Abstract
Scoliosis is a prevalent condition among adolescents, and the spinal manipulation is one of the conservative treatment methods for scoliosis patients. Impairment in movement function stands out as a typical characteristic in cases of scoliosis. This study utilized a single-arm clinical trial design involving 35 patients aged 18 to 20 with idiopathic scoliosis (IS) and Cobb angles ranging from 10° to 30°. The treatment protocol consisted of spinal manipulation sessions three times a week, each lasting 40 min, administered over a span of six weeks. Pre- and post-intervention assessments focused on the Cobb angle and lower limb kinematics and kinetics during functional movements such as level walking, stair ascent, and descent. Patients with IS showed improvements in the Cobb angle, as well as changes in lower limb kinematics and kinetics during functional activities, such as walking and stair navigation, following six weeks of spinal manipulation intervention. The study further demonstrated that spinal manipulation reduced lower limb’s sagittal joint mobility, increased stability in individuals with IS. Patients with IS exhibited significant changes in lower limb kinematics and kinetic following spinal manipulation, which may serve as a potential mechanism underlying the alteration of the Cobb angle. Future studies, particularly RCTs, are needed to further validate the effectiveness of spinal manipulation in treating IS.
Similar content being viewed by others
Introduction
Idiopathic scoliosis (IS) represents the most prevalent form of spinal deformity, the incidence rate of IS can reach up to 12% among individuals aged 10 to 181. The condition progresses with age, worsening deformity and significantly impacting the quality of life2,3. Presently, various treatment strategies are employed depending on the degree of scoliosis curvature. For younger patients with a Cobb angle below 25°, conservative therapy is typically implemented, with follow-up assessments conducted every 3–6 months1. The International Scoliosis Association advocates spinal correction manipulation as a conservative treatment for IS4. Research indicates that spinal manipulation is a beneficial intervention for improving spinal deformity in individuals with IS5,6.
Notably, impaired movement function stands out as a prominent concern in IS patients, affecting up to 85% of individuals with this condition7,8. Numerous studies have shown that individuals with IS exhibit bilateral asymmetry in ground reaction forces during walking9. Another study suggests a decrease in gait parameter deviations, such as reduced ranges of motion in the hip joint and pelvis, indicating that the observed “careful walking” strategy could serve as a compensatory mechanism to minimize energy expenditure in individuals with IS10. This association may be linked to the presence of vertebral joint abnormalities in IS patients, resulting in abnormal gait patterns11. It is crucial to address the irregular gait in IS for scoliosis treatment as it not only improves mobility limitations but also corrects movement patterns7.
Climbing stairs is a common daily activity for humans, requiring more muscle and joint effort in the lower limbs than walking on a flat surface, thereby consuming more energy. The ability to climb stairs is vital for enhancing quality of life12,13. While current research has primarily examined gait analysis during level walking for individuals with IS, multiple studies have highlighted that stair climbing poses greater demands and challenges on the human body12,14,15. Investigating the biomechanics of stair climbing in IS patients is imperative for assessing and guiding the daily functional recovery of individuals with IS.
The objective of this research is to investigate the lower limbs’ biomechanics changes after the spinal manipulation technique for individuals with IS. We used the Qualisys motion analysis system to examine changes in the kinematics and kinetics of the lower limbs before and after spinal manipulation intervention in scoliosis patients during walking and stair tasks. This study aims to assess the development of advantageous movement patterns post-treatment, elucidate the underlying effects of spinal manipulation, and propose an innovative clinical approach that incorporates modifications in movement behaviors into forthcoming scoliosis intervention protocols.
Methods
Study design
This study employed a single-arm trial design, wherein participants meeting the inclusion criteria were assigned to the intervention group. The intervention comprised a six-week spinal manipulation regimen, with sessions scheduled thrice weekly, each lasting 40 min. Pre- and post-intervention evaluations included assessing the Cobb angle, alongside conducting three-dimensional motion analysis of the lower extremities.
Recruitment and informed consent
The study was conducted at the Third People’s Hospital affiliated with Fujian University of Traditional Chinese Medicine, where eligible patients diagnosed with IS were recruited from the outpatient department. Prior to commencing the study, approval was acquired from the ethics committee, and written informed consent was obtained from all participants. The process of signing the informed consent form entailed the researcher providing a comprehensive explanation of the study’s objectives, potential risks, and benefits to the participants in a secluded and confidential setting, utilizing both verbal and written communication methods tailored to the participants’ understanding.
Ethics and dissemination
This trial was approved by the Medical Science Research Ethics Committee of the Third People’s Hospital of Fujian University of Traditional Chinese Medicine (Approval No: 2023-KL-047) and registered with the Chinese Clinical Trial Registry (ChiCTR2300074648) on August 11, 2023.
Eligibility
Diagnostic criteria for IS:
(1) Conduct a standing position X-ray with full spine anteroposterior views to measure the coronal Cobb angle > 10°; (2) Assess the symmetry and alignment of the examinee’s shoulders and iliac crests while observing if the line of spinous processes extends to one side of the trunk; (3) Administer the Adam’s forward bend test on the spine, with the examinee standing and both knees extended, slowly bending the trunk forward. The physician sequentially examines both sides of the spine from top to bottom to assess alignment and symmetry; (4) Primary clinical symptom: spinal pain.
Inclusion criteria
(1) Individuals meeting the diagnostic criteria for this condition; aged 18–20, of any gender; with a Cobb angle on X-ray screening within 30° (including 30°); (2) signing the informed consent form and voluntarily participating in this trial can be included.
Exclusion criteria
The study will exclude individuals meeting any of the following conditions: (1) those with congenital, neurogenic muscle type, neurofibromatosis, interstitial lesions, or acquired scoliosis; (2) patients with severe osteoporosis or other conditions unsuitable for manual therapy; (3) individuals with significant skin damage or dermatological conditions in the treatment area; (4) patients unable to adhere to the prescribed treatment schedule or non-compliant with treatment; (5) participants currently involved in other clinical trials that could impact the evaluation of study results.
Interventions
Before the intervention, all participants were provided with education regarding the condition’s etiology, including information on risk factors, prevention strategies, treatment options, prognosis, maintaining a healthy lifestyle, and recommended exercise regimens. During the intervention session, participants received spinal manipulation administered by experienced chiropractors with a minimum of three years of clinical practice. The intervention involved thoracic spine extension adjustments for the primary affected segment in the thoracic region, along with lumbar spine rotation adjustments for the primary affected segment in the lumbar spine.
-
1.
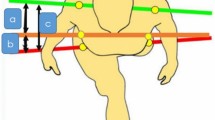
Thoracic spine extension manipulation16: The patient is positioned prone and instructed to fully relax. The therapist applies controlled force to the spine to achieve proper alignment. Palpation is performed on the affected spinal segment using the “butterfly hand” technique, where the therapist’s hands are interlocked. Leveraging their body weight, the therapist applies a rapid anterior–posterior and lateral thrust to the spine (see Fig. 1). Sudden, brief pressure is applied to the spinal area. If the surrounding muscles are tense, there is a risk of muscle injury; therefore, it is essential to relax the soft tissues around the vertebrae before proceeding with chiropractic manipulation. Thoracic vertebral correction is performed on the transverse processes of the thoracic vertebrae using the therapist’s hands.
-
2.
Lumbar spine rotation manipulation: The patient is positioned in a side-lying posture with the knee flexed and pelvic rotation, enabling flexion of the spine towards the affected segment. The therapist maintains the affected segment at a perpendicular angle to the ground, directing force towards the ilium. The patient is kept relaxed, and prior to manipulation, the therapist stabilizes the area with methods like traction, slight lateral bending, flexion, or extension of the spine. Pressure is exerted by both elbows as the body swiftly descends to administer a thrust (see Fig. 1).
The treatment protocol involves three sessions per week, with each session lasting for 40 min. Specifically targeting the affected segment located in the thoracic or thoracic-lumbar region, the interventions include thoracic spine extension techniques and lumbar spine rotation manipulation. This treatment regimen extends over a period of 6 weeks.
All participants received personalized guidance on self-exercise training tailored to their specific condition, along with education on sustaining a healthy lifestyle.
Outcome measurements
Standardized objective assessment criteria were utilized for evaluations performed by professional medical staff who were not part of the treatment team. Assessments were conducted before the initial treatment session following grouping and on the day of completion of the 6-week treatment period.
-
1.
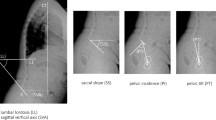
Cobb angle: The Cobb angle was assessed via X-ray to evaluate the coronal plane deformity of the spine while the individual was in a standing position17. Reductions in curvature exceeding 5° will be deemed as minimal clinically significant changes.
-
2.
Spinal Appearance Questionnaire (SAQ): The SAQ assesses patients’ and their families’ perceptions of spinal deformities using standardized images and questions. The total score of the questionnaire is 80 points, with higher scores indicating greater dissatisfaction with appearance.
-
3.
Scoliosis Research Society-22 (SRS-22): The SRS-22 is widely used to assess the impact of scoliosis and the effectiveness of treatments. The highest possible score for each item is 5, and the lowest is 1. Higher scores indicate more severe functional impairment.
-
4.
Oswestry Disability Index (ODI): The ODI is a self-administered questionnaire for quantifying functional disability in patients with spinal disorders. The original version includes 10 items, each with 6 response options (scored 0–5), where a score of 0 indicates no functional disability. Higher scores reflect more severe disability.
-
5.
Analysis of the kinematics and kinetics of the lower limbs18.
Three-dimensional motion analysis: markers were meticulously positioned on various anatomical sites of the participants in accordance with the specifications of the 3D motion analysis system from Motion Analysis Corporation (Eagle-4, USA). The lower limb marker set adopted the CAST/Cleveland Clinic Model19, featuring markers on the thighs (femoral midshaft, femoral medial and lateral epicondyles - FLE, FME), lower legs (tibial midshaft, medial malleolus - TAM, lateral malleolus - FAL), and feet (dorsal aspect of the fifth metatarsal head - FM5, second metatarsal head - FM2, first metatarsal head - FM1, calcaneus - FCC). Elastic bands were utilized to affix fluorescent spheres at the corresponding locations on the outer surface of the body, and data collection involved the calibration of eight cameras (sampling rate of 1500Hz) using the motion analysis system’s workstation.
The tracking points’ positions are illustrated in Fig. 2.
Data collection: The data collection process of the three-dimensional motion analysis system involves acquainting the participants with the walkway before data recording commences. Participants are instructed to walk at a self-perceived comfortable pace along a flat walkway measuring approximately 10 meters in length (with an effective data collection zone of 4 meters) and 2.4 meters in width. Eight customizable adjustable steps, each with a height of 20cm and a depth of 30cm, are utilized for recording stair ascent and descent activities. Specifically, two force plates (Kistler, Model 9260AA, Switzerland, dimensions: 60cm x 50cm) are positioned on the third and fourth steps, operating at a sampling frequency of 1000Hz.
Data analysis: The data analysis of the three-dimensional motion analysis system entails recording the patient’s gait during level ground walking and ascending/descending movements. The gait data is subsequently analyzed using the Visual 3D software, developed by C-motion in the USA. This analysis encompasses two main aspects: a. Kinematic parameters, focusing on the joint movements of the lower limbs (hip, knee, ankle) in the sagittal, coronal, and horizontal planes during the walking cycle on level ground. b. Kinetic parameters, derived from data collected through force plates during level ground walking, which include peak ground reaction force and peak joint moments in three dimensions for the lower limbs. The ground reaction force undergoes standardization based on body weight, and all joint moments are standardized with consideration of body weight and leg length (%BM*Height) to facilitate further analysis post-standardization.
Data processing: Data processing in the three-dimensional motion analysis system entails rectifying and completing incomplete data collection to ensure that each participant has a minimum of 5 valid data sets for every task. A smoothing filter with a scale of 10 is utilized to eliminate evident noise in the data. Motion videos recorded synchronously during data acquisition are referenced to select and input various motion data from the corresponding cycles into Excel 2016 (Microsoft, Inc.) for analysis. The process involves selecting data from 5 gait cycles showing similar patterns for each participant, calculating the mean from these data sets among the 5 groups, consolidating the means, and deriving average and standard deviation curves for joint motion angles. Consequently, each frame of motion data is presented as "mean ± standard deviation". This study opts to use the maximum value in the gait cycle to portray kinematic traits and conducts separate comparisons between participants’ motion data and that of the normal group.
Data management
Individual participants will be assigned unique identification numbers, to which all data will be linked. The data entry, validation, and analysis processes were supervised by an impartial data manager who is independent of the allocation process. Both paper and electronic data will be securely stored at the Third People’s Hospital of Fujian University of Traditional Chinese Medicine.
Sample size calculation
The Cobb angle is widely recognized as the primary outcome measure for evaluating clinical efficacy in patients with IS. A review of the literature indicates that, following spinal manipulation, the treatment group demonstrated an improvement of 16.0 ± 6.9° in the Cobb angle. Using the sample size calculation software G*Power 3.1, the effect size was determined to be 0.678. For a two-tailed test with α = 0.05 and a power of (1 − β) = 0.8, an effect size of 0.7 was selected. Based on these parameters, the required group size was calculated to be 26 cases to achieve the desired statistical power. Considering an anticipated dropout rate of 20%, a total sample size of approximately 32 cases was determined for the study.
Statistical analysis
The original data were inputted into EXCEL 2013, and statistical analysis was performed using SPSS 24.0 software. Before and after the intervention, categorical data were presented in terms of composition ratios. Quantitative data and normally distributed data were described using \(\overline{x} \pm s\). Non-normally distributed data were characterized by the median (M) and interquartile range (IQR) where the lower quartile (Q1) and upper quartile (Q3) were designated as P25 and P75 respectively. Within normally distributed groups, paired sample t-tests were administered, while non-normally distributed data within groups were analyzed using paired sample rank sum tests. The hypothesis testing threshold was set at P < 0.05 to denote statistical significance.
Results
General information
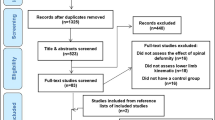
After screening 100 individuals initially, 40 met the eligibility criteria, five participants withdrew from the study voluntarily, citing increased exercise in competitive events as the reason, whereas four were lost to follow-up, the final analysis included 35 patients. Figure 3 presents the flowchart, while Table 1 provides the demographic details of the participants, including age, gender, height, weight, BMI, and the distribution of scoliotic segments at onset.
Cobb angle
The results presented in Table 2 demonstrate a significant reduction in the post-intervention Cobb angle (8.83 ± 4.20° vs. 15.67 ± 4.09°) among patients with IS compared to the pre-intervention measurements (P < 0.001).
Incidence of adverse events
We identified potential adverse events associated with the research process, including muscle strain, hypoglycemia, heatstroke, localized skin redness, itching, and allergic reactions. The incidence of these adverse events is presented below:
Questionnaire
The results presented in Table 3 showed that there were no significant differences in the SRS-22, SAQ, and ODI scores before and after spinal manipulation for IS (P > 0.05).
Kinematics in level walking
The findings presented in Table 4 indicate that, among individuals with IS in level walking, subsequent to intervention, the ROM for hip flexion/extension on the concave side decreased (38.64 ± 4.38° vs. 40.05 ± 4.73°), as did the ROM for hip internal/external rotation on the concave side (11.68 ± 3.07° vs. 13.25 ± 3.37°), and the ROM for knee flexion/extension on the convex side (63.16 ± 5.16° vs. 64.70 ± 5.68°) (P < 0.05). No statistically significant differences were noted in the remaining lower limb kinematics before and after the intervention (P > 0.05).
Kinematics and kinetics in ascent stairs
Table 5 results reveal that following the intervention among IS patients in the task of ascending stairs, there was a notable decrease in the ROM for various joint movements. Specifically, the hip convex side of flexion/extension decreased from 62.15 ± 4.94° to 63.63 ± 4.82°, the hip concave side of flexion/extension decreased from 62.29 ± 4.39° to 63.26 ± 5.09°, the hip convex side of internal/external rotation decreased from 11.03 ± 2.95° to 12.59 ± 3.66°, and the knee convex side of flexion/extension decreased from 91.07 ± 6.59° to 93.65 ± 6.08° (P < 0.05). Notably, there were no statistically significant differences in the remaining lower limb kinematics (P > 0.05).
Table 6 results indicate that following intervention in IS patients during stair climbing, the peak moment of ankle convexity joint in flexion–extension [1.39 (1.36, 1.42) vs. 1.45 (1.42, 1.48) Nm/kg] was observed to be lower post-intervention compared to pre-intervention (P < 0.05). However, no statistically significant variances were found in the other kinematic indicators (P > 0.05).
Kinematics and kinetics in descent stairs
Table 7 findings indicate that during down stairs activities, IS patients exhibited a reduction in the ROM on the hip convex side of internal/external rotation (13.71 ± 3.02° vs. 15.22 ± 3.34°), as well as a decrease in ROM on the knee concave side of flexion/extension (95.73 ± 5.74° vs. 97.43 ± 5.75°) post-intervention compared to pre-intervention (P<0.05). Additionally, there was an increase in ROM on the ankle concave side of flexion/extension (68.14 ± 6.30° vs. 66.71 ± 5.67°) post-intervention compared to pre-intervention (P < 0.05). No statistically significant variances were observed in the remaining kinematics (P > 0.05).
The findings from Table 8 indicate that following intervention in down stairs activities, IS patients exhibited an increase in knee concave side joint peak moment for flexion–extension (1.23 ± 0.22 vs. 1.17 ± 0.24 NM/Kg) compared to pre-intervention levels (P < 0.05). Moreover, the AP convexity of ground reaction force [0.14(0.13,0.15) vs. 0.15(0.14,0.15) N/Kg], ML concavity of ground reaction force [0.09(0.08,0.09) vs. 0.14(0.10,0.18) N/Kg], Vertical convexity of ground reaction force [1.39(1.36,1.3) vs. 1.47(1.43,1.51) N/Kg], and Vertical concavity of ground reaction force [1.41(1.38,1.43) vs. 1.48(1.43,1.52) N/Kg] were lower post-intervention than pre-intervention (P < 0.05). No statistically significant differences were observed in the remaining kinematic indicators (P > 0.05).
Discussion
This trial aims to investigate the kinematics and kinetics changes in level walking and stair activities after spinal manipulation in patients with scoliosis. Our findings presented in Table 2 of this study demonstrate a significant mean improvement of 7 degrees in the Cobb angle among individuals with IS following intervention, with a statistically significant effect (P < 0.001). A change in the Cobb angle exceeding 5 degrees is considered clinically meaningful, as it meets the minimum clinically important difference (MCID)20. The guidelines established by the Scoliosis Research Society (SRS) emphasize the effectiveness of manipulation in improving joint alignment and muscle balance in the treatment of IS21. This is achieved by alleviating abnormal muscle tension and reducing pain, thereby facilitating effective management of the condition. Additionally, a substantial body of evidence from various studies supports the clinical efficacy of chiropractic manipulation in managing scoliosis5,6,16,21,22,23,24,25.
We assessed structural changes in individuals with IS before and after intervention, focusing on variations in lower limb kinematics and kinetics during routine activities such as level walking and stair activities.
-
1.
Level walking: Among patients with IS walking on flat ground, a movement pattern trend is observed, characterized by reduced sagittal plane motion, a decreased anterior–posterior range, diminished sway, and improved stability. During level walking activities, individuals with IS post-intervention exhibited decreased the ROM for hip flexion/extension on the concave side, as did the ROM for hip internal/external rotation on the concave side, and the ROM for knee flexion/extension on the convex side (P < 0.05). Following the intervention, the ROM in the sagittal plane of the patient’s hip joints, and knee joints all decreased. Specifically, there was a reduced ROM in the hip joint’s horizontal plane. It is hypothesized that post-intervention, the sagittal plane activity of patients with IS decreased during level walking, contributing to enhanced stability. This decrease in activity is offset by an increase in angular momentum in the horizontal plane. Subsequent to the intervention for IS patients, the ROM of hip joint flexion/extension and internal/external rotation decreased to align with the body’s walking pattern utilizing the spiral-diagonal paradigm (Proprioceptive Neuromuscular Facilitation pattern, PNF). Additionally, there was a reduction in ROM on the knee joint convex side to maintain equilibrium in the body’s center of gravity. During walking, the human body orchestrates joint movements to optimize energy efficiency. The spine must maintain its natural curvature and engage in controlled rotation for balanced center of gravity (COG)26. Through manipulation intervention, adjustments are made to joint and muscle movements, enhancing spine biomechanics. Although movement patterns of these patients remain largely unchanged during flat surface ambulation. To identify further aberrant movement patterns in IS patients, challenging activities like stair climbing were integrated.
-
2.
Ascent stairs: The intervention in patients with IS led to a reduction in the joint ROM in both the spine and lower limbs along the sagittal plane, enhancing joint stability during stair ascent. Climbing stairs presents a significant challenge for the general population27, with a particular risk of falls for individuals with scoliosis. Engagement in such functional tasks is more likely to elicit atypical movement patterns in those with compromised functions. During ascending stair activities, the hip convex side of flexion/extension decreased, the hip concave side of flexion/extension decreased, the hip convex side of internal/external rotation decreased, and the knee convex side of flexion/extension decreased (P < 0.05). Regarding kinetics, the peak moment of ankle convexity joint in flexion–extension was observed to be lower post-intervention compared to pre-intervention (P < 0.05). Our findings indicate that IS patients experienced decreased ROM in the sagittal plane of the hips, and knee joints following intervention during stair ascent. In the transverse plane post-intervention, there was a decrease in flexion/extension ROM in hip joints. This noteworthy observation highlights the diminished ROM across various joints in IS patients across all three planes during stair ascent, with the most notable changes occurring in the sagittal plane. It is speculated that this reduction may be attributed to the heightened instability and sway experienced by IS individuals undertaking this relatively hazardous activity compared to their healthy counterparts. Subsequent to manipulation intervention, a noticeable decrease in anterior–posterior ROM in the sagittal plane was evident, possibly linked to the technique’s enhancement of the three-dimensional spinal joint abnormalities and restoration of spinal biomechanics. Thus, the reduced ROM, decreased sagittal plane displacement, and lower work output post-intervention indicate improved efficiency in individuals with IS during challenging stair climbing tasks. Research findings indicate during stair climbing with the step-over-step technique, significant compensation mechanisms were found as a consequence of leg length inequalities28. Individuals with IS also utilize compensatory mechanisms to navigate challenging stair climbing tasks. Transitioning from a level surface to a staircase demands heightened joint mobility and muscle strength. The lower limbs, providing support, bear the body’s weight while maintaining stability under load, while the advancing limbs execute rapid joint flexion to move from the supporting step-side to the subsequent higher step. Ascending taller steps necessitates bending of the knee joints to generate the required power and flexibility for lifting the body. During knee flexion, the joint deviates from its stable and locked state typically observed during flat-ground ambulation29. Before the intervention on IS patients, the center of gravity was biased towards the concave side, resulting in increased weight-bearing on the concave lower limb. Following the intervention, spinal alignment improved, shifting the center of gravity towards the midline and reducing the weight-bearing asymmetry between the lower limbs. This adjustment also correlated with enhanced stability in the convex-side lower limb, leading to a decrease in the range of motion of the knee joint on that side. Additionally, post-intervention, there was a reduction in both activity and load on the ankle joint bilaterally, with more pronounced changes observed in the ankle joint of the convex side. Manual intervention by adjusting the joints of IS patients may have contributed to reshaping muscle arrangement, thereby improving muscle function, increasing strength, reducing joint mobility, and enhancing overall bodily stability. Nevertheless, the assessment of muscle performance in IS patients was not conducted, highlighting the need to include this evaluation in future verification efforts.
Before the intervention on IS patients, the center of gravity was biased towards the concave side, resulting in increased weight-bearing on the concave lower limb. Following the intervention, spinal alignment improved, shifting the center of gravity towards the midline and reducing the weight-bearing asymmetry between the lower limbs. This adjustment also correlated with enhanced stability in the convex-side lower limb, leading to a decrease in the ROM of the knee joint on that side. Additionally, post-intervention, there was a reduction in both activity and load on the ankle joint bilaterally, with more pronounced changes observed in the ankle joint of the convex side. Consequently, the intervention in IS patients resulted in decreased joint movement range of the spine and lower limbs in the sagittal plane, promoting joint stability. Manual intervention by adjusting the joints of IS patients may have contributed to reshaping muscle arrangement, thereby improving muscle function, increasing strength, reducing joint mobility, and enhancing overall bodily stability. Nevertheless, the assessment of muscle performance in IS patients was not conducted, highlighting the need to include this evaluation in future verification efforts.
-
3.
Descent stairs: The spinal manipulation in patients with IS was achieved through improved performance of the spine and lower limb muscle groups, enhanced movement control during descent, and increased balance capacity due to stronger centrifugal contraction, ultimately reducing the risk of falls. In the post-intervention stepping down activity, IS patients exhibited a reduction in the ROM on the hip convex side of internal/external rotation, as well as a decrease in ROM on the knee concave side of flexion/extension post-intervention compared to pre-intervention (P < 0.05). Additionally, there was an increase in ROM on the ankle concave side of flexion/extension post-intervention compared to pre-intervention (P < 0.05). For changes in kinetics, IS patients exhibited an increase in knee concave side joint peak moment for flexion/extension compared to pre-intervention levels (P < 0.05). Moreover, the AP convexity of ground reaction force, ML concavity of ground reaction force, Vertical convexity of ground reaction force, and Vertical concavity of ground reaction force were lower post-intervention than pre-intervention (P < 0.05). After the intervention, there was an increase in the ROM in ankle joints. Additionally, in the horizontal plane following the intervention, the ROM for hip joint flexion/extension decreased. Upon analyzing descent activities, it was observed that individuals with IS displayed a distinct movement pattern compared to ascent activities, with descent tasks being prone to greater instability as individuals execute a series of movements to prevent falls30.
When descending stairs, the primary centrifugal activity occurs in the sagittal plane. Throughout descent, the ground reaction forces (GRF) in the anterior–posterior, medial–lateral, and vertical directions decrease in IS patients, potentially due to reduced propulsion needed during stair descent, indicating a greater reliance on gravity for downward movement, thus improving centrifugal control. An increase in the ROM for ankle joint flexion/ extension is noted, reflecting improved ankle joint control.
-
4.
Movement patterns alteration following spinal manipulation: Initial investigations conducted by our research team revealed distinct muscle and joint movement patterns in individuals with IS compared to typical individuals during activities on level ground and stair navigation31,32,33. After a six-week spinal manipulation intervention, individuals with IS exhibited significant changes in movement, including a reduction in hip and knee flexion/extension ROM and an increase in ankle flexion/extension ROM during activities such as walking and stair climbing. Since these activities are crucial for daily functioning, future assessments and treatment strategies for IS should consider these changes in movement characteristics to optimize functional outcomes.
Limitation
The main limitation of this study is that the research design cannot demonstrate the effectiveness of spinal manipulation in treating IS. In the future, we will include a control group to further explore the relationship between its clinical efficacy and biomechanics. Another limitations stem from its narrow focus on individuals aged 18–20 with scoliosis curves measuring less than 30°, potentially limiting the extrapolation of spinal manipulation methods to broader IS populations. The intervention duration was set at 6 weeks. Future studies with longer intervention periods may reveal more pronounced biomechanical changes. Future research should include a broader age range and a larger sample size to improve generalizability. It is also essential to investigate treatment based on the affected segments in order to better understand the mechanisms of manual therapy. Furthermore, incorporating clinical physical assessments and biomechanical matching would provide valuable guidance for clinicians. Furthermore, the muscle attributes of IS patients were not assessed. Prospective studies could delve into muscle functionality to acquire a more profound comprehension of the biomechanical aspects of IS during physical exertion and to refine rehabilitation protocols.
Conclusion
Our findings suggest that individuals with IS exhibited significant changes in lower limb kinematics and kinetics during functional activities such as walking and stair climbing following six weeks of spinal manipulation therapy. Furthermore, the study demonstrated that spinal manipulation reduced joint mobility while enhancing stability in IS patients, which may serve as a potential mechanism underlying the alteration of the Cobb angle. Future studies, particularly RCTs, are needed to further validate the effectiveness of spinal manipulation in treating IS.
Data availability
All data generated or analyzed during this study are included in this article.
References
Negrini, S. et al. SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 13(1), 3 (2016).
Mahaudens, P., Banse, X., Mousny, M. & Detrembleur, C. Gait in adolescent idiopathic scoliosis: Kinematics and electromyographic analysis. Eur. Spine J. 18(4), 512–521 (2009).
Weiss, H., Karavidas, N., Moramarco, M. & Moramarco, K. Long-term effects of untreated adolescent idiopathic scoliosis: A review of the literature. Asian Spine J. 10(6), 1163–1169 (2016).
Society. SR. Treating Scoliosis. 2016. Available from: http://www.srs.org/patients-and-families/conditions-and-treatments/adolescents/treating-scoliosis
Lotan, S. & Kalichman, L. Manual therapy treatment for adolescent idiopathic scoliosis. J. Bodyw. Mov. Ther. 23(1), 189–193 (2019).
Sun, W. et al. Effect of spinal manipulation on degenerative scoliosis. J. Tradition. Chin. Med. 40(6), 1033–1040 (2020).
Park, H. et al. Analysis of coordination between thoracic and pelvic kinematic movements during gait in adolescents with idiopathic scoliosis. Eur. Spine J. 25(2), 385–393 (2016).
Pialasse, J., Descarreaux, M., Mercier, P., Blouin, J. & Simoneau, M. The vestibular-evoked postural response of adolescents with idiopathic scoliosis is altered. PLoS One 10(11), e0143124 (2015).
Yang, J. H., Suh, S., Sung, P. S. & Park, W. Asymmetrical gait in adolescents with idiopathic scoliosis. Eur. Spine J. 22(11), 2407–2413 (2013).
Mahaudens, P. & Mousny, M. Gait in adolescent idiopathic scoliosis. Kinematics, electromyographic and energy cost analysis. Stud. Health Technol. Inform. 158, 101–106 (2010).
Kim, D. S., Park, S. H., Goh, T. S., Son, S. M. & Lee, J. S. A meta-analysis of gait in adolescent idiopathic scoliosis. J. Clin. Neurosci. 81, 196–200 (2020).
Namnik, N. et al. Examination of lumbopelvic and lower extremity movements in two subgroups of people with chronic low back pain based on the movement system impairment model during a stair descending task. Ortopedia Traumatologia Rehabilitacja 21(3), 197–205 (2019).
Lee, J. K., Desmoulin, G. T., Khan, A. H. & Park, E. J. Comparison of 3D spinal motions during stair-climbing between individuals with and without low back pain. Gait Posture 34(2), 222–226 (2011).
Kuai, S. et al. Prediction of the spinal musculoskeletal loadings during level walking and stair climbing after two types of simulated interventions in patients with lumbar disc herniation. J. Healthc. Eng. 2019, 6406813 (2019).
Lee, J. K. & Park, E. J. 3D spinal motion analysis during staircase walking using an ambulatory inertial and magnetic sensing system. Med. Biol. Eng. Comput. 49(7), 755–764 (2011).
Byun, S. & Han, D. The effect of chiropractic techniques on the Cobb angle in idiopathic scoliosis arising in adolescence. J. Phys. Ther. Sci. 28(4), 1106–1110 (2016).
Wang, J. et al. Measurement of scoliosis Cobb angle by end vertebra tilt angle method. J. Orthop. Surg. Res. 13(1), 223 (2018).
List, R., Gülay, T., Stoop, M. & Lorenzetti, S. Kinematics of the trunk and the lower extremities during restricted and unrestricted squats. J. Strength Cond. Res. 27(6), 1529–1538 (2013).
Abdullah, M., Hulleck, A. A., Katmah, R., Khalaf, K. & El-Rich, M. Multibody dynamics-based musculoskeletal modeling for gait analysis: A systematic review. J. Neuroeng. Rehabil. 21(1), 178 (2024).
Richards, B. S., Bernstein, R. M., D’Amato, C. R. & Thompson, G. H. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine 30(18), 2068–2075 (2005).
Rowe, D. E. et al. Chiropractic manipulation in adolescent idiopathic scoliosis: A pilot study. Chiropract. Osteop. 14, 15 (2006).
Cuka, C., Mcdevitt, A. W., Porter-Hoke, A. & Karas, S. Spinal manipulation after multiple fusions in an adult with scoliosis: A case report. J. Manual Manipulat. Ther. 27(2), 115–124 (2019).
Morningstar, M. W. & Joy, T. Scoliosis treatment using spinal manipulation and the Pettibon weighting system: A summary of 3 atypical presentations. Chiropract. Osteopathy 14, 1 (2006).
Sun, Y., Zhang, Y., Ma, H., Tan, M. & Zhang, Z. Spinal manual therapy for adolescent idiopathic scoliosis: A systematic review and meta-analysis of randomized controlled trials. Biomed. Res. Int. 2023, 7928429 (2023).
Théroux, J. et al. Spinal manipulative therapy for adolescent idiopathic scoliosis: A systematic review. J. Manipulat. Physiol. Ther. 40(6), 452–458 (2017).
Umberger, B. R. & Martin, P. E. Mechanical power and efficiency of level walking with different stride rates. J. Exp. Biol. 210(Pt 18), 3255–3265 (2007).
Ram, M. et al. Stair-fall risk parameters in a controlled gait laboratory environment and real (domestic) houses: A prospective study in faller and non-faller groups. Sensors (Basel, Switzerland) 24(2), 526 (2024).
Siebers, H. L. et al. Biomechanical compensation mechanisms during stair climbing—The effect of leg length inequalities. Gait Posture 91, 290–296 (2022).
Gonçalves, G. H., Selistre, L. F. A., Petrella, M. & Mattiello, S. M. Kinematic alterations of the lower limbs and pelvis during an ascending stairs task are associated with the degree of knee osteoarthritis severity. Knee 24(2), 295–304 (2017).
Wang, K. et al. Differences between gait on stairs and flat surfaces in relation to fall risk and future falls. IEEE J. Biomed. Health Inform. 21(6), 1479–1486 (2017).
Gou, Y. et al. Spinal muscle characteristics during three different types of locomotion activities among college students with idiopathic scoliosis. BMC Musculoskelet Disord. 25(1), 862 (2024).
Gou, Y. et al. Biomechanical analysis of trunk and lower limbs during stair activity in patients with scoliosis. Sci. Rep. 14(1), 14541 (2024).
Gou, Y. et al. Trunk kinematic analysis of ascent and descent stairs in college students with idiopathic scoliosis: A case-control study. Spine J. 24(9), 1712–1722 (2024).
Funding
Project supported by the National Natural Science Foundation of China (Grant No. 82205306).
Author information
Authors and Affiliations
Contributions
Yanyun GOU contributed to designing the trial, write the manuscript and the submissions. Huangwei LEI helped design the trial and draft the manuscript. Lin MENG contributed to oversaw the manuscript. Shaoqing CHEN contributed to the statistical analysis. Zheng JIANG contributed to the trial design.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent to participate was obtained from all subjects and/or their legal guardian(s); this study has obtained approval from the Ethics Committee of the Third People’s Hospital Affiliated to Fujian University of Traditional Chinese Medicine (Approval No: 2023-kl-047). It has also been registered with the Chinese Clinical Trial Registry on 11/08/2023, under the registration number ChiCTR2300074648.
Consent for publication
Informed consent to participate was obtained from all subjects and/or their legal guardian(s).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gou, Y., Meng, L., Chen, S. et al. Analysis of kinematic and kinetic changes in scoliosis following spinal manipulation. Sci Rep 15, 3881 (2025). https://doi.org/10.1038/s41598-025-87812-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87812-z