Abstract
This study aimed to accessed the current status of the physical activity and the prevalence of comorbidity among the elderly (≥ 65 years old) in rural areas and to investigate the effect of physical activity intensity on hypertension-diabetes comorbidity in the elderly. A cross-sectional survey was conducted in Jia County, Pingdingshan, Henan Province from July 1 to August 31, 2023. A questionnaire was used to collect information on socio-demographic factors and chronic diseases, and the IPAQ (short form) to collect information about physical activity. Multivariate logistic regression models were performed to identify factors influencing the prevalence of comorbidity in rural areas. Propensity score matching (PSM) was performed to explore the effects of high-intensity versus low-intensity physical activity on the prevalence of comorbidity among the elderly in rural areas. In total of 16,795 participants were recruited. The prevalence of comorbidity was lower in participants with high-intensity physical activity than in those with low-intensity physical activity (45.4% vs. 58.3%). After adjusting for the effects of potential confounders, we found that the prevalence of comorbidity was higher in females (OR 1.194, 95% CI [1.122–1.271]) than in males. Participants’ education level, occupation, and income all influenced the occurrence of comorbidity. PSM analysis revealed a 13.2% difference in comorbidity prevalence between high-and low-intensity physical activity participant. The prevalence of comorbidity is lower in participants with high-intensity physical activity than in those with low-intensity physical activity in rural areas. Physical activity interventions may be strengthened to encourage the elderly to actively increase their physical activity levels. Furthermore, we advocate that more attention should be paid to the physical activity of the elderly, improving the construction of sports facilities in rural areas, and village clinics should strengthen guidance to encourage the elderly to participate in high-intensity physical activities.
Similar content being viewed by others
Introduction
In the context of global aging, the number of people aged 65 and above is rapidly increasing, and the prevalence of chronic diseases in the elderly population is rising sharply1. What is more concerning is that the majority of elderly patients with chronic diseases often suffer from multiple chronic diseases concurrently2, as, chronic diseases are often characterized by complex etiologies, insidious onsets, long duration and difficulties in treatment. The World Health Organization (WHO) defines the presence of two or more chronic diseases as chronic disease comorbidity3. Compared to having a single chronic disease, comorbidity not only seriously reduces the quality of life of the middle-aged and the elderly, but also increases the economic burden on families and society4. In China, studies have shown that by 2018,the rate of chronic disease comorbidity among middle-aged and the elderly had reached 55.77%5. making it a pressing public health challenge.
The high incidence of multiple chronic diseases in China’s rural areas echoes the challenge of global aging. The 'healthy ageing framework advocated by the World Health Organization emphasizes that integrating lifestyle interventions, such as physical activity, with primary care is a core strategy to address the burden of comorbidities. Emerging evidence suggests that higher-intensity physical activity may impose stronger physiological adaptations that are critical for mitigating comorbidity risk. For instance, high-intensity activity (e.g., aerobic exercise at 70–85% of maximal heart rate) enhances insulin sensitivity more effectively than moderate-intensity exercise in patients with metabolic disorders6,7, which is particularly relevant for hypertension-diabetes comorbidity prevalent in rural elderly populations. In response, many countries have adopted to promote healthy lifestyles, including physical activity interventions, as a novel approach to combat the rising prevalence of comorbidity8. While prior research has established the benefits of exercise for single chronic diseases (e.g., hypertension or diabetes), evidence on how physical activity intensity specifically impacts comorbidity patterns—such as the co-occurrence of hypertension and diabetes—remains sparse, particularly in rural settings. Despite significant investment in biomedical technology, these efforts have had limited success in rural areas, where awareness, treatment, and control rates of comorbidity remain substantially lower than urban counterparts. Recent national health expenditure reports indicate that rural chronic disease screening coverage remains below 40% despite a 12% annual increase in biomedical technology investments9.This calls for a shift in approach—one that emphasizes healthy aging, maintaining basic health, and improving the quality of life for the elderly through multidisciplinary, multimodal strategies that integrate healthcare, physical activity, and the establishment of healthy lifestyle systems10.
With the popularization of the concept of “Exercise is Medicine”, intervening in the intensity of physical activity which can influence the prevalence of comorbidity has become one of the basic public health strategies in a majority of countries, because Compared to medication or surgical interventions, physical activity interventions do not require additional medical costs (such as drug purchases or hospitalizations) and may indirectly reduce long-term health care costs by reducing chronic disease complications11. Numerous studies have shown that appropriate physical activity contributes to improved health outcomes in comorbid populations. However, these studies have mainly focused on the effects of physical activity in the elderly on a particular chronic disease, with limited evidence exploring the relationship between physical activity intensity and comorbidity12. Previous studies focused on the impact of physical activity on a single chronic disease, such as hypertension or diabetes, but there is still a lack of large-scale empirical evidence on the association between different intensity of physical activity and multiple chronic diseases, such as hypertension combined with diabetes. its adoption and feasibility in elderly rural populations—often constrained by limited infrastructure or cultural preferences for low-intensity activities like walking—remain underexplored. This study is the first to systematically compare the difference between high intensity and low intensity activity in rural elderly population to fill this gap.
Given this gap, public health policymakers tended to take physical activity interventions as an auxiliary means of controlling comorbidity in the elderly, rather than recognizing its pivotal role in the prevention and treatment. Surveys of Chinese rural health administrators suggest that 68% prioritized medication adherence over structured PA programs13. This highlights a potential underutilization of PA in current policies. This study aims to address this gap by examining the relationship between physical activity intensity and comorbidity prevalence employing a propensity score matching methodology. By exploring the effect of physical activity intensity on comorbidity, while minimizing the influence of potential disturbance variables, this study provides a more accurate assessment of the net benefits of different physical activity levels. This study will provide valuable theoretical insights for health promotion among the elderly in rural areas and contribute to the development of a new public health service model.
Methods
Procedures and study participants
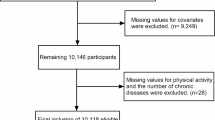
From July 1 to August 31, 2023, we conducted a cross-sectional survey in Jia County, Henan Province (one of the national demonstration areas for comprehensive prevention and control of chronic diseases). We conducted the survey simultaneously in batches, centered on the townships, with villages or communities as the units, covering 377 villages or communities across 15 townships in Jia County. Our research team consists of 70 highly trained students with a background in public health and 4–5 professional public health persons from each township. During the survey, each of the 377 villages or communities dispatched 1 to 2 general practitioners to assist throughout the investigation. Quality control personnel regularly conduct quality control check on the questionnaire to ensure the reliability and validity of the collected data. These examinations included a random examination of questionnaire records and a feedback session with the assessment team. Utilizing whole cluster sampling, we assessed hypertensive individuals aged 65 and above registered under the National Basic Public Health Hypertension Management program. Participants gave written informed consent, answered an interview questionnaire, and underwent a physical examination by trained health personnel. A total of 21,379 residents with diabetes and hypertension were included. Inclusion criteria: (1) age ≥ 65 years, clear consciousness, no communication barriers; (2) no motor disabilities, reaching the village clinics independently; (3) cooperating with the completion of questionnaires and physical examination; (4) permanent residents of the study site. Exclusion criteria: (1) those who suffered from other serious diseases and could not cooperate in completing the study N = 479 (2) those who were missing basic information N = 3507 (3) those who could not express themselves N = 598. 16,795 participants were finally included in the study. All participants provided informed consent before data collection and all data is kept strictly confidential.
Assessment of covariates
A structured questionnaire was used to collect information through face-to-face interviews, namely (1) basic demographic characteristics: sex, age, household registration, education level, marital status, occupation, annual household income, and self-reported health status; (2) disease status: Seven chronic diseases were surveyed (hypertension, diabetes, bone and joint diseases, COPD, digestive diseases, heart disease, and stroke). Comorbidity in this study was operationally defined as the concurrent diagnosis of hypertension and diabetes. In addition, we used the Age-adjusted Charlson Comorbidity Index to assess the severity of comorbidities by stratification (see Table TS9 for score details). The higher the score, the higher the severity of comorbidities14. In this study, 1 represents no comorbidity: Hypertension or Diabetes alone; 2 represents comorbidity: Hypertension and diabetes. Other chronic diseases (e.g., COPD, heart disease, etc.) were exclusively used to calculate the Age-adjusted Charlson Comorbidity Index (ACCI). The ACCI score reflects the cumulative burden of non-focal diseases but was independent of the primary comorbidity outcome. (3) physical examination indicators: height, weight, BMI was calculated as weight in kilograms divided by squared height in meters (kg/m2) (4) Lifestyle indicators: Physical activity intensity: referring to the International Physical Activity Questionnaire (IPAQ)15, which is a more widely used questionnaire for measuring the physical activity level of adults worldwide, and has good validity and reliability in our empirical studies. We used rigorous quality control procedures (e.g., trained interviewers, repeated verifications) aimed to minimize reporting errors. The situation of exercises was that an individual’s total weekly energy expenditure was calculated based on the number of days per week that the individual was engaged in low/moderate/high levels of physical activity, the length of the day, and the metabolic equivalent (MET) of each level of activity (low MET was assigned 3.3, moderate MET was assigned 4.0, and high MET was assigned 8.0). The formula is 1 week of exercise energy expenditure = MET corresponding to exercise level × duration of daily activity × number of activity days per week. And according to the International Physical Activity Questionnaire (IPAQ), the physical activity level of middle-aged and the elderly were categorized into high physical activity (assignment: ≥ 1500 MET-min/w = 3) medium physical activity (assignment: ≥ 5 days per week, each time ≥ 30 min = 2) and low physical activity (assignment: dissatisfy the medium–high physical activity = 1).
Statistical analysis
Data were entered using Epi Data 3.0. Counting data were expressed as percentages. Measurement data that conformed to normal distribution were described by mean ± standard deviation, and when they did not conform to normal distribution, they were expressed by quartiles (P25,P75). The χ2 test was used, and multivariate analyses were performed using logistic regression models. Using these to examine factors associated with the prevalence of comorbidity among the elderly while adjusting for potential confounders. In addition, we conducted a multiple linear regression analysis using SPSS to examine the association between the Age-adjusted Charlson Comorbidity Index (ACCI) and physical activity intensity. PSM was performed to minimize potential confounding bias by Logistic to select the sets of covariates whenever possible (p < 0.05). A one-to-one nearest neighbor matching algorithm was applied with a caliper value of 0.03 in our study. The Probit regression model was performed to estimate the propensity scores of participants with moderate- to low-intensity physical activity and high-intensity physical activity. Finally, 3387 were selected from 16,795 participants, and the differences in comorbidity between high-intensity physical activity and other levels of physical activity intensity were compared by using 1:1 propensity score matching, after controlling for confounders. A bilateral test was utilized, and p < 0.05 was considered statistically significant.
Results
General characteristics of participants
A total of 16,795 participants were included in this study, aged from 65 to 104, with a mean age of 73.1 ± 5.58. Among them, 7534 (44.9%) were male and 9261 (55.1%) were female. The elderly with low-intensity physical activity were 2944 (17.5%), with moderate-intensity physical activity were 10,464 (62.3%), and with high-intensity physical activity were 3387 (20.2%). 7434 (44.3%) suffered from one chronic disease, and 9361 (55.7%) suffered from comorbidity. Demographic characteristics are shown in Table 1.
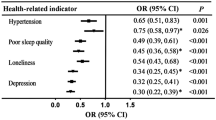
Multivariate logistic regression analysis on the prevalence of comorbidity
Multivariate logistic regression analysis was performed with whether the participants had comorbidity as the dependent variables (assignment: 0 = no 1 = yes), and intensity of physical activity as the categorical independent variables. The result showed that Participants engaging in high-intensity physical activity had a 14.3% reduced odds (OR 0.857, 95% CI [0.812–0.905], p < 0.001) of comorbidity compared to those in the low-intensity group. The absolute risk reduction (ARR) was 13.2%, indicating that one comorbidity case could be prevented for every 7.6 elderly individuals transitioning to high-intensity activity. In addition, gender, age, income, occupation, and educational background was also influencing factors for comorbidity among the elderly in rural areas (p < 0.05), as shown in Table 2, Fig. 1, TS10.
Differences in the prevalence of comorbidity among the elderly after PSM
Moderate-intensity physical activity was not associated with the prevalence of comorbidity in the elderly. Participants who were in moderate-intensity physical activity were combined with those who were in low-intensity physical activity for better propensity score matching. In total, 6774 participants from 16,795 participants were matched using PSM. The intensity of physical activity was significantly associated with the prevalence of comorbidity after PSM for gender, age, income, occupation, marital status, education, and BMI (p < 0.001). Based on the balanced samples, the differences in the prevalence of comorbidity between low- and moderate-intensity physical activity participants and high-intensity physical activity participants were shown in Fig. 1, which suggested that the prevalence of comorbidity in high-intensity physical activity participants (45.4%, 95% CI [0.531–0.65]) was still lower than that of the low- and moderate-intensity physical activity population (58.6%, 95% CI [0.872–1.03]) by 13.2% (p < 0.05). After adjusting for potential confounders in the multiple linear regression analysis, physical activity intensity showed a coefficient of − 0.82 (p < 0.001) in relation to the Age-adjusted Charlson Comorbidity Index (ACCI). In other words, as physical activity intensity increases, the ACCI score decreases, indicating a negative correlation between physical activity intensity and comorbidity burden (as shown in TS8) Notably, this finding is consistent with the results obtained from the PSM analysis. Figure 3 illustrates sex- and age-stratified differences in comorbidity prevalence after propensity score matching. While high-intensity activity males aged 65–70 showed higher comorbidity rates than females (54.2% vs. 48.9%, p < 0.05), this pattern reversed in older cohorts: females exhibited progressively greater comorbidity risks than males from ages 71–75 (58.8% vs. 52.1%), 76–80 (61.3% vs. 55.7%), and ≥ 81 years (63.1% vs. 57.4%, all p < 0.01).As shown in Figs. 2 and 3. (Balance test in TS2 and TS4).
Discussion
Physical activity status of the elderly in rural areas
The results of this study showed that the physical activity level of the elderly in rural areas was low. Only 20.2% of the elderly performed high-intensity physical activity every week, while 17.5% of the elderly did not perform physical activity every week or only performed low-intensity physical activity. 62.3% of the elderly engaged in medium-intensity physical activity. This phenomenon may be attributed to a multitude of factors, including aging, declining physical functions, and a sedentary lifestyle16, which makes the willingness of the elderly to engage in physical activity gradually decrease, and most of the elderly are only willing to do simple physical activity, such as walking, housework, and other activities. Only a minority of the elderly are willing to jogging, cycling, and other high-intensity physical activities. Walking is a relatively safer and easier way to exercise for the elderly, which may be related to the lack of knowledge and guidance on other forms of physical activity17.
Some studies have shown that the situation of chronic disease comorbidity among the elderly in China is rigorous. With the aggravation of population aging, the rate of chronic disease comorbidity among the middle-aged and elderly may continue to increase in the future18. Extensive studies have shown that there is an effective relation between the amount of physical activity and health status, with increasing physical activity will bring about cumulative health benefits19. Regular physical activity plays a positive role in preventing disease and promoting health by reducing mortality, lowering the risk of comorbidity, and improving the quality of life20. Concurrently, appropriate physical activity is beneficial to the physiology of the elderly, the functional activity of the brain and nervous system, and the quality of sleep21, and helps to improve physical and mental health. Therefore, village clinics could provide health education to the elderly about the benefits of increasing physical activity for their physical and mental health, as well as education and guidance on safety and precautions for physical activity. The elderly may benefit from active learning of simple motor skills, which could enhance their interest in exercise and facilitate the formation of a regular exercise daily routine22.
While our findings highlight the benefits of high-intensity physical activity in reducing comorbidity among ambulatory elderly populations, they may not generalize to individuals with severe mobility limitations. Policymakers should consider supplementary interventions tailored to non-ambulatory elderly populations, who face distinct barriers to physical activity and higher chronic disease risks. Such as accessible community exercise programs and home-based rehabilitation.
Comorbidity status of the elderly in rural areas
This study found that the prevalence of comorbidity among the elderly in rural areas was 55.7%. This result is slightly higher than the co-prevalence rate of chronic diseases in the elderly obtained by Xu Xiaobing et al. based on CHARLS data analysis (45.92%)23 and lower than the result obtained by Sun Ying et al. using the data of elderly inpatients in a hospital (83.74%)24. However, it is lower than the results of foreign studies, for instance, the U.S. National Health Interview Survey (NHIS) showed that the prevalence of comorbidity in the elderly over 65 years old was 63.7%25, and the comorbidity rate of the elderly of advanced age in the community of Kawasaki City, Japan was 94.7%26. Although the prevalence of comorbidity varies from study to study, it indicated that the prevalence of comorbidity was higher among the elderly in rural areas, and the situation is not optimistic. This phenomenon that the risk of comorbidity among the elderly is increasing may be attributed to the fact that the proportion of the elderly population is rising as the aging process is accelerating, and their physical functioning is declining as well as the body’s susceptibility to disease is increasing27. Simultaneously, the elderly in rural areas generally have low education levels, limited awareness of healthy lifestyles, insufficient physical exercise, unhealthy diet, with smoking and excessive drinking, and other bad lifestyles are more common28, increasing the risk of the higher prevalence of comorbidity of the elderly in rural areas. Moreover, economic reasons may also be one of the reasons for the increasing prevalence of comorbidity among the elderly in rural areas. The elderly in rural areas have a single source of income, mainly relying on renting out their cultivated land or selling their food crops as well as government subsidies to obtain income. Chronic comorbidity requires long-term medication and regular checkups, but most of the elderly can only choose cheap therapeutic drugs, and it is even harder for them to undergo regular checkups, which makes it difficult to ensure the effectiveness of drug treatment29. Moreover, due to the age-related decline in self-control and memory, it is easy for the elderly to forget to take their medication, which undoubtedly increases the burden of disease on the elderly30.
Factors influencing the decrease in the prevalence of comorbidity in participants with high-intensity physical activity
This study found that the prevalence of comorbidity decreased by 13.2% in participants who performed high-intensity physical activity after matching the variables of gender, age, occupation, education, income, marital status, and BMI. it means that with the increase of intensity of physical activity, the probability of comorbidities decreases in the elderly. This decrease may be related to the fact that the level of physical activity in the elderly has an impact on bone mineral density. Studies have found that the elderly with insufficient physical activity mostly have abnormal bone density compared with those with sufficient physical activity31. Previous studies have established a close relationship between physical activity levels and bone density, with higher activity levels being associated with a lower risk of low bone density32. The higher the physical activity levels are, the less prone to low bone density problems. Studies have shown that gradually increasing daily activity levels can prevent the decrease in bone density for postmenopausal elderly females; increasing physical activity and exercise can improve bone health for both elderly males and females33,34. Therefore, elderly individuals with insufficient physical activity should be encouraged to exercise more to maintain bone density and reduce the risk of fragility fractures. However, this does not mean that the elderly can carry out high-intensity physical activities without concern, and the exercise intensity and exercise time should be reasonably arranged according to their actual situation to avoid the possibility of injury caused by exercise.
Gender differences in comorbidity prevalence in rural areas
Our analysis revealed sex-specific differences in comorbidity prevalence across age groups (Fig. 3). High-intensity physical activity reduced comorbidity prevalence overall, but age- and sex-stratified analyses revealed nuanced patterns. While males aged 65–70 engaging in high-intensity activity paradoxically exhibited higher comorbidity rates than females (54.2% vs. 48.9%), this trend reversed sharply after age 70, with older females (≥ 71 years) experiencing disproportionately greater risks than males in the same age groups (p < 0.01).This divergence likely stems from sex-specific biological trajectories (e.g., postmenopausal metabolic shifts in women) and rural occupational exposures. Which is similar to the findings of Yuan Yupeng35. In rural areas, where physical labor is predominant, men are mainly engaged in higher-intensity agricultural activities, such as construction, and heavy lifting, while women often perform lower-intensity housework, resulting in lower overall activity for women. In addition, we also found that the prevalence of comorbidity among females who engaged in high-intensity physical activity increased with age. The reason for this may be related to female-specific physiological factors36. Domestic and foreign studies consistently agreed that this phenomenon may be related to female-specific physiological factors and longer average life expectancy. On the one hand, Females are at increased risk of chronic comorbidity due to pregnancy, menopause, and so forth, resulting in poorer health for females compared to males. On the other hand, female bear multiple responsibilities, including caring for the family, providing for elderly parents, and farming, while the medical services available to them are more limited37. As women age, it is no longer appropriate for them to engage in high-intensity physical activity. It is recommended that females actively participate in other types of physical activity, such as square dancing, traditional Chinese medicine health exercises, Baduanjin exercise, and other moderate-intensity exercise programs, to increase their level of physical activity38.
Occupational differences in the prevalence of comorbidity in rural areas
The results of the study showed that different occupations also had an impact on the prevalence of comorbidity among the elderly in rural areas. In the present study, 43.7% of the elderly people whose occupation was farming did not suffer from comorbidity, 45.1% of the elderly whose occupation was housework did not suffer from comorbidity, and 46% of the elderly with other occupations did not suffer from comorbidity. It indicated that farming in rural areas could be used as a way of high-intensity physical activity for the elderly, based on which they can appropriately participate in low-intensity physical activities to avoid the harm caused by overwork to the body. It is also necessary to pay more attention to the non-farmers39 and to increase the activity time and activity intensity of this group accordingly. For people engaged in non-agricultural labor, low-intensity physical activity should be supplemented with high-intensity physical activity with a weekly metabolic equivalent of ≥ 1500 MET-min/w. Surveys have found that non-farmers in rural areas generally spend a lot of time sitting still, and a large number of studies have shown that long sitting time is often significantly correlated with low levels of physical activity40. Health interventions may be necessary to encourage non-farmers to engage in more physical exercise, reduce sedentary behavior, and adopt healthier lifestyles41.
Strengths and weakness of this study
There are several strengths in our study. First, it is a big survey conducted among the elderly across an entire county, allowing for more comprehensive data on the aggregation of diseases in rural areas. Second, the large sample size and scientific methodology, particularly the use of PSM, we employed PSM analysis to exclude confounding variables when exploring the association between physical activity and comorbidity prevalence. This study goes beyond previous research in its scope and depth of analysis. Third, it specifically examined the effects of high-intensity physical activity on comorbidity, expanding the research on the relationship between physical activity and comorbidity. Last, The ACCI served as a supplementary tool to control for variations in overall disease burden arising from conditions other than hypertension and diabetes. For instance, participants with higher ACCI scores (indicating severe comorbidity beyond hypertension/diabetes) showed lower adherence to physical activity interventions. This stratification underscores that our findings on physical activity and hypertension-diabetes comorbidity remain statistically robust even in participants with additional chronic diseases. However, some limitations exist. First, while this study identified associations between gender, age, physical inactivity, and chronic diseases, it could not establish causality. Across-sectional nature of the study design may be another limitation that precluded the establishment of cause-and-effect associations. Second, the self-reported nature of physical activity data via the IPAQ short form introduces potential social desirability and recall biases. Participants may have overestimated their activity levels due to a tendency to report socially acceptable behaviours or inaccurately recalled the duration and intensity of their physical activities over the past 7-day period. These biases could lead to misclassification of high- versus low-intensity activity groups, thereby affecting the validity of the observed associations. The IPAQ’s 7-day recall period may also fail to capture long-term physical activity patterns, which could influence chronic disease outcomes. These limitations highlight the need for future studies to incorporate objective measures and longer monitoring periods to validate self-reported data and strengthen causal inferences. Third, while PSM was used to control for known confounders, unknown covariates may still have influenced the results. unmeasured variables such as dietary habits, medication use, and broader social determinants of health were not considered, which could influence comorbidity prevalence. Future research should prioritize the use of objective measures (e.g., accelerometers) to validate self-reported physical activity data and address these biases. Longitudinal designs are needed to clarify temporal relationships and disentangle the effects of activity intensity on comorbidity. Fourth, while we employed whole-cluster sampling to reflect real-world population structures in rural healthcare settings, our analysis did not formally assess or adjust for intra-cluster correlation (ICC). Although propensity score matching (PSM) helped control individual-level confounders, residual clustering effects may persist if health behaviors or environmental factors shared within villages influenced outcomes. This limitation suggests that estimates of physical activity benefits could be marginally overprecise. Future investigations should incorporate multilevel modeling to disentangle individual- and cluster-level effects on comorbidity risk among rural elderly populations.
Conclusions and implications
This study found that healthier individuals might engage in more high-intensity exercise in rural areas. Besides, the prevalence of comorbidity is influenced by a variety of factors, including gender, age, and occupation. It is recommended that the farming population maintain a balance between high-intensity physical activity (at least three days per week for 63 min per time each session) and low-intensity activity to optimize health benefits while avoiding overexertion. Moreover, we may pay more attention to the non-farming population, encouraging an increase in both the intensity and duration of physical activity to mitigate the harmful effects of a sedentary lifestyle. Additionally, Given the heightened comorbidity risk among women—particularly those aged ≥ 71—tailored interventions should address age- and sex-specific barriers. While older women may benefit from community-based exercise promoting more frequent engagement in physical activities and the development of healthy exercise habits. For younger men (65–70 years), appropriate increases in the intensity or duration of physical activity should be considered.
Data availability
The data set for the current study has not been made public, but are available from the corresponding author on reasonable request.
References
Chou, C. Y. et al. Disease-related disability burden: A comparison of seven chronic conditions in middle-aged and older adults. BMC Geriatr. 21(1), 201 (2021).
Jiang, G. Development and innovation of prevention and control of chronic noncommunicable diseases in China. Chin. J. Prevent. Control Chronic Dis. 30(6), 406–407 (2022).
Tang, T. et al. Chinese Geriatrics Society. Chinese expert consensus on the term and definition of multimorbidity in older adults. Chin. J. Geriatr. 41(9), 1028–1031 (2022).
Doncheva, A. I. et al. Extracellular vesicles and microRNAs are altered in response to exercise, insulin sensitivity and overweight. Acta Physiol. (Oxf.) 236(4), e13862 (2022).
Nguyen, L. T. K. et al. Physical activity and diet quality modify the association between comorbidity and disability among stroke patients. Nutrients 13(5), 1641 (2021).
Zheng, Q., Liu, S. & Xie, L. Investigation and prognostic analysis of chronic disease co-morbidity in the elderly population. J. Public Health Prevent. Med. 35(3), 103–106 (2024).
Wang, H., Zhang, L., Fang, X., et al. Prevalence and spatial analysis of chronic comorbidity among chinese middle-aged and elderly people. Chin. Gen. Pract. 25(10), 1186–1190, 1196 (2022).
Tiffany, B. et al. A systematic review and meta-analysis of adherence to physical activity interventions among three chronic conditions: cancer, cardiovascular disease, and diabetes. BMC Public Health 19(1), 636 (2019).
National Health Commission. China Health Statistical Yearbook 2022 (Peking Union Medical University Press, 2022).
Yao, S. et al. Prevalence and patterns of multimorbidity in a nationally representative sample of older chinese: Results from the china health and retirement longitudinal study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 75(10), 1974–1980 (2020).
Zhu, Q. & Li, H. On the latest development of the intervention on chronic diseases by exercise in China. Phys. Educ. Rev. 38(11), 98–99 (2019).
Gobbens, R. J. Cross-sectional and longitudinal associations of environmental factors with frailty and disability in older people. Arch. Gerontol. Geriatr. 85, 103901 (2019).
Yu, Y. et al. Association between physical exercise and biomarkers of oxidative stress among middle-aged and elderly community residents with essential hypertension in China. Biomed. Res. Int. 2018, 1–11 (2018).
Yi, B. C. et al. Efficacy of the modified frailty index and the modified Charlson comorbidity index in predicting complications in patients undergoing operative management of proximal humerus fracture. J. Shoulder Elbow Surg. 30(3), 658–667 (2021).
Qu, N. & Li, K. Study on the reliability and validity of international physical activity questionnaire (Chinese Vision,IPAQ). Chin. J. Epidemiol. 3, 87–90 (2004).
Wang, J. et al. Analysis on combinations of multimorbidity in the elderly in shanghai communities and the influence factors. Geriatr. Health Care 23(2), 97–101 (2017).
Cai, W., Xie, H., Wang, F. et al. Analysis on status and influencing factors of physical inactivity among the elderly in community. Chin. J. Gen. Pract. 20(7), 1170–1173, 1177 (2022).
Yan, Z. & Chen, D. Research progress on the patterns of multimorbidity. Chin. J. Dis. Control Prevent. 27(4), 471–475 (2023).
Yu, R. et al. Is neighborhood green space associated with less frailty? Evidence from the Mr. and Ms. Os (Hong Kong) study. J. Am. Med. Directors Assoc. 19, 528–534 (2018).
Gu, S., Zhang, X. & Peng, Y. A serial mediation model of physical exercise and loneliness: the role of perceived social support and resilience. BMC Geriatr. 24, 811 (2024).
Wu, W. et al. The effects of traditional exercises on sleep quality in older adults:a Meta-analysis. Chin. J. Nurs. 51(2), 216–224 (2016).
Duan, Y. M. et al. Physical exercise helped to maintain and restore functioning in chinese older adults with mild cognitive impairment: A 5-year prospective study of the Hong Kong Memory and Ageing Prospective Study (HK-MAPS). J. Am. Med. Dir. Assoc. 18(4), 306–311 (2017).
Xu, X. et al. Analysis of chronic diseases comorbidity among the elderly in China based on association rules. Chin. J. Prevent. Control Chronic Dis. 29(11), 808–812 (2021).
Tom, O. D., Laura, D. & Fiona, W. Exercise and physical activity in systemic lupus erythematosus: A systematic review with meta-analyses. Seminars Arthritis Rheumatism 47(2), 204–215 (2017).
Boersma, P., Black, L. I. & Ward, B. W. Prevalence of multiple chronic conditions among US adults, 2018. Prev. Chronic Dis. 17, 200130 (2020).
Takayuki, A. et al. Association between multimorbidity, self-rated health and life satisfaction among independent, community-dwelling very old persons in Japan: Longitudinal cohort analysis from the Kawasaki Ageing and Well-being Project. BMJ Open 12(2), e049262 (2022).
Zhao, H., Wang, Z., Ma, T. Research on influence of chronic disease comorbidity on depressive symptom among middle-aged and elderly people in China based on propensity score matching. Med. Soc. 35(6), 127–132, 144 (2022).
Wang, M. et al. Prevalence rate of multiple chronic conditions in middle-aged and elderly chinese people from 2010 to 2019: A meta-analysis. Chin. Gen. Pract. 24(16), 2085–2091 (2021).
Franchi, C. et al. Medication adherence in community-dwelling older people exposed to chronic polypharmacy. J. Epidemiol. Community Health 75(9), 854–859. https://doi.org/10.1136/jech-2020-214238 (2021).
Hauger, A. V. et al. Physical capability, physical activity, and their association with femoral bone mineral density in adults aged 40 years and older: The Tromsø Study 2015–2016. Osteoporos. Int. 32(10), 2083–2094 (2021).
Segev, D., Hellerstein, D. & Dunsky, A. Physical activity-does it really increase bone density in postmenopausal women? A review of articles published between 2001–2016. Curr. Aging Sci. 11(1), 4–9 (2018).
McMillan, L. et al. Physical activity for the prevention and treatment of osteoporosis in older adults. Healthcare 5(4), 85 (2017).
World Health Organization. Physical status: The use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 854:1–452 (1995).
Subramaniam, M. et al. Patterns of physical activity and health-related quality of life amongst patients with multimorbidity in a multi-ethnic Asian population. BMC Public Health 19(1), 1612 (2019).
Chudasama, Y. V. et al. Physical activity, multimorbidity, and life expectancy: A UK biobank longitudinal study. BMC Med. 17(1), 108 (2019).
Sun, Y. & Zhang, L. Consensus on health management of climacteric women in primary medical institutions edition. Chin. Gen. Pract. 24(11), 1317–1324 (2021).
Xu, X. et al. The differences and influencing factors of chronic comorbidities among urban-rural elderly people in China. Chin. J. Prevent. Control Chronic Dis. 31(06), 427–432 (2023).
Ye, B., Gao, J. & Fu, H. Associations between lifestyle, physical and social environments and frailty among Chinese older people: A multilevel analysis. BMC Geriatr. 18, 314 (2018).
Liang, C., Wang, Y., Wang, P., et al. Physical activity and its influencing factors among rural residents in eastern, central, and western provinces of China. Mod. Prevent. Med. 49(20), 3730–3735, 3765 (2022).
Virginia, B. K. et al. Effects of physical activity in knee and hip osteoarthritis: A systematic umbrella review. Med. Sci. Sports Exerc. 51(6), 1324–1339 (2019).
Seo, Y. et al. Differences in the association of neighborhood environment with physical frailty between urban and rural older adults: The Korean Frailty and Aging Cohort Study (KFACS). J. Am. Med. Dir. Assoc. 22(3), 590-597.e1 (2021).
Acknowledgements
All authors thank all participants involved in the study.
Funding
The series of cohort studies on healthy lifestyle in tertiary hypertension population (20230013B/20230014B/20230015B).
Author information
Authors and Affiliations
Contributions
Conceptualization: XiaoLi FU, ChiWen Wang, YaoYing Wang, LiJun Gong, Han Liu, ZhanLei Shen, DongFang Zhu, JingBao Zhang, RuiZhe Ren, JunWen Bai, JinXin Cui, MingYue Zhen, JiaJia Zhang, Xinran Li, YuDong Miao. Data curation: Xiaoli FU, ChiWen Wang, YaoYing Wang, Lijun Gong, Han Liu, ZhanLei Shen, DongFang Zhu, JingBao Zhang, RuiZhe Ren, JunWen Bai, JinXin Cui, MingYue Zhen, JiaJia Zhang, XinRan Li, Yudong Miao. Formal analysis: XiaoLi FU, ChiWen Wang, YaoYing Wang, LiJun Gong, Han Liu, ZhanLei Shen, DongFang Zhu, JingBao Zhang, RuiZhe Ren, JunWen Bai, JinXin Cui, MingYue Zhen, JiaJia Zhang, XinRan Li, YuDong Miao Funding acquisition: XiaoLi Fu, YuDong Miao. Investigation: XiaoLi FU, ChiWen Wang, YaoYing Wang, LiJun Gong, Han Liu, ZhanLei Shen, DongFang Zhu, JingBao Zhang, RuiZhe Ren, JunWen Bai, JinXin Cui, MingYue Zhen, JiaJia Zhang, XinRan Li, Yudong Miao.Methodology: XiaoLi Fu, YuDong Miao, ChiWen Wang. Project administration: XiaoLi Fu, YuDong Miao.Resources: XiaoLi Fu, YuDong Miao. Software: ChiWen Wang. Writing—original draft: ChiWen Wang. Writing—review & editing: XiaoLi Fu, YuDong Miao, ZhanLei Shen. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the Zhengzhou University Medical Ethics Committee (number: 2023-318). All participants provided informed consent before data collection and all data is kept strictly confidential. The data set for the current study has not been made public, but are available from the corresponding author on reasonable request.
Statement
All methods were carried out in accordance with relevant guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fu, X., Wang, C., Wang, Y. et al. The association between physical activity and the prevalence of comorbidity: a cross-sectional survey. Sci Rep 15, 21040 (2025). https://doi.org/10.1038/s41598-025-06064-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-06064-z