Abstract
Persistence of high-risk Human papillomaviruses (HR-HPV) infection increases the risk of precancerous lesions development. The aim of this study was to assess the persistence and clearance rate of HPV infection. A prospective cohort study was conducted between January and December 2023 among patients attending gynecology unit of FHCSH in Bahir Dar, northwest Ethiopia. Out of 297 study participants, 95 women with HPV infected and cytological abnormalities were followed; of these 93.7% were HPV positive at the baseline study. Of which, 46.1% did not receive treatment, the rest 53.9% were treated. Among the women without treatment, HPV persistence and clearance rates were 65.9% and 34.1% respectively while persistence rate of 46.3% and clearance rate of 53.7% were observed in 12-month follow up period. Among women who received treatment, HPV persistence rate of 45.8% and clearance rate of 54.2% were recorded in six while persistence rate of 33.3% and clearance rate of 66.7% were observed in 12- month follow up period. The findings of our study indicated that the high persistence rate and low clearance rate of HPV infection. Detection of persistent HPV infection without treatment or after treatment should be considered as the main risk factor for the development or recurrence of cervical neoplasia.
Similar content being viewed by others
Introduction
Infections of Human papillomaviruses (HPVs) frequently spread through sexual contact. These viruses have the ability to infect squamous epithelial cells found in the skin and mucosa1,2. These viruses, including 40 human infecting different varieties, can lead to cervical cancer by infecting the mucous membranes lining the uterus and transforming neighboring cells into malignant ones3. Although most cervical HPV infections are transient, some people experience persistent HPV infections. In middle-aged women, persistent high risk (HR) HPV, infection is strongly linked to both precancerous lesions and cervical cancer. Persistent HPV infections are those that result in positive findings from two consecutive HPV tests that are spaced at least six months apart4.
Cervical intraepithelial neoplasia (CIN) is a protracted phase of cytological alterations that typically precedes cervical cancer and takes 15 to 20 years before the invasive carcinoma manifests. Therefore, if cellular alterations are identified and treated at an early stage, cervical cancer can be prevented5. With appropriate follow-up and treatment, premalignant lesions can be treated to prevent them from developing into in-situ or invasive cancer6.
The recommended therapy for high-grade cervical intraepithelial neoplasia (CIN) based on histological diagnosis is ablative or excisional treatment to stop the disease’s development to cervical cancer. But even after excisional surgeries, 10–53% of women may still have the disease7.
In most industrialized nations where timely treatment, high-quality screening, and follow-up care services are consistently provided, cervical cancer rates have decreased8. The bulk of cases and fatalities occur in low- and middle-income countries (LMICs), where progress in reducing incidence and mortality has been poor. Several countries have reported rises in incidence or mortality rates in the last ten years9,10.
Precancerous lesions and cervical cancer are mostly caused by persistent infections with specific types of the high-risk human papillomavirus11,12. Most HPV-infected women typically clear the virus within 6–12 months, while the likelihood and time-to-viral clearance may vary depending on factors such as the women’s age, HPV type, sexual behavior, and treatment status at baseline13.
About 70% of HPV infections resolve spontaneously within one year, and 90% in two years; the virus still exists in the remaining cases. An efficient cell-mediated immune response is necessary for HPV elimination. As a result, HIV-positive people who contract HPV are more likely to develop benign warts and malignant tumors because they are less likely to clear the infections between one and two years14.
Currently, our understanding of the natural history, carcinogenic characteristics, screening, and preventative strategies of HPV infection is comparatively clear. Nonetheless, HPV infection rates are high, particularly in underdeveloped nations where the incidence and prevalence of cervical cancer are still high. Low socioeconomic standing, a lack of population knowledge, and poorly executed screening and immunization programs are some of the causes15.
Prior research has demonstrated that regional and national differences in HPV incidence, persistence, and clearance16. The aim of this study was to assess the persistence and clearance rate of HPV infection among women who received treatment and not treated for cervical dysplasia.
Results
In this study, a total of 324 study participants were enrolled in the study but 27 of them had insufficient PAP smears and they were excluded from the study, the rest 297 were included, HPV DNA or VIA or PAP positive or CIN II+women (113/297) from the baseline assessment were included in the follow up study, of which 18/113 women (15.93%) were lost during follow up. The major reason to follow up was change of contact details which made the patients to be unreachable, referred to an oncology center for advanced treatment and death. A total of 95 women were followed, 89/95 was HPV positive in the baseline study. Of which 41/89 were not treated due to only HPV positive, LSIL for PAP and VIA positive but not eligible for treatment according to the WHO classification. However, the rest 48/89 women were treated. Majority of study participants (75.3%; 67/89) were age between 30 and 50 years old. The details of socio-demographic, sexual and reproductive characteristics are presented in Table 1.
HPV persistent rate and clearance rate among non-treatment group
Among the non-treatment group, HPV persistence rate of 65.9% (27/41) and clearance rate of 34.1% (14/41) were recorded in 6 month follow up time at (95% CI 0.190–0.493, P < 0.001) while persistence rate of 46.3% (19/41) and clearance rate of 53.7% (22/41) were observed in 12 month follow up period at (95% CI: 0.377–0.696, P < 0.001).
HPV-16 had high persistent rate 92.31%(12/13) among women who were not treated in 6 month follow up period, and its clearance rate was 7.69%(1/13), and at 12 month follow up period, the persistent rate of 76.92%(10/13) and clearance rate of 23.08%(3/13) were recorded at (95% CI:0.034-0.496, P = 0.082). The persistent rate of multiple infection was 84.6%(11/13) at 6 month follow up, were higher than the persistent rate of single infection (57.1%(16/28). The persistent rate of multiple infection at 12 month was 76.9%(10/13) which was also higher than the persistent rate of single infection(32.1%(9/28)). The details are presented in Tables 2 and 3.
HPV persistence rate and clearance rate among treatment group
Among women who received treatment, persistence rate of 45.8% (22/48) and clearance rate of 54.2% (26/48) were observed in 6 month follow up period at (95% CI: 0.395–0.688), P < 0.001), persistence rate of 33.3% (16/48) and clearance rate of 66.7% (32/48) were observed in 12 month follow up period at (95% CI: 0.1528–0.805), P < 0.001).
At 6 month follow up period after treatment, other high risk HPVs (HPV-31/33/39/45/51/56/59/66/68) had the highest persistence rate of 66.67%(6/9) and low clearance rate of 33.33%(3/9) with (95%CI: -0.51-0.718, P = 0.081), followed by HPV-52, HPV-18 and HPV-16 with persistent rate of 62.5%(5/8), 55.59%(5/9), 51.85%(14/27) and clearance rate of 37.5%(3/8) with (95%CI:0.058–0.808, P = 0.081), 44.44%(4/6) with (95%CI:0.039–0.850, P = 0.035) and 48.15%(13/27) at (95% CI: 0.280–0.683, P < 0.001).
At 12 month follow up period after treatment, HPV-18 had the highest persistent rate of 44.44%(4/9) and clearance rate of 55.56%(5/9) with (95%CI: 0.150–0.961, P = 0.013), followed by other high risk HPVs, HPV-16 and HPV58 with persistence rate of 44.44%(4/9), 40.74%(11/27), 30%(3/10) and clearance rate of 55.56%(5/9) with (95%CI: 0.150–0.961, P = 0.013), 59.26%(16/27) with (95%CI:0.359–0.791, P < 0.001), and 70%(7/10) with (95% CI:0.354–1.046, P < 0.001).
The persistent rate of multiple infection was 61.1%(11/18)at 6 month follow up, were higher than the persistent rate of single infection 36.7%(11/30). The persistent rate of multiple infection at 12 month was 38.8%(7/18) which was also higher than the persistent rate of single infection(30%(9/30)). The details are presented in Tables 4 and 5.
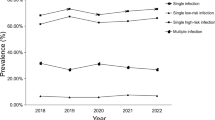
Comparison of HPV persistent infection rate between treatment and non-treatment group
The rate of persistence shows some differences between treatment group and non-treatment group. At 12 month, the persistent rate of high and probable high risk genotypes in treatment group was 33.33%, whereas the persistent rate of non-treatment group was 46.34% (Fig. 1). At 12 month, the persistent rate of possible and low risk genotypes in treatment group was 30%, whereas the persistent rate of non-treatment group was 47.62% (Fig. 2).
Discussion
To our knowledge, the present study is the first to examine the persistence and clearance rate of HPV infection in women who received treatment and untreated for cervical dysplasia. HPV positive women in the baseline study were followed for one year with a six month interval. Persistent infection of HPV will lead to development of precancerous lesions and cervical cancer. Since women treated for cervical cancer and precancerous lesions are at risk of disease recurrence, monitoring of HPV infection at follow-up is crucial. The objective of the current prospective study was to determine the persistence rate and clearance rate of HPV infection at six and twelve months among women without treatment and women who received treatment.
In the present study, among women without treatment, persistence rate of 65.9% and clearance rate of 34.1% were recorded in 6 month follow up period, persistence rate of 46.3% (19/41) and clearance rate of 53.7% (22/41) were observed in 12 month follow up period. This finding is consistent with a study conducted in Zimbabwe, which found that the rates of persistence and clearance were 34.6% and 65.4%, respectively17, . Our results also almost similar to a Ugandan study that found 31.2% of women completely clearing their infections18.
However our finding is low compared to a Brazilian study that found 40.4% and 59.6% of women, respectively, experienced viral infection clearance or persistence19. A Chinese study reported that, of 298 HPV-positive patients with CIN1 or normal cervical histology at baseline, 120 (40.26%) had persistent infection whereas 178 (59.74%) cleared their infection after a year20. The observed difference might be attributed to variations in the studies’ follow-up periods, sample sizes, and recruitment of women with normal and cervical squamous intraepithelial lesions (SILs).
In the current study, HPV-16 had high persistent rate of (92.31%; 12/13) among women without treatment in six- month follow up whereas its clearance rate was low (7.69%; 1/13). However at 12 month follow up, the persistence rate was 76.92%(10/13) while clearance rate was 23.08%(3/13). HPV-52 had by persistent rate of 75%(3/4) and clearance rate of 25%(1/4). HPV 18 had persistent rate of 57.14%(4/7) and clearance rate of 42.9%(3/7) at 12 month follow up period comparable with a Zimbabwean study which indicated HPV-16 was the most persistent type (53.8%), HPV-52 was the second most persistent type17.
In this study, among women who were treated, persistence rate of 45.8% (22/48) and clearance rate of 54.2% (26/48) were recorded in 6 month follow up period., persistence rate of 33.3% (16/48) and clearance rate of 66.7% (32/48) were observed in 12 months, highly consistent with a Korean study indicated that following cold knife conization or loop electrosurgical excision treatment, fifty-eight patients (33.7%) had HPV infection17. This result is also consistent with findings from other Korean studies that indicate from 398 patients, 28 (30.2%) had persistence after conization or Loop electrosurgical excision procedure (LEEP)21, and 48 (30%) had persistent HR HPV infections and 112 (70.7%) had HPV cleared following therapy22. However, this result is greater than that of an Italian study that found 96 individuals (23.5%) continued to have at least one genotype following therapy23.
In the present study, HPV-18 had the highest persistent rate 44.44%(4/9) among treated women in 12 month follow up and its clearance rate was 55.56%(5/9), followed by other high risk HPVs, HPV-16 and HPV58 with persistent rate of 44.44%(4/9), 40.74%(11/27), 30%(3/10) and clearance rate of 55.56%(5/9), 59.26%(16/27), and 70%(7/10), similar with a Turkish study which indicated HPV-18 was cleared in almost all (95.8%) cases, followed by HPV 16 (69.9%) and other HR HPV types (65.6%)7. However other studies found that the persistent infection rate for HPV-16 was higher than that of other HPV strains17,24,25.
In our study, the persistent rate had decreased from six month to twelve month in both women who were not treated (from 65.9 to 46.34%) and women who were treated (from 45.83 to 33.33%). This result is supported by a systematic review by Hoffman et al.26 which reported that median HPV persistence tended to decline over time: 27% at three-month, 21% at six-month and 10% at 24 -month after treatment. Additionally, they stated that a variety of factors, including the patient’s age, the type of HPV, the method of detection, the course of treatment, and the minimum interval between HPV post-treatment tests, affected the persistence of post-treatment HPV. The result of the current study indicted there is a need to follow HPV positive women for the persistent infection and development of cervical abnormalities or recurrence of cervical neoplasia, which is supported by a study conducted in the United States that found women with persistent HPV infection had a higher risk of developing abnormalities in their epithelial cells27.
Conclusion
Our study contributes to the knowledge of persistence rate and clearance rate of HPV infection among women who received treatment and untreated for cervical dysplasia. There were high persistence rate and low clearance rate of HPV infection among women who received treatment and untreated for cervical dysplasia in Amhara regional state. Detection of persistent HPV infection among women who received treatment and untreated for cervical dysplasia should be considered as the main risk factor for the development or recurrence of cervical neoplasia. Our results confirmed the clinical impact of HPV genotyping for more frequent follow up and on management and post-treatment surveillance of cervical neoplasia. Further larger-scale with longer period studies with minimum interval between HPV tests are necessary for the better understanding of the persistence rate and clearance rate of HPV infections and development or recurrence of precancerous lesions and cervical cancer.
Methods
Study setting and population
A prospective cohort study was conducted among patients attending gynecology unit of FHCSH in Bahir Dar, northwest Ethiopia, between January and December 2023. A total of 297 women were enrolled in the study. All study participants were screened with Visual Acetic Acid (VIA) test, genotyping of the HPV DNA and cervical cytology examination with PAP test. Study participants with positive results from the screening tests were examined with colposcopy and biopsy was taken for histopathology. Two follow-up visits were scheduled at 6 and 12 months after the baseline visit. After the result of baseline diagnosis, a total of 95 of 297women were followed, 89/95 were HPV positive in the baseline study, were followed for persistence and clearance of HPV infection at 6 and 12 month period.
Study population
The study population was all women of age above 30 and HIV positive women with all age range who visited FHCSH Gynecological unit and suspected for cervical cancer.
Sample size determination
Study one: A single population proportion sample size determination formula (study population size less than 10,000 32) was used with the assumption of 19% proportion of, 5% margin of error, and 95% desired level of confidence interval and considering a 10% non- response rate, the sample size was 281.
Study two: Sample size was determined from formulation of sensitivity and specificity test using Power Analysis and Sample Size (PASS) software based on desired type I error, power and effect size 33. The minimum sample size was determined by taking the prevalence of a disease 19%, by assuming sensitivity of the kit is comparable with the gold standard, and specificity of the kit is greater than 70%, the power is set to be at least 80% and the p-value, is set to be less than 0.05. The sample size for sensitivity and specificity of Onco E6 performance study was 49 positive for histopathology, 196 negative samples with the gold standard histopathology examination and 49 negative controls. By taking 10% contingency, the sample size was 324. The final sample size was the highest sample size of the upper studies, 324 sample size was determined for this study.
Sampling technique and procedure
The sampling technique was systematic random sampling. Every third study participants was selected after a random starting study participant who was selected by lottery method.
Follow up visits
All study participants were screened with Visual acetic acid test (VIA), genotyping of the HPV DNA test and cervical cytology examination with PAP test. Study participants with positive results from screening tests were examined with colposcopy and biopsy was taken for histopathology. Participants with positive results of the screening or diagnostic tests were followed. Two follow-up visits were scheduled 6 and 12 months after the baseline visit. Women with positive results for VIA, PAP smear and histopathology were treated with thermocoagulation, Loop Electrosurgical Excision Procedure (LEEP) and cryotherapy.
Specimen collection
Data were collected at three time points during the study: baseline, 6-month follow-up and 12-month follow-up. At the baseline visit, upon arrival at the cervical cancer unit, trained gynecologists currently working on cervical cancer unit conducted physical and gynecological examination, screen with VIA and collect swab for HPV DNA test, smear for cytologic specimens. Tissue biopsy was collected for all positive study participants from the screening tests when there were positive results of colposcopic impression. Swab specimens were collected using PreservCyt solution (Halogic.Inc., Marlborough MA, USA) following the manufacturer’s instructions for collecting and handling cervical specimens in preservCyt solution. The study procedures were explained to each study participants and written informed consent was obtained from those who agreed to participate. Treatment was given for women with positive for VIA or HSIL+ for PAP or CIN II+ for histopathology.
HPV genotyping and histopathology examinations
HPV genotyping was performed to detect high-risk HPV DNA in cervical swabs. DNA extraction, amplification and HR-HPV partial genotyping was performed using the Abbott Real Time HR-HPV assay (Abbott Molecular, Des Plaines, IL, USA). This is an automated process that uses micro beads technology for DNA extraction. The assay is a qualitative in-vitro test that amplifies and detects HR-HPV DNA in cervical cells. Detection of all 14 h-HPV genotypes (HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68) was achieved through a primer mix targeting the conserved L1 region of HR-HPV genomes and single stranded DNA probes28.Then extended genotyping was performed by Anyplex™ II PCR System to detect human papillomavirus DNA in cervical swabs, based on a real-time multiplex PCR assay that allows simultaneous amplification, detection, and differentiation of target nucleic acids of 19 high-risk HPV types (-16, -18, -26, -31, -33, -35, -39, -45, -51, -52, -53, -56, -58, -59, -66, -68, -69, -73, -82) and 9 low-risk HPV types (-6, -11, -40, -42, -43, -44, -54, -61, -70)29.
Biopsies were independently examined by two experienced pathologists. When the diagnosis differed between the two pathologists, the sample was reviewed by a third pathologist and consensus obtained. Histo-pathological diagnosis had confirmed test results as Negative for Dysplasia/malignancy, CIN I, CIN II, CIN III, and cervical cancer cases.
Statistical analysis
Statistical analyses were performed using SPSS version 26.0. Descriptive statistics such as frequency and cross tabulation were performed to summarize the data. Proportion difference at six and twelve months from baseline proportion was analyzed for persistent and clearance of infection. Persistent infection was defined as positive test results for specific HPV genotype detected at 6 months and 12 months tests. Clearance of HPV infection was defined as the first negative test result at any follow-up after a baseline positive test result for the specific genotype. HPV persistence and clearance rates were calculated for individual HPV types. Proportion was calculated using Z-test. Crude Odds Ratio (COR) and Adjusted Odds Ratio (AOR) at 95% confidence interval were calculated to assess the degree of association between the odds of persistence and clearance rate of specific HPV type among women who received treatment and the odds of persistence and clearance rate of specific HPV type among women who did not receive treatment (Considered as reference category in logistic regression). Finally, variables with a p-value of less than 0.05 were considered statistically significant.
Data availability
All the generated data in this article are included in the manuscript. Theoriginal data can be obtained from the principal investigator upon request. Alemayehu Abate [email protected].
Abbreviations
- DNA:
-
Deoxyribonucleic acid
- HPV:
-
Human Papilloma virus
- HR-HPV:
-
High-risk human Papilloma virus
- CI:
-
Confidence interval
- STIs:
-
Sexually transmitted Infections
- CIN:
-
Cervical intraepithelial neoplasia
- ICC:
-
Invasive cervical cancer
- PCR:
-
Polymerase chain reaction
References
Singh, S., Ahmad, S., Srivastava, A. N. & Misra, J. S. A review on role of Human Papilloma Virus (HPV) in health-related diseases. Adv Med., Dent Heal Sci. 3(3), 34–40 (2020).
Fiorillo, L. et al. Human Papilloma Virus: Current Knowledge and Focus on Oral Health (BioMed Research International. Hindawi Limited, 2021).
Hadi, A. A. M. et al. J. Water Res. 1(1), 65 (2023).
Qiao, Y., Wang, A., Fang, L. & Wang, L. Gynecology and Obstetrics Clinical Medicine incidence of persistent and high-risk human papillomavirus infection and associated factors among HIV-positive women in China. Gynecol. Obstet. Clin. Med. [Internet]. 1(3), 130–137 (2021).
Rampuria, S. & Chandwaskar, N. Comparative study of PAP smear and colposcopy with cervical biopsy. Int. J. Reprod. Contracept. Obstet. Gynecol. 12(7), 2113–2118 (2023).
Cemil Oğlak, S. & Obut, M. Comparison of pap-smear and colposcopy in the absence of HPV test for the diagnosis of premalignant and malignant cervical lesions. East. J. Med. 25(2), 299–304 (2020).
Kilic, D. et al. Predictors of human papillomavirus (HPV) persistence after treatment of high grade cervical lesions; does cervical cytology have any prognostic value in primary HPV screening? Ann. Diagn. Pathol. 49. (2020).
Niyodusenga, A., Musoni, E. & Niyonsaba, S. Comparative study of pap smear test and VIA test in cervical carcinoma screening among women aged over 20 years. Rwanda J. Med. Heal Sci. 3(1), 21–29 (2020).
Singh, D. et al. Global estimates of incidence and mortality of cervical cancer in 2020: A baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob Heal. 11(2), e197–206 (2023).
Hull, R. et al. Cervical cancer in low and middle income countries (review). Oncol. Lett. 20(3), 2058–2074 (2020).
Su, P., Ma, J., Yu, L., Tang, S. & Sun, P. Clinical Significance of Extended high-risk Human Papillomavirus Genotyping and Viral load in Cervical cancer and Precancerous Lesions Vol. 3p. 22–29 (KeAi Communications Co., 2023). Gynecology and Obstetrics Clinical Medicine.
Okunade, K. S. Human papillomavirus and cervical cancer. J. Obstet. Gynaecol. (Lahore) 40(5), 602–608. https://doi.org/10.1080/01443615.2019.1634030 (2020)
Akaaboune, M. et al. Clearance and persistence of the human papillomavirus infection among Cameroonian women. Women’s Heal 14, (2018).
Adebamowo, S. N. et al. Genome-wide association study of prevalent and persistent cervical high-risk human papillomavirus (HPV) infection. 1–10. (2020).
Chan, C. K., Aimagambetova, G., Ukybassova, T., Kongrtay, K. & Azizan, A. Human Papillomavirus infection and cervical cancer: Epidemiology, screening, and vaccination - review of current perspectives. J. Oncol. (2019).
Li, M. et al. Incidence, persistence and clearance of cervical human papillomavirus among women in Guangdong, China 2007–2018: A retrospective cohort study. J. Infect. Public. Health. 14(1), 42–49 (2021).
Chibvongodze, R., Dupwa, T., Muchiri, L. & Nyirakanani, C. Persistence and clearance patterns of cervical high risk human papillomavirus (Hr-HPV) infections in women with negative cytology results in Harare, Zimbabwe. Int. J. Clin. Obstet. Gynaecol. 5(4), 166–169 (2021).
Banura, C. et al. Type-specific incidence, clearance and predictors of cervical human papillomavirus infections (HPV) among young women: A prospective study in Uganda. Infect. Agent Cancer 5(1) (2010).
Miranda, P. M. et al. Persistence or clearance of human papillomavirus infections in women in Ouro Preto, Brazil. Biomed. Res. Int. (2013).
Tuerxun, G., Abudurexiti, G. & Abulizi, G. Prevalence, persistence, clearance and risk factors for HPV infection in rural Uyghur women in China. BMC Womens Health 23(1), (2023).
Ouh, Y. T. et al. Risk factors for type-specific persistence of high-risk human papillomavirus and residual/recurrent cervical intraepithelial neoplasia after surgical treatment. Obstet. Gynecol. Sci. 63(5), 631–642 (2020).
So, K. A., Lee, I. H., Kim, T. J. & Lee, K. H. Risk factors of persistent HPV infection after treatment for high-grade squamous intraepithelial lesion. Arch. Gynecol. Obstet. 299(1), 223–227 (2019).
Daniela Iacobone, A. et al. Human Papillomavirus Same Genotype Persistence and Risk of Cervical Intraepithelial Neoplasia2 + Recurrence. https://doi.org/10.3390/cancers13153664 (2021).
Zhang, Y., Ni, Z., Wei, T. & Liu, Q. Persistent HPV infection after conization of cervical intraepithelial neoplasia—A systematic review and meta-analysis. BMC Womens Health 23(1), (2023).
Bruno, M. T., Cassaro, N., Garofalo, S. & Boemi, S. HPV16 persistent infection and recurrent disease after LEEP. Virol. J. 16(1), (2019).
Hoffman, S. R. et al. Patterns of persistent HPV infection after treatment for cervical intraepithelial neoplasia (CIN): A systematic review. 23, 8–23 (2017).
Shanmugasundaram, S. & You, J. Targeting persistent human papillomavirus infection. Viruses 9(8), (2017).
Rantshabeng, P., Kasvosve, I., Ndlovu, A., Gaseitsiwe, S. & Moyo, S. Prevalence of high-risk human papilloma virus in women with high-grade squamous cell intraepithelial lesions in Botswana using Abbott RealTime HPV assay. PLoS One. 14(1), 1–9 (2019).
Id, I. B., Romundstad, P. R., Eide, M. L. & Jonassen, C. M. Clinical performance of Anyplex II HPV28 by human papillomavirus type and viral load in a referral population, 1–15 (2019).
Funding
No funding was given to support this study.
Author information
Authors and Affiliations
Contributions
The corresponding author (A.A.) was involved in the conception, design, drafted the present manuscript and data analysis. All authors (A.A., A.M., E.N., M.A., A.Mu., A.M., A.Ab., D.H.A. and A.A.l) were involved in analysis and interpretation of data. A.A. (corresponding author), A.M., E.N., A.mu., M.A. and A.Mu. have been involved in critically revising the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from Institutional Review Board (IRB), Bahir Dar University. Written informed consent was ensured from all study participants to take part in the study voluntarily after they get informed about the objective and purpose of the study. This study was performed in accordance with the Declaration of Helsinki.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abate, A., Munshea, A., Nibret, E. et al. Persistence and clearance rates of human papillomaviruses in a cohort of women treated or not treated for cervical dysplasia in northwest Ethiopia. Sci Rep 15, 8218 (2025). https://doi.org/10.1038/s41598-025-87568-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87568-6