Abstract
Increasing evidence suggests that endocrine-disrupting chemicals (EDCs) have adverse effects on breast cancer (BC). The aim of this study was to assess the association between exposure to prevalent EDCs—phenols and parabens—and the risk of developing BC. Data on urinary bisphenol A (BPA), triclosan (TRS), benzophenone-3 (BP3), methyl paraben (MPB), ethyl paraben (EPB), propyl paraben (PPB), and butyl paraben (BUP) were obtained from the 2005–2014 National Health and Nutrition Examination Survey. A total of 4455 subjects were included in this cross-sectional study. The results from the weighted multivariable regression models indicated that exposure to elevated concentrations of TRS increased the risk of developing BC by 2.33 (Q2: 95% CI = 1.45–3.75, p < 0.001) and 1.94 times (Q3: 95% CI = 1.21–3.09, p = 0.006), respectively. The nonlinear association between TRS concentrations and the risk of developing BC was statistically significant (P nonlinear = 0.007), with the restricted cubic splines (RCS) curve exhibiting an inverted U shape. The association between TRS concentrations and the risk of developing BC was more pronounced among overweight individuals (BMI ≥ 25 kg/m2), those aged < 60 years, and white individuals. Weighted quantile sum (WQS) and Bayesian Kernel Machine Regression (BKMR) analysis revealed no significant overall association between mixtures of urinary phenol and paraben metabolites and BC risk. However, TRS exposure was the most influential, with higher TRS concentrations (both continuous and categorical) significantly associated with an increased BC risk, particularly in overweight individuals (BMI ≥ 25 kg/m2), those aged < 60 years, and white individuals.
Similar content being viewed by others
Introduction
Breast cancer (BC) is one of the most prevalent malignant tumors in women1. As indicated by the data released by the American Cancer Society in 2024, the incidence rate of BC in the United States continued an upward trend, rising by 1% annually during 2012–20212. Epidemiological studies have indicated that early menarche, late first birth, menopause, and other potential reproductive and family history are risk factors for BC, yet these factors only partially account for the risk of developing BC3,4. Endocrine-disrupting chemicals (EDCs), a group of synthetic and naturally occurring chemicals, can disrupt the endocrine system in the human body. They are increasingly being recognized as a significant and urgent threat to public health and may emerge as one of the major environmental risks globally5. Studies have confirmed the association between EDCs and endocrine gland cancers6,7,8, and population studies have also suggested that BC development may be associated with exposure to certain organic solvents, polycyclic aromatic hydrocarbons, and organochlorine compounds9,10,11. Consequently, the role of hormonally active EDCs in the occurrence and development of BC is gaining increased attention.
Phenolic substances and parabens are ubiquitous and are two representative families of EDCs. Human exposure to these compounds occurs through industrial pollution, pesticide use, food consumption, and the use of personal care products12,13. Bisphenol A (BPA) is employed in the manufacture of polycarbonate plastics and epoxy resins and is found in protective coatings for food containers, as well as in dental composites and sealants14. Triclosan (TRS) is utilized as an antibacterial agent in soap and is present in other personal care products15. Benzophenone-3 (BP3) is used as a sunscreen for skin protection and as a UV filter in cosmetics and plastics16. Parabens, a group of alkyls (such as methyl paraben (MPB), ethyl paraben (EPB), propyl paraben (PPB), and butyl paraben (BUP)), are widely used as antimicrobial preservatives in personal care products and can also be used in pharmaceuticals and food and beverage processing17. Several studies have proven that phenol and paraben metabolites disrupt endocrine function18,19, and their widespread exposure is linked to the increased risks of endocrine-related diseases, including gestational diabetes20, abnormal breast development21, obesity22, and uterine leiomyomas23.
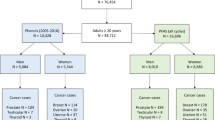
Previous animal studies have revealed that phenols and parabens compounds, including BPA and TRS, may be associated with the progression and metastasis of BC24,25,26. However, there is a scarcity of research examining their association with the risk of developing BC based on large population samples. Therefore, in this study, we utilized data from five cycles of the National Health and Nutrition Examination Survey (NHANES) (2005–2014), a nationally representative sample of the noninstitutionalized civilian population in the United States, to examine the associations between urinary concentrations of phenols (BPA, TRS, BP3) and parabens (MPB, EPB, PPB, BUP) and the risk of developing BC (Fig. 1). Additionally, stratified analyses of BMI, age, and race were conducted to further explore the impact of exposure to these metabolites on the risk of developing BC in different populations of women aged 20 and older in the United States.
Materials and methods
Study design
The NHANES is a cross-sectional survey that uses a complex, multistage probability sampling method, with the aim of representing the civilian, noninstitutionalized population of the United States27. We utilized publicly available data from 50,965 participants who participated in the NHANES from 2005 to 2014. The dataset encompasses sociodemographic data, laboratory measurements of urinary phenol and paraben levels, and medical condition questionnaire data. We selected this time period because it includes comprehensive data on key urinary metabolites (BPA, TRS, BP3, MPB, EPB, PPB, and BUP), while later cycles (2015–2016) lacked creatinine data, which is essential for normalizing metabolite concentrations28,29. After data integration, we sequentially excluded males (N = 25,260), individuals under the age of 20 (N = 11,045) due to the lack of cancer-related questionnaire data for this group, and participants with missing phenol and paraben data (N = 10,205). Ultimately, this study included a total of 4,455 individuals with complete exposure and outcome data. The research approach of this paper is depicted in Fig. 2.
The research ethics review committee of the Centers for Disease Control and Prevention (CDC) approved all research protocols of the NHANES, and all participants provided written informed consent (https://www.cdc.gov/nchs/nhanes/irba98.htm). The data analyzed in this study can be publicly obtained from the NHANES website.
Measurement of phenols and parabens
Urine samples were collected from participants in standard urine collection cups (at least 5 ml), labeled, and frozen. The samples were stored at appropriate refrigerated (− 20 ℃) until transported to the National Center for Environmental Health for analysis. According to the NHANES protocol, there are no specific instructions regarding the time of urine collection, and the samples were not restricted to morning urine. The NHANES staff developed a sensitive method for measuring BPA, TRS, BP3, and four parabens30. This method employs solid-phase extraction combined with high-performance liquid chromatography and tandem mass spectrometry, which is highly accurate and sufficient for measuring the levels of urinary phenols, parabens, and triclosan in nonoccupationally exposed subjects. Creatinine correction normalized the concentrations of all urinary phenol and paraben metabolites.
From 2005 to 2012, the lower limits of detection (LLODs) for BPA, TRS, BP3, MPB, EPB, PPB, and BUP were 0.40, 2.30, 0.40, 1.00, 1.00, 0.20, and 0.20 ng/mL, respectively. The LLODs for 2013–2014 were 0.20, 1.70, 0.40, 1.00, 1.00, 0.10, and 0.10 ng/mL, respectively. Subjects with values below the LOD were assigned the designated NHANES concentration, i.e., LLOD/√2 (https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/VOCWB_I.htm).
Diagnosis of BC
Information about BC was collected during face-to-face interviews using the NHANES Medical Conditions Questionnaire. All questions in the questionnaire were administered by trained interviewers using a computer-assisted personal interviewing system at mobile examination centers. In essence, participants were asked, “Have you ever been told by a doctor or other health professional that you had cancer or a malignancy of any kind?”. Individuals who responded affirmatively were further asked, “What kind of cancer was it?” Females who reported a diagnosis of “breast cancer” were classified as having BC31.
Covariates
Referring to previous literature, several potential confounding factors were included in our analysis of the NHANES study29,32,33,34. These included demographic information (age, race, poverty income ratio (PIR), educational level, and marital status), physical examination parameters (body mass index (BMI, kg/m2)), lifestyle factors (smoking and drinking), and comorbidity information (diabetes, hypercholesterolemia, hypertension, and cardiovascular disease (CVD)). The participants’ educational level was divided into below high school, high school, and above high school. Marital status was divided into married or living with a partner and living alone. Participants’ smoking status was classified as never smoked, past smoker, or current smoker. Participants’ drinking status was divided into ever drank and never drank. Comorbidity data are defined by positive responses to self-reported doctor diagnoses of these diseases. CVD encompassed congestive heart failure, coronary heart disease, angina/angina pectoris, heart attack, and stroke.
Statistical analysis
The analysis of NHANES laboratory data must be conducted in conjunction with key survey design and basic demographic variables, i.e., using the stratum and PSU variables (SDMVSTRA and SDMVPSU, respectively) in the demographic data file. Furthermore, considering the complex multistage sampling survey design, all analyses in this study adjusted weights according to the NHANES analysis guidelines.
First, we calculated descriptive statistics for the baseline characteristics of the patients in the BC and non-BC groups. Continuous variables are presented as the mean ± standard deviation. For normally distributed data, comparisons were made using the student’s t-test. However, as our data did not follow a normal distribution and had unequal variances, the non-parametric Kruskal–Wallis test was chosen. Categorical variables are represented as frequencies and percentages and were analyzed using the chi-square test. For covariates with missing data, the R package “missForest”35 was used for imputation. This method employs random forest algorithms to predict and impute missing values based on the observed data, without requiring specific assumptions about the data distribution. Urinary phenol and paraben metabolite concentrations were normalized by log10 transformation to improve normality and reduce the influence of extreme values, and the sample was divided into low, medium, and high exposure groups based on tertiles to evaluate the impact of different exposure levels on BC risk. Spearman correlation coefficients were calculated to determine the correlations among the seven variables. A correlation coefficient of < 0.3 is considered weak, 0.3–0.5 as moderate, 0.5–0.7 as strong, and ≥ 0.7 as very strong36.
Second, we conducted weighted multivariate logistic regression analysis to explore the associations between phenol/paraben concentrations and the risk of developing BC, constructing three models to adjust for different confounding factors. Model 1 was unadjusted for any covariates, Model 2 was adjusted for age, race/ethnicity, education level, family PIR, and BMI, and Model 3 was further adjusted for all other covariates (including marital status, smoking status, alcohol status, and comorbid condition) based on Model 2. The results are expressed as odds ratios (OR) and 95% confidence intervals (CI). We designated the first quartile (Q1) of each exposure as the control group. A linear trend test across groups was performed by transforming the groups into continuous variables. Restricted cubic splines (RCS) were used to analyze the dose‒response association between each exposure factor and the risk of developing BC, as this method allows for the flexible modeling of non-linear relationships and helps avoid the assumptions of traditional linear models. In our analysis, all covariates were adjusted for, which provided more accurate risk estimates.
In addition, we stratified the population by age (≥ 60/ < 60), BMI (≥ 25/ < 25 kg/m2), and race (white/nonwhite) to assess whether the relationship between phenol/paraben exposure and the risk of developing BC within different subgroups would change due to stratification variables. All covariates except stratification variables were adjusted during subgroup analysis.
Subsequently, we executed a weighted quantile sum (WQS) analysis37,38, wherein we computed the weighted linear index and allocated corresponding weights to assess the impacts of exposure to combined and individual phenols/parabens on the risk of developing BC. In this study, we employed bootstrapping with 2,000 iterations to construct the WQS index, as this number provides robust estimates while maintaining computational feasibility. We then inspected the corresponding weights to ascertain the relative contribution of each exposure within the index. Similar to the weighted multivariate logistic regression analysis, we also formulated three models for the WQS analysis.
In the final analysis, a Bayesian variable selection framework was utilized to explore the overall impact of phenol/paraben exposure on BC risk. Specifically, the Bayesian Kernel Machine Regression (BKMR) model examined the impact of specific quartile exposure levels compared to the median39,40. Furthermore, a single-variable exposure‒response function was used to evaluate the individual effects of the exposure factors.
All the statistical analyses were conducted using R software (version 4.3.2). A P value < 0.05 was considered to indicate statistical significance.
Results
Population characteristics
Table 1 presents the demographic attributes of 4,455 individuals in the NHANES spanning from 2005 to 2014, with an average age of 47.52 ± 16.98 years. Of these participants, 134 were diagnosed with BC, 68.08% were non-Hispanic white, and 82.80% had attained an education level above high school. The data revealed significant disparities in age, BMI, race/ethnicity, diabetes status, hypertension status, hypercholesterolemia status, and CVD status between the BC group and the control group (p < 0.05 for all). Compared to participants without BC, those diagnosed with BC were more likely to be Non-Hispanic White, older (65.29 ± 12.84 vs. 47.00 ± 16.80 years old), and obese (BMI: 29.95 ± 6.80 vs. 28.68 ± 7.41 kg/m2).
Distribution of urine phenols and parabens metabolites
Supplementary Table S1 displays the count and percentage of metabolites below the lower limit of detection for each of the five 2-year cycles from 2005 to 2014. Except for EPB (58.92%) and BUP (54.48%), which had relatively low detection rates, the detection rates of the metabolites were considerably high (ranging from 76.39% for TRS to 99.62% for MPB). Table 2 illustrates the distribution of urinary phenol and paraben metabolite concentrations (all log10-transformed) for the NHANES participants from 2005 to 2014. Among the seven metabolites, MPB had the highest median blood drug concentration (4.86 ng/mL), followed by PPB (3.19 ng/mL) and BP3 (2.88 ng/mL), with BUP exhibiting the lowest median blood drug concentration.
Spearman correlation analysis
Spearman correlation analysis was employed to evaluate the correlations among the seven phenols/parabens, as depicted in Fig. 3. Most correlations between the metabolites were relatively weak, exhibiting mild to moderate positive associations, with correlation coefficients ranging from 0.14 to 0.45. The correlation between PPB and MPB concentrations was relatively higher, with a correlation coefficient of 0.81, and this relationship was statistically significant (p < 0.05). This indicates that the strong correlation observed between PPB and MPB is unlikely to be attributed to sampling error. The strength of the correlations between metabolites may influenced by their chemical structures and metabolic processes in the body. Both PPB and MPB belong to the paraben class of compounds, and their high correlation suggests that these two chemicals may undergo similar enzymatic transformations in liver metabolism, following comparable metabolic pathways.
Pairwise spearman correlations among the 7 log10-transformed urine phenols and parabens metabolites in the population (N = 4,455), NHANES, USA, 2005–2014. *p < 0.05, indicating that the observed correlation is statistically significant and unlikely to be due to sampling error. BPA Bisphenol A, TRS Triclosan, BP3 Benzophenone-3, MPB Methyl paraben, EPB Ethyl paraben, PPB Propyl paraben, BUP Butyl paraben.
Urine phenols and parabens metabolites and BC risk in the logistic regression model
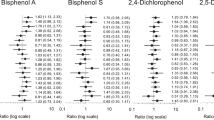
To evaluate the potential associations between log10-transformed urinary phenol and paraben metabolite concentrations and BC risk, we utilized univariate and multivariate regression models. Figure 4 indicates that in Model 1, which did not adjust for any covariates, no significant association was observed between log10-transformed TRS and BC. However, this association became significant in Models 2 and 3 (Model 2: TRS (OR = 1.10, 95% CI = 1.02–1.18, p = 0.018); Model 3: TRS (OR = 1.11, 95% CI = 1.02–1.20, p = 0.014)). Furthermore, we observed that individuals with high TRS concentrations had an increased risk of developing BC. According to the crude model, compared to that in the group with the lowest concentration, the risk of developing BC in the Q2 concentration group increased by 1.92 times (95% CI = 1.18–3.13, p = 0.009). In Model 2, which was adjusted for several covariates, compared to that in Q1, the risk of developing BC for participants in Q2 increased by 2.29 times (95% CI = 1.44–3.66, p < 0.001), and the risk for those in Q3 increased by 1.87 times (95% CI = 1.20–2.93, p = 0.007). In Model 3, which was adjusted for all covariates, the results remained robust and statistically significant. Compared to those in Q1, the risk of developing BC for participants in Q2 and Q3 increased by 2.33 (95% CI = 1.45–3.75, p < 0.001) and 1.94 times (95% CI = 1.21–3.09, p = 0.006), respectively. Linear trend analysis demonstrated that there was a significant association between log10 TRS concentrations and the risk of developing BC in multivariate regression Models 2 and 3 (see Fig. 4 for details, p for trend < 0.05 for both). We did not observe any associations between the concentrations of other metabolites and BC risk.
Multivariate logistic regression analysis of log10-transformed urine phenols and parabens metabolites for the risk of breast cancer. Data are presented as OR (95%CI). BPA Bisphenol A, TRS Triclosan, BP3 Benzophenone-3, MPB Methyl paraben, EPB Ethyl paraben, PPB Propyl paraben, BUP Butyl paraben. Model 1: Non-adjusted. Model 2: Adjusted for age, race/ethnicity, educational level, PIR, and BMI. Model 3: Adjusted for age, race/ethnicity, educational level, PIR, BMI, marriage, smoking status, alcohol consumption, and history of hypercholesterolemia, hypertension, diabetes, and CVD.
Dose–response relationship between urine phenols and parabens metabolites and BC risk
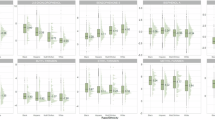
We constructed RCS to fit the logistic regression model to further scrutinize the associations between exposures and outcomes. As depicted in Fig. 5, after adjusting for all covariates, among the seven urinary phenol and paraben metabolites, only TRS exhibited a statistically significant nonlinear association with BC risk (P nonlinear = 0.007). When the log10 TRS increased from 0 to 3.51, the risk of developing BC increased to its peak with increasing TRS concentration and then decreased with increasing TRS concentrations, demonstrating an overall inverted U-shaped curve.
Restricted cubic spline fitting for the association between urine phenols and parabens metabolites and breast cancer risk. (A) Log10 BPA; (B) Log10 TRS; (C) Log10 BP3; (D) Log10 MPB; (E) Log10 EPB; (F) Log10 PPB; (G) Log10 BUP. BPA Bisphenol A, TRS Triclosan; BP3, Benzophenone-3, MPB Methyl paraben, EPB Ethyl paraben, PPB Propyl paraben, BUP Butyl paraben.
Subgroup analysis
All subgroup analyses were conducted with the lowest exposure group as the reference group, utilizing weighted multivariate logistic regression to explore whether stratified variables would impact the robustness of the results. All other covariates were adjusted during the model construction process, excluding the stratified variables. Figure 6 presents the forest plot outcomes of subgroup analyses conducted by BMI (≥25 or <25 kg/m2, Fig. 6A,B), age (<60 or ≥60 years, Fig. 6C,D), and race (white or nonwhite, Fig. 6E,F). We observed that the associations between TRS concentrations and the risk of developing BC remained consistent in the BMI≥25 kg/m2 subgroup (Q2: OR=2.63, 95% CI=1.57–4.39, p<0.001; Q3: OR=1.93, 95% CI=1.02–3.68, p=0.044), age<60 subgroup (Q2: OR=6.90, 95% CI=2.09-22.84, p=0.002; Q3: OR=3.96, 95% CI=1.08–14.46, p=0.038), and white race subgroup (Q2: OR=3.08, 95% CI=1.69–5.62, p<0.001; Q3: OR=2.38, 95% CI=1.32–4.30, p=0.005). In the BMI<25 kg/m2 subgroup, exposure to EPB (Q2: OR=3.19, 95% CI=1.47–6.93, p=0.004) and BUP (Q3: OR=2.19, 95% CI=1.09–4.42, p=0.029) also increased the risk of developing BC. In addition, in the BMI<25 kg/m2, age≥60, and nonwhite subgroups, no significant differences were detected in the levels of other urinary phenol or paraben metabolites associated with BC risk. Our findings suggest that high TRS exposure is more likely to induce BC in overweight individuals (BMI≥25 kg/m2), those under 60 years of age, and white individuals.
Association between urine phenols and parabens metabolites concentrations and breast cancer in subgroups stratified by BMI, age, and race. (A) BMI ≥ 25 kg/m2; (B) BMI < 25 kg/m2; (C) Age < 60 years old; (D) Age ≥ 60 years old; (E) White race; (F) Non-white race. The results were adjusted for all covariates except the stratified variables.
Urine phenols and parabens metabolites and BC risk in WQS model
We applied the WQS model to scrutinize the combined effect of 7 urinary phenol and paraben metabolites on the risk of developing BC. We discovered that in the WQS models adjusted for different covariates, the mixture of 7 metabolites did not exhibit any significant association with BC risk (Model 1: β = − 0.085, 95% CI = − 0.29–0.13, p = 0.428; Model 2: β = 0.066, 95% CI = − 0.17–0.30, p = 0.580; Model 3: β = 0.050, 95% CI = − 0.18–0.28, p = 0.666). Nevertheless, as illustrated in Fig. 7, in all three WQS models, the highest weight contributing to BC risk was TRS, accounting for more than 50% of the variance in each model, while all other variables also had weights in the positive direction.
The WQS model weights of urine phenols and parabens metabolites and breast cancer risk. (A) Model 1: Non-adjusted. (B) Model 2: Adjusted for age, race/ethnicity, educational level, PIR, and BMI. (C) Model 3: Adjusted for age, race/ethnicity, educational level, PIR, BMI, marriage, smoking status, alcohol consumption, and history of hypercholesterolemia, hypertension, diabetes, and CVD. WQS weighted quantile sum, BPA Bisphenol A, TRS Triclosan, BP3 Benzophenone-3, MPB Methyl paraben, EPB Ethyl paraben, PPB Propyl paraben, BUP Butyl paraben.
Urine phenols and parabens metabolites and BC risk in the BKMR model
According to the BKMR model, compared to the median risk, the risk of developing BC due to combined exposure to phenols and parabens initially increased and then decreased. However, this trend did not reach statistically significant, which is consistent with the results obtained from the WQS model (Fig. S1). A possible explanation for this is that, while TRS may independently affect BC risk, nonlinear or complex interactions between variables could obscure the overall mixed effect. As depicted in Fig. S2, when the concentrations of all other urinary phenol and paraben metabolites were maintained at the median, the association between TRS levels in the urine and BC risk exhibited an inverse U-shaped pattern. This pattern aligns with the multivariate logistic regression analysis in Fig. 4, where the OR for Q2 compared to Q1 was higher than that for Q3 compared to Q1 across all three models.
In contrast to the WQS model, the BKMR model did not emphasize the dominant role of TRS in the mixed effect. This discrepancy highlights the distinct strengths of the two methods. Specifically, BKMR is capable of capturing nonlinear interactions between variables, whereas WQS assigns greater weight to individual metabolites. This difference in methodology may account for the more pronounced independent effect of TRS observed in the WQS model.
Discussion
In this investigation, we preliminarily analyzed the associations between exposure to two classic types of EDCs, phenols and parabens, and the risk of developing BC using a nationally representative sample of adult women aged 20 and older in the United States over a 10-year period. We discovered that the detection rate of MPB in urine was the highest (99.62%), followed by that of PPB (97.51%) and BP3 (96.97%), indicating widespread exposure to these metabolites in this population. Further weighted multifactorial logistic regression analysis substantiated the speculation that exposure to certain EDCs (particularly TRSs) is associated with the risk of developing BC. We found that a higher concentration of TRS (as a continuous or categorical variable) is strongly related to an increased risk of developing BC. This association was more pronounced in overweight individuals (BMI ≥ 25 kg/m2), those under 60 years of age, and white individuals. These findings may augment our understanding of the association between exposure to EDCs and the risk of developing BC.
The endocrine regulatory effects of phenol and paraben metabolites are widely acknowledged, and their role in the development of BC has garnered much attention. For BPA, He et al. discovered that the concentration of BPA in the urine of BC patients was greater than that in the urine of healthy individuals (p < 0.001)41, and a series of studies at the level of BC cells and mouse models also confirmed the promoting effect of BPA exposure on BC24,42,43. Researchers have endeavored to explain the adverse prognostic effect of BPA on the risk of developing BC through alterations in the tumor microenvironment44 and disorders of the obesity–inflammation–aromatase axis45. However, large-sample epidemiological studies in the population are quite limited. Lizbeth’s team studied 394 histologically confirmed BC patients and 404 age-matched control participants and found that free BPA (the biological form of BPA) may be an environmental cofactor associated with the risk of developing BC46. Ayesha et al. conducted a cohort study in the Pakistani population and found a relationship between BPA exposure and the progression of BC47. However, the evidence linking BPA exposure to BC from epidemiological studies remains limited, and our findings do not support this association. This discrepancy may be attributed to differences in study design and population characteristics. A literature review and meta-analysis by Fauconnier and Liu also support our conclusion48,49, indicating that current research does not provide sufficient evidence to establish a link between BPA exposure and BC. Further studies are needed to explore this relationship more thoroughly.
In addition to BPA, a substantial number of in vitro and animal studies have linked paraben exposure to the development of BC. Roje et al. confirmed that parabens augment the proliferation of estrogen-sensitive BC cells50, and subsequent researchers discovered that MPB exposure may inflict carcinogenic damage to estrogen receptor-positive BC cells51, and that exposure to MPB and PPB induces significant progression and metastasis of BC in mice26. In terms of epidemiological research in the population, Aushev et al. identified differentially expressed genes in response to low-dose MPB exposure in a rat model and demonstrated in a cohort of 606 women with primary BC that the tumor expression of MPB response genes is related to BC mortality52. Humberto’s team reported that urinary MPB and PPB are related to an increased risk of developing BC, and after a median follow-up of 17.6 years, they reported that MPB and PPB exposure are also related to all-cause mortality53. Later, their team utilized global DNA methylation (DNAm) as an entry point, measured the promoter methylation status of 13 genes in 509 tumor samples, and found that exposure to parabens may increase the risk of developing BC in women with low DNA methylation54. These findings are inconsistent with those of Wu et al., who conducted a nested case–control study involving 1032 postmenopausal BC patients and 1,030 matched controls to investigate the relationship between EDC exposure and BC risk. Their study found a weak negative association between hydroxylated parabens and BC risk in a multi-ethnic population55. In contrast, our cross-sectional study did not reveal any significant association between parabens and the risk of BC in women over the age of 20. The differences in findings may be due to factors such as age distribution, study design, and sample size.
Several cell and animal studies have suggested that TRS may trigger endocrine disruption by affecting the distribution and metabolome of BC cells56, activating the G protein-coupled estrogen receptor signaling pathway25, and promoting the epithelial–mesenchymal transition, migration, and invasion of BC cells57. Wu et al. research revealed a weak negative association between TRS exposure and BC risk in multiethnic postmenopausal populations55. However, their study population differs from ours in terms of age, ethnicity, study design, and sample size, which may help explain the discrepancy between their findings and ours. In addition, their research also revealed that the association between TRS exposure and the risk of developing BC is observed primarily in women with overweight/obesity. Later, Mmadili’s team also emphasized that when assessing the impact of urinary TRS concentrations on the health status of women, body fat and menopausal status should be considered58. Considering these previous studies, we used race (white or nonwhite), age (< 60 or ≥ 60 years), and BMI (≥ 25 or < 25 kg/m2) as stratified variables and observed that the association between urinary TRS concentrations and the risk of developing BC remained consistent in the BMI ≥ 25 kg/m2 subgroup, age < 60 years subgroup, and white subgroup. In addition, in the BMI < 25 kg/m2 subgroup, we found that exposure to EPB and BUP also increased the risk of developing BC, which is consistent with the findings of Humberto’s research. They found that in women with a BMI < 25 kg/m2, the association between parabens and the incidence of BC is more pronounced53.
Through the preceding literature review, we discerned that research on the relationship between environmental exposure to phenols and parabens (as assessed by the presence of their metabolites in urine) and the risk of developing BC in cell and animal studies is abundant, and the conclusions are consistent. However, epidemiological studies involving large population are scarce and their findings are inconsistent. Furthermore, future studies should aim to explore the molecular and cellular mechanisms through which TRS affects BC risk, as well as investigate the critical role of body fat and metabolic processes in this pathway. Currently, for BC patients or high-risk groups for BC, when using personal care products containing phenols and parabens, they should be cautious about their ingredients.
We used both WQS and BKMR analyses to further explore the overall mixed effects and individual variable effects of multiple metabolites. These nonlinear modeling approaches are commonly employed to assess the joint effects of multiple variables, particularly to explore the combined effects of various metabolites. In our weighted multivariable logistic regression analysis, we found that TRS was significantly associated with BC risk. However, neither the WQS nor BKMR analyses revealed a statistically significant mixed effect of these metabolites is either not significant or that their interactions are nonlinear, making it difficult to capture their relationship. Such discrepancies are common in environmental health research, where different methods highlight different aspects of the effects. Future research could further investigate the interactions between these metabolites and their potential nonlinear relationships to better understand their impact on BC risk.
The strengths of this study include the use of a nationally representative sample from the NHANES over 10 years and the measurement of phenol and paraben metabolites in urine following strict quality control standards. In addition, we considered confounding factors, including demographic data, lifestyle, and comorbidity information, during the analysis process. However, several limitations of this study should also be acknowledged. First, our study was cross-sectional, so it is difficult to infer causality and temporal associations. Second, the phenol and paraben metabolite analyses were based on a single-measurement value assessment, so although the concentration of urinary metabolites reflects the chronic exposure level over a period of time, errors in the exposure assessment of nonpersistent EDCs may also be unavoidable. Third, although we considered important potential confounders in the analysis, we cannot rule out the possibility of other unmeasured confounders that may have affected the association between the concentrations of urinary metabolites and the risk of developing BC (such as other EDCs (e.g., phthalates) and drug and hormone use). Fourth, our study relied on self-reported disease status, which may be subject to recall bias or cultural influences, leading to misclassification or underreporting of cases. Future studies could address this bias by utilizing more objective disease confirmation methods, such as medical records or clinical diagnoses. Additionally, the NHANES database does not provide information on the half-life of phenol and paraben metabolites, which is influenced by factors like individual metabolism, renal function, and exposure levels. This limits our understanding of how long these metabolites remain in the body and may affect the interpretation of the relationship between urinary metabolite concentrations and BC risk. Finally, the proportion of cases in our analysis was small (3.01%, with 134 cases out of 4455 total participants), and we did not include male BC populations, primarily due to sample size limitations. This may impact the generalizability and reliability of our results. Future research should consider conducting larger-scale case–control analyses and using tightly matched controls (with the same covariates) to reduce bias and improve the accuracy and generalizability of findings.
Conclusion
Our nationwide cross-sectional analysis revealed a complex relationship between exposure to phenol and paraben metabolites and the risk of developing BC in adult women. Specifically, our research results emphasize that a higher urinary concentration of TRS (as a continuous or categorical variable) is associated with a greater risk of developing BC. However, when considering multiple metabolites comprehensively, the association between exposure to all the studied metabolites combined and the risk of developing BC was not apparent, which may be attributed to the intricate comprehensive connections between chemical mixtures. Considering the widespread exposure of the population to phenol and paraben metabolites, the precise relationships and potential mechanisms between TRS and the risk of developing BC still need to be explored and confirmed through prospective epidemiological research and in vitro and in vivo experimental research.
Data availability
The data used in this study can be accessed through the links provided in the article. Further queries can be directed to the corresponding author.
References
Trapani, D. et al. Global challenges and policy solutions in breast cancer control. Cancer Treat. Rev. 104, 102339 (2022).
Giaquinto, A. N. et al. Breast cancer statistics 2024. CA Cancer J. Clin. 74(6), 477–495 (2024).
C. Collaborative Group on Hormonal Factors in Breast, Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies, Lancet Oncol 13(11) 1141–51. (2012).
S. Loibl, F. Andre, T. Bachelot, C.H. Barrios, J. Bergh, H.J. Burstein, M.J. Cardoso, L.A. Carey, S. Dawood, L. Del Mastro, C. Denkert, E.M. Fallenberg, P.A. Francis, H. Gamal-Eldin, K. Gelmon, C.E. Geyer, M. Gnant, V. Guarneri, S. Gupta, S.B. Kim, D. Krug, M. Martin, I. Meattini, M. Morrow, W. Janni, S. Paluch-Shimon, A. Partridge, P. Poortmans, L. Pusztai, M.M. Regan, J. Sparano, T. Spanic, S. Swain, S. Tjulandin, M. Toi, D. Trapani, A. Tutt, B. Xu, G. Curigliano, N. Harbeck, E.G.C.E.a. [email protected], Early breast cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up, Ann Oncol 35(2) 159–182. (2024).
Kahn, L. G., Philippat, C., Nakayama, S. F., Slama, R. & Trasande, L. Endocrine-disrupting chemicals: implications for human health. Lancet Diabetes Endocrinol. 8(8), 703–718 (2020).
Modica, R., Benevento, E. & Colao, A. Endocrine-disrupting chemicals (EDCs) and cancer: new perspectives on an old relationship. J. Endocrinol. Invest. 46(4), 667–677 (2023).
Buoso, E., Masi, M., Racchi, M. & Corsini, E. Endocrine-disrupting chemicals’ (EDCs) effects on tumour microenvironment and cancer progression: Emerging contribution of RACK1. Int. J. Mol. Sci. https://doi.org/10.3390/ijms21239229 (2020).
Lacouture, A., Lafront, C., Peillex, C., Pelletier, M. & Audet-Walsh, E. Impacts of endocrine-disrupting chemicals on prostate function and cancer. Environ. Res. 204(Pt B), 112085 (2022).
Santaliz Casiano, A., Lee, A., Teteh, D., Madak Erdogan, Z. & Trevino, L. Endocrine-disrupting chemicals and breast cancer: disparities in exposure and importance of research inclusivity. Endocrinology https://doi.org/10.1210/endocr/bqac034 (2022).
Wan, M. L. Y., Co, V. A. & El-Nezami, H. Endocrine disrupting chemicals and breast cancer: a systematic review of epidemiological studies. Crit. Rev. Food Sci. Nutr. 62(24), 6549–6576 (2022).
Liu, H. et al. Endocrine-disrupting chemicals and breast cancer: a meta-analysis. Front. Oncol. 13, 1282651 (2023).
Nowak, K., Jablonska, E. & Ratajczak-Wrona, W. Immunomodulatory effects of synthetic endocrine disrupting chemicals on the development and functions of human immune cells. Environ. Int. 125, 350–364 (2019).
Wei, F., Mortimer, M., Cheng, H., Sang, N. & Guo, L. H. Parabens as chemicals of emerging concern in the environment and humans: A review. Sci. Total Environ. 778, 146150 (2021).
Tarafdar, A. et al. The hazardous threat of Bisphenol A: Toxicity, detection and remediation. J. Hazard. Mater. 423(Pt A), 127097 (2022).
Sanidad, K. Z., Xiao, H. & Zhang, G. Triclosan, a common antimicrobial ingredient, on gut microbiota and gut health. Gut Microbes 10(3), 434–437 (2019).
Schneider, S. L. & Lim, H. W. Review of environmental effects of oxybenzone and other sunscreen active ingredients. J. Am. Acad. Dermatol. 80(1), 266–271 (2019).
Nowak, K., Jablonska, E. & Ratajczak-Wrona, W. Controversy around parabens: Alternative strategies for preservative use in cosmetics and personal care products. Environ. Res. 198, 110488 (2021).
Hassan, S. et al. Endocrine disruptors: Unravelling the link between chemical exposure and Women’s reproductive health. Environ. Res. 241, 117385 (2024).
Sotelo-Orozco, J. et al. Exposure to endocrine disrupting chemicals including phthalates, phenols, and parabens in infancy: Associations with neurodevelopmental outcomes in the MARBLES study. Int. J. Hyg. Environ. Health 261, 114425 (2024).
Liu, W. et al. Parabens exposure in early pregnancy and gestational diabetes mellitus. Environ. Int. 126, 468–475 (2019).
Yoon, L. S. et al. Variability in urinary phthalates, phenols, and parabens across childhood and relation to adolescent breast composition in Chilean girls. Environ. Int. 170, 107586 (2022).
Kim, J. & Chevrier, J. Exposure to parabens and prevalence of obesity and metabolic syndrome: An analysis of the Canadian health measures survey. Sci. Total Environ. 713, 135116 (2020).
Wesselink, A. K. et al. Urinary concentrations of phenols, parabens, and triclocarban in relation to uterine leiomyomata incidence and growth. Fertil. Steril. 116(6), 1590–1600 (2021).
Torres-Alamilla, P., Castillo-Sanchez, R., Cortes-Reynosa, P., Gomez, R. & Perez Salazar, E. Bisphenol A increases the size of primary mammary tumors and promotes metastasis in a murine model of breast cancer. Mol. Cell Endocrinol. 575, 111998 (2023).
He, T. T. et al. Triclocarban and triclosan promote breast cancer progression in vitro and in vivo via activating G protein-coupled estrogen receptor signaling pathways. Sci. Total Environ. 931, 172782 (2024).
Tong, J. H. et al. Chronic exposure to low levels of parabens increases mammary cancer growth and metastasis in mice. Endocrinology https://doi.org/10.1210/endocr/bqad007 (2023).
Curtin, L. R. et al. National health and nutrition examination survey: sample design, 2007–2010. Vital Health Stat. 2(160), 1–23 (2013).
Xu, X. et al. Phthalate exposure and markers of biological aging: The mediating role of inflammation and moderating role of dietary nutrient intake. Ecotoxicol. Environ. Saf. 281, 116649 (2024).
Cathey, A. L. et al. Exploratory profiles of phenols, parabens, and per- and poly-fluoroalkyl substances among NHANES study participants in association with previous cancer diagnoses. J. Expo Sci. Environ. Epidemiol. 33(5), 687–698 (2023).
Zhou, X., Ye, X. & Calafat, A. M. Automated on-line column-switching HPLC-MS/MS method for the quantification of triclocarban and its oxidative metabolites in human urine and serum. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 881–882, 27–33 (2012).
Bell, B. C., Zhu, J. & Wei, Y. Urinary concentrations of endocrine-disrupting metals and prevalent breast cancer in US women. Biol. Trace Elem. Res. 201(9), 4230–4237 (2023).
Deng, Z. et al. Association between parity and female mortality: the mediative role of depressive symptoms. Hum. Reprod. 39(10), 2341–2352 (2024).
Gao, X. et al. Combined influence of nutritional and inflammatory status and breast cancer: findings from the NHANES. BMC Public Health 24(1), 2245 (2024).
Cai, Y., Zhaoxiong, Y., Zhu, W. & Wang, H. Association between sleep duration, depression and breast cancer in the United States: a national health and nutrition examination survey analysis 2009–2018. Ann. Med. 56(1), 2314235 (2024).
Stekhoven, D. J. & Buhlmann, P. MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 28(1), 112–118 (2012).
Deng, Z. M. et al. The clinical value of miRNA-21 in cervical cancer: A comprehensive investigation based on microarray datasets. PLoS ONE 17(4), e0267108 (2022).
Carrico, C., Gennings, C., Wheeler, D. C. & Factor-Litvak, P. Characterization of weighted quantile sum regression for highly correlated data in a risk analysis setting. J. Agric. Biol. Environ. Stat 20(1), 100–120 (2015).
Czarnota, J., Gennings, C. & Wheeler, D. C. Assessment of weighted quantile sum regression for modeling chemical mixtures and cancer risk. Cancer Inform. 14(Suppl 2), 159–171 (2015).
Lu, Y. et al. Exposure to multiple trace elements and miscarriage during early pregnancy: A mixtures approach. Environ. Int. 162, 107161 (2022).
Zhang, Y. et al. Association between exposure to a mixture of phenols, pesticides, and phthalates and obesity: Comparison of three statistical models. Environ. Int. 123, 325–336 (2019).
He, H. et al. Urinary bisphenol A and its interaction with CYP17A1 rs743572 are associated with breast cancer risk. Chemosphere 286(Pt 3), 131880 (2022).
Liu, J. et al. Bisphenol P and bisphenol M promote triple-negative breast cancer metastasis through activation of AKT pathways. Sci. Total Environ. 892, 164748 (2023).
Deng, P. et al. Bisphenol A promotes breast cancer cell proliferation by driving miR-381-3p-PTTG1-dependent cell cycle progression. Chemosphere 268, 129221 (2021).
Kwon, Y. Potential pro-tumorigenic effect of bisphenol A in breast cancer via altering the tumor microenvironment. Cancers (Basel) https://doi.org/10.3390/cancers14123021 (2022).
Engin, A. B. & Engin, A. The effect of environmental Bisphenol A exposure on breast cancer associated with obesity. Environ. Toxicol. Pharmacol. 81, 103544 (2021).
Lopez-Carrillo, L., Merida-Ortega, A., Gomez-Ruiz, H., Hernandez-Garciadiego, L. & Gamboa-Loira, B. Exposure to bisphenol A and breast cancer risk in northern Mexican women. Int. Arch. Occup. Environ. Health 94(4), 699–706 (2021).
Ishtiaq, A. et al. A cohort study investigating the role of Bisphenol A in the molecular pathogenesis of breast cancer. J. Cancer Res. Clin. Oncol. 149(16), 14565–14575 (2023).
Fauconnier, M. B. et al. Bisphenol A and breast cancer: State of knowledge and meta-analysis. Bull. Cancer 110(2), 151–159 (2023).
Liu, G. et al. The association of bisphenol A and phthalates with risk of breast cancer: A meta-analysis. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph18052375 (2021).
Roje, Z. et al. Synergistic effects of parabens and plastic nanoparticles on proliferation of human breast cancer cells. Arh. Hig. Rada. Toksikol. 70(4), 310–314 (2019).
Elsehly, W. M. et al. The potential implications of estrogenic and antioxidant-dependent activities of high doses of methyl paraben on MCF7 breast cancer cells. J. Biochem. Mol. Toxicol. 36(5), e23012 (2022).
Aushev, V. N. et al. Tumor expression of environmental chemical-responsive genes and breast cancer mortality. Endocr. Relat. Cancer 26(12), 843–851 (2019).
Parada, H. Jr. et al. Urinary concentrations of environmental phenols and their associations with breast cancer incidence and mortality following breast cancer. Environ. Int. 130, 104890 (2019).
Parada, H. Jr. et al. Urinary parabens and breast cancer risk: Modification by LINE-1 and LUMA global DNA methylation, and associations with breast cancer defined by tumor promoter methylation status. Mol. Carcinog. 61(11), 1002–1015 (2022).
Wu, A. H. et al. Risk of breast cancer and prediagnostic urinary excretion of bisphenol A, triclosan and parabens: The multiethnic cohort study. Int. J. Cancer 149(7), 1426–1434 (2021).
Gopalakrishnan, K. et al. Changes in mammary histology and transcriptome profiles by low-dose exposure to environmental phenols at critical windows of development. Environ. Res. 152, 233–243 (2017).
Chen, J. et al. Spatial metabolomics and lipidomics reveal the mechanisms of the enhanced growth of breast cancer cell spheroids exposed to triclosan. Environ. Sci. Technol. 57(29), 10542–10553 (2023).
Ilozumba, M. N., Shelver, W. L., Hong, C. C., Ambrosone, C. B. & Cheng, T. D. Urinary concentrations of triclosan, Bisphenol A, and brominated flame retardants and the association of triclosan with demographic characteristics and body fatness among women with newly diagnosed breast cancer. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph19084681 (2022).
Funding
This research was supported by grants from the Interdisciplinary Innovative Talents Foundation from Renmin Hospital of Wuhan University (JCRCFZ-2022-015); the Fundamental Research Funds for the Central Universities (2042019kf0229); the Natural Science Foundation of Hubei Province, China (2023AFB701); the Fundamental Research Funds for the Central Universities (2042023kf0020); the Open Project of Hubei Key Laboratory (2023KFZZ008).
Author information
Authors and Affiliations
Contributions
Yao Xiong and Zhiyu Li contributed to the conceptualization and design of the study. Zixuan Luo, Kaixin Zhong and Jiawei Hu collected and initially screened the data. Yao Xiong and Xiong Xiong performed a visual analysis of the data and was the main contributor to the manuscript. Chuang Cheng and Shengrong Sun supervised and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xiong, Y., Li, Z., Xiong, X. et al. Associations between phenol and paraben exposure and the risk of developing breast cancer in adult women: a cross-sectional study. Sci Rep 15, 4038 (2025). https://doi.org/10.1038/s41598-025-88765-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-88765-z