\alpha\:\) for gains on patient strategy selection.(C) Impact of the perceived value sensitivity coefficient \(\:\alpha\:\) for gains on government strategy selection.
As seen in Fig. 7 A, when \(\:\alpha\:\) is low, healthcare organizations exhibit a weaker perception of benefits, resulting in periodic oscillations without any significant decline in their participation behavior. This phenomenon can be attributed to healthcare organizations repeatedly weighing short-term costs and benefits due to the absence of stable incentive benefits under low benefit perception conditions, thus making it difficult for them to form sustained participation willingness. However, as \(\:\alpha\:\) increases, healthcare organizations become more sensitive to diminishing marginal returns, which leads to a stronger inclination for active participation. The increase in perceived benefits enhances their willingness to invest and motivates further involvement in the integration process, accelerating the overall evolutionary rate of healthcare organizations. As observed in Fig. 7B, when \(\:\alpha\:\) is low, patients have a weak perception of gains. Under such conditions, they struggle to establish a clear link between participation behavior and long-term benefits. Conversely, when α increases to a certain threshold, the increase in patients’ sensitivity to gain perception accelerates their evolution toward greater active participation.
In Fig. 7 C, as α increases, the government’s gain sensitivity also increases, and its participation strategy gradually shifts from active to passive participation. This shift can be interpreted as a natural evolution of the system as it continues to matures. As healthcare institutions and patients engage autonomously, the government reduces its direct intervention and assumes more of a regulatory and supervisory role to support the system’s self-sustainability. Eventually, the system tends toward an equilibrium state defined by (active participation, active participation, negative participation). However, when \(\:\alpha\:\) reaches a critical threshold, the government’s sensitivity to gains reaches its peak, renewing its willingness to engage in system integration. This leads to a shift in strategy toward (active participation, active participation, active participation), as the government reassesses the public health and resource allocation benefits of EHR integration, thereby increasing its level of investment and intervention to ensure equity and long-term system stability.
Figure 8 presents the evolutionary paths of the three parties when the perceived value sensitivity coefficient for losses takes values of 0.22, 0.44, 0.66, 0.88, and 0.99, with other parameters held constant. As illustrated in Figs. 8(A) and 8(B), as β increases, the probability of active participation for healthcare organizations and patients converges to 1 more gradually. The rate of convergence decreases more significantly for healthcare organizations than for patients. A higher indicates heightened perception of loss, leading both healthcare organizations and patients more cautious in evaluating risks and benefits. Healthcare organizations, as key healthcare providers, face greater resource investment, data security concerns, and policy pressures, rendering them more sensitive to potential losses. Although patients are also affected by loss perceptions, their reluctance to actively participate is less pronounced than that of healthcare organizations due to the lower cost of participation. As a result, the reduction rate is smaller for patients.
Furthermore, as seen in Fig. 8(C), the government’s likelihood of active participation slows as \(\:\beta\:\) increases. At higher values of, the government’s sensitivity to risk rises, leading to a quicker transition to negative participation. This shift from positive to negative participation reflects the government’s transition from a direct promotional role to a more regulatory and supportive one, in response to growing loss perceptions. This strategic adjustment also indicates the government’s reevaluation of its role as the system matures, ensuring resource efficiency and giving healthcare organizations and patients greater autonomy to promote system self-sustainability.
(A) Impact of the perceived value of loss sensitivity coefficient \(\:\beta\:\) on hospital strategy choice. (B) Effect of the perceived value of loss sensitivity coefficient \(\:\beta\:\) on patient strategy choice. (C) Impact of the perceived value of loss sensitivity coefficient \(\:\beta\:\) on government strategy choice.
Impact of loss aversion coefficients on evolutionary outcomes
To analyze the influence of decision-makers’ degree of loss aversion on the system’s evolution, the evolutionary paths of the three parties are examined at different sensitivity levels of loss aversion intensity (λ = 1.05, 1.1, 1.2, 1.5, and 2), with all other parameters held constant. A larger value of λ indicates a higher degree of risk aversion and greater loss sensitivity32.
As shown in Fig. 9(A), when the sensitivity of loss aversion intensity (\(\:\lambda\:\)) is set to 2, the participation behavior of healthcare institutions exhibits a cyclical pattern, initially rising and then declining. This is because, in the early stage of EHR integration, medical institutions actively explore collaborative models and revenue mechanisms, driven by the potential for profit generation. However, the high sensitivity to loss aversion makes them acutely aware of the risks associated with integration failure, prompting them to shift from active to passive participation as the process progresses.
Furthermore, high loss aversion sensitivity suggests that medical institutions are particularly sensitive to the risks of integration failure. As they do not quickly achieve stable returns or significantly mitigate their risk perception in the early integration phase, their participation strategy fluctuates. However, long-term gains and competitive pressures induce cyclical behavior, leading to a reversal back to active participation later in the process.
As shown in Fig. 9(B), as the sensitivity of loss aversion intensity (\(\:\lambda\:\)) increases, patients’ willingness to engage actively decreases. When the sensitivity of potency loss aversion (\(\:\lambda\:\)) reaches 1.2, the trade-off between benefits and risks tends to balance, resulting in neutral stance, with no significant bias towards either active or passive participation. As \(\:\lambda\:\) increases further, the rate of negative participation rises. This is because higher loss intensity aversion sensitivity makes patients more sensitive to the possibility of failure or insufficient gains, with concerns about potential losses outweighing expectations of gain. Consequently, their risk perception increases sharply, leading to a rapid decline in their willingness to engage.
As shown in Fig. 9(C), in the early stages of EHR integration, government participation was heavily driven by policy and dependent on regulatory oversight. However, as healthcare organizations and patients increasingly participated spontaneously, the government gradually reduced its direct intervention, shifting to a guiding and regulatory role, evolving from a “facilitator” to a “regulator”, and eventually becoming a “supporter,” ultimately reaching a stable state of passive participation. As \(\:\lambda\:\) increases, the government’s shift to negative participation accelerates. High loss aversion sensitivity causes the government to focus more on the potential risks of policy or integration failure, leading to a reduction in intervention to minimize policy risks. However, when \(\:\lambda\:\) is set to 2, the government’s strategic behavior initially matches that observed at lower values of λ. However, its participation probability exhibits a cyclical pattern, initially rising and then falling. This indicates the government’s need to adapt to the complexity of the integration process, adjusting dynamically based on the evolving benefits and risks. Strengthening early-stage policy intervention aims to guide the system onto the correct path. When the initial outcomes under high sensitivity fail to meet expectations, the government opts for increased intervention to address the situation. However, as risk aversion grows, it eventually shifts back to passive participation.
Discussion
Main findings
Based on the assumption of limited rationality of decision makers, this paper introduces the value function and decision weight function from prospect theory into the evolutionary game model, to analyze the evolutionary process of interactions between medical institutions, patients, and the government in the vertical integration of electronic health record. By incorporating factors such as loss aversion, sensitivity to profit and loss, and record awareness and utilization, the behavioral tendencies of the three parties in the game are analyzed from the perspective of value perception. This approach fills the gap in existing models that overlook decision makers’ psychological cognition and corrects biases in traditional evolutionary game theory and classical expected utility theory regarding the integration of electronic health record. Furthermore, we explore the influence of key parameters on system evolution through simulation and analyze underlying factors such as insufficient policy incentives and the low willingness of stakeholders to participate in the process of vertical integration of electronic health record. The findings of this study are as follows:
-
(1)
Enhancing participants’ initial willingness to engage, increasing the value of file awareness, and strengthening the closeness of the healthcare consortium are key factors in promoting the active participation of the three main stakeholders in the EHR integration process. By increasing the initial willingness of medical institutions, patients, and the government to participate and recognize the value of electronic health record, the participation of all parties can be significantly accelerated, thereby promoting the rapid integration and stable development of the system. Additionally, increasing the closeness of the healthcare consortium can enhance the willingness of all parties in the system to cooperate, thereby improving overall integration efficiency.
-
(2)
The value of archival awareness \(\:\left(\rho\:\right)\) and the degree of closeness of the healthcare consortium \(\:\phi\:\) significantly influence the participation behavior of the three main stakeholders. As these factors increase, the willingness of medical institutions and patients to participate rises significantly, and the speed of participation is accelerated. This suggests that the value of the records and the level of support from the healthcare consortium can effectively enhance the motivation of participating parties, thereby promoting the EHR integration process. The government’s high willingness to participate in the initial stage gradually diminishes as the system matures, shifting to a regulatory and supportive role.
-
(3)
The perceived value sensitivity coefficient for gains and losses and the coefficient of loss aversion affect system evolution results through different pathways. The coefficient of perceived value sensitivity to profit and loss reflects the degree to which the three parties are sensitive to returns, affecting their perception of both future and marginal returns. Higher loss aversion and gain/loss sensitivity lead healthcare organizations and patients to exhibit greater caution when facing system integration, resulting in slower participation. Additionally, an increase in loss aversion sensitivity further strengthens the three parties’ concern about potential losses, leading them to make more rational and robust decisions. These factors suggest that, in the process of EHR integration, policymakers need to comprehensively consider the risk perception characteristics of each party and adjust policies to promote the stable operation and sustainable development of the system.
Recommendations
Although progress in the initial promotion of EHR integration, challenges such as variability and instability in the willingness and behavior of healthcare institutions, patients, and the government to participate remain. Therefore, it is crucial to ensure sustained motivation from all parties and the long-term management of the system. In this context, this study offers the following recommendations:
-
(1)
The government and healthcare organizations should enhance the initial willingness of all stakeholders to engage by providing policy support and incentives, particularly during the early stages, and implementing strong promotional measures to stimulate participation. For example, the government could offer financial subsidies or tax incentives to encourage healthcare organizations to participate in system integration, while patients’ engagement and trust could be enhanced through measures such as health management and information transparency.
-
(2)
The awareness and understanding of EHR among medical institutions and patients, as well as the level of integration among medical groups, directly affects the effectiveness of integration. It is recommended that the government enhance the awareness of the value of EHR among medical institutions and patients through specialized training and promotional activities. Additionally, policy guidance should be used to promote the development of medical consortia, thereby improving synergy and information sharing among all stakeholders in the system.
-
(3)
The sensitivity of all stakeholders to potential losses plays a critical role in system participation. The government can reduce loss-averse behaviors among medical institutions and patients by guiding stakeholders to understand the potential gains and risks in the integration process and providing risk compensation mechanisms or safeguards. Additionally, policymakers should focus on enhancing the overall sustainability of the system through risk-sharing mechanisms and reducing the decision-making burden for all stakeholders to ensure the smooth progress of EHR integration.
Limitations and future directions
This study explores the decision-making process of the three parties involved in the promotion of the hierarchical diagnosis and treatment system, which offers insights for further improvement. However, this study has certain limitations that need to be addressed. First, the data and parameter values used in the simulation may not fit the real situation well and can only give the optimal explanation within a certain range. Second, the promotion of the hierarchical medical system also involves the participation of pharmaceutical manufacturing companies, and our study only analyzes the problem from a macroscopic perspective. This aspect could be further explored in future research.
Data availability
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
References
Jing, L. B. et al. Blue Book of Healthcare: Development Report on County-Level Medical Community in China. (2022).
Lu, L. P., Wang, Z. H., Li, Y. T., Zhang, C. & Yun, Z. Z. Problems and Countermeasures of Electronic Health Record Management for Residents under the Medical Consortium of Inner Mongolia People’s Hospital. China Archives, 62–63 (2019).
Liu, H. & Liang, R. D. Research on electronic health record data governance based on the 5W1H analysis method. Beijing archives, 26–28 (2023).
Akkaoui, R., Hei, X. & Cheng, W. in 2020 Information Communication Technologies Conference (ICTC). 277–281 (IEEE).
Liu, W., Long, S., Xie, D., Liang, Y. & Wang, J. How to govern the big data discriminatory pricing behavior in the platform service supply chain? An examination with a three-party evolutionary game model. Int. J. Prod. Econ. 231, 107910 (2021).
Kabir, K. A. & Tanimoto, J. Evolutionary game theory modelling to represent the behavioural dynamics of economic shutdowns and shield immunity in the COVID-19 pandemic. Royal Soc. Open. Sci. 7, 201095 (2020).
Mu, L. L., Tu, J. T. & Fu, Y. F. Evolutionary game analysis of regulatory measures in the transportation sector and illegal occupation of emergency lanes by traffic participants. J. Beijing Jiaotong Univ. (Social Sci. Ed. 21, 76–86 (2022).
u, F. P. & Wang, W. Can price subsidies and water quality information disclosure supervision solve the problem of long promotion but little adoption of reclaimed water?—A policy simulation based on ABM. Soft Sci. 39 (01), 93–100 (2025).
Guo, P., Wang, X. & Meng, X. -r. Evolutionary game study and empirical analysis of the adoption of green coal mining technology: A case study of ITMDB. Energy 313, 134019 (2024).
Zhu, G., Wu, H. Y. & Liu, W. Research on the interaction mechanism and evolutionary trend of privacy behaviors among four entities in the context of smart healthcare. Mod. Inform. 45 (01), 135–149 (2025).
Ji, S., Zhao, D. & Luo, R. -j. Evolutionary game analysis on local governments and manufacturers’ behavioral strategies: impact of phasing out subsidies for new energy vehicles. Energy 189, 116064 (2019).
Zhu, L. L., Rong, J. M. & Zhang, S. Y. Tri-party evolutionary game and simulation analysis of drug safety and quality supervision under government incentive and penalty mechanisms. Chin. J. Manage. Sci. 29, 55–67. https://doi.org/10.16381/j.cnki.issn1003-207x.2019.0481 (2021).
Encarnação, S. et al. Paradigm shifts and the interplay between state, business and civil sectors. Royal Soc. Open. Sci. 3, 160753 (2016).
He, P., Shang, Q., Wang, X. J., Wang, T. Y. & Chen, Z. S. Evolutionary game analysis of e-commerce supply chain considering platform regulation under the live streaming+ context. Syst. Eng. Theory Pract. 43, 2366–2379 (2023).
Hosseini-Motlagh, S. M., Choi, T. M., Johari, M. & Nouri-Harzvili, M. A profit surplus distribution mechanism for supply chain coordination: an evolutionary game-theoretic analysis. Eur. J. Oper. Res. 301, 561–575 (2022).
Han, T. A. Institutional incentives for the evolution of committed cooperation: ensuring participation is as important as enhancing compliance. J. Royal Soc. Interface. 19, 20220036 (2022).
Han, T. A., Lenaerts, T., Santos, F. C. & Pereira, L. M. Voluntary safety commitments provide an escape from over-regulation in AI development. Technol. Soc. 68, 101843 (2022).
Ogbo, N. B., Elragig, A. & Han, T. A. Evolution of coordination in pairwise and multi-player interactions via prior commitments. Adapt. Behav. 30, 257–277 (2022).
Bova, P. & Di Stefano, A. Both eyes open: vigilant incentives help auditors improve AI safety. J. Physics: Complex. 5, 025009 (2024).
Shen, J. et al. Prospect theory in an evolutionary game: construction of watershed ecological compensation system in Taihu lake basin. J. Clean. Prod. 291, 125929 (2021).
Wang, S. & Liu, Q. Decentralized multi-agent collaborative innovation platform for new energy vehicle core technology breakthrough with digital empowerment: from the perspective of prospect theory. Heliyon 9 (2023).
Zhang, Z. M., Wang, X. P., Su, C. & Sun, L. H. Evolutionary game of quality coordination in shared manufacturing under different cost-benefit amortization mechanisms. J. Syst. Manage. 33, 341 (2024).
National Health Commission of China, Ministry of Finance, National Administration of Traditional Chinese Medicine & Chinese Center for Disease Control and Prevention. Notice on Carrying Out the 2024 Basic Public Health Service Work, (2024). https://www.gov.cn/zhengce/zhengceku/202409/content_6975491.htm
Anthony, D. L. & Campos-Castillo, C. A looming digital divide? Group differences in the perceived importance of electronic health records. Inform. Communication Soc. 18, 832–846 (2015).
Zhou, X. Y. Research on the value perception and promotion strategy of electronic health records. J. Med. Inf. 39, 1–8 (2018).
Abdel-Khalek, S. et al. Leveraging AI-Generated content for synthetic electronic health record generation with deep learning-based diagnosis model. IEEE Trans. Consumer Electronics (2024).
Alalawi, Z. & Zeng, Y. Toward Understanding the interplay between public and private healthcare providers and patients: an agent-based simulation approach. EAI Endorsed Trans. Industrial Networks Intell. Syst. 7, 166668 (2020).
Kai-Ineman, D. & Tversky, A. Prospect theory: an analysis of decision under risk. Econometrica 47, 363–391 (1979).
Tversky, A. & Kahneman, D. Advances in prospect theory: cumulative representation of uncertainty. J. Risk Uncertain. 5, 297–323 (1992).
Liu, N. N. & Zhou, G. H. Evolutionary analysis of resource-sharing in collaborative innovation of major projects based on prospect theory. J. Industrial Eng. Eng. Manage. 37, 69–79. https://doi.org/10.13587/j.cnki.jieem.2023.03.007 (2023).
Zhao, Z. B. & Man, Q. P. Evolutionary game analysis of risk management behavior in major infrastructure projects based on prospect theory. J. Syst. Manage. 27, 109–117 (2018).
Diao, S. J., Kuang, H. B., Meng, B. & Shi, B. F. Evolutionary game analysis of LSSC service quality control strategy based on prospect theory. Chin. J. Manage. Sci. 29, 33–45. https://doi.org/10.16381/j.cnki.issn1003-207x.2018.1536 (2021).
Li, Z. H., Qiao, G. H., Xu, X. Y. & Tian, M. H. Evolutionary game research on knowledge-sharing and collaborative Cooperation in blockchain autonomous organizations based on prospect theory. Oper. Res. Manage. 32, 139–146 (2023).
Xu, J. Z. & Xu, Y. Y. Diffusion mechanism of low-carbon technology innovation under government environmental regulations—An evolutionary game analysis based on prospect theory. Syst. Eng. 33, 118–125 (2015).
Tian, S. H. Research on the motivation mechanism of vertical integration of electronic health records in medical alliances, (2023).
Xu, J., Chen, F. J., Ma, L. T., Wang, J. Y. & Wang, Z. Tri-party evolutionary game analysis of new energy vehicle promotion policies from the perspective of prospect theory. Sci. Technol. Manage. Res. 42, 66–72 (2022).
Lyapunov, A. M. The general problem of the stability of motion. Int. J. Control. 55, 531–534 (1992).
Fan, W. et al. Evolutionary game analysis on industrial pollution control of local government in China. J. Environ. Manage. 298, 113499 (2021).
Xu, X., Liu, J., Ampon-Wireko, S., Asante Antwi, H. & Zhou, L. Towards an integrated healthcare system: evolutionary game analysis on competition and Cooperation between urban and rural medical institutions in China. Front. Public. Health. 10, 825328 (2022).
Tao, C. et al. How to promote the hierarchical diagnosis and treatment system: A tripartite evolutionary game theory perspective. Front. Psychol. 13, 1081562 (2023).
Wang, F., Yin, X. W., Shi, C. L. & Yu, L. A. Evolutionary game analysis of information-sensitive e-waste recycling based on prospect theory. Syst. Sci. Math. 44, 694–710 (2024).
Acknowledgements
The authors are grateful to the editors for their guidance and to the reviewers for their constructive suggestions.This research was supported by the Key Research Center for Humanities and Social Sciences in Hubei Province (Hubei University of Medicine) under Grant No. 2023YB006.
Author information
Authors and Affiliations
Contributions
Xinqi Hu contributed to the model building as well as the manuscript writing. and made multiple revisions for the final publication. Ruina Wang and Yuanyuan Wei supported the total work of Xinqi Hu and contributed to the empirical analysis and text writing. Hongwei Lin and Xiaomiao Gui contributed to the overall quality of literature organization and manuscript revision. All authors discussed the conclusions and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hu, X., Wang, R., Wei, Y. et al. Evolutionary game analysis of the longitudinal integration of electronic health record based on prospect theory. Sci Rep 15, 20583 (2025). https://doi.org/10.1038/s41598-025-05301-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-05301-9