Abstract
This study aimed to evaluate ocular surface temperature (OST) in post-COVID-19 patients with different degrees of fever via infrared thermal imaging. There were 16 participants (32 eyes) in the control group, 22 participants (44 eyes) in the moderate and low post-COVID-19 fever group (M & L fever group), and 18 participants (36 eyes) in the high post-COVID-19 fever group (H fever group). All participants underwent an ophthalmic slit lamp examination and ocular thermography. Among the control group, M & L fever group and H fever group, there were no significant differences in the upper eyelid temperature (UET), inner canthus temperature (ICT), outer canthus temperature (OCT), initial central corneal temperature (initial CCT), third-second central corneal temperature (3s-CCT), or sixth-second central corneal temperature (6s-CCT). However, the change in central corneal temperature measured within 1, 3, and 6 s (change in CCT within 1, 3, and 6 s) of the H fever group were significantly greater than those of the control group (0.15 ± 0.12 °C vs. 0.08 ± 0.09 °C, p = 0.007; 0.30 ± 0.22 °C vs. 0.17 ± 0.17 °C, p = 0.005; 0.45 ± 0.30 °C vs. 0.26 ± 0.23 °C, p = 0.004, respectively) and M & L fever group (0.15 ± 0.12 °C vs. 0.08 ± 0.08 °C, p = 0.008; 0.30 ± 0.22 °C vs. 0.16 ± 0.14 °C, p = 0.001; 0.45 ± 0.30 °C vs. 0.23 ± 0.20 °C, p < 0.001, respectively). To further investigate the relationship between OST and post-COVID-19 fever, we compared the OST of long recovery time (5 days < recovery time < 14 days; 9 patients, 18 eyes) and short recovery time (recovery time ≤ 5 days; 9 patients, 18 eyes) in the H fever group. We found that the 6s-CCT in the short recovery time group was significantly lower than that in the long recovery time group (32.43 ± 1.09 °C vs.33.10 ± 0.82 °C, p = 0.044). Additionally, the change in CCT within 1 s, 3 s, and 6 s in the short recovery time group were all significantly greater than those in the long recovery time group (0.19 ± 0.13 °C vs. 0.11 ± 0.10 °C, p = 0.048; 0.38 ± 0.24 °C vs. 0.22 ± 0.17 °C, p = 0.026; 0.58 ± 0.31 °C vs. 0.32 ± 0.24 °C, p = 0.016, respectively). In conclusion, the central corneal temperature (CCT) of patients who have an insufficient recovery time from COVID-19 infection or who exhibit severe infection symptoms could decrease faster when the eyes open. This may be due to dry eye disease.
Similar content being viewed by others
Introduction
The novel coronavirus, officially designated as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was initially discovered in December 2019 following a cluster of cases involving atypical pneumonia in Wuhan, China1. Subsequently, SARS-CoV-2 was rapidly transmitted around the world and escalated into a public health crisis, leading to its classification as a pandemic by the World Health Organization (WHO). Patients diagnosed with COVID-19 can exhibit a wide range of clinical symptoms, ranging from mild to severe respiratory and multiorgan failure. The most frequently observed symptoms include fever, cough, and difficulty breathing2. Several studies have investigated ocular symptoms since the COVID-19 pandemic, including conjunctivitis3,4,5,6,7, keratoconjunctivitis8, foreign body sensation, epiphora, dry eye, and blurred vision2,9.
Ocular thermography is a noncontact and nonintrusive temperature measurement technique. This technology has already been used in a variety of medical fields and has been widely used in the field of ophthalmology. This method has been employed for the examination of inflammatory conditions affecting the human lacrimal drainage system, dry eye disease, carotid artery stenosis, glaucoma, unilateral exophthalmos, Tolosa–Hunt syndrome, and ophthalmic postherpetic neuralgia10.
Some studies have suggested that individuals with a greater degree of pneumonia severity have an increased risk of ocular manifestations11 and that patients with elevated viral loads have an increased risk of ocular surface symptoms12. These findings suggest that the severity of COVID-19 may cause or exacerbate ocular surface symptoms to varying degrees. Moreover, ocular surface symptoms can be assessed through ocular surface temperature (OST). It remains unclear whether post-COVID-19 patients with different degrees of fever have different OSTs. Therefore, this study applied infrared thermal imaging to detect the ocular surface of post-COVID-19 patients and evaluated the OST of post-COVID-19 patients with different degrees of fever.
Methods
Study participants
This study was conducted in accordance with the guidelines outlined in the Declaration of Helsinki. Approval for the research was granted by the Ethics Committee of Xin Hua Hospital Affiliated to Shanghai Jiao Tong University School of Medicine (Approval No. XHEC-D-2023-047). Written informed consent was obtained from all individual participants (> 16 years) included in the study; Written informed consent was obtained from the parents of participants ( < = 16 years). The participants were 40 patients (80 eyes) who recovered from post-COVID-19 fever, and the time between when the body temperature returned to normal and the day of the examination was less than two weeks. In addition, 16 healthy individuals (32 eyes) were included in the control group. The participants underwent an ophthalmic slit lamp examination (slit-lamp examination, SL-3G, TOPCON Corporation, Japan) and ocular thermography (Xcore LT640, Iray Tech Co., Ltd., China) at Shanghai Xinhua Hospital between February 2023 and December 2023. According to the maximum fever temperature (armpit thermometry) measured during the COVID-19 fever, the 40 participants were divided into two groups. There were 22 participants (44 eyes) in the moderate and low post-COVID-19 fever group (M & L fever group), maximum fever temperature ≤ 39 °C and 18 participants (36 eyes) in the high post-COVID-19 fever group (H fever group), maximum fever temperature > 39 °C. For the study of the relationship between ocular surface temperature (OST) and recovery time (the time between when the body temperature returned to normal and the day of the examination) in the H fever group, we divided the participants into two groups based on their recovery time, long recovery time group (5 days < recovery time < 14 days; 9 patients, 18 eyes) and short recovery time group (recovery time ≤ 5 days; 9 patients, 18 eyes). The exclusion criteria were as follows: underwent refractive surgery or experienced ocular trauma in the past; underwent ophthalmic surgery within the previous year; wore contact lenses within the previous 3 months; had existing ocular surface conditions such as conjunctivitis, keratitis, pterygium; used topical medications such as lubricants or glaucoma eye drops. Individuals were also excluded if they had systemic disorders.
Ocular thermography
Thermal imaging data were collected via a longwave infrared thermal camera operating within the 8–14 μm wavelength range. The camera was configured to capture images and videos at a frame rate of 30 Hz, with a spatial resolution of 640 pixels × 512 pixels and a pixel size of 14 μm × 14 μm. The device boasted a measurement accuracy of ± 2%. Before the commencement of testing, we preheated the infrared thermal camera for 20 min via automatic nonuniformity correction with a correction interval of one minute. Additionally, each participant was instructed to rest for 10 min in the designated examination room. The environmental conditions within the room were closely monitored and maintained at a temperature of 22 ± 1 °C and a humidity level of 40 ± 5%. The data collection took place within the operational hours of the hospital, which spanned from 9:00 a.m. to 5:00 p.m. The procedure for measuring participants’ facial temperature involved the following steps. First, participants were required to maintain a stable head position via a chin rest and forehead rest, and were directed to focus on a fixed point. An infrared thermal camera was subsequently used to record the temperature of each participant’s forehead. The participants were subsequently instructed to close their eyes, after which the infrared thermal camera captured images of the upper eyelids of both eyes. Finally, the participants were asked to open their eyes, blink, and then keep their eyes open for 6 s while the infrared thermal camera recorded a video of either the left or right eye.
Data analysis
Image processing was carried out via custom MATLAB scripts developed by MathWorks, Inc. Mean temperatures were assessed at three specific sites: the forehead (Fig. 1A), upper eyelid (Fig. 1B), and ocular surface (Fig. 1C). The ocular surface was further divided into three regions of interest (ROIs), the central cornea, inner canthus, and outer canthus, with diameters of 5 mm, 2 mm, and 2 mm, respectively.
In the context of measuring the ocular surface, information was gathered once the eye was fully open and the upper eyelid had settled to accommodate the placement of three ROIs on the ocular surface without being obstructed by the lid or eyelashes. This was done to capture the earliest possible OSTs.
The change in central corneal temperature was assessed starting from the point at which the eye achieved adequate opening and the upper eyelid was no longer elevated to accommodate the placement of three ROIs on the ocular surface without any interference from the lid or eyelashes. A series of 13 infrared thermal images of the ocular surface were subsequently captured from the infrared thermal video at intervals of 0.5 s over 6 s for each eye, and the average temperature of the central cornea was determined at each instance. Consequently, the fluctuations in central corneal temperature (CCT) within the initial 6 s of eye opening were derived from infrared thermal images of the ocular surface. The alterations observed in the infrared thermal images of the ocular surface were not conspicuous in the control group and M & L fever group (Fig. 2A, B). In contrast, obvious changes were observed in the H fever group (Fig. 2C). The temperature scale ranges from 30 to 38 °C (Fig. 2D).
(A) Changes in the infrared thermal images of the ocular surface in the control group. (B) Changes in the infrared thermal images of the ocular surface in the moderate and low post-COVID-19 fever group (M & L fever group). (C) Changes in the infrared thermal images of the ocular surface in the high post-COVID-19 fever group (H fever group). (D) The temperature scale ranged from 30 to 38 °C.
Statistical analysis
Categorical variables are presented in terms of frequency rates and percentages, whereas continuous variables that followed a normal distribution were described via measures of central tendency, such as the means and standard deviations. Among the control group, M & L fever group, and H fever group, one-way analysis of variance (ANOVA) was used to identify differences in age, forehead temperature, body temperature, upper eyelid temperature (UET), inner canthus temperature (ICT), outer canthus temperature (OCT), initial central corneal temperature (initial CCT), first-second central corneal temperature (1s-CCT), third-second central corneal temperature (3s-CCT), sixth-second central corneal temperature (6s-CCT), change in central corneal temperature measured within 1 s (change in CCT within 1 s), change in central corneal temperature measured within 3 s (change in CCT within 3 s), and change in central corneal temperature measured within 6 s (change in CCT within 6 s) between groups with Tukey’s HSD (Honest Significant Difference) used in the case of ANOVA returning a significant result. Unpaired t-tests were employed to assess differences between the long recovery time group and the short recovery time group. Statistical analyses were carried out via SPSS version 22.0 software. A significance level of p < 0.05 (two-tailed) was deemed statistically significant.
Results
Participants and baseline characteristics
A total of 40 post-COVID-19 participants were enrolled, including 22 (44 eyes) patients in the M & L fever group and 18 (36 eyes) in the H fever group. In addition, 16 (32 eyes) healthy individuals were included in the control group. There were no significant differences in age (p = 0.138), forehead temperature (p = 0.465), or body temperature (p = 0.448), as shown in Table 1.
Upper eyelid temperature (UET) and ocular surface temperatures
All data are shown in Table 2; Fig. 3. Although the mean UET, ICT, OCT, and initial CCT in the H fever group were higher than those in the control group and M & L fever group. There were no significant differences were observed in UET (p = 0.177), ICT (p = 0.915), OCT (p = 0.652), or initial CCT (p = 0.925).
Comparison of upper eyelid temperature (UET), inner canthus temperature (ICT), outer canthus temperature (OCT), initial central corneal temperature (initial CCT) among the control group, moderate and low post-COVID-19 fever group (M & L fever group) and high post-COVID-19 fever group (H fever group).
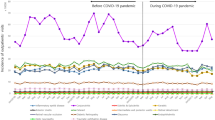
Changes in central corneal temperature measured within 6 s
No statistically significant differences were found in initial CCT (p = 0.925), 1s-CCT (p = 0.989), 3s-CCT (p = 0.929), or 6s-CCT (p = 0.812) among the control group, M & L fever group and H fever group. However, change in CCT within 1 s, change in CCT within 3 s, and change in CCT within 6 s of the H fever group were significantly greater than those of the control group (p = 0.007, p = 0.005, and p = 0.004, respectively) and M & L fever group (p = 0.008, p = 0.001, and p < 0.001, respectively). Detailed data can be found in Table 3; Figs. 4 and 5. The continuous change in central corneal temperature measured within 6 s is displayed in Fig. 6.
Comparison of initial central corneal temperature (initial CCT), first-second central corneal temperature (1s-CCT), third-second central corneal temperature (3s-CCT), sixth-second central corneal temperature (6s-CCT) among the control group, moderate and low post-COVID-19 fever group (M & L fever group) and high post-COVID-19 fever group (H fever group).
Comparison of the change in central corneal temperature measured within 1, 3, and 6 s (change in CCT within 1, 3, and 6 s) among the control group, moderate and low post-COVID-19 fever group (M & L fever group) and high post-COVID-19 fever group (H fever group). **P < 0.01 (Tukey’s HSD), ***P < 0.001 (Tukey’s HSD).
Ocular surface temperature of long recovery time and short recovery time in the high post-COVID-19 fever group
There were no significant differences in UET, ICT, OCT, initial CCT, 1s-CCT, and 3s-CCT between the short recovery time group and the long recovery time group (p = 0.984, p = 0.276, p = 0.061, p = 0.108, p = 0.074, and p = 0.056, respectively). However, the 6s-CCT in the short recovery time group was significantly lower than that in the long recovery time group (p = 0.044). The change in CCT within 1 s, 3 s, and 6 s in the short recovery time group were all greater than those in the long recovery time group, with significant differences (p = 0.048, p = 0.026, and p = 0.016, respectively). Detailed comparisons can be found in Table 4.
Discussion
Among the control group, moderate and low post-COVID-19 fever group (M & L fever group) and high post-COVID-19 fever group (H fever group), there were no significant differences in the upper eyelid temperature (UET), inner canthus temperature (ICT), outer canthus temperature (OCT), and initial central corneal temperature (initial CCT). The findings are inconsistent with our initial assumption. There are two primary factors to consider. First, this study specifically excluded patients diagnosed with conjunctivitis and keratitis, resulting in the absence of significant conjunctival hyperemia among the participants. Second, during ocular thermography, the eyes open, which facilitates evaporation of the tear film and consequently leads to a decrease in the ocular surface temperature (OST). Additionally, the thermal energy from the ocular surface is transferred to the cooler surrounding environment13,14. The initial OST must be captured at the moment the eyes are opened, which demands highly sensitive equipment.
No statistically significant differences were found in initial CCT, first-second central corneal temperature (1s-CCT), third-second central corneal temperature (3s-CCT), or sixth-second central corneal temperature (6s-CCT) among the control group, M & L fever group, and H fever group. However, the change in central corneal temperature measured within 1, 3, and 6 s (change in CCT within 1, 3, and 6 s) of the H fever group were significantly greater than those of the control group and M & L fever group. It means that when the eyes are opened, the CCT of the H fever group decreased faster than that of the control group and M & L fever group. This is the most interesting finding of this study. A faster decrease in the CCT indicates faster evaporation of the tear film15,16. Mapstone posits that the thermodynamic processes related to the ocular surface can be understood through the principles of convection, radiation, and evaporation. In particular, airflow over a surface facilitates heat loss through convection, whereas radiant heat loss occurs when thermal energy is transferred to cooler ambient temperatures13. When the eye is open and the tear film evaporates, the ocular surface experiences a reduction in temperature. This cooling effect is attributed to the positive latent heat of vaporization, which involves the dissipation of heat into the surrounding environment during the phase transition from liquid to gas14. The literature suggests that individuals with dry eye disease (DED) experience a more rapid cooling rate of the ocular surface than do individuals with normal ocular conditions. This phenomenon is presumed to be attributable to an increased rate of tear film evaporation14,15,17,18,19. Moreover, some studies have examined the impact of COVID-19 on dry eyes6,12,20,21. Therefore, individuals in the H fever group could experience DED, especially those with evaporative dry eyes (EDEs). Nevertheless, the relationship between DED and COVID-19 infection has not been definitively established. COVID-19 can lead to meibomian gland dysfunction12, a temporary disruption in the microbial community of the eye resulting from viral infection22, ocular surface viral infection23 or the interaction of the virus with the ocular surface, thus triggering an immune-mediated response that exacerbates and disrupts the balance of tear film homeostasis24. Wearing face masks for extended periods could be associated with dry eyes25,26,27. Prolonged eye use20 and affective interference21,28 were also found to aggravate dry eyes during the COVID-19 era. There could be additional factors contributing to this situation.
To further investigate the relationship between OST and post-COVID-19 fever, we compared the OST of long recovery time and short recovery time in the H fever group. We found that the 6s-CCT in the short recovery time group was significantly lower than that in the long recovery time group. Additionally, the change in CCT within 1 s, 3 s, and 6 s in the short recovery time group were all greater than those in the long recovery time group, and there were significant differences. This means that as the recovery time from COVID-19 fever becomes sufficient, the change in CCT after opening the eyes decreases and dry eye symptoms alleviate. In other words, during the phase of COVID-19 fever and for some time afterward, the symptoms of dry eye may occur or worsen. This is because the onset of dry eye is multifactorial29,30. Infection with the COVID-19 virus can lead to varying degrees of symptoms throughout the body, including the eyes11,12. As the body recovers from the infection, the eye symptoms gradually improve, and the symptoms of dry eye also alleviate.
This study has several limitations and areas for further research. First, only infrared thermography was used to detect dry eye symptoms in this study. Using other established dry eye diagnostic tests, such as the measurement of the tear film breakup time (TBUT), simultaneously to validate findings can strengthen the study’s findings. Second, in this study, the mean age of the participants was relatively high. If this study was expanded to middle-aged individuals or children, it could reveal differences in OST caused by COVID-19 infection among different age groups. Third, the study included 56 participants, which is a small sample size, and collected data from both eyes, which may have led to biased statistical results. Fourth, this study did not collect data on viral loads; therefore, we were unable to examine the correlation between viral loads and OST. If viral loads are associated with OSTs, this could elucidate whether viral factors directly influence ocular symptoms.
Conclusion
In conclusion, the central corneal temperature (CCT) of patients who have an insufficient recovery time from COVID-19 infection or who exhibit severe infection symptoms could decrease faster when the eyes open. This may be due to dry eye disease.
Data availability
The datasets used during the current study could be available from the corresponding author on reasonable request.
References
Zhu, N. et al. A novel coronavirus from patients with Pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733 (2020).
Meduri, A. et al. Ocular surface manifestation of COVID-19 and tear film analysis. Sci. Rep. 10, 20178 (2020).
Daruich, A., Martin, D. & Bremond-Gignac, D. Unilateral conjunctivitis as first presentation of Coronavirus Disease 2019 (COVID-19): a telemedicine diagnosis. J. Fr. Ophtalmol. 43, e167–e168 (2020).
Khavandi, S., Tabibzadeh, E., Naderan, M. & Shoar, S. Corona virus disease-19 (COVID-19) presenting as conjunctivitis: atypically high-risk during a pandemic. Contact Lens Anterior Eye. 43, 211–212 (2020).
Zhou, Y. et al. Ocular findings and proportion with Conjunctival SARS-COV-2 in COVID-19 patients. Ophthalmology 127, 982–983 (2020).
Hong, N. et al. Evaluation of ocular symptoms and tropism of SARS-CoV‐2 in patients confirmed with COVID‐19. Acta Ophthalmol. 98, (2020).
Wu, P. et al. Characteristics of ocular findings of patients with Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 138, 575 (2020).
Cheema, M. et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID-19). Can. J. Ophthalmol. 55, e125–e129 (2020).
Ho, D. et al. COVID-19 and the ocular surface: a review of transmission and manifestations. Ocul Immunol. Inflamm. 28, 726–734 (2020).
Tan, J. H., Ng, E. Y. K., Rajendra Acharya, U. & Chee, C. Infrared thermography on ocular surface temperature: a review. Infrared Phys. Technol. 52, 97–108 (2009).
Chen, Y. Y., Yen, Y. F., Huang, L. Y. & Chou, P. Manifestations and Virus Detection in the Ocular Surface of Adult COVID-19 Patients: A Meta-Analysis. J Ophthalmol 1–12 (2021). (2021).
Wan, K. H. et al. Ocular surface disturbance in patients after acute COVID-19. Clin. Exp. Ophthalmol. 50, 398–406 (2022).
Mapstone, R. Determinants of corneal temperature. Br. J. Ophthalmol. 52, 729–741 (1968).
Craig, J. P., Singh, I., Tomlinson, A., Morgan, P. B. & Efron, N. The role of tear physiology in ocular surface temperature. Eye 14, 635–641 (2000).
Kamao, T. et al. Screening for Dry Eye with newly developed ocular surface Thermographer. Am. J. Ophthalmol. 151, 782–791e1 (2011).
Abreau, K. et al. Temperatures of the ocular surface, lid, and Periorbital Regions of Sjögren’s, Evaporative, and aqueous-deficient dry eyes relative to normals. Ocul Surf. 14, 64–73 (2016).
Fujishima, H., Toda, I., Yamada, M., Sato, N. & Tsubota, K. Corneal temperature in patients with dry eye evaluated by infrared radiation thermometry. Br. J. Ophthalmol. 80, 29–32 (1996).
Su, T. Y. et al. Noncontact detection of dry eye using a custom designed infrared thermal image system. J. Biomed. Opt. 16, 046009 (2011).
Wolffsohn, J. S. et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 15, 539–574 (2017).
Giannaccare, G., Vaccaro, S., Mancini, A. & Scorcia, V. Dry eye in the COVID-19 era: how the measures for controlling pandemic might harm ocular surface. Graefe’s Arch. Clin. Exp. Ophthalmol. 258, 2567–2568 (2020).
Koh, S. & Rhee, M. K. COVID-19 and dry eye. Eye Contact Lens: Sci. Clin. Pract. 47, 317–322 (2021).
Borroni, D. et al. Metagenomics in ophthalmology: current findings and future prospectives. BMJ Open. Ophthalmol. 4, e000248 (2019).
Alves, M., Angerami, R. N. & Rocha, E. M. Dry eye disease caused by viral infection: review. Arq. Bras. Oftalmol. 76, 129–132 (2013).
Sánchez-González, M. C., Sánchez-González, J. M. & De-Hita-Cantalejo, C. Ocular surface impairment after coronavirus disease 2019: a cohort study. Cornea 41, e1–e1 (2022).
Moshirfar, M., West, W. B. & Marx, D. P. Face Mask-Associated Ocular Irritation and Dryness. Ophthalmol. Ther. 9, 397–400 (2020).
Boccardo, L. Self-reported symptoms of mask-associated dry eye: a survey study of 3,605 people. Contact Lens Anterior Eye. 45, 101408 (2022).
Hadayer, A. et al. Retina 40, 1651–1656 (2020).
Hallak, J. A., Jassim, S., Khanolkar, V. & Jain, S. Symptom burden of patients with dry eye disease: a four ___domain analysis. PLoS One. 8, e82805 (2013).
Bron, A. J. et al. TFOS DEWS II pathophysiology report. Ocul Surf. 15, 438–510 (2017).
Shimazaki, J. Definition and diagnostic criteria of Dry Eye Disease: historical overview and future directions. Investig. Opthalmol. Visual Sci. 59, DES7 (2018).
Author information
Authors and Affiliations
Contributions
B.L., S.Z. and Z.G. participated in the study design. C.W. collected the data. Y.H. provided technical support. B.X. participated in the analysis of data. Z.G. participated in the clinical management of the patients enrolled in the study. C.W. wrote the main manuscript text and created the tables. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, C., Li, B., Huang, Y. et al. Evaluation of ocular surface temperature in post-COVID-19 patients with different degrees of fever via infrared thermal imaging. Sci Rep 15, 2273 (2025). https://doi.org/10.1038/s41598-025-86407-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-86407-y