Abstract
To determine correlation between the Extended Disability Status Scale(EDSS) grade and the progression of neuromyelitis optica(NMO) patients’ levels of the chemokine CXC ligand 13 (CXCL13) in their serum and cerebrospinal fluid. This research included forty-one patients diagnosed with neuromyelitis optica(NMO) and forty-three patients diagnosed with multiple sclerosis(MS). The control group consisted of forty-three non-inflammatory neurological disease(NND) patients. The patients’ serum and cerebrospinal fluid CXCL13 levels were measured. Patients in NMO group and MS group had serum and cerebrospinal fluid with CXCL13 levels that were substantially greater than those in the NND group. When comparing the CXCL13 levels of blood and cerebrospinal fluid between patients in the EDSS ≥ 3.5 group and the EDSS<3.5 group, with the EDSS ≥ 3.5 group’s CXCL13 levels being greater(P<0.05). There was a positive correlation between the serum CXCL13 and the EDSS grades of both the NMO and MS groups(r = 0.884, P < 0.001); The cerebrospinal fluid CXCL13 of the NMO and MS groups showed a positive correlation with their EDSS grades(r = 0.681, P < 0.001). EDSS scores of NMO patients were positively correlated with their serum BLC-1 (r = 0.896, P < 0.001); EDSS scores of NMO patients were positively correlated with their cerebrospinal fluid BLC-1 (r = 0.678, P < 0.001).EDSS scores of MS patients were positively correlated with their serum BLC-1 (r = 0.852, P < 0.001); EDSS scores of MS patients were positively correlated with their cerebrospinal fluid BLC-1 (r = 0.613, P < 0.001). Serum and cerebrospinal fluid levels of CXCL13 may serve as an important biomarker for the presumptive assessment of the degree of disability in NMO and MS disease, providing a basis for the treatment and control of the disease.
Similar content being viewed by others
Introduction
Neuromyelitis optica (NMO) is a relapsing neuropathy that can infiltrate the optic nerve and spinal cord. It is a central nervous system inflammatory demyelinating illness caused by the immune system1,2. It mainly occurs in areas with high levels of expression of water channel aquaporin-4 (AQP4) on the astrocyte membrane, and is more common in the spinal cord, optic nerve and brain3,4. The spinal cord-related symptoms are mainly transverse spinal cord damage, and the clinical symptoms related to the optic nerve are mostly blurred vision, vision loss, etc. Recent studies have found that NMO can also induce other central nervous system-related symptoms, such as: vertigo, nausea, mild hemiplegia, etc., and severe cases may even induce cognitive impairment5. More than 90% of such patients have a long course of disease, and many patients may be accompanied by severe sequelae, such as limb dysfunction and visual impairment, which seriously affect the patients’ daily life6. At present, the impairment of spinal cord nerve function caused by NMO has become one of the main causes of disability (not caused by trauma) in young and middle-aged people, and its incidence has been on the rise in recent years, and it is getting younger7. Adrenocorticoids are widely used therapeutic medications for the therapy of autoimmune demyelinating illnesses of the central nervous system because of their anti-inflammatory and immunosuppressive properties. During the acute relapse stage of the illness, short-term intravenous pulse therapy can reduce the length of the relapse period and encourage functional recovery. At present, the specific mechanism of action of glucocorticoids in the treatment of MS and NMO is not yet clear. It may promote the destruction and disintegration of lymphocytes by inhibiting the phagocytosis and processing of antigens by macrophages, promoting their removal from blood vessels and reducing the number of lymphocytes in the circulation. The dose may inhibit plasma cells and antibody production, thereby inhibiting humoral immunity8. However, traditional treatment options, such as acute-phase treatment options that focus on suppressing and blocking humoral immunity, include: (1) “glucocorticoid shock” therapy: inhibiting plasma cell function and promoting the production of anti-inflammatory factors; (2) Maintenance treatment plan during the remission period: Inhibition of “immune cells”; (3) “Plasma exchange” therapy: It can quickly metabolize autoimmune antibodies out of the body; (4) Immunoglobulin shock therapy that blocks the activity of autoimmune antibodies. The therapeutic effect has limitations. Traditional treatment plans still cannot effectively control the patient’s condition and are prone to recurrent attacks. Moreover, most drugs currently used in clinical practice are based on multiple sclerosis (MS), lacking in-depth research on the pathogenesis of NMO and the development of immune targeted drugs. Consequently, in order to provide a foundation for the clinical diagnosis and management of this illness, it is imperative to begin from the immune perspective of NMO and investigate its mechanism from the standpoint of immune regulation. The chemokine CXC ligand 13 (CXCL13) is a crucial component of the chemokine family. It is crucial for the movement, aggregation, and growth of B cell secondary lymphoid tissue9 and is a marker of B lymphocyte aggregation10. CXCL13 can contribute to the development of autoimmune illnesses by interacting with B cells, and B lymphocytes are crucial to the pathophysiology of the condition11. At the same time, chemokines can induce and activate immune cells in peripheral blood, thereby selectively destroying the blood-brain barrier, thus promoting the formation of cerebrospinal fluid oligoclonal bands and demyelinating lesions, leading to neurological dysfunction. Nevertheless, CXCL13’s function in NMO illness is still not entirely understood. In order to identify new targets for NMO immunotherapy, this investigation will examine the expression of CXCL13 in the serum and cerebrospinal fluid of NMO patients as well as examine CXCL13’s function in the disease’s pathophysiology.
Materials and methods
General information
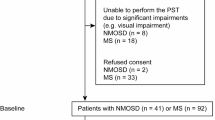
The investigation included 41 patients with neuromyelitis optica (NMO) and 43 patients with multiple sclerosis (MS) who received treatment at our hospital between February 2022 and July 2023. The control group consisted of forty-three non-inflammatory neurological disease (NND) patients who came to our institution in the same time frame. There were 43 MS patients, 29 females, and 14 males, with an average age of (37.48 ± 2.76) years, an average disease duration of (10.27 ± 3.14) years, and an average number of relapses of (3.86 ± 1.10); There were 41 NMO patients, 30 women, and 11 men, with an average age of (36.92 ± 2.58) years an average disease duration of (10.15 ± 3.31) years, and an average number of recurrences (3.98 ± 1.06); The average age of the 43 NND patients (including 25 cases of vascular headache and 18 cases of epilepsy)was (37.14 ± 2.62) years; there were 31 female and 12 male. There was no statistically significant variation in the overall data for every group (P > 0.05), and they were similar to each other. The Ethics Committee of Chenzhou First People’s Hospital gave its approval for this research, in accordance with the Declaration of Helsinki. Signed informed consent were also obtained from all participants.
Criteria of diagnostic
Patients with NMO satisfy the NMO diagnostic requirements12: necessary conditions: (1) Acute myelitis; (2) Optic neuritis. Supporting conditions: (1) Spinal cord lesions ≥ 3 segments; (2) Aquaporin 4 (AQP4) antibody test result is positive; (3) The multiple sclerosis (MS) diagnosis criteria are not met by brain MRI. If two or more of the three supporting conditions are met at the same time, NMO can be diagnosed.
MS patients meet the 2017 McDonald MS diagnostic criteria13.
Criteria of inclusion
(1) The patients fit the diagnostic requirements listed above; (2) All patients develop new symptoms and signs of neurological deficit, which last for at least 24 h or more, and the Expanded Disability Functional Status Scale (EDSS) grade increases by ≥ 1 point, that is, all patients are in the condition of acute relapse period, and the clinical type is relapsing-remitting type; (3) NMO and MS patients within 1 week of the acute relapse period; (4) Both patients can accept the examination plan of this study; (5) Patients’ and their families’ informed consent for this research, as well as the signing of an informed consent form; (6) For six months, none of the study participants had taken any medications that impair immune function.
Criteria of exclusion
(1) Combined with other systemic diseases that affect the EDSS score; (2) Patients are taking hormones or immunosuppressants before blood collection; (3) Combined with infectious diseases, rheumatic immune diseases or malignant tumor diseases; (4) Combined with important organs functional impairment; (5) The patient’s mental and neurological status is unable to cooperate with this researcher; (6) Additional autoimmune antibodies that are positive include glial fibrillary acidic protein antibody (GFAP Ab) and anti-myelin oligodendrocyte glycoprotein antibody (MOG Ab); (7) Pregnant or lactating women; (8) Clinical data are incomplete.
Specimen collection
Before immunotherapy (including hormone, immunosuppressant or immunomodulator treatment), four milliliters of venous blood from fasting volunteers were drawn in the morning and put in an EDTA anticoagulant tube after all research subjects gave their informed consent. The supernatant was centrifuged at 3000 r/min for 15 min at room temperature, and it was then saved in an EP tube at -80 °C for further use.
After all patients signed the informed consent form for lumbar puncture, 4 ml of cerebrospinal fluid was collected through lumbar puncture and stored in an EP tube at -80 °C for future use.
Detection of CXCL13 levels
Using an enzyme-linked immunosorbent assay, the CXCL13 levels in the serum and cerebrospinal fluid of each group of patients were ascertained by carefully according to the kit’s instructions.
Expanded disability functional status scale (EDSS) grade
The Expanded Disability Status Scale (EDSS) grade developed by Kurtzke14 was used to judge patients in the onset stage of NMO and NND. The EDSS score can be divided into 3 levels: 0 to 3 are classified as mild disability, 3.5 to 5.5 is classified as moderate disability, and 6.0 to 10 is classified as severe disability. The lower the grade, the better the client’s optic nerve condition.
Observation indicators
(1) Compare the CXCL13 levels in serum and cerebrospinal fluid of each group ; (2) Examine the differences between the NMO and MS groups’ EDSS grades; (3) Sort the patients based on their EDSS grades, then contrast the CXCL13 levels in their serum and CSF fluid between those with varying EDSS grades; (4) Examine the relationship between EDSS grades and the levels of CXCL13 in the serum and cerebrospinal fluid.
Statistical methods
Software called SPSS 22.0 was used to do the statistical analysis. Measurement data were expressed as mean ± standard deviation (\(\bar{x}\) ± s). One-way analysis of variance was used to compare groups, and t-tests were used to compare groups further in pairs. Count data were expressed as frequencies (n), χ2 test was used; For the correlation analysis, Spearman correlation was employed, and a statistically significant variation was defined as P < 0.05.
Results
CXCL13 levels in serum and cerebrospinal fluid of each group
Patients in the NMO group and MS group had considerably higher serum and cerebrospinal fluid CXCL13 levels contrasted to the NND group. Additionally, the CXCL13 level in the NMO group was considerably higher than that in the MS group, with statistically meaningful disparities (P < 0.05). See Table 1; Fig. 1.
Contrast of EDSS grades between NMO group and MS group
Patients in the NMO group had significantly higher EDSS scores than those in the MS group, with a statistically meaningful distinction (P < 0.05). See Table 2; Fig. 2.
Comparison of serum and cerebrospinal fluid CXCL13 levels in NMO and MS patients with different EDSS scores
Patients in the EDSS ≥ 3.5 group had greater serum and cerebrospinal fluid CXCL13 levels than those in the EDSS<3.5 group, and this disparity was of statistical significance (P < 0.05). See Table 3; Fig. 3.
Correlation analysis of CXCL13 and EDSS score in NMO and MS patients
There was a positive correlation between the serum CXCL13 and the EDSS grades of both the NMO and MS groups (r = 0.884, P < 0.001); The cerebrospinal fluid CXCL13 of the NMO and MS groups showed a good correlation with their EDSS grades (r = 0.681, P < 0.001). See Table 4. EDSS scores of NMO patients were positively correlated with their serum BLC-1 (r = 0.896, P < 0.001); EDSS scores of NMO patients were positively correlated with their cerebrospinal fluid BLC-1 (r = 0.678, P < 0.001). See Table 5. EDSS scores of MS patients were positively correlated with their serum BLC-1 (r = 0.852, P < 0.001); EDSS scores of MS patients were positively correlated with their cerebrospinal fluid BLC-1 (r = 0.613, P < 0.001). See Table 6.
Discussion
A demyelinating condition of the central nervous system, neuromyelitis optica (NMO) primarily affects the optic nerve and spinal cord. The brain can also be affected, which can be caused by humoral immune disorders widely involved in cellular immunity. It is often characterized by unilateral or bilateral optic neuritis and/or longitudinally extended long segment transverse myelitis, which is more prevalent in middle-aged and young women, has a high rate of recurrence and impairment, and has the potential to significantly lower patients’ life quality7. Another demyelinating condition of the central nervous system with an unclear etiology is multiple sclerosis (MS). Myelitis and optic neuritis symptoms can appear clinically in both MS and NMO. Neuroinflammatory illnesses are frequently hard to diagnose. Immune responses are aberrant in both MS and NMO, and they are crucial to the pathophysiology of both conditions15. Numerous investigations have demonstrated the critical role B lymphocytes play in the development of autoimmune demyelinating disorders affecting the central nervous system16. Chemokines have been linked to a number of physiological processes in the body, including immunological responses, according to current research. Among them, the CXC subfamily is closely related to the body ‘s inflammatory response. CXCL13 is an important member of the CXC subfamily, which can bind to the chemokine CXC receptor 5 (CXCR5) and play a crucial role in immune response, lymphogenesis, and lymphoid tissue17,18. Chemokines can participate in acute and chronic inflammatory reactions, and can chemoattract different leukocyte subtypes to the inflammatory response area and induce the localization of inflammatory cells in tissues19. In the process of neuroinflammatory response, CXCL13 is the main factor recruiting B cells, mainly secreted by follicular dendritic cells in B cell follicles. It can bind to CXCR5 receptors on the surface of mature B lymphocytes, play a chemotactic role in B cells20, and participate in various immune inflammatory response related diseases in the central nervous system, such as multiple sclerosis, anti NMDA receptor encephalitis, neurolyme disease, and HIV encephalopathy21,22. CXCL13 is obviously related to the lymphatic microenvironment in the body. Studies have found that the receptor of CXCL13 is located in B cells. After CXCL13 binds to CXCR5, it can promote the induction of enhanced B cell activity, thereby aggravating the body ‘s immune inflammatory response. And it is significantly related to the degree of B cell activation, and then participates in the development of autoimmune diseases 20. We identified and examined CXCL13 in the peripheral blood and cerebrospinal fluid of NMO patients in order to learn more about the function of CXCL13 in the pathophysiology of NMO and whether there is a relationship with disease activity.
Research has revealed that individuals with neuromyelitis optica (NMO) have specific antibodies in their serum against the astrocytic water channel aquaporin-4 (AQP4), which is produced by plasma cells. This finding confirms the pathogenic function of B cells in NMO. B cell activating factor (BAFF) and CXCL13 are two essential components in the generation of antibodies23. The essence of NMO is impaired function of astrocytes, which have antigen-presenting effects. Astrocytes can secrete multiple types of cytokines after activation or injury, thereby inducing immune responses24, thereby destroying the blood-brain barrier, causing inflammatory cells such as eosinophils and neutrophils and their related cytokines to enter the central nervous system from the peripheral blood circulation, further participating in white matter demyelination lesions and axonal degeneration in the central nervous system. CXCL13 is an important component of the immune system by regulating the directional chemotaxis of B cells and causing B cells to produce antibodies with the assistance of follicular helper T cells (Tfh). In this research, patients in the NMO group and MS group had serum and cerebrospinal fluid CXCL13 levels that were substantially greater than those of the NND group, and the CXCL13 level of the NMO group was considerably higher than that of the MS group. Both of the variations have statistical significance (P < 0.05). Previous studies25 have shown that individuals with NMO had greater serum CXCL13 levels than individuals with other non-inflammatory neurological disorders. It aligns with the findings of this investigation. Some scholars have found through studies of serum cytokines in NMO and MS patients that compared with MS patients, patients with NMOs exhibit a more robust inflammatory and anti-inflammatory response mechanism26. This may also be the reason for the increased levels of CXCL13 in the serum and cerebrospinal fluid of NMO group patients compared to MS patients. By attracting inflammatory cells to the central nervous system, CXCL13 may contribute to the pathophysiology of MS and NMO. The pathophysiology of both MS and NMO may be significantly influenced by CXCL13, and CXCL13 levels in serum and cerebrospinal fluid may be employed as markers to differentiate NMO from MS. In B lymphocyte follicles, follicular dendritic cells and secondary lymphoid tissue germinal center -follicular helper T cells can express CXCL13, and CXCR5 expressed by B cells and follicular helper T cells is its receptor, and the interaction between the two can chemotaxis guide the migration of B lymphoid follicles, and can strengthen the interaction between follicular helper T cells and B cells in the germinal center of secondary lymphoid tissue27. Although CXCL13 mostly acts locally, its steady concentration can be found in the blood, and variations in serum CXCL13 levels can indicate the degree of immunological activation. The specific receptor for CXCL13, CXCR5, is mainly localized in astrocytes. The activation or damage of astrocytes may be closely related to the level of CXCL13 in the cerebrospinal fluid of the NMO group. The increase in CXCL13 levels can affect the survival and differentiation of B cells, further upregulating the autoantibody AQP4 antibody produced by B cells, thereby promoting the pathophysiological process of NMO 28. Patients in the EDSS ≥ 3.5 group in this research had greater blood and cerebrospinal fluid CXCL13 levels than patients in the EDSS<3.5 group, and the distinction was statistically meaningful (P <0.05). This indicates that CXCL13 levels in patients’ serum and cerebrospinal fluid may be closely related to their disease disability and clinical manifestations. The increased expression levels of CXCL13 in the serum and cerebrospinal fluid of NMO patients regulate the survival and differentiation of B cells, which in turn leads to increased levels of AQP4-Ab formed by B cells, ultimately promoting the pathological and physiological processes of NMO disease. CXCL13 has been proposed as a biomarker for serum and cerebrospinal fluid that may be used to predict the severity of MS and NMO patients. The present investigation’s correlation analysis of EDSS grades revealed a positive link between the EDSS grades of the NMO group and the MS group and their blood CXCL13 (r = 0.884, P < 0.001); The EDSS grades of NMO and MS groups are positively correlated with their cerebrospinal fluid CXCL13 (rs =0.681, P < 0.001), that is, for NMO and MS patients in the acute relapsing stage, EDSS grades and CXCL13 levels in blood and cerebrospinal fluid are correlated, which is consistent with the above-mentioned research results. The clinical symptoms are more severe the higher the EDSS grade, suggesting that as CXCL13 levels increase, disease disability may increase, indicating that CXCL13 levels in serum and cerebrospinal fluid may serve as an important biomarker for inferring the degree of disability in NMO and MS diseases.
In summary, serum and cerebrospinal fluid levels of CXCL13 may serve as an important biomarker for the presumptive assessment of the degree of disability in NMO and MS disease, providing a basis for the treatment and control of the disease.
Data availability
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
References
Levy, M., Fujihara, K. & Palace, J. New therapies for neuromyelitis optica spectrum disorder. Lancet Neurol. 20(1), 60–67. https://doi.org/10.1016/S1474-4422(20)30392- (2021).
Wallach, A. I., Tremblay, M. & Kister, I. Advances in the treatment of neuromyelitis optica spectrum disorder. Neurol. Clin. 39(1), 35–49. https://doi.org/10.1016/j.ncl.2020.09 (2021).
Dutra, B. G. et al. Neuromyelitis optica spectrum disorders: Spectrum of MR imaging findings and their differential diagnosis. Radiographics. https://doi.org/10.1148/rg.2018170141 (2018). Erratum in: Radiographics. 2018;38(2):662. 38(1):169–193.
Alves Do Rego, C. & Collongues, N. Neuromyelitis optica spectrum disorders: Features of aquaporin-4, myelin oligodendrocyte glycoprotein and double-seronegative-mediated subtypes. Rev. Neurol. (Paris). 174(6), 458–470. https://doi.org/10.1016/j.neurol.2018.02.084 (2018).
Jarius, S., Paul, F., Weinshenker, B.G., Levy, M., Kim, H.J., Wildemann, B. Neuromyelitis optica. Nat. Rev. Dis. Primers. 6(1), 85 (2020).
Brown, F. S. Factors affecting relapse rate in patients with neuromyelitis optica spectrum disorder. Lancet Neurol. 19(7), 564. https://doi.org/10.1016/S1474-4422(20)30184-8 (2020).
Simaniv, T. O. et al. Optikoneĭromielita [Neuromyelitis optica and neuromyelitis optica spectrum disorders]. Zh Nevrol Psikhiatr Im SS Korsakova 119(10. Vyp. 2), 35–48 https://doi.org/10.17116/jnevro20191191035 (2019). Russian.
Matsushita, T. Corticosteroid therapy in patients with Autoimmune diseases of the Central Nervous System. Brain Nerve. 73(5), 408–413. https://doi.org/10.11477/mf.1416201779 (2021). Japanese.
Kim, Y. H. et al. Serum CXCL13 reflects local B-cell mediated inflammatory demyelinating peripheral neuropathy. Sci. Rep. 9(1), 16535. https://doi.org/10.1038/s41598-019-52643-2 (2019).
Armas-González, E. et al. Role of CXCL13 and CCL20 in the recruitment of B cells to inflammatory foci in chronic arthritis. Arthritis Res. Ther. 20(1), 114. https://doi.org/10.1186/s13075-018-1611-2 (2018).
Furman, M. J. et al. B cell targeted therapies in inflammatory autoimmune disease of the central nervous system . Front. Immunol. 14, 1129906. https://doi.org/10.3389/fimmu.2023.1129906 (2023).
Wingerchuk, D. M. et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85(2), 177–189. https://doi.org/10.1212/WNL.0000000000001729 (2015). Epub 2015 Jun 19. PMID: 26092914; PMCID: PMC4515040.
Thompson, A. J. et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria . Lancet Neurol. 17(2), 162–173. https://doi.org/10.1016/S1474-4422(17)30470-2 (2018).
Kurtzke, J. F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS) . Neurology 33(11), 1444–1452. https://doi.org/10.1212/wnl.33.11.1444 (1983).
Khan, A. W. et al. Autoimmune Neuroinflammatory diseases: Role of interleukins . Int. J. Mol. Sci. 24(9), 7960. https://doi.org/10.3390/ijms24097960 (2023).
Zouali, M. et al. DNA methylation signatures of autoimmune diseases in human B lymphocytes. Clin. Immunol. 222, 108622. https://doi.org/10.1016/j.clim.2020.108622. [1 8 ], . Cancers (Basel). 2021;13(23):6132. doi: 10.3390/cancers13236132. (2021).
Henningsson, A. J., Lager, M., Brännström, R. et al. The chemokine CXCL13 in cerebrospinal fluid in children with Lyme neuroborreliosis. Eur. J. Clin. Microbiol. Infect. Dis. 37(10), 1983–1991. https://doi.org/10.1016/j.ejphar.2019.172545 (2018).
Matsuo, T., Yoshie, O., Nakayama, T. Multifaceted roles of chemokines and chemokine receptors in tumor immunity. Cancers (Basel). 13(23), 6132 https://doi.org/10.3390/cancers13236132.
Kolanko, E. et al. Increased immunomodulatory capacity of human amniotic cells after activation by pro-inflammatory chemokines . Eur. J. Pharmacol. 859, 172545. https://doi.org/10.1016/j.ejphar.2019.172545 (2019).
Pan, Z. et al. Role of the CXCL13/CXCR5 axis in autoimmune diseases. Front Immunol. 13, 850998. https://doi.org/10.3389/fimmu.2022.850998 (2022). Erratum in: Front Immunol. 2022;13:1061939.
Smíšková, D. et al. Cerebrospinal fluid CXCL13 in non-borrelial central nervous system infections: Contribution of CXCL13 to the differential diagnosis. Infect. Dis. (Lond.) 55(8), 551–558. https://doi.org/10.1080/23744235.2023.2222178 (2023).
Leth, T. A. et al. Discriminating between Lyme neuroborreliosis and other central nervous system infections by use of biomarkers CXCL13 and IL-6. Ticks Tick Borne Dis. 13(5), 101984. https://doi.org/10.1016/j.ttbdis.2022.101984. (2022).
Yi, M. et al. Correlation between serum levels of endothelin-1 and disease severity in patients with neuromyelitis optica spectrum disorders. Immunobiology 225(3), 151959. https://doi.org/10.1016/j.imbio.2020.151959 (2020).
Farina, C., Aloisi, F. & Meinl, E. Astrocytes are active players in cerebral innate immunity . Trends Immunol. 28(3), 138–145. https://doi.org/10.1016/j.it.2007.01.005 (2007). Epub 2007 Feb 2. PMID: 17276138.
Alvarez, E. et al. CXCL13 is a biomarker of inflammation in multiple sclerosis, neuromyelitis optica, and other neurological conditions . Mult Scler. 19(9), 1204–1208. https://doi.org/10.1177/1352458512473362 (2013). Epub 2013 Jan 15. PMID: 23322500; PMCID: PMC3959125.
Wang, K. C. et al. Distinct serum cytokine profiles in neuromyelitis optica and multiple sclerosis. J. Interferon Cytokine Res. 33(2), 58–64. https://doi.org/10.1089/jir.2012.0040 (2013).
Ellrichmann, G. et al. Peripheral CD19 + B-cell counts and infusion intervals as a surrogate for long-term B-cell depleting therapy in multiple sclerosis and neuromyelitis optica/neuromyelitis optica spectrum disorders . J. Neurol. 266(1), 57–67. https://doi.org/10.1007/s00415-018-9092-4 (2019).
Zhang, P., Sun, H. & Ji, Z. Downregulating lncRNA PVT1 relieves astrocyte overactivation induced neuropathic pain through targeting miR-186-5p/CXCL13/CXCR5 axis. Neurochem. Res. 46(6), 1457–1469. https://doi.org/10.1007/s11064-021-03287-0 (2021).
Acknowledgements
None.
Funding
This study is funded by the School level scientific research project of Xiangnan University (2022JX128).
Author information
Authors and Affiliations
Contributions
We declare that all the listed authors have participated actively in the study and all meet the requirements of the authorship. Dr. JZ designed the study and wrote the paper, Dr. SLL performed research, Dr. XXY managed the literature searches and analyses, Dr. HPL undertook the statistical analysis, Dr. YW contributed to the correspondence and paper revision. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The Ethics Committee of Chenzhou First People’s Hospital gave its approval for this research, in accordance with the Declaration of Helsinki. Signed informed consent were also obtained from all participants.
Consent for publication
Not Applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, J., Luo, S., Yao, X. et al. Analysis of changes in the chemokine CXC ligand 13 in serum and cerebrospinal fluid of patients with neuromyelitis optica. Sci Rep 15, 2113 (2025). https://doi.org/10.1038/s41598-025-85650-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-85650-7