Abstract
Pediatric acquired brain injuries (ABIs) may cause significant cognitive deficits. Early rehabilitation is recommended, but there is no solid evidence on the best intervention formats. This randomized clinical trial investigated the efficacy of two multidomain cognitive interventions for children aged 5:0–17:11. A personalized intervention was compared with an intervention providing a fixed-dose cognitive stimulation. 40 children were randomized into the 2 study arms and received 12-week rehabilitation (3 45-minute daily sessions for 5 days per week). 34 children completed the intervention and were assessed at baseline (T0) and post-intervention (T1). Visual sustained attention and other cognitive measures of attention, memory, visual-spatial/visual-constructional abilities and executive functions were primary and secondary outcomes, respectively. Primary and 14 of the 16 secondary outcomes showed an improvement at T1 with a medium-to-very-large effect, but training effects could not be disentangled from spontaneous recovery. No differences were found between interventions, likely because of the prolonged multidomain stimulation provided by both of them, which might have been helpful in improving the widespread cognitive deficits of children in both groups. Therefore, while for the chronic phase the guidelines recommend a personalized approach, in the early phase of recovery a standardized intervention may also be effective.
Similar content being viewed by others
Introduction
Acquired brain injury (ABI) is one of the principal causes of death and disability among children and young people1,2,3,4,5. ABI refers to any damage to the brain that occurs after birth, either of traumatic (traumatic brain injury-TBI) or non-traumatic etiology (non-traumatic brain injury-non-TBI, including cerebrovascular accidents, hypoxic events, cerebral infections etc.)6. Neurological impairments associated with ABI may include an initial Disorder of Consciousness and, usually, subsequent motor, linguistic and cognitive deficits4,7,8. With respect to cognitive functioning, in addition to intellectual abilities, specific cognitive domains, such as attention, memory, visual-spatial abilities, executive functions and social cognition skills, are affected, with a negative impact on academic functioning, behavioral outcomes and social integration, also in the long-term8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25.
Injury severity, etiology, age at the event and coma duration predict persisting cognitive impairments15,18,19,21,22,23,24,25, with children generally having poorer recovery than adults15,22,23. This is because cognitive functions develop during infancy, childhood and adolescence, and injuries in these periods may consistently alter their normal developmental pattern, with a frequent worsening over time after a recovery plateau15,22,26. Persisting cognitive impairments are reported in a wide range of patients16,18,26,27.
Hence, there is a need to provide interventions that target cognitive abilities in this population to support recovery and adjustment in daily life. It has been suggested that treatments should start as early as possible, already in the subacute phase8,28. Nevertheless, while specific recommendations for the rehabilitation of cognitive functions have been provided for adults with ABI and important efforts have been made in identifying the most effective and evidence-based interventions29,30,31,32,33, there is a lack of scientific evidence on the best treatments to adopt in the pediatric population34,35,36. A systematic review published in 201937 reported updated guidelines for effective treatments of children with ABI, indicating evidence for family/caregiver-focused interventions, as well as interventions aimed to directly improve attention, memory, executive functioning, and emotional/behavioural functioning. Despite these efforts, heterogeneity in participant inclusion criteria and methodological shortfalls of examined studies limited comparability and, thus, generalizability of findings. Hence, there is a significant need to develop and improve specific interventions for children with ABI and to design studies on their efficacy including more stringent inclusion criteria and an examination of the effects of their specific rehabilitation components38.
This study is a randomized controlled trial (RCT) aimed at assessing and comparing the efficacy of two multidomain cognitive inpatient interventions for children aged 5–17 years with moderate-to-severe ABI in the subacute phase, immediately after the emergence of consciousness. Due to the interconnected nature of brain networks39,40, cognitive deficits after emergence from a disorder of consciousness are generally multiple and complex, involving different cognitive domains that reciprocally influence each other8,41– 42. For this reason, for both interventions a multidomain cognitive stimulation was used, for which positive effects for patients with ABI in the chronic phase have already been reported in previous studies43,44,45,46,47. However, the long-term and far-transfer (transfer to untrained cognitive abilities) benefits of such a stimulation have been questioned and evidence seems to support improvements only after prolonged stimulation of each cognitive ability48,49,50,51,52. Thus, the two interventions tested in this study were designed to target various cognitive domains for a long period. This was done by using an intensive rehabilitation approach (3 45-minute daily sessions for 5 days a week for a total of 12 weeks) including neuropsychological, speech therapy and psychoeducational treatments. Both interventions focused on the level of functions (the ability to perform a specific neuropsychological task, e.g., to remember target stimuli in a memory task) or activities (the ability to use a specific cognitive function in daily tasks, e.g. to remember important daily tasks)38.
The interventions targeted the cognitive domains of attention, memory, visual-constructional abilities, and executive functioning. These domains were selected as they are not only primary rehabilitation targets in children with ABI34,38,48,52,53 but have also shown improvement in previous interventions focused on functions and activities37,38,48,49,52 similar to those in this study. Within the ___domain of executive functioning, social cognition was included as a target subdomain. Research has shown that social cognition is frequently impaired in individuals with ABI54,55,56,57, and studies have begun to investigate the neurological mechanisms underlying these deficits in children9,58. Recent guidelines for cognitive rehabilitation after ABI have highlighted that social cognition skills are often omitted from assessment and rehabilitation protocols59,60,61,62, despite repeated emphasis on their importance9,58,61,62,63. Therefore, the interventions of this study were specifically designed to address also this subdomain.
The intervention component which this study focused on was treatment personalization based on patient cognitive profile vs. treatment standardization. With this aim, a personalized cognitive treatment was compared with one providing a fixed-dose rehabilitation on the various cognitive abilities. Specifically, in the personalized intervention, named ‘COgnitive REehabilitation for ABI’ -CORE-ABI-, each patient received greater stimulation of the most deficient cognitive function(s), while at the same time being trained on all the other functions. This intervention method was based on the hypothesis that a person-centered process, with flexible activities tailored to the individual’s needs, could lead to the best outcomes37,48,64. Differently, the second intervention, named ‘SEquential Treatment for ABI’ -SET-ABI, relied on a fixed-dose stimulation of each cognitive function following a sequential order, based on a ‘bottom-up’ model65. This format was supported by the hypothesis that an improvement in basic cognitive skills is an essential precondition for the rehabilitation of higher-order cognitive abilities66,67. It is important to note that, because they were delivered in a neurorehabilitation setting, both interventions were not only based on drill-based exercises, but also benefited from therapists teaching instructions, metacognitive strategies and rules. This more comprehensive and integrative rehabilitation approach has been indicated to provide more advantages to patients with ABI64, also in the pediatric age38,48,68.
However, as the best intervention format to sustain cognitive recovery in children with ABI is still under debate38,48,53, this study could provide new insights, by evaluating the effects of early multidomain inpatient interventions and by assessing if a personalized approach could lead to better effects than a standardized rehabilitation approach. The study has several relevant features: first, the included interventions were started early, in the subacute phase following acute ABI, which is a phase where research on the efficacy of cognitive interventions is very limited. As far as we know, there are no RCTs that analyzed the efficacy of cognitive inpatient rehabilitation in the subacute phase (< 3 months after the event) in children aged 5–17 years48,53, so this study is unique in the field. Only two studies69– 70 have examined the effectiveness of cognitive rehabilitation, implemented with the same individualized intervention approach, in 11- to 18-year-olds who had experienced an ABI (specifically, a mild or severe TBI) in the previous 1–6 months. However, such an intervention was web-based, delivered at home, and focused primarily on the level of adaptive behavior rather than on functions or activities, differing in key components from the interventions included in this study. Thus, the present study may provide important information on inpatient clinician-delivered interventions aimed to enhance specific cognitive domains at an early stage of recovery from an ABI. Second, interventions of this study were unusually intense, consisting of 12 weeks of training, 5 days a week, with 3 daily 45 min sessions, for a total of 135 h of rehabilitation. Overall treatment duration (intended as total hours of treatment) of interventions for children with ABI reported in the literature up to 201738 was significantly lower. Specifically, those that consisted of drill-based exercises had an average duration ranging approximatively from 6 to 24 h total38; differently, those that combined metacognition/strategy use and drill-based exercises generally had a longer duration38, but the maximum total treatment hours slightly exceeded half of the rehabilitation hours provided by the interventions of this study. Third, the characteristics of the exercises and activities offered for each cognitive ___domain by the interventions of this study are clearly detailed in this paper (see Supplementary Information 1), which enables other clinicians and researchers to replicate the rehabilitation and study methodology. Fourth, the measures used to assess outcomes were all standardized and performance-based, which should ensure stronger empirical evidence.
To examine intervention efficacy, we assessed a wide range of cognitive outcomes, in light of the treatments’ multidomain stimulation. We identified as primary outcome visual sustained attention, which has been reported by extant literature to be crucial for the development of higher order cognitive abilities71,72,73. In addition, attention network alterations have been found to be associated with various cognitive impairments in children with ABI42, supporting the choice to identify this cognitive ___domain as primary outcome. At a methodological level, sustained attention was heavily stimulated by both study treatments, either directly, by using ad hoc exercises, or indirectly, by requiring children to stay quiet and pay attention to challenging cognitive activities for a long period of time.
This work was developed in a rehabilitation center with several decades of specific expertise in the pediatric field. This allowed a neurodevelopmental approach to the implementation of the rehabilitation interventions, as adult procedures cannot be adopted with children, especially when considering cognitive abilities36. The data of this study allow the pediatric rehabilitation community to get informed about effective tools to improve patients’ outcomes in order to enhance the quality of care provided and could also help draw more accurate guidelines for children, which are still lacking in the literature. Based on findings from previous studies and recommendations available in extant literature on the usefulness of a personalized approach37,6474–77, we hypothesized that both treatments of the present study would lead to cognitive benefits, but that the personalized CORE-ABI treatment could provide more consistent and widespread gains.
This study included only moderate-to-severe ABI, as mild injuries are associated with multifactorial nature of cognitive complaints and evaluating cognitive outcomes after rehabilitation across severity levels could be challenging, as reported by a team of experts on neurocognitive rehabilitation for TBI29. This fact, together with the choice of a very narrow time frame from the ABI to implement interventions, may have reduced the sources of variation that could adversely affect the investigation of intervention efficacy.
Materials and methods
Study design and procedure
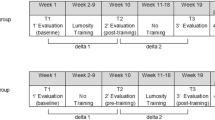
The present study is a single-blind RCT including two groups, the CORE-ABI group, receiving a mutidomain cognitive stimulation through a personalized approach, and the SET-ABI group, receiving a cognitive stimulation through a bottom-up approach identical for each participant. Participants were allocated to intervention groups according to a 1:1 ratio.
The study is registered with ClinicalTrials.gov with identifier NCT04499092 (05/08/2020).
Children were recruited while being inpatients in the Acquired Brain Injury Unit of Scientific Institute IRCCS Eugenio Medea, Bosisio Parini, Lecco, Italy. The study Principal Investigators (V.P. and S.S.) identified those children meeting study eligibility criteria. Then, a research assistant presented the study to parents (all participants were underage children), providing detailed information on study objectives and methodology. In case of willingness to participate, all parents were required to sign a written informed consent.
Demographic and clinical data of all patients enrolled in the study were collected before randomization. Allocation of children to groups and pre-treatment evaluation were scheduled within one week of receipt of informed consent. Cognitive evaluations were conducted at pre-treatment (T0) and immediately after the treatment (T1). All data were inserted in a password protected database, to which access was permitted to the research Principal Investigators and members of the research team responsible for data management.
No change to methods after trial commencement was performed.
Recruitment for this study started on 01.10.2019 and the study ended on 31.12.23. The study stopped at the reaching of the established sample size.
Ethics declaration
This study was approved by the Ethical Committee of Scientific Institute, IRCCS E. Medea, Bosisio Parini, Lecco, Italy (project number 607 Rev.1–v.1) on 25.02.2019.
Study procedures were conducted in accordance with the protocol and the principles of the 1964 Declaration of Helsinki and subsequent amendments.
This study was conducted in accordance with CONSORT guidelines for non-pharmacological interventions78,79.
Informed consent was obtained from all legal guardians of children participating in the study.
Sample size and power calculation
Effect size and power calculations were calculated using G*Power (latest ver. 3.1.9.7; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany; http://www.gpower.hhu.de/)80. With a statistical power of 0.8 and an alpha level of p = 0.05, an a-priori power calculation suggested that a total sample size of N = 40 (20 per group) allowed detecting a moderate effect size f = 0.25 for our 2 × 2 (2 timepoints x 2 groups) linear mixed model statistics, with a correlation of 0.40 among repeated measures. The effect size was estimated based on the average effect size related to the effects on various outcomes of cognitive training programs for children with ABI reported by previous literature48, considering the lowest effect levels (i.e. moderate effect) to be conservative.
Due to limited sample size, no stratification was planned for patients’ allocation.
Randomization and blinding
Participants were randomized to either the CORE-ABI (G1) or the SET-ABI (G2) group, applying a coin flip procedure. Specifically, randomization was generated by an independent statistician prior to RCT start by using the randomization tool of Microsoft Excel: an automated numerical identifier was associated in a random manner to each patient, determining allocation to G1 (0 to 0.49) or G2 (0.50 to 1). The generated numerical identifiers of patients with group allocation were reported on a sheet, which was then delivered to the research team. The research team progressively assigned patients to groups based on the numerical identifier, which followed recruitment order. The research team was not blinded to allocation, as it was not possible to conceal this information in the clinical neurorehabilitation setting. In fact, weekly meetings between the neuropsychologists of the research team and patients’ referring clinical staff were conducted to discuss patients’ clinical status, update treatment objectives, share environmental recommendations, suggest external aids to be used etc. Differently, families and participants were not informed about which intervention they had been assigned to and also assessors were blinded to patients’ allocation. Thus, this is a single-blinded RCT.
Participants and eligibility criteria
To be eligible for the study, children had to meet the inclusion and exclusion criteria described below.
Inclusion criteria were:
-
age: 5.0-17.11 years.
-
diagnosis: moderate to severe ABI assessed through Glasgow Coma Scale (GCS)81: score ≤ 12 at injury or onset;
-
Level of Cognitive Functioning Assessment Scale (LOCFAS;82) score at enrollment in the study > 5, thus excluding a confusional state;
-
time between the event and first study cognitive assessment < 3 months, with patients being in a subacute phase, immediately after the emergence of consciousness.
Exclusion criteria were:
-
a documented history of previous neurological or neurodevelopmental disorders (i.e., autism, learning disorders, attention disorders etc.);
-
ABI due to brain tumor;
-
presence of severe motor impairments or sensory deficits, causing the need for a device or the mediation of a therapist for communication, perception and/or execution of activities;
-
presence of aphasia, apraxia, acalculia or hemispatial neglect, which are more frequently associated with focal brain injury29,83.
Interventions
Both the interventions used in the study, namely the CORE-ABI (personalized treatment) and the SET-ABI (sequential treatment) interventions, had a duration of 12 weeks. Specifically, 3 daily individual rehabilitation sessions were delivered to each patient 5 days per week, for a total of 60 days of treatment,180 rehabilitation sessions and 135 h of intervention. The 3 daily sessions consisted of one session of neuropsychological treatment, one of speech therapy treatment and one of psycho-educational treatment, each lasting 45 min. Two psychologists with expertise in neuropsychology delivered the neuropsychological treatment, two speech therapists delivered the speech-therapy treatment and two professional educators delivered the psycho-educational treatment. Their involvement with patients assigned to the two groups was randomly determined.
Both the CORE-ABI and the SET-ABI interventions aimed to improve the following cognitive domains: attention, visual-spatial/visual-constructional abilities, memory and executive functions. However, whereas in the CORE-ABI intervention each child was primarily trained on his/her most deficient cognitive function(s), in the SET-ABI intervention a fixed-dose cognitive stimulation was provided.
Exercises used in the rehabilitation sessions were pencil and paper activities, computer-based exercises or games, both ad-hoc-created and common board ones. All the activities were previously classified by the research team and therapists based on the cognitive function(s) addressed. If the same activity or game could be used for the stimulation of more than one cognitive ___domain, a clear description of its different use was provided. Further, exercises were classified based on children’s age and difficulty level and were assigned to each rehabilitation setting: neuropsychological treatment, speech therapy treatment or psycho-educational treatment. Exercises assigned to neuropsychological treatment primarily involved visual stimuli or non-verbal auditory stimuli, those assigned to speech therapy treatment mostly included verbal or written stimuli (such as phonemes/graphemes, letters, words or short stories), while those assigned to psycho-educational treatment were mostly board games or activities based on concrete stimuli, frequently having high similarity to every-day activities.
Each therapist received a list of exercises to adopt according to the specific cognitive function to train and patients’ characteristics.
A detailed description of interventions and related methodology is provided below.
SET-ABI intervention
In the SET-ABI intervention, the stimulation of cognitive functions was provided following a sequential order, identical for each child and for each session in each setting (neuropsychological treatment, speech therapy treatment and psychoeducational treatment). Each session had a duration of 45 min.
Specifically, the first three weeks (weeks 1–3) of treatment targeted attention, with the stimulation of selective attention in week 1, sustained and divided attention in week 2 and inhibition and shifting in week 3. In weeks 4–6, the ___domain of visual-spatial and visual-constructional abilities was addressed, with training of visual-perceptual abilities in week 4, visual-spatial abilities in week 5 and visual-constructional abilities in week 6. In weeks 7–9, memory was the target ___domain, with training of short-term memory in week 7, long-term memory in week 8 and working-memory in week 9. In weeks 10–12, executive functions and socio-emotional skills were addressed, with the stimulation of categorization/reasoning/abstraction in week 10, problem-solving/planning in week 11 and socio-emotional skills in week 12. Therefore, each cognitive ___domain was addressed for a total of 33.75 h.
During monitoring meetings scheduled at the end of each rehabilitation week, the neuropsychologists reviewed the exercised performed by the child in the intervention sessions in each setting (each therapist provided a folder reporting activities and performance score of each child), but did not provide specific recommendations based on patients’ strengths and weaknesses. Neuropsychologist weekly supervision had the aim to ensure treatment fidelity and manage eventual therapist difficulties.
Supplementary Information 1 reports the exercises and activities delivered for each cognitive ___domain in the different rehabilitation settings.
CORE-ABI intervention
In the CORE-ABI intervention, the stimulation of cognitive functions was based on a weekly evaluation of child’s cognitive profile by a qualified neuropsychologist. In particular, during the first meeting scheduled before the intervention, the neuropsychologist presented to the therapists each child’s cognitive functioning based on baseline assessment data, describing strengths and weaknesses and identifying the cognitive ability(ies) to primarily train during the rehabilitation path. 30 min per session in each setting were devoted to such a training, while the remaining 15 min ensured the stimulation of the various cognitive subdomains addressed by the SET-ABI intervention. Therefore, also in the CORE-ABI intervention, the following subdomains were addressed: selective attention, sustained and divided attention, inhibition and shifting, visual-perceptual abilities, visual-spatial abilities, visual-constructional abilities, short-term memory, long-term memory, working-memory, categorization/reasoning/abstraction, problem-solving/planning and social cognition. A single cognitive subdomain was addressed each week, but the order of stimulation of the subdomains could be different from that established for the SET-ABI intervention and it was decided by the neuropsychologist. Each cognitive ___domain could be addressed for a minimum of 11.25 h and a maximum of 101.25 h.
During monitoring meetings scheduled at the end of each rehabilitation week, the neuropsychologists reviewed the exercises performed by the child in the intervention sessions in each setting (each therapist provided a folder reporting activities and performance scores of each child) and, based on performance, suggested activities to carry on in the subsequent week, identifying specific cognitive processes to address and related exercised to deliver to favor recovery. This monitoring also ensured treatment fidelity.
Data collection
Demographical, clinical and intellectual data
For all the patients enrolled in the study, the following demographic data were collected before randomization: age at the ABI, socio-economic status (SES) and age at admission to the rehabilitation center. Further, the following clinical data were collected, as they were considered to be prognostic of adjustment: etiology of the ABI (TBI vs. non-TBI, i.e.: cerebrovascular accidents, hypoxic events/anoxia, cerebral infections etc.), data on neurosurgery after the ABI, days of coma, GCS score, tracheotomy before study start, enteral nutrition before study start and pharmacotherapy before study start. After intervention conclusion, days of intervention for each patient (including drop-outs were collected).
Further, each child received an intellectual evaluation by the administration of the age-related Wechsler Scales: the Wechsler Preschool and Primary Scale of Intelligence (WPPSI-IV)84,85 was used for children aged 5:0–5:11 years; the Weschler Intelligence Scale for Children-Fourth Edition (WISC-IV)86,87 was adopted with children aged 6:0–16:11; the Wechsler Intelligence Scale for Adults-Fourth Edition (WAIS-IV)88 was used for children aged 17:0–17:11.
All data related to the study participants were collected at the Scientific Institute IRCCS E. Medea, Bosisio Parini, Lecco, Italy.
Cognitive outcome measures
This study intended to evaluate the effects of two multidomain rehabilitation interventions on the various core cognitive domains affected by a pediatric ABI immediately after the emergence of consciousness, which have been reported to be multiple and interconnected8,41. Hence, a comprehensive battery of well-known cognitive outcome measures was adopted. Assessments of outcomes were carried out at T0 and T1.
All cognitive measures used in this study involved tasks with setting and stimuli different from those used during the interventions, to evaluate whether benefits were not solely associated with practice-related effects (engagement), but occurred in the trained domains on different tasks (near-transfer effects). All tasks were administered at Scientific Institute IRCCS E. Medea, Bosisio Parini, Lecco, Italy.
Primary cognitive outcome
Visual sustained attention
The study primary cognitive outcome was visual sustained attention assessed by using the Conners Kiddie Continuous Performance Test–2nd Edition K-CPT-289, for children aged up to 7:11 years, and the Continuous Performance Test-3rd Edition -CPT-390, for children aged 8:0–17:11 years. During this computerized task, children had to press as fast as possible the spacebar in front of the presentation of alphabetical letters appearing on the screen, except when letter X appeared. Missed targets (omissions), incorrect responses to non-targets (commissions) and random or anticipatory responses (perseverations) were automatically counted by the program. The detectability score (KCPT-2/CPT-3 Detectability) was considered for our study, as it represents the ability to discriminate between targets and non-targets, constituting a global score of the sensitivity to targets during a long-time interval. Scores were expressed as T scores (Mean-M = 50, Standard Deviation-SD = 10). Higher scores indicated worse outcomes.
Secondary cognitive outcomes
Secondary cognitive outcomes included other cognitive processes related to the ___domain of attention and other cognitive domains.
Attention
Visual selective attention: the visual selective attention task (BVN Visual selective attention) from the Italian battery ‘Batteria di valutazione neuropsicologica per l’età evolutiva –BVN 5–11’ [‘Battery for neuropsychological evaluation for developmental age -BVN 5–11’]91 was used for children aged 5:0–11:11 years; the same task included in the Italian battery ‘Batteria di Valutazione Neuropsicologica per l’adolescenza –BVN 12–18’ [‘Battery for neuropsychological evaluation for adolescence –BVN 12–18’]92 was used for children aged 12:0–17:11 years. The task was a barrage test in which children were required to detect a target geometric shape (a square with two differently oriented lines) among a series of distracting shapes. The target was shown at the top of the sheet, followed by 2 practice lines and 17 test lines. Children had to search and mark the shapes identical to the target in 1 min. Scores were expressed as z-scores (M = 0; SD = 1). Higher scores indicated better outcomes.
Visual-spatial and visual-constructional abilities
-
Visual-spatial orientation: the Benton Judgment of Line Orientation Test93 was used to test this cognitive ability. The test targets subjects from 7:0 years onwards. In this task, children were required to match the angle and orientation of lines in space. Scores were expressed as z-scores (M = 0; SD = 1). Higher scores indicated better outcomes.
-
Visual information processing: the Italian version of the Test of Visual Perceptual Skills-3rd Edition -TVPS-394 was used. The test targets subjects from 4:0 years through 18:11. In this task, children were presented with black and white line drawings that they had to process using the following visual analysis processes: visual discrimination (namely, the ability to identify forms based on their characteristics), visual figure ground (namely, the ability to distinguish figures filtering out irrelevant information), visual memory (namely, the ability to recognize and recall visually presented information) and visual closure (namely, the ability to visually complete an image partially missing of some parts). The overall score (TVPS-3 Overall), consisting of the sum of scaled scores related to each visual process, was considered for this study. Scores were expressed as Standard scores (M = 100; SD = 15). Higher scores indicated better outcomes.
-
Visual-constructional abilities: the Rey-Osterrieth Complex Figure Test-copy task95 (ROCF Copy) was adopted. The test targets subjects from 4:0 years onwards. In this task children were asked to reproduce a complicated line drawing by coping it from a stimulus figure placed in front of them. In addition to visual-motor integration, this task also relied also on motor planning. Scores were expressed as z scores (M = 0; SD = 1). Higher scores indicated better outcomes.
Memory
-
Long-term visual-spatial memory: the Rey-Osterrieth Complex Figure Test95 recall task (ROCF Recall) was used. In this task children were required to reproduce a complicated line drawing 30 min after presentation. Scores were expressed as z scores (M = 0; SD = 1). Higher scores indicated better outcomes.
-
Visual-spatial working-memory: the Corsi block tapping task96 (BVN Corsi) included in the Italian ‘Batteria di valutazione neuropsicologica per l’età evolutiva –BVN 5–11’ [‘Battery for neuropsychological evaluation for developmental age -BVN 5–11’]91 was used for children aged 5:0–11:11; the same task included in the Italian ‘Batteria di Valutazione Neuropsicologica per l’adolescenza –BVN 12–18’ [‘Battery for neuropsychological evaluation for adolescence –BVN 12–18’]92 was used for children aged 12:0–17:11 years. In the task, children were asked to reproduce a visual-spatial sequence on spatial separated blocks glued on a tablet, in the same order as presented by the examiner. Different block-tapping series of increasing length were presented, with 3 trials per series. The memory span corresponded to the maximum length of the series in which at least 2 trials were correctly performed by children. Scores were expressed as z-scores (M = 0; SD = 1). Higher scores indicated better outcomes.
-
Short-term verbal memory and verbal working-memory: the digit span test included in the Italian ‘Batteria di valutazione neuropsicologica per l’età evolutiva -BVN 5–11’ [‘Battery for neuropsychological evaluation for developmental age -BVN 5–11’]91 was used for children aged 5:0–11:11 years, while the one included in the Italian ‘Batteria di Valutazione Neuropsicologica per l’adolescenza –BVN 12–18’ [‘Battery for neuropsychological evaluation for adolescence –BVN 12–18’]92 was used for children aged 12:0–17:11 years. Both forward (BVN Forward digit span) and backward (BVN Backward digit span) digit span were considered for this study. Patients were required to repeat a sequence of numbers presented by the examiner, in either the same order as presented (BVN Forward digit span) or in a reverse order (BVN Backward digit span). Scores were expressed as z-scores (M = 0; SD = 1). Higher scores indicated better outcomes.
-
Short-term verbal memory, verbal learning and long-term verbal memory: the immediate and delayed word list recall tasks included in the Italian ‘Batteria di valutazione neuropsicologica per l’età evolutiva –BVN 5–11’ [‘Battery for neuropsychological evaluation for developmental age -BVN 5–11’]91 was used for children aged 5:0–11:11 years, while the one included in the Italian ‘Batteria di Valutazione Neuropsicologica per l’adolescenza –BVN 12–18’ [‘Battery for neuropsychological evaluation for adolescence –BVN 12–18’]92 was used for children aged 12:0–17:11 years. A list including 12 words was orally presented by the examiner and children were required to repeat as many words as possible after the first presentation. Then, in the subsequent presentations the examiner repeated only the words not recalled by the child, until a maximum of 8 presentations. The delayed task was administered 30 min after the end of the immediate task. Scores were expressed as z-scores (M = 0; SD = 1). Higher scores indicated better outcomes.
Executive Functions
-
Cognitive flexibility: the computerized Modified Card Sorting Test97 (MCST) was used for children aged 5:0–7:11 and the computerized Wisconsin Card Sorting Test98 (WCST) was used for children aged 8:0–17:11. In this task, children were required to find a rule for associating cards and, subsequently, to modify it in a flexible way based on computerized feedback. The number of total errors (MCST/WCST Errors), which represented the sum of perseverative and non-perseverative errors, was considered for this study. Scores were expressed as Standard scores (M = 100; SD = 15). Higher scores indicated better outcomes.
-
Planning: the Tower of London99 (ToL) was used to assess planning and related problem-solving abilities. In this task children were required to reproduce an end-state picture showed by the examiner, by moving three color balls across three wooden pegs of different length mounted on a wood strip. For each problem, a minimum number of moves was given, with exceeding moves reflecting lower planning abilities. Total moves score (ToL Total moves) and total planning time score (ToL Total planning time) were considered for this study. Scores were expressed as Standard scores (M = 100; SD = 15). Higher scores indicated better outcomes. The administration sheet and normative data are available for children aged 7:0–15:11 years and adolescents and adults aged 16:0 years or older; thus children of this study aged less than 7:0 years were not administered this test.
-
Phonemic Fluency: the phonemic fluency task (BVN Phonemic fluency) included in the Italian ‘Batteria di valutazione neuropsicologica per l’età evolutiva 5–11’ [‘Battery for neuropsychological evaluation for developmental age -BVN 5–11’]91 was used for children aged 5:0–11:11 and the one included in the Italian ‘Batteria di Valutazione Neuropsicologica per l’adolescenza’ [‘Battery for neuropsychological evaluation for adolescence –BVN 12–18’]92 was used for children aged 12:0–17:11 years. In this task, children were required to generate as much words as possible in a minute beginning with a specific phoneme indicated by the examiner. 3 different phonemes (c, s and p) were used, for a total duration of 3 min for the whole task. Scores were expressed as z-scores. (M = 0; SD = 1). Higher scores indicated better outcomes.
Social cognition abilities
The ‘Theory of mind’ and ‘Affect recognition’ subscales from the Italian version of the battery -A Developmental NEuroPSYchological Assessment-II (NEPSY-II)100,101 were administered. The Theory of Mind subscale-part A assessed the understanding of mental functions and other people’s perspectives; the Theory of Mind subscale-part B tested the ability to match basic emotions to specific situations. The total score related to the Theory of Mind subscale (NEPSY-II ToM), consisting of the sum of the scores on Theory of Mind subscale-part A and –part B, was considered for this study. The Affect Recognition subscale (NEPSY-II AR) assessed the ability to recognize emotions on facial expressions. Scores were expressed as scaled scores (M = 10, SD = 3), ranging from 1 to 19. Higher scores indicated better outcomes. As NEPSY-II was developed and validated for children aged 3:0–16:11 years, scores of adolescents aged 17:0–17:11 years have been calculated by considering norms for adolescents aged 15:0–16:11 years.
Statistical analyses
Differences between G1 (CORE-ABI) and G2 (SET-ABI) on demographic, clinical and intellectual variables at baseline (T0) were checked by using the t-test (two-tailed) for continuous variables and the chi-square test or Fisher’s exact test for binary variables. Correlations were calculated by using Pearson’s method.
To evaluate intervention efficacy, intention-to-treat analysis was used. Indeed, all children who were randomized into the two study groups were included in the analysis according to their randomized allocation, irrespective of adherence to treatment in the CORE-ABI or the SET-ABI arm. A total of 39 children were considered, as one child of the 40 randomized was excluded immediately after the start of the intervention because of aphasia. No imputation of missing baseline (T0) or post-intervention (T1) data was performed. Linear mixed models (LMMs) were used to determine the effects of ‘group’ (G1: CORE ABI vs. G2: SET-ABI), ‘time’ (T0 vs. T1) and ‘group x time’ interaction on each cognitive outcome measure, with patients included as a random factor. Variables significantly differing between groups at baseline were included as covariates in distinct LMMs to control for possible confounding effects.
Finally, as suggested by a reviewer, individual-level analyses were performed to capture clinically meaningful changes from treatment at the individual level, alongside group-level statistical significance. With this aim, the number and percentage of children who exhibited no/<1 SD improvement or improvement ≥ 1 SD after treatment were calculated and compared by using chi-square test or Fisher’s exact test. Results of these analyses are reported in Supplementary Table S1.
No interim analyses were performed
Data analyses were performed using R software, version 4.3.2, (R Foundation for Statistical Computing, Vienna, Austria)102 and SPSS, version 29.0.2103. Level of significance was set at p < 0.05.
Results
Among the 77 patients in a subacute phase being inpatients at the Scientific Institute IRCCS E. Medea, Bosisio Parini, Lecco during the research timeframe, 37 were excluded for the following reasons: 16 due to severe motor impairment or sensory deficits, causing the need for a device; 5 due to presence of aphasia; 8 due to presence of a previous diagnosis of learning or attention disorder; and 8 declined to participate into the study (due to excessive intervention duration). Thus, 40 patients were included in the study and randomized into the 2 study groups. However, shortly after the beginning of the treatment (specifically, at session 2), a patient in G2 was excluded due to presence of aphasia not diagnosed before. 39 children were then included in the study, 20 allocated in G1 (CORE-ABI) and 19 allocated in G2 (SET-ABI). In the whole sample, 25 children were boys and 14 girls. Mean age of children at the ABI was 12.04 years (SD = 3.11) and mean age at admission to the rehabilitation center was 12.12 years (SD = 3.12). ABI etiology was mixed, with 18 TBI, 19 cerebrovascular accidents, 1 cerebral infection and 1 anoxic event. Furthermore, participation was revoked during the training by 2 children in G1 (at training day 26 and 28, respectively) and 3 children in G2 (at training day 19, 26 and 36, respectively). Therefore, 34 children completed the training and were assessed at T1, 18 assigned to G1 and 16 assigned to G2. Dropout rate was 10% in G1 and 15.8% in G2 (average dropout rate = 12.8%).
Figure 1 depicts the study flowchart.
No significant differences between groups were found for the following demographic and clinical variables at baseline (T0): gender (χ2 (1) = 0.01, p = 0.91); age (years) at the ABI (t(37) = 0.31, p = 0.76); SES (t(37) = 0.87; p = 0.39); age (years) at admission to the rehabilitation center (t(37) = 0.29, p = 0.78); age (years) at baseline evaluation (t(37) = 0.30, p = 0.77); time (months) between the ABI and baseline evaluation (t(37)=-0.50, p = 0.62); etiology of the ABI (χ2(3) = 2.92, p = 0.40); neurosurgery after the ABI (χ2(1) = 0.21, p = 0.65); GCS score (χ2(37) = -0.36, p = 0.72); days of coma (t(37)=-0.21, p = 0.83); tracheotomy before study start (χ2(1) = 0.01, p = 0.95); enteral nutrition before study start (χ2(1) = 3.40, p = 0.07); and pharmacotherapy before study start (χ2(1) = 0.05, p = 0.82). Finally, no differences in intellectual functioning were found (t(37) = 1.53, p = 0.14).
No between-group differences were found for days of treatment (t(37) = 0.25, p = 0.81). This calculation was performed on the whole sample, including drop-outs. All children who concluded the allocated intervention received complete therapy dose, consisting of 60 total sessions.
Table 1 reports the demographic, clinical and intellectual data at baseline (T0) for the whole sample and the two groups, separately.
With respect to cognitive functioning, some missing data were found among the 17 outcome measures, both at T0 and T1. Missing data could be due to age (i.e., children aged less than the age range covered by cognitive measures) or clinical reason (e.g., children refused to receive the evaluation for at least 2 times per assessment or the assessment was too difficult for the child causing excessive frustration). Specifically, at T0 missing data of one patient, all due to clinical reason, was found for: BVN Visual selective attention, BVN Immediate word list recall, BVN Delayed word list recall, TVPS-3 Overall, NEPSY-II ToM and NEPSY-II AR. Missing data of 2 patients were found for: Benton Judgment of line orientation (missing data for one child was due to age), ROCF Copy, ROCF Recall and WCST Errors. Missing data of 6 children were found for: ToL Total moves (missing data for 2 children were due to age) and ToL Total planning time (missing data for 2 children were due to age). At T1, excluding drop-outs,1 missing data was found for BVN Backward digit span, Benton Judgment of line orientation (missing data was due to age) and ToL Total moves (missing data was due to age).
At baseline (T0) no differences on outcomes measures were found between the 2 groups on the primary cognitive outcome and on 13 of 16 outcomes; in contrast, TVPS-3 Overall, NEPSY-II ToM and NEPSY-II AR differed between the 2 groups, with G1 that showed higher scores than G2. Cognitive data at baseline (T0) and post-intervention (T1) for both the CORE-ABI (G1) and the SET-ABI (G2) group, including p values on the differences at T0, are reported in Table 2.
Treatment effects on cognitive outcomes
5 children out of the total 39 discontinued the intervention, 2 in G1 and 3 in G2, thus post-intervention data (T1) on 34 children were included in LMMs, 18 in G1 and 16 in G2. Baseline data (T0) were, instead, included for all the 39 children.
For the primary cognitive outcome (CPT/KPT Detectability: visual sustained attention) and all secondary cognitive outcomes no interaction effect was found (all p ≥ 0.06). Therefore, LMMs were repeated including only ‘time’ and ‘group’ effects. LMMs were calculated inserting variables significantly differing between groups at baseline as covariates (i.e., TVPS-3 Overall, NEPSY-II ToM and NEPSY-II AR). LMMs yielded time effect for the primary cognitive outcome and 14 out of 16 secondary outcomes, except for BVN Forward digit span and ToL Total planning time. No group effect was found on any cognitive outcome measures. Results for each group and the estimated effect size are reported in Table 3.
Correlations between age at baseline evaluation and change in cognitive outcomes
Correlations between age at baseline evaluation (T0) and the pre-post intervention difference (delta T1-T0) on cognitive outcome measures yielded no significance for the following variables: KCPT-2/CPT-3 Detectability, BVN Visual selective attention, BVN Forward digit span, BVN Backward digit span, BVN Phonemic fluency, Benton Judgment of line orientation, ROCF Copy, ROCF Memory, WCST, ToL Total moves, ToL Total planning time, TVPS-3 Overall, NEPSY-II ToM and NEPSY-II AR (all r ≤ 0.32, all p ≥ 0.67). Instead, significant correlations were found for: BVN Immediate word list recall (r = 0.40, p = 0.02), BVN Delayed word list recall (r = 0.41, p < 0.02) and BVN Corsi (r = 0.47, p < 0.01), with older children having better performance.
Discussion
This RCT aimed at assessing and comparing the efficacy of two 12-week inpatient cognitive rehabilitation interventions for children with ABI aged 5–17 years, immediately after the emergence of consciousness. Two different intervention formats, both addressing multiple cognitive abilities, have been adopted, namely a personalized intervention (CORE-ABI), stimulating the most deficient cognitive function(s) with a concomitant stimulation of all the other functions, and a sequential intervention (SET-ABI), addressing each cognitive function following a sequential order. This study was conducted in view of the need indicated by previous literature for post-acute neurorehabilitation in this population20,104 and the very limited evidence on the topic for the subacute phase following an ABI53,105. An important aspect of this work is the inclusion of children in a specific and temporally limited phase of recovery after ABI (subacute phase: <3 months since ABI), whose age at onset, age at study entry and evaluation, and time since onset to evaluation were reported. This, together with the use of standardized neurocognitive tools for outcome assessment, allowed us to clearly describe characteristics and functioning of children, which until now have rarely been reported in the literature on rehabilitation and functional outcomes of pediatric ABI36,106.
A wide range of cognitive abilities (attention, memory, visual-spatial/visual-constructional abilities and executive functions) were trained through both interventions and outcomes in all these cognitive domains were evaluated. Results showed significant differences at post-intervention in all domains, with no differences between interventions, supporting the importance of early cognitive rehabilitation to sustain recovery in pediatric patients with ABI8,20,104– 105. Both the primary cognitive outcome, namely visual sustained attention (importantly, tested by using a computerized tool, thus excluding possible subjective influences of assessors) and all secondary outcomes, except for short-term verbal memory (BVN Forward digit span) and time used in tasks requiring planning (ToL Total planning time), showed an improvement after the intervention, irrespective of its format (i.e., the personalized CORE-ABI and the sequential SET-ABI). The primary cognitive outcome showed a change after treatment with a large effect, consistent with the continuous stimulation provided on attention skills, either directly through ad hoc exercises or indirectly through the continuous attentional focus that children had to maintain on challenging tasks for a long time. In relation to secondary outcomes, 13 out of the total 16 showed a change with a medium-to-large effect and one with a very large effect (BVN Immediate word list recall), supporting intervention efficacy. Instead, the absence of a change on short-term verbal memory with numerical information (BVN Forward digit span), in contrast with the large improvement showed by children on verbal recall with word stimuli (BVN Immediate word list recall and BVN Delayed word list recall showed a change with a very large and large effect size, respectively), could highlight that verbal memory could benefit from semantic grouping strategies to improve. This appears to be in accordance with the work done by therapists in treatment, characterized by implementation of metacognitive strategies. Otherwise, a ceiling effect for immediate verbal memory (BVN Forward digit span) could have occurred, as both groups scored in the low range of the average at baseline. No change in planning time (ToL Total planning time) could be due to the fact that children were trained by therapists to stop and think before doing an action, thus they could spend more time in action planning with a beneficial effect on planning accuracy (ToL Total moves).
The two study groups did not differ in any demographic, clinical and cognitive measures at baseline except for visual-perceptual and social cognition abilities on which children allocated to the personalized CORE-ABI intervention scored better. This may have limited the detection of the effects of the CORE-ABI intervention compared with the SET-ABI intervention, as children included in the latter group had lower cognitive abilities and, therefore, were more likely to have higher score differences between pre- and post-treatment. Related to visual-perceptual abilities (TVPS-3 Overall), while the CORE-ABI intervention group had a score falling in the average range, thus being at risk for the ceiling effect, the SET-ABI intervention group scored in the low average, potentially benefitting more from treatment. However, when statistically controlling for this issue using baseline scores on visual-perceptual abilities as a covariate in LMM analyses, no significant changes in main effect of time or interaction time x group were found, leading to exclude this possibility. On the contrary, the group effect lost statistical significance, confirming the existence of significant differences only at baseline. With respect to social cognition (NEPSY-II AR and NEPSY-II ToM), both groups showed an impairment at baseline, but the CORE-ABI group scored below the average while the SET-ABI group showed a more severe impairment. Nevertheless, also in this case, the inclusion of affect recognition and theory of mind scores at baseline as covariates in distinct LMMs did not lead to identify any significant changes in main effect of time or interaction. The group effect lost its significance, confirming the presence of differences only at baseline. This allowed attesting the comparable effects of the two interventions on social cognition at a group level, although individual-level analyses indicated a higher percentage of changes ≥ 1 SD related to NEPSY-II AR in the SET-ABI group, probably due to a greater possibility of improvement of some children due to lower baseline skills. No other between-group effects were detected by individual-level analyses, supporting the results of group-level analyses. In sum, findings seem to indicate that cognitive interventions, albeit different formats, may sustain cognitive recovery early after a pediatric ABI and, thus, should be ensured to patients to favor the best functional outcomes. Nevertheless, no passive control group was included in the study, due to ethical reasons associated with ensuring the earliest care as possible to patients, thus this RCT cannot provide clear data on the effects of cognitive rehabilitation irrespective of spontaneous recovery.
Previous literature suggested the importance of a personalized rehabilitation approach to favor recovery and generalization of the effects of cognitive interventions to everyday activities in pediatric patients with ABI in the chronic phase37,64,74,75,76,77. The usefulness of highly individualized recommendations and strategies for children with ABI across the various stages of recovery has also been highlighted by a collaborative of pediatric psychologists with expertise in neuropsychology8. Tailored interventions based on child’s age, developmental functioning, etiology and neurobehavioral impairments (e.g., sensory impairments, hemiparesis, aphasia etc.) have been indicated as the optimal option to provide neuropsychological treatment to children with ABI8,75, thus leading to opposite conclusions compared to this RCT. This discrepancy could be attributed to the fact that this RCT is the first one available in the literature evaluating inpatient rehabilitation interventions at a very early stage of recovery, which might suggest that a personalized approach may be beneficial at a later stage of recovery, when the impact of rehabilitation on daily activities becomes stronger. In fact, the stage in which interventions of this study have been delivered, which is not coincidentally called ‘stage of acute cognitive impairment’8, is characterized by children that usually present with deficits in a wide range of cognitive abilities and exhibit slow learning41, with some deficits that may resolve over time and others, generally the primary areas of impairments, that may persist in the long-term8,41. These persisting deficits, that become the focus of subsequent interventions and rehabilitation post discharge8,41,107,108, could require a more personalized approach to be addressed, as they intersect with demands and expectations in home, school, community and work settings. Differently, at an early stage of recovery everyday environmental needs are limited and a standardized cognitive rehabilitation protocol could be used for a variety of patients, with no beneficial effects of a personalized approach based on continuous clinical monitoring of patients’ cognitive strengths and weaknesses.
Significant cognitive deficits affecting multiple cognitive domains early after an ABI may have contributed to the absence of differences between the CORE-ABI and the SET-ABI intervention because, although with different formats, both treatments addressed the various cognitive functions over a long period of time with continuous clinical support. This may have been beneficial for all patients, regardless of the severity of their impairment and the exact amount of rehabilitation provided on each cognitive function by the two interventions. Given that RCTs available in the extant literature on cognitive rehabilitation for pediatric ABI included interventions with shorter overall treatment duration and fewer weekly sessions than those in this study38, it could be hypothesized that treatment intensity played a crucial role in leading to the significant changes reported here. In addition, the active role of therapists in the rehabilitation sessions might have further boosted cognitive improvement, as they taught instructions, metacognitive strategies, and rules at an early stage of recovery from ABI, when patients might need one-to-one support to perform activities. Close monitoring of strategies used by children with ABI when coping with complex tasks and swift adjustments enabled by clinicians have been suggested as factors that may increase feelings of control and self-efficacy in children and therapists during rehabilitation109, which might in turn have contributed to the efficacy of both interventions of this study.
In addition, the outcome measures included in this study assessed discrete cognitive tasks, considering improvement in cognitive functioning without assessing the skills needed for daily living, social interaction or community participation. Indeed, the administration of measures assessing quality of life and everyday functioning, which usually refer to adaptive behavior in the ecological setting, was not reasonable for inpatients in the subacute stage after ABI. However, the adoption of a battery focused on cognitive functioning only might not be meaningful for detecting the functional changes necessary for community participation, which instead gain more importance in the chronic stages of recovery/rehabilitation. In our study this may have masked any differences between the two interventions in fostering improvements in overall functioning. Further, previous research indicated that performance-based measures and informant rating scales of neuropsychological functioning evaluate different constructs110,111,112,113. Therefore, the results of this RCT should be considered generalizable to patients who sustained an ABI no more than 3 months before receiving cognitive rehabilitation and to changes on the level of functions, not of adaptive behavior.
Up to now, many patients do not receive adequate intervention after an ABI for different reasons, such as geographical barriers to reaching specialized rehabilitation centers, poor understanding of the consequences of an ABI by non-specialists and families, patchy and inadequate resources or insurance status114,115,116. However, the possibility to administer an identical intervention protocol to children with different cognitive functioning could allow reducing the costs related to involvement of qualified personnel in intervention design and delivery, which could represent an incentive to the creation of rehabilitative services affiliated to hospitals managing injuries or having a local service configuration. The unmet cognitive rehabilitation needs of children with ABI represents an important health issue since more than two decades28,115,116,117, which should be urgently addressed.
In this respect, the SET-ABI protocol described in this study could inform about a feasible and potentially effective cognitive rehabilitation practice to be adopted with children with moderate-to-severe ABI in the early recovery phase. The long duration (12 weeks) of the intervention and its intensity (3 sessions/day per 5 days) could represent a barrier to its implementation, but engagement in early intensive rehabilitation could prevent negative cascade effects of an ABI on cognitive and social functioning; however, the potential of rehabilitation still seems to be too overlooked114. In our clinical experience we encountered an initial acceptance barrier from therapists, as they strongly believed in the superiority of a personalized approach; in particular, they were reluctant about the possibility to adopt the same protocol to patients with various cognitive functioning and to address an only cognitive ___domain for an entire week. However, this RCT demonstrates the viability of such a practice, which might gain the dose intensity required to trigger neuroplasticity118 and could help enhancing the quality of care provided to children with ABI with an advantageous cost-benefit ratio. This study included children of a wide age range, demonstrating benefits for those aged as early as the last year of nursery school through adolescence; however, for the memory ___domain (specifically for the following measures: BVN Immediate word list recall, BVN Delayed word list recall and BVN Corsi task) older children were found to obtain higher gains. This could have occurred because they had a better understanding of their ability and task difficulty than younger children, being abler to adapt metacognitive strategies to task demands.
Even though the SET-ABI intervention protocol does not needlessly require children hospitalization to be delivered but could be adopted also by local services, we cannot exclude that the important cognitive gains exhibited by children at post-treatment could have been boosted by the rehabilitation potential of the 24-hour program of care provided by the whole team in the clinical context119. Future research should evaluate the effects of rehabilitation, also including ingredients generally considered peripheral, such as the whole nursing and care staff, whose actions also cover weekends and the evenings119.
Limitations of this study should be acknowledged. First, as clearly discussed above, the absence of a passive control group, which could allow controlling for time effects and spontaneous recovery of children, could have caused an overestimation of training effects. This choice was however motivated by the fact that it was not considered to be ethical not ensuring early rehabilitation interventions to patients at the emergence of consciousness. Second, no follow-up data have been collected to evaluate whether an intervention format could have more long-term benefits than the other. This aspect could be of particular interest for future research, as previous literature suggested more benefits of a personalized approach for the chronic phase of an ABI; therefore, it might be interesting to consider whether some benefits observed in the chronic phase could also be achieved through personalized rehabilitation at an earlier stage of recovery, by scheduling one or more follow-up assessments. Third, the relatively small sample size, even though calculated through power analysis, warrants further exploration in larger samples. Additionally, the exclusion of children with severe sensory and motor deficits limits the generalizability of study findings to a selected group of children with moderate-to-severe ABI, namely those with lower disability level and potential better prognosis. Generalizability of findings is also affected by the non-inclusion of children with mild ABI, which was however established to reduce potential sources of variation affecting results. Fourth, a wide age range was included, which could have masked a potential age effect. Even though we tried to explore this aspect by correlation analyses between children’s age and pre-post treatment change in cognitive performance, future studies should clearly control for it, benefiting from narrower age ranges, as already suggested by previous literature33. Fifth, even though treatment fidelity was supported by scheduled meetings between the rehabilitation therapists and the neuropsychologists, differences in modality of activity delivering could have occurred, possibly influencing outcomes. Nevertheless, exercises and activities delivered were previously selected by the research team, neuropsychologists and therapists and classified according to the specific cognitive function to train, patients’ characteristics and rehabilitation settings, which could have mitigated such a risk. Finally, this study was partly conducted during COVID-19 pandemic (2020–2021), which could have negatively impacted on types of ABI included (in particular, a lower number of cases of TBI due to vehicle accidents was registered) and willingness of families to stay in a hospital for a long time, possibly influencing dropout rate. In addition, this fact could have caused limitations in the use of non-verbal communication due to the use of face masks, with potential reduction of benefits of child-therapist interaction.
Conclusions
Findings of this RCT suggest the potential benefits of early rehabilitation interventions on cognitive functions after a pediatric ABI. However, no definite conclusions on the effects of the interventions irrespective of spontaneous change can be drawn, as no passive control group to test time effects and spontaneous recovery was included in the study. Data highlights that a personalized approach is not strictly necessary to obtain better cognitive gains in the early recovery phase after an ABI, in contrast with evidence for the chronic phase for which extant literature recommends personalized treatments to ensure generalization and better adjustment37,6474–77. This could be due to the wide range of cognitive deficits exhibited by children at an early stage, which could have led to find no differences between two rehabilitation interventions simultaneously addressing different cognitive functions for a long time. It could be that individualized and tailored interventions are more beneficial at a subsequent stage, in which everyday environmental needs become stronger. The SET-ABI (standardized approach) and CORE-ABI (personalized approach) protocols described in this study may be considered viable and potentially effective rehabilitation tools for children with moderate-to-severe ABI in the subacute phase.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Rivara, F. P. et al. Incidence of disability among children 12 months after traumatic brain injury. Am. J. Public. Health. 102 (11), 2074–2079. https://doi.org/10.2105/AJPH.2012.300696 (2012).
Guice, K. S., Cassidy, L. D. & Oldham, K. T. Traumatic injury and children: a National assessment. J. Trauma. 63 (6), S68–S86. https://doi.org/10.1097/TA.0b013e31815acbb6 (2007).
Theodorou, C. M., Nuño, M., Yamashiro, K. J. & Brown, E. G. Increased mortality in very young children with traumatic brain injury due to abuse: A nationwide analysis of 10,965 patients. J. Pediatr. Surg. 56(6), 1174–1179 (2021). (2021). https://doi.org/10.1016/j.jpedsurg.2021.02.044
McKinlay, A. et al. Service provision for children and young people with acquired brain injury: practice recommendations. Brain Inj. 30 (13–14), 1656–1664. https://doi.org/10.1080/02699052.2016.1201592 (2016).
Dewan, M. C., Mummareddy, N., Wellons, J. C. 3, Bonfield, C. M. & rd., Epidemiology of global pediatric traumatic brain injury: qualitative review. World Neurosurg. 91 (e1), 497–509. https://doi.org/10.1016/j.wneu.2016.03.045 (2016).
Slomine, B. & Locascio, G. Cognitive rehabilitation for children with acquired brain injury. Dev. Disabil. Res. Rev. 15 (2), 133–143. https://doi.org/10.1002/ddrr.56 (2009).
Giacino, J. T., Fins, J. J., Laureys, S. & Schiff, N. D. Disorders of consciousness after acquired brain injury: the state of the science. Nat. Rev. Neurol. 10 (2), 99–114. https://doi.org/10.1038/nrneurol.2013.279 (2014).
Watson, W. D. et al. The role of the neuropsychologist across the stages of recovery from acquired brain injury: a summary from the pediatric rehabilitation neuropsychology collaborative. Child. Neuropsychol. 29 (2), 299–320. https://doi.org/10.1080/09297049.2022.2086691 (2023).
Corti, C., Butti, N., Bardoni, A., Strazzer, S. & Urgesi, C. Body processing in children and adolescents with traumatic brain injury: an exploratory study. Brain Sci. 12 (8), 962. https://doi.org/10.3390/brainsci12080962 (2022).
Bellesi, G., Barker, E. D., Brown, L. & Valmaggia, L. Pediatric traumatic brain injury and antisocial behavior: are they linked? A systematic review. Brain Inj. 33 (10), 1272–1292. https://doi.org/10.1080/02699052.2019.1641621 (2019).
Chavez-Arana, C. et al. Parenting and the dysregulation profile predict executive functioning in children with acquired brain injury. Child. Neuropsychol. 25 (8), 1125–1143. https://doi.org/10.1080/09297049.2019.1589442 (2019).
Holthe, I. L. et al. Neuropsychological Impairment, Brain Injury Symptoms, and Health-Related Quality of Life After Pediatric TBI in Oslo. Front Neurol. 12, 719915; (2022). https://doi.org/10.3389/fneur.2021.719915 (2022).
Li, L. & Liu, J. The effect of pediatric traumatic brain injury on behavioral outcomes: a systematic review. Dev. Med. Child. Neurol. 55 (1), 37–45. https://doi.org/10.1111/j.1469-8749.2012.04414.x (2013).
Ryan, N. P. et al. Unraveling the association between pediatric traumatic brain injury and social dysfunction: the mediating role of Self-Regulation. J. Neurotrauma. 36 (20), 2895–2903. https://doi.org/10.1089/neu.2018.6308 (2019).
Anderson, V. A. et al. Predicting neurocognitive and behavioural outcome after early brain insult. Dev. Med. Child. Neurol. 56 (4), 329–336. https://doi.org/10.1111/dmcn.12387 (2014).
Strazzer, S. et al. Long-Term vocational outcome at 15 years from severe traumatic and Non-Traumatic brain injury in pediatric age. Brain Sci. 13 (7), 1000. https://doi.org/10.3390/brainsci13071000 (2023).
McKinlay, A., Corrigan, J., Horwood, L. J. & Fergusson, D. M. Substance abuse and criminal activities following traumatic brain injury in childhood, adolescence, and early adulthood. J Head Trauma Rehabil. 29 (6), 498–506. https://doi.org/10.1097/HTR.0000000000000001 (2014).
Keenan, H. T., Clark, A. E., Holubkov, R., Cox, C. S. & Ewing-Cobbs, L. Psychosocial and executive function recovery trajectories one year after pediatric traumatic brain injury: the influence of age and injury severity. J. Neurotraum. 35 (2), 286–296. https://doi.org/10.1089/neu.2017 (2018).
King, D. J. et al. Developmental divergence of structural brain networks as an indicator of future cognitive impairments in childhood brain injury: executive functions. Dev. Cogn. Neuros-Neth. 42, 100762. https://doi.org/10.1016/j.dcn.2020.100762 (2020).
Limond, J., Dorris, L. & McMillan, T. M. Quality of life in children with acquired brain injury: parent perspectives 1–5 years after injury. Brain Inj. 23 (7–8), 617–622. https://doi.org/10.1080/02699050902997870 (2009).
Forsyth, R. & Basu, A. The promotion of recovery through rehabilitation after acquired brain injury in children. Dev. Med. Child. Neurol. 57 (1), 16–22. https://doi.org/10.1111/dmcn.12575 (2015).
Gracey, F. et al. Age of injury, emotional problems and executive functioning in Understanding disrupted social relationships following childhood ABI. Soc. Care Neurodisabil. 5 (3), 160–170. https://doi.org/10.1108/SCN-08-2013-0030 (2014).
Karver, C. L. et al. Age at injury and long-term behavior problems after traumatic brain injury in young children. Rehabil Psychol. 57 (3), 256–265. https://doi.org/10.1037/a0029522 (2012).
Pastore, V. et al. Psychological and adjustment problems due to acquired brain lesions in pre-school-aged patients. Brain Inj. 27 (6), 677–684. https://doi.org/10.3109/02699052.2013.775482 (2013).
Pozzi, M. et al. Severe acquired brain injury aetiologies, early clinical factors, and rehabilitation outcomes: a retrospective study on pediatric patients in rehabilitation. Brain Inj. 33 (12), 1522–1528. https://doi.org/10.1080/02699052.2019.1658128 (2019).
Keenan, H. T., Clark, A. E., Holubkov, R. & Cox, C. S. & Ewing-Cobbs, L. Trajectories of Children’s Executive Function After Traumatic Brain Injury. JAMA Netw. Open 4(3), e.212624 (2021). https://doi.org/10.1001/jamanetworkopen.2021.2624
Van Zellem, L. et al. Long-term neuropsychological outcomes in children and adolescents after cardiac arrest. Intens Care Med. 41, 1057–1066. https://doi.org/10.1007/s00134-015-3789-y (2015).
Slomine, B. S. et al. Health care utilization and needs after pediatric traumatic brain injury. Pediatrics 117 (4), e663–e674. https://doi.org/10.1542/peds.2005-1892 (2006).
Bayley, M. T. et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury: methods, overview, and principles. J. Head Trauma. Rehab. 38 (1), 7–23. https://doi.org/10.1097/HTR.0000000000000838 (2023).
Cicerone, K. D. et al. Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Arch. Phys. Med. Rehab. 92 (4), 519–530. https://doi.org/10.1016/j.apmr.2010.11.015 (2011).
Giacino, J. T. et al. Minimum competency recommendations for programs that provide rehabilitation services for persons with disorders of consciousness: a position statement of the American Congress of rehabilitation medicine and the National Institute on disability, independent living and rehabilitation research traumatic brain injury model systems. Arch. Phys. Med. Rehab. 101 (6), 1072–1089. https://doi.org/10.1016/j.apmr.2020.01.013 (2020).
Oberholzer, M. & Müri, R. M. Neurorehabilitation of traumatic brain injury (TBI): A clinical review. Med. Sci. 7 (3), 47. https://doi.org/10.3390/medsci7030047 (2019).
Togher, L. et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, part iv: cognitive-communication and social cognition disorders. J. Head Trauma. Rehab. 38 (1), 65–82. https://doi.org/10.1097/HTR.0000000000000835 (2023).
Camm, S., Porter, M., Brooks, A., Boulton, K. & Veloso, G. C. Cognitive interventions for children with acquired brain injury: a systematic review. Neuropsychol. Rehabil. 31 (4), 621–666. https://doi.org/10.1080/09602011.2020.1722714 (2021).
Irzan, H. et al. Emerging treatments for disorders of consciousness in paediatric age. Brain Sci. 12 (2), 198. https://doi.org/10.3390/brainsci12020198 (2022).
Slomine, B. & Molteni, E. Pediatric disorders of consciousness: considerations, controversies, and caveats. Neurorehabilitation 54 (1), 129–139. https://doi.org/10.3233/NRE-230131 (2024).
Laatsch, L. et al. Evidence-based systematic review of cognitive rehabilitation, emotional, and family treatment studies for children with acquired brain injury literature: from 2006 to 2017. Neuropsychol. Rehabil. 30 (1), 130–161. https://doi.org/10.1080/09602011.2019.1678490 (2020).
Resch, C., Rosema, S., Hurks, P., de Kloet, A. & van Heugten, C. Searching for effective components of cognitive rehabilitation for children and adolescents with acquired brain injury: A systematic review. Brain Inj. 32 (6), 679–692. https://doi.org/10.1080/02699052.2018.1458335 (2018).
Tooley, U. A. et al. The age of reason: functional brain network development during childhood. J. Neurosci. 42 (44), 8237–8251. https://doi.org/10.1523/JNEUROSCI.0511-22.2022 (2022).
Marek, S. et al. Identifying reproducible individual differences in childhood functional brain networks: an ABCD study. Dev. Cogn. Neurosci. 40, 100706. https://doi.org/10.1016/j.dcn.2019.100706 (2019).
Babikian, T. & Asarnow, R. Neurocognitive outcomes and recovery after pediatric TBI: meta-analytic review of the literature. Neuropsychology 23 (3), 283–296. https://doi.org/10.1037/a0015268 (2009).
Strazzer, S. et al. Altered recruitment of the attention network is associated with disability and cognitive impairment in pediatric patients with acquired brain injury. Neural Plast. 104282 https://doi.org/10.1155/2015/104282 (2015).
Bangirana, P. et al. Immediate neuropsychological and behavioral benefits of computerized cognitive rehabilitation in Ugandan pediatric cerebral malaria survivors. J. Dev. Behav. Pediatr. 30 (4), 310–318. https://doi.org/10.1097/DBP.0b013e3181b0f01b (2009).
Bangirana, P. et al. Cognition, behaviour and academic skills after cognitive rehabilitation in Ugandan children surviving severe malaria: a randomised trial. BMC Neurol. 11 https://doi.org/10.1186/1471-2377-11-96 (2011).
Sohlberg, M. M., Harn, B., MacPherson, H. & Wade, S. L. A pilot study evaluating attention and strategy training following pediatric traumatic brain injury. Clin. Prac Ped Psychol. 2 (3), 263–280. https://doi.org/10.1037/cpp0000072 (2014).
Vander Linden, C. et al. Cognitive training benefit depends on brain injury ___location in adolescents with traumatic brain injury: a pilot study. Eur. J. Phys. Rehab Med. 55 (5), 585–594. https://doi.org/10.23736/S1973-9087.18.05548-X (2019).
Verhelst, H., Vander Linden, C., Vingerhoets, G. & Caeyenberghs, K. How to train an injured brain? A pilot feasibility study of home-based computerized cognitive training. Games Health J. 6 (1), 28–38. https://doi.org/10.1089/g4h.2016.0043 (2017).
Corti, C. et al. Remote Technology-Based training programs for children with acquired brain injury: A systematic review and a Meta-Analytic exploration. Behav. Neurol. 1346987 https://doi.org/10.1155/2019/1346987 (2019).
Corti, C. et al. Home-based cognitive training in pediatric patients with acquired brain injury: preliminary results on efficacy of a randomized clinical trial. Sci. Rep. 10 (1), 1391. https://doi.org/10.1038/s41598-020-57952-5 (2020).
Robinson, K. E., Kaizar, E., Catroppa, C., Godfrey, C. & Yeates, K. O. Systematic review and meta-analysis of cognitive interventions for children with central nervous system disorders and neurodevelopmental disorders. J. Pediatr. Psychol. 39 (8), 846–865. https://doi.org/10.1093/jpepsy/jsu031 (2014).
Oldrati, V. et al. Effectiveness of computerized cognitive training programs (CCTP) with Game-like features in children with or without neuropsychological disorders: a Meta-Analytic investigation. Neuropsychol. Rev. 30 (1), 126–141. https://doi.org/10.1007/s11065-020-09429-5 (2020).
Corti, C. et al. Randomized clinical trial on the effects of a computerized cognitive training for pediatric patients with acquired brain injury or congenital malformation. Sci. Rep. 13 (1), 14559. https://doi.org/10.1038/s41598-023-41810-1 (2023).
Chavez-Arana, C., van IJzendoorn, M. H., Serrano-Juarez, C. A., de Pauw, S. S. W. & Prinzie, P. Interventions to improve executive functions in children and adolescents with acquired brain injury: a systematic review and multilevel meta-analysis. Child. Neuropsychol. 30 (1), 164–187. https://doi.org/10.1080/09297049.2023.2172150 (2024).
Maggio, M. G. et al. Social cognition in patients with acquired brain lesions: an overview on an under-reported problem. Appl. Neuropsychol. Adult. 29 (3), 419–431. https://doi.org/10.1080/23279095.2020.1753058 (2022).
McDonald, S. Impairments in social cognition following severe traumatic brain injury. J. Int. Neuropsychol. Soc. 19 (3), 231–246. https://doi.org/10.1017/S1355617712001506 (2013).
McDonald, S., Fisher, A., Flanagan, S. & Honan, C. A. Impaired perception of sincerity after severe traumatic brain injury. J. Neuropsychol. 11 (2), 291–304. https://doi.org/10.1111/jnp.12086 (2017).
McDonald, S. & Genova, H. The effect of severe traumatic brain injury on social cognition, emotion regulation, and mood. Handb. Clin. Neurol. 183, 235–260. https://doi.org/10.1016/B978-0-12-822290-4.00011-6 (2021).
Corti, C. et al. Visual perception and Spatial transformation of the body in children and adolescents with brain tumor. Neuropsychologia 120, 124–136. https://doi.org/10.1016/j.neuropsychologia.2018.10.012 (2018).
Kelly, M., McDonald, S. & Frith, M. H. J. A survey of clinicians working in brain injury rehabilitation: are social cognition impairments on the radar? J. Head Trauma. Rehabil. 32, E55–E65. https://doi.org/10.1097/HTR.0000000000000269 (2017).
Togher, L. et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, part IV: Cognitive-communication and social cognition disorders. J. Head Trauma. Rehabil. 38, 65–82. https://doi.org/10.1097/HTR.0000000000000835 (2023).
Sirois, K. et al. The contribution of social cognition in predicting social participation following moderate and severe TBI in youth. Neuropsychol. Rehabil. 29, 1383–1398. https://doi.org/10.1080/09602011.2017.1413987 (2019).
Rivas-García, S., García-Bermúdez, O., Catena, A. & Caracuel, A. Pilot study on the effectiveness of the social Mind program for the rehabilitation of social cognition following acquired brain injury. Front. Psychol. 15, 1338335. https://doi.org/10.3389/fpsyg.2024.1338335 (2024).
Turner-Stokes, L. & Wade, D. Rehabilitation following acquired brain injury: concise guidance. Clin. Med. 4, 61–65. https://doi.org/10.7861/clinmedicine.4-1-61 (2004).
Wade, D. T. What is rehabilitation? An empirical investigation leading to an evidence-based description. Clin. Rehab. 34 (5), 571–583. https://doi.org/10.1177/0269215520905112 (2020).
Dams-O’Connor, K. & Gordon, W. Integrating interventions after traumatic brain injury: A synergistic approach to neurorehabilitation. Brain Impair. 14 (1), 51–62. https://doi.org/10.1017/BrImp.2013.9 (2013).
Mahncke, H. W., Bronstone, A. & Merzenich, M. M. Brain plasticity and functional losses in the aged: scientific bases for a novel intervention. Prog Brain Res. 157, 81–109. https://doi.org/10.1016/S0079-6123(06)57006-2 (2006).
Merzenich, M. M., Tallal, P., Peterson, B., Miller, S. L. & Jenkins, W. M. Some neurological principles relevant to the origins of – and the cortical plasticity-based remediation of –developmental Language Impairments in Neuronal Plasticity: Building a Bridge from the Laboratory To the Clinic (eds Grafman, J. & Christen, Y.) 169–187 (Springer-, (1999).
Wade, S. L. et al. Pediatric rehabilitation in APA Handbook of neuropsychology - Volume 2: Neuroscience and Neuromethods. (eds King, G. G., Haaland, T. Z. & Crosson, B.) K.Y., 375–392 (American Psychological Association, (2023).
Karver, C. L. et al. Cognitive reserve as a moderator of responsiveness to an online problem-solving intervention for adolescents with complicated mild-to-severe traumatic brain injury. Child. Neuropsychol. 20 (3), 343–357. https://doi.org/10.1080/09297049.2013.796918 (2014).
Tlustos, S. J. et al. A randomized problem-solving trial for adolescent brain injury: changes in social competence. Rehabil Psychol. 61 (4), 347–357. https://doi.org/10.1037/rep0000098 (2016).
Hypher, R. E. et al. Paediatric goal management training in patients with acquired brain injury: study protocol for a randomised controlled trial. BMJ Open. 9 (8), e029273. https://doi.org/10.1136/bmjopen-2019-029273 (2019).
Levine, B. et al. Rehabilitation of executive functioning in patients with frontal lobe brain damage with goal management training. Front. Hum. Neurosci. 5, 9. https://doi.org/10.3389/fnhum.2011.00009 (2011).
Stuss, D. T. & Knight, R. T. Principles of Frontal Lobe Function (Oxford University Press, 2002).
Wade, S. L. et al. Widespread clinical implementation of the teen online problem-solving program: progress, barriers, and lessons learned. Front. Rehabil Sci. 7 (3), 1089079. https://doi.org/10.3389/fresc.2022.1089079 (2023).
Locascio, G. & Slomine, B. Cognitive Rehabilitation for Pediatric Neurological Disorders (Cambridge University Press, 2018).
Wade, S. L. et al. Telepsychotherapy with children and families: lessons gleaned from two decades of translational research. J. Psychother. Integr. 30 (2), 332–347. https://doi.org/10.1037/int0000215 (2020).
Wade, S. L. et al. Pediatric rehabilitation. In (eds Brown, G. G., Crosson, B., Haaland, K. Y. & King, T. Z.) APA Handbook of Neuropsychology: Neuroscience and Neuromethods (375–392). (American Psychological Association, https://doi.org/10.1037/0000308-018 (2023).
Boutron, I. et al. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann. Intern. Med. 148 (4), 295–309. https://doi.org/10.7326/0003-4819-148-4-200802190-00008 (2008).
Campbell, M. K., Elbourne, D. R. & Altman, D. G. CONSORT group. CONSORT statement: extension to cluster randomised trials. BMJ 328 (7441), 702–708. https://doi.org/10.1136/bmj.328.7441.702 (2004).
Kang, H. Sample size determination and power analysis using the G*Power software. J. Educ. Eval Health Prof. 18, 17. https://doi.org/10.3352/jeehp.2021.18.17 (2021).
Teasdale, G. & Jennett, B. Assessment of coma and impaired consciousness. A practical scale. Lancet 2 (7872), 81–84. https://doi.org/10.1016/s0140-6736(74)91639-0 (1974).
Flannery, J. in The Levels of Cognitive Functioning Assessment Scale. Measurement of Nursing Outcome – Second Edition. 34–56 (eds Strickland, O. L. & DiIorio, C.) (Springer Publishing Company, 2003).
Trauner, D. A. Hemispatial neglect in young children with early unilateral brain damage. Dev. Med. Child. Neurol. 45 (3), 160–166. https://doi.org/10.1111/j.1469-8749.2003.tb00924.x (2003).
Wechsler, D. Wechsler Preschool and Primary Scale of Intelligence–Fourth Edition (WPPSI-IV): Administration and Scoring Manual (The Psychological Corporation, 2012a).
Wechsler, D. Wechsler Preschool and Primary Scale of Intelligence–Fourth Edition (WPPSI-IV): Technical and Interpretative Manual (The Psychological Corporation, 2012b).
Wechsler, D. Manual for the Wechsler Intelligence Scale for Children-Fourth Edition (The Psychological Corporation, 2003a).
Wechsler, D. Wechsler Intelligence Scale for Children-Fourth Edition Technical and Interpretive Manual (The Psychological Corporation, 2003b).
Wechsler, D. WAIS-IV Administration and Scoring Manual (The Psychological Corporation, 2008).
Conners, C. Conners’ Kiddie Continuous Performance Test – Second Edition (Conners K-CPT 2) (Multi-Health Systems, 2006).
Conners, C. K. Conners Continuous Performance Test - Third Edition (Conners CPT 3) & Conners Continuous Auditory Test of Attention (Conners CATA): Technical Manual (Multi-Health Systems Inc., 2014).
Bisiacchi, P. S., Cendron, M., Gugliotta, M., Tressoldi, P. E. & Vio, C. BVN 5–11 - Batteria di valutazione neuropsicologica per l’età evolutiva. [BVN 5–11. Neuropsychological Assessment Battery for adolescence]Erickson,. (2005).
Gugliotta, M., Bisiacchi, P. S., Cendron, M., Tressoldi, P. E. & Vio, C. BVN 12–18 Batteria di Valutazione Neuropsicologica per l’adolescenza. [BVN 12–18. Neuropsychological Assessment Battery for adolescence]Erickson,. (2009).
Benton, A. L., Sivan, A. B., deS Hamsher, K., Varney, N. R. & Spreen, O. Contributions To Neuropsychological Assessment. A Clinical Manual (Oxford University Press, 1983).
Martin, N. A. Test of Visual Perceptual Skills – Third Edition (TVPS-3) (Academic Therapy, 2006).
Rey, A. & Osterrieth, P. A. Rey-Osterrieth Complex Figure Copying Test (APA PsycTests, 1941).
Corsi, P. M. Human memory and the medial temporal region of the brain. Doctoral dissertationDissertation Abstracts International, McGill University,. (1972).
Sannio-Fancello, G. & Cianchetti, C. MCST: Modified Card Sorting Test: Adattamento Italiano Per L’età Evolutiva Del Wisconsin Card Sorting Test Manual (Organizzazioni Speciali, 2003).
Heaton, R. K., Chelune, G. J., Talley, J. L., Kay, G. C. & Curtiss, G. Wisconsin Card Sorting Test manual – Revised and Expanded (Psychological Assessment Resources, 1993).
Culbertson, W. C. & Zillmer, E. A. The tower of London(DX): a standardized approach to assessing executive functioning in children. Arch. Clin. Neuropsychol. 13 (3), 285–301. https://doi.org/10.1016/S0887-6177(97)00033-4 (1998).
Korkman, M., Kirk, U. & Kemp, S. NEPSY-II: Clinical and Interpretative Manual. ( 2nd ed edn (Harcourt Assessment, 2007).
Urgesi, C., Campanella, F. & Fabbro, F. NEPSY-II: contributo alla taratura italiana 2.Giunti Organizzazioni Speciali, (2011).
R Core Team. R: a language and environment for statistical computing. (R. Foundation for Statistical Computing, 2021).
IBM Corp. IBM SPSS Statistics for Windows, Version 29.0.2.0 Armonk (IBM Corp, 2023).
Sargénius, H. L. et al. Cognitive rehabilitation in paediatric acquired brain injury-A 2-year follow-up of a randomised controlled trial. Front. Neurol. 14, 1173480. https://doi.org/10.3389/fneur.2023.1173480 (2023).
Linden, M. et al. (ed Board of Directors of the IPBIS, A.) Further recommendations of the international paediatric brain injury society (IPBIS) for the post-acute rehabilitation of children with acquired brain injury. Brain Inj 38 3 151–159 https://doi.org/.1080/02699052.2024.2309252 (2024).
Molteni, E. et al. Scoping Review on the Diagnosis, Prognosis, and Treatment of Pediatric Disorders of Consciousness. Neurology, Aug 8;101(6):e581-e593, (2023). https://doi.org/10.1212/WNL.0000000000207473 Erratum in: Neurology. Jan 23;102(2):e208068; 10.1212/WNL.0000000000208068.
DePompei, R. & Blosser, J. Pediatric Traumatic Brain Injury: Proactive intervention – Third Edition (Plural Publishing Inc., 2019).
Yeates, K. O. et al. A prospective study of short- and long-term neuropsychological outcomes after traumatic brain injury in children. Neuropsychology 16 (4), 514–523. https://doi.org/10.1037/0894-4105.16.4.514 (2002).
Rohrer-Baumgartner, N. et al. Rehabilitation for children with chronic acquired brain injury in the child in context intervention (CICI) study: study protocol for a randomized controlled trial. Trials 23 (1), 169. https://doi.org/10.1186/s13063-022-06048-8 (2022).
Olson, K., Jacobson, K. K. & Van Oot, P. Ecological validity of pediatric neuropsychological measures: current state and future directions. Appl. Neuropsychol. Child. 2 (1), 17–23. https://doi.org/10.1080/21622965.2012.686330 (2012).
Tamm, L. & Peugh, J. Concordance of teacher-rated and performance-based measures of executive functioning in preschoolers. Child. Neuropsychol. 25 (3), 410–424. https://doi.org/10.1080/09297049.2018.1484085 (2019).
Tan, A., Delgaty, L., Steward, K. & Bunner, M. Performance-based measures and behavioral ratings of executive function in diagnosing attention-deficit/hyperactivity disorder in children. Atten. Defic. Hyperact Disord. 10 (4), 309–316. https://doi.org/10.1007/s12402-018-0256-y (2018).
Vriezen, E. R. & Pigott, S. E. The relationship between parental report on the BRIEF and performance-based measures of executive function in children with moderate to severe traumatic brain injury. Child. Neuropsychol. 8 (4), 296–303. https://doi.org/10.1076/chin.8.4.296.13505 (2002).
Menon, D. K. & Bryant, C. Time for change in acquired brain injury. Lancet Neurol. 18 (1). https://doi.org/10.1016/S1474-4422(18)30463-0 (2019).
Shah, A. A. et al. Gaps in access to comprehensive rehabilitation following traumatic injuries in children: A nationwide examination. J. Pediatr. Surg. 54 (11), 2369–2374. https://doi.org/10.1016/j.jpedsurg.2019.06.001 (2019).
Wade, S. L. et al. Adapting intervention approaches to new contexts: three case studies of international adaptation of the teen online problem solving (TOPS) program. Rehab Psychol. 66 (4), 356–365. https://doi.org/10.1037/rep0000414 (2021).
Greenspan, A. I. & MacKenzie, E. J. Use and need for post-acute services following paediatric head injury. Brain Inj. 14 (5), 417–429. https://doi.org/10.1080/026990500120529 (2000).
Kleim, J. A. & Jones, T. A. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. JSLHR 51(1), S225–S239; (2008). https://doi.org/10.1044/1092-4388(2008/018) (2008).
Forsyth, R. et al. Paediatric rehabilitation ingredients measure: a new tool for identifying paediatric neurorehabilitation content. Dev. Med. Child. Neurol. 60 (3), 299–305. https://doi.org/10.1111/dmcn.13648 (2018).
Acknowledgements
We would like to acknowledge the help and effort in the project of the following speech and neurocognitive therapists, who allowed selecting and categorizing activities and exercises delivered to children: Brivio Veronica, Liggi Claudio, Mapelli Sara, Miccoli Annalisa, Molteni Chiara, Panzeri Maura, Pigazzini Teresa, Sala Chiara and Spicuzza Maria.
Funding
This work was supported by Italian Ministry of Health (Ricerca Corrente 2019–2023 to V.P. and S.S., Ricerca Corrente 2024–2025 to S.S. and Ricerca Corrente 2024–2025 to Emilia Biffi). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
S.S., S.G., M.R., V.P., C.C. and C.U. contributed to the design of the work. C.C. and S.F. wrote the main manuscript and prepared tables and figures. C.C. and F.S. performed statistical analyses. S.F. and C.P. contributed to data storage. S.S. and V.P. were project administrators. S.S., V.P. and E.B. were responsible for funding acquisition. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Corti, C., Frigerio, S., Recla, M. et al. Randomized clinical trial on the effects of early cognitive interventions for children with acquired brain injury. Sci Rep 15, 22189 (2025). https://doi.org/10.1038/s41598-025-06793-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-06793-1