Abstract
To investigate the impact of the COVID-19 pandemic on the incidence and clinical characteristics of rhegmatogenous retinal detachment (RRD) patients referred to a high-volume center, Farabi Eye Hospital, Iran. In a retrospective study, all new RRD patients referred to Farabi Eye Hospital between March 2019 and March 2020 (pre-pandemic, Group 1) and March 2020 and March 2021 (post-pandemic, Group 2) were analyzed. The groups were compared based on demographic and clinical data. A total of 375 patients were included (131 pre-pandemic, 244 post-pandemic, and 34 during lockdowns). The during-pandemic group had a shorter referral time (44.97 vs. 76.76 days, p = 0.031) and surgical wait time (4.64 vs. 8.63 days, p < 0.001). No significant differences were found in pre-operative features (etiology, proliferative vitreoretinopathy, break type), surgical procedures, or initial treatment failure rates between the groups. General anesthesia use was significantly higher in the during-pandemic group (81.6% vs. 71.8%, p = 0.029). The COVID-19 pandemic did not significantly alter the demographic, clinical characteristics, or initial surgical outcomes of RRD patients. However, patients were referred and treated more expeditiously during the pandemic. The increased use of general anesthesia requires further investigation.
Similar content being viewed by others
Introduction
Rhegmatogenous retinal detachment (RRD), a sight-threatening condition, occurs when a retinal break permits vitreous fluid to accumulate in the subretinal space, thereby separating the neurosensory retina from the retinal pigment epithelium (RPE)1. With a prevalence of 1 in 10,000 individuals2, RRD necessitates prompt intervention to prevent significant vision loss3. Delays in management not only increase the risk of macular detachment but also correlate with poorer final visual acuity and a higher likelihood of requiring multiple or more complex surgeries4,5.
Proliferative vitreoretinopathy (PVR) is a significant complication of RRD, potentially leading to treatment failure and re-surgery by forming tractional bands within the vitreous that cause tractional retinal detachment6,7. Early diagnosis and treatment of RRD are crucial to prevent PVR and subsequent surgical failure7,8.
The emergence of COVID-19 restricted patient access to healthcare facilities, resulting in a substantial decrease in routine clinical and surgical activity worldwide9,10. This disruption may have resulted in delayed referral and follow-up for RRD patients11,12. Studies from various countries suggest that the COVID-19 pandemic has impacted the incidence, clinical presentation, prognosis, recurrence rates, and treatment approaches for RRD11,12,13,14,15.
In this retrospective study, we compared RRD patients presenting at Farabi Eye Hospital, a tertiary referral center in Iran, pre- and during- the COVID-19 pandeimc. This analysis aims to inform ophthalmologic management of RRD during lockdowns and similar situations.
Methods
The principles of the Declaration of Helsinki were followed in this retrospective study. This study was approved by the Ethics Committee for Biomedical Research at Tehran University of Medical Sciences (code: IR.TUMS.FARABIH.REC.1401.037). Written informed consent was obtained from all participants for data collection and inclusion in the study database. Patient identifiers were anonymized to ensure confidentiality, with access restricted to researchers and data collectors.
We conducted a retrospective analysis of all new cases of RRD managed by two surgeons (E.K. and H.R.) at Farabi Eye Hospital, a tertiary referral center in Iran, from March 2019 to March 2021. This period included one year before the COVID-19 pandemic (March 2019–March 2020) and one year during the pandemic (March 2020–March 2021). Patients were divided into two groups: pre-pandemic (Group 1: March 2019–March 2020) and during-pandemic (Group 2: March 2020–March 2021). Additionally, a subgroup analysis focused on patients who presented during the three official lockdown periods in Iran (March 20–April 9, 2020; August 18–24, 2020; and November 21–December 4, 2020).
Patients with tractional, exudative, or recurrent RRD were excluded from the study to ensure a homogeneous study population focused on primary RRD cases. Additional exclusion criteria included the presence of significant ocular comorbidities that could affect visual outcomes or complicate the surgical intervention, such as advanced diabetic retinopathy, severe uveitis, or extensive ocular penetrating trauma. Patients with a history of vitreoretinal surgery for any reason were excluded to mitigate the potential confounding effects of past surgical treatments. We defined post-surgical RRD as retinal detachment occurring six weeks following any anterior segment surgery. Furthermore, patients with incomplete medical records or missing critical data points necessary for the analysis, such as demographic information, baseline visual acuity, or details of the surgical procedure, were excluded to maintain the integrity and reliability of the study data.
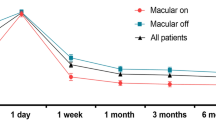
Data collected from medical records included demographics (age, gender), RRD etiology (idiopathic, traumatic, post-surgical), symptom duration to initial presentation, baseline visual acuity (LogMAR), macular involvement (macula-on, partially-off, macula-off), number of involved quadrants (1 to 4), lens status (phakic, pseudophakic, aphakic), PVR grade (absent, A, B, C Anterior, C Posterior), presence of concurrent choroidal detachment, surgical procedures performed (23 guage PPV + Silicon Oil (SO) endotamponade, Scleral buckle (SB), Pneumatic retinopexy with SF6), time interval between initial visit and surgery, anesthesia type (general vs. sedation and local), break ___location (anterior vs. posterior to equator), and need for secondary RRD surgery.
The secondary surgeries for rhegmatogenous retinal detachment (RRD) included Pars plana vitrectomy (PPV) revision following initial PPV, PPV performed after primary scleral buckle placement, PPV after primary pneumatic retinopexy, and scleral buckle surgery following primary PPV. These procedures were performed to address recurrent or failed cases of RRD, to achieve successful retinal reattachment, and to preserve visual function.
Following established protocols16, visual acuities were converted to the LogMAR scale as follows: count fingers (CF) at 6 m (1.0), CF at 3 m (1.5), CF at 1 m (1.75), hand motion (2.0), light perception (2.5), and no light perception (3.0).
Funduscopy using a slit lamp or indirect ophthalmoscopy and macular optical coherence tomography (OCT) were performed using Heidelberg instruments (Heidelberg Engineering, Germany) to assess macular involvement when feasible. B-scan ultrasonography was utilized for cases with vitreous hemorrhage.
Statistical analysis
The Kolmogorov-Smirnov and Shapiro-Wilk tests have been used to assess the continuous variables for normality. The data was reported as mean ± standard deviation (SD) if normality could be assumed; otherwise, it was reported as median ± interquartile range (IQR). Frequency (percentage) was used to report qualitative values. We used the Mann-Whitney test to compare the means between groups due to the non-parametric nature of the data. To compare quantitative variables, we used Fisher’s exact test and Chi-square test based on sample size criteria for each comparison. For the prediction of a nominal outcome variable with more than two categories lacking any rank or order, multinomial logistic regression was used. For data analysis, the Statistical Package for the Social Sciences (SPSS Inc., version 26.0, Chicago, IL, USA) was used at a significance level of 0.05.
Results
A total of 375 patients with RRD were treated at Farabi Eye Hospital during the study period. The majority were male (245, 65.33%) compared to female (130, 34.67%). Patients were divided into pre-pandemic (n = 131, 34.93%) and during-pandemic (n = 244, 65.07%) groups, with 34 patients in the latter group undergoing surgery during official lockdowns.
Demographic and clinical characteristics (age, gender, best-corrected visual acuity, etiology, macular involvement, number of involved quadrants, lens status, PVR grade, break type, and presence of choroidal detachment) did not differ significantly between the pre-pandemic and during-pandemic groups (Table 1).
However, following the COVID-19 pandemic, patients presented significantly earlier after the onset of symptoms (44.97 ± 104.51 vs. 76.76 ± 143.34 days; p = 0.031) and underwent surgery more swiftly after diagnosis (4.64 ± 8.88 vs. 8.63 ± 7.41 days; p < 0.001) compared to the pre-pandemic group. Notably, the proportion of patients with pre-equatorial breaks was significantly higher in the pre-pandemic group (84.0% vs. 70.5%; p = 0.007) (Table 1).
Regarding surgical procedures (Table 2), general anesthesia use increased significantly in the during-pandemic era (81.6% vs. 71.8%; p = 0.029). There were no statistically significant differences between the groups in terms of primary surgery success rate, secondary surgery rate, or primary treatment failure rate.
Subgroup analysis of patients presenting during official lockdown periods within the during-pandemic group revealed no significant differences in demographics, clinical characteristics, surgical techniques, or outcomes compared to those presenting outside lockdowns (Table 3).
Discussion
This retrospective study investigated the impact of the COVID-19 pandemic on the incidence, clinical characteristics, and surgical management of RRD patients referred to a high-volume referral center in Iran. Our findings revealed no significant differences between the pre-pandemic and during-pandemic groups in terms of demographics, clinical features (etiology, PVR grade, macular involvement, etc.), surgical procedures, or primary treatment failure rates. However, we observed a significant decrease in referral time and surgical wait time for RRD patients after the pandemic’s onset. Additionally, the proportion of patients undergoing general anesthesia for RRD surgery increased significantly in the during-pandemic era.
The COVID-19 pandemic significantly disrupted healthcare systems worldwide, impacting patient visits and surgeries, including those in ophthalmology17,18. Our study adds to the growing body of research exploring the pandemic’s effect on the management of RRD patients, offering novel insights from the first such investigation in Iran. Notably, our findings diverge from previous reports in some key aspects.
Our study found an increase in RRD surgeries during the pandemic (244 patients) compared to the pre-pandemic period (131 patients) which is contrary to Patel et al. and Jasani et al. studies which showed a decrease in surgeries11,19. This might be attributed to Farabi Eye Hospital’s role as a specialized ophthalmic center, remaining fully operational even during lockdowns. This factor potentially attracted referrals from other closed institutions and positioned it as one of the most active ophthalmic centers during the first year of the COVID-19 pandemic in Iran. This underscores the importance of maintaining access to emergency ophthalmic care during public health crises.
Consistent with other studies the gender distribution showed a predominance of males in both pre- and during-pandemic groups13,15,20. Furthermore, our study revealed a significantly shorter referral time after symptom onset in the during-pandemic group (44.97 days compared to 76.76 days). This could be due to heightened public awareness campaigns regarding RRD symptoms or anxieties about healthcare accessibility during lockdowns, prompting patients to seek earlier evaluation. Additionally, the potential use of telemedicine for initial consultations during the pandemic could have facilitated faster referrals. Future studies exploring these possibilities are warranted. Although an average presentation delay of 44 days for RRD seems high, it’s important to note that the standard deviation was high in both pre- and during-pandemic groups, suggesting significant variability in presentation times. This variability may be attributed to a variety of factors, such as differences in symptom severity or patient awareness, which could potentially explain the similar results in the macula-off status or involved quadrants of pre- and during-pandemic groups. Additionally, our study relied on patient recall for symptom onset, which might introduce some limitations in accuracy. Future prospective studies with more precise data collection methods may provide more definitive insights into presentation timelines for RRD.
Interestingly, our study revealed a significant decrease in surgical wait time for RRD patients in the during-pandemic group. This finding is particularly noteworthy as it contrasts with the anticipated strain on healthcare systems during pandemics, often leading to longer wait times for elective surgeries (e.g., cataract surgery). There are several possible explanations for this unexpected observation, likely related to the unique operational approach of Farabi Eye Hospital.
First, Farabi Eye Hospital, as the only sub-specialized ophthalmology hospital in Iran, remained fully operational for emergency care throughout the COVID-19 pandemic. This decision, along with public announcements, might have diverted patients directly to our center, bypassing the usual referral system during non-lockdown periods. Moreover, the cancellation of elective surgeries likely resulted in more available operating room time, enabling expedited scheduling of emergency retinal surgeries. This efficient 24/7 approach could have minimized delays in care and potentially prevented complications like macular involvement or increased PVR, which are typically associated with delayed presentations observed in other studies10,13,15,19,21,22.
Despite the significant decrease in referral and surgical wait times observed in the during-pandemic group, our study revealed that the proportion of macula-off RRD patients remained unchanged between the pre- and during-pandemic periods. This finding suggests that the time to surgery and referral, while critical, may not solely dictate the complexity of RRD presentations or the severity of macular involvement. Factors such as the underlying etiology of the detachment, patient awareness of symptoms, and the biological variability in disease progression may play a more pivotal role in determining the proportion of macula-off cases. Our results emphasize the need for further investigation into the interplay between these factors to enhance understanding and management strategies for RRD patients.
Therefore, the experience of Farabi Eye Hospital during the pandemic can be introduced as a successful model for managing ocular emergency patients during lockdowns. Understanding the specific strategies employed, such as maintaining core emergency services and clear communication with the public, can inform future practices to optimize RRD care delivery even outside of public health emergencies.
Our study found no significant difference in surgical technique selection between the pre- and during-pandemic groups. This aligns with some previous studies13,23,24and might be explained by the absence of differences in macular involvement and PVR prevalence observed in our data. In contrast, other studies reported a shift towards PPV with silicone oil tamponade during the pandemic due to the anticipated increase in complex cases with macular involvement and PVR14,20,25.
The proportion of patients who were aphakic was approximately 5% in both groups. This matter may be clarified as follows that some patients may develop retinal detachment following traumatic lens extraction, uneventful cataract surgery, or intracapsular cataract extraction. Consequently, these patients undergo a period of aphakia as a result of the fact that a significant number of surgeons elect to perform secondary procedures to implant intraocular lenses. RRD may be detected as a complication during the initial postoperative follow-up of these patients. According to our findings, there were no significant differences in lens status (phakic, pseudophakic, and aphakia) across the groups. These findings are in line with the findings of a comparable study that reported lens status26.
Similarly, our findings showed no significant difference in primary treatment failure rates between the groups. These results are consistent with studies reporting comparable anatomical success rates despite the pandemic20,24,25. However, the retrospective nature of our study and limited follow-up period necessitate caution in interpreting these findings. Prospective studies with longer follow-ups are crucial to definitively assess the long-term impact of the pandemic on surgical outcomes. The study by Mizuno et al.13 highlights this point, demonstrating a decrease in initial reattachment rates during the pandemic, but ultimately comparable final outcomes between groups.
While our study found no significant difference in secondary surgery rates between the groups, it’s important to acknowledge the potential limitations of a retrospective analysis. The inherent reliance on patient medical records might introduce data collection biases. Additionally, our study design could not account for possible changes in surgical techniques or surgeon expertise during the study period. Prospective studies with standardized outcome measures and longer follow-up periods would be ideal to definitively assess the potential impact of the COVID-19 pandemic on long-term surgical outcomes for RRD patients.
Furthermore, our subgroup analysis of patients presenting during official lockdown periods revealed no significant differences compared to those presenting outside lockdowns. This suggests that the observed decrease in referral and surgical wait times might not be solely attributable to lockdown restrictions. Future research investigating the specific factors influencing patient referral behavior and surgical scheduling during pandemics is warranted.
Interestingly, our study revealed a significant increase in the use of general anesthesia for RRD surgery during the pandemic. This contrasts with studies reporting a decrease in ocular surgeries due to anesthesia limitations20,25. The observed shift at our center might be attributed to concerns about patient cooperation under local anesthesia or sedation, particularly in the context of potential COVID-19 transmission. The use of disposable antiviral filters during endotracheal intubation, as reported elsewhere27, could have mitigated these concerns and facilitated the increased use of general anesthesia. Additionally, changes in resource allocation or staffing patterns within the hospital during the pandemic might have influenced the choice of anesthesia. Further investigation into the rationale behind this shift in anesthesia preference among surgeons and anesthesiologists at our center would be valuable.
The retrospective nature of our study and introduces potential biases in data collection. Medical record review relies on the accuracy and completeness of documentation, which can vary (e.g., IOP measurments and intentional hole during the surgery). There might also be inherent selection bias in the study population as those who presented for care during the pandemic could be different from those who didn’t. Future studies with standardized data collection methods would provide a more robust analysis. Incomplete follow-up data limited our ability to assess final visual acuity and long-term retinal attachment rates definitively. We could only evaluate primary treatment failure rates at the 6-month mark. Long-term outcomes, especially visual acuity, might not be fully captured within this timeframe. The ___location of our hospital, attracting referrals from distant cities, might have also contributed to the follow-up challenge. Patients from afar might have opted for closer follow-up care, leading to incomplete data for our center. Future studies with longer follow-up and strategies to improve patient retention, such as telemedicine consultations, are crucial for a comprehensive evaluation. The generalizability of our findings might be limited. Farabi Eye Hospital, as a specialized center, might have unique protocols and resources compared to other facilities. Additionally, the healthcare landscape and pandemic response strategies might differ significantly between Iran and other countries. As this study constitutes exploratory research, we did not account for P value adjustments for multiple comparisons. Consequently, we need to take caution in interpreting the reported P values. Further research across various institutions and geographic locations is necessary to determine the broader applicability of our observations. Finally, chronic RRD is indicated by a low intraocular pressure (IOP) during the initial visit28. Regrettably, we were unable to evaluate IOP values in this study due to the fact that they were not reliable, as they were measured by various individuals and using different methods. It is proposed that IOP be compared between groups in other investigations.
Conclusions
Our study in an ophthalmic tertiary referral center in Iran revealed unique findings on the impact of COVID-19 on RRD management. While referral rates surged at our center, possibly due to its continued operation, patients experienced faster presentation and treatment. Unlike prior studies, we observed no significant changes in clinical characteristics, surgical techniques, or primary treatment failure rates. Notably, the continued operation of emergency services and public awareness campaigns might have contributed to these observations. An interesting finding was the decrease in surgical wait time, possibly due to heightened public awareness or prioritization within the hospital. The shift towards general anesthesia warrants further investigation. Our study highlights the importance of maintaining core ophthalmic emergency services and clear communication during public health crises. Future prospective studies with longer follow-ups are crucial to definitively assess long-term outcomes.
Data availability
Upon the corresponding author’s request, the data that backs up the conclusions of this study will be provided.
References
D’Amico, D. J. Primary retinal detachment. N. Engl. J. Med. 359 (22), 2346–2354 (2008).
Kwok, J. M., Caberry, W. Y. & Christakis, P. G. Retinal detachment. Cmaj 192 (12), E312–E (2020).
Feltgen, N. & Walter, P. Rhegmatogenous retinal detachment—an ophthalmologic emergency. Deutsches Ärzteblatt Int. 111 (1–2), 12 (2014).
Eibenberger, K., Georgopoulos, M., Rezar-Dreindl, S., Schmidt-Erfurth, U. & Sacu, S. Development of surgical management in primary rhegmatogenous retinal detachment treatment from 2009 to 2015. Curr. Eye Res. 43 (4), 517–525 (2018).
Fischer, C., Kulanga, M. & Hoerauf, H. Trends in retinal detachment surgery: what has changed compared to 2001? Der Ophthalmologe. 115, 663–668 (2018).
Koto, T. et al. Six months primary success rate for retinal detachment between vitrectomy and scleral buckling. Retina 41 (6), 1164–1173 (2021).
BomdicaPR et al. Risk of Rhegmatogenous Retinal detachment (RRD) with Proliferative Vitreoretinopathy (PVR) in a patient’s Second Eye after RRD with PVR development in the First Eye: Vestrum Database Analysis. Investig. Ophthalmol. Vis. Sci. 64 (8), 4558 (2023).
Zhao, P. Retinal Detachment and PVR. Surg. Retina 67–75 (2019).
Toro, M. D. et al. Early Impact of COVID-19 Outbreak on eye care: Insights from EUROCOVCAT Groupp. 5–9 (SAGE Publications Sage UK, 2021).
Poyser, A. et al. Impact of COVID-19 pandemic and lockdown on eye emergencies. Eur. J. Ophthalmol. 31 (6), 2894–2900 (2021).
Patel, L. G. et al. Clinical presentation of rhegmatogenous retinal detachment during the COVID-19 pandemic: a historical cohort study. Ophthalmology 128 (5), 686–692 (2021).
Franzolin, E., Longo, R., Casati, S., Ceruti, P. & Marchini, G. Influence of the COVID-19 pandemic on admissions for retinal detachment in a tertiary eye emergency department. Clin. Ophthalmol. 15, 2127–2131 (2021).
Mizuno, M. et al. Effect of the COVID-19 Pandemic on Surgical outcomes for Rhegmatogenous Retinal detachments. J. Clin. Med. 12 (4), 1522 (2023).
Dmuchowska, D. et al. The impact of three waves of the COVID-19 pandemic on the characteristics of primary rhegmatogenous retinal detachments at a tertiary referral centre. Clin. Ophthalmol. 15, 3481–3491 (2021).
Ferreira, A., Afonso, M., Silva, N. & Meireles, A. The impact of COVID-19 pandemic on surgical primary retinal detachments. Ophthalmologica 245 (2), 111–116 (2022).
Moussa, G., Bassilious, K. & Mathews, N. A novel excel sheet conversion tool from Snellen fraction to LogMAR including ‘counting fingers’, ‘hand movement’, ‘light perception’ and ‘no light perception’ and focused review of literature of low visual acuity reference values. Acta Ophthalmol. 99, 963–965 (2021).
Legrottaglie, E. F. et al. Management of an ophthalmology department during COVID-19 pandemic in Milan, Italy. Eur. J. Ophthalmol. 31 (5), 2259–2267 (2021).
Wasser, L. M. et al. The impact of COVID-19 on intravitreal injection compliance. SN Compr. Clin. Med. 2 (12), 2546–2549 (2020).
Jasani, K. M. et al. Changing clinical patterns of Rhegmatogeneous Retinal detachments during the COVID19 pandemic lockdown in the North West of the UK. Eur. J. Ophthalmol. 31 (6), 2876–2880 (2021).
Li, J., Zhao, M. & She, H. The impact of the COVID-19 pandemic on rhegmatogenous retinal detachment treatment patterns. BMC Ophthalmol. 21, 1–10 (2021).
Roshanshad, A. & Binder, S. Retinal detachment during COVID-19 era: a review of challenges and solutions. Spektrum Der Augenheilkunde. 36 (1), 32 (2022).
Awad, M. et al. Delayed presentation and increased prevalence of proliferative vitreoretinopathy for primary rhegmatogenous retinal detachments presenting during the COVID-19 pandemic lockdown. Eye 35 (4), 1282–1283 (2021).
Weber, C., Stasik, I., Holz, F. G. & Liegl, R. Impact of COVID-19 before and after 2020 on retinal detachment management in a tertiary eye hospital in Germany. Ophthalmologica 245 (6), 577–587 (2023).
Moussa, G. et al. Sustained impact of COVID-19 on primary retinal detachment repair in a tertiary eye hospital from March to December 2020. Spektrum Der Augenheilkunde. 37 (1), 1–8 (2023).
Wu, P-Y. et al. Surgical decisions and outcomes of rhegmatogenous retinal detachment during the coronavirus disease 2019 pandemic: data from a tertiary referral center in Taiwan. Indian J. Ophthalmol. 71 (6), 2548–2554 (2023).
Arjmand, P. et al. Impact of the COVID-19 pandemic on characteristics of retinal detachments: the Canadian experience. Can. J. Ophthalmol. 56 (2), 88–95 (2021).
Upadhyay, P., Ichhpujani, P. & Solanki, A. Recent trends in anesthetic agents and techniques for ophthalmic anesthesia. J. Anaesthesiol. Clin. Pharmacol. 39 (3), 343–348 (2023).
Wang, Q., Thau, A., Levin, A. V. & Lee, D. Ocular hypotony: a comprehensive review. Surv. Ophthalmol. 64 (5), 619–638 (2019).
Author information
Authors and Affiliations
Contributions
Elias Khalili Pour & Hamid Riazi-Esfahani & Hooshang Faghihi prepared the idea and Ali Momeni & Mahdi Jamalitootakani prepared a proposal, Ali Momeni & Fariba Ghassemi collected data, Hassan Asadigandomani & Mohammadreza Mehrabi Bahar analyzed data and prepared the primary draft. All authors read and proofed the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The local ethics committee of Tehran University of Medical Sciences approved the study in accordance with Helsinki’s ethical principles (IR.TUMS.FARABIH.REC.1401.037).
Consent for publication
In the written informed consent form, patients gave us permission to publish their information without including their names.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Momeni, A., Asadigandomani, H., Jamalitootakani, M. et al. Faster referral and surgical intervention for rhegmatogenous retinal detachment during COVID-19: a comparison of pre- and during-pandemic cases. Sci Rep 15, 1699 (2025). https://doi.org/10.1038/s41598-025-86206-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-86206-5