Abstract
Bodyweight loss is a common occurrence in Nasopharyngeal Carcinoma (NPC) patients during Radiotherapy (RT). Previous studies found that the prognostic value of percentage weight loss (pWL) during RT is not credible. We aimed to develop a novel progression predictor surrogated to pWL by modelling all bodyweight records measured during the treatment interval. This retrospective study included two independent hospitals of 624 patients. The Predicted Progression Probability (PPP) was obtained from deep learning-guided differential equation solution, model by the patient’s age, sex, body height, and the weekly measured bodyweight records. The performance of PPP in predicting disease progression was assessed, its association with prognosis and adjuvant chemotherapy response was evaluated. The PPP was learnt from the training cohort (N = 257) with 7 weeks of bodyweight records. The prediction performance was validated with 367 patients of the testing cohort sub-divided according to the number of bodyweight records found. The area under of curve for patients with 7 weeks (N = 155), 6 weeks (N = 176), and 5 weeks bodyweight records (N = 32) were 0.76, 0.73, and 0.95 respectively. PPP was significantly associated with progression-free and remained an independent prognostic factor adjusting for clinicopathologic variables in multivariate analysis in all study cohort (adjusted hazard ratio [HR] range: 2.50–7.04, all p < 0.001). Patients with high-PPP derived progression benefit from adjuvant chemotherapy (HR: 0.41–0.54, all p < 0.03), whereas those with low-PPP did not for both cohorts. The trajectory of bodyweight change during RT is more robust than the pWL to give a progression prediction after RT. The PPP is a reliable predictor for estimating the risk of residual diseases after RT course, which also helps to predict adjuvant chemotherapy response in locally advanced NPC patients.
Similar content being viewed by others
Introduction
Owing to the deep-seated anatomic ___location of Nasopharyngeal Carcinoma, radiotherapy (RT) has been the mainstay and primary curative treatment choice as compared to surgical removal1. On the same side, bodyweight loss (WL) was commonly found in patients during RT due to the unavoidable damage of irradiation at the head and neck region2,3,4,5,6. Therefore, monitoring the patients’ bodyweight during RT becomes a common practice for playing a critical role in post-RT decision-making, example of RT-replanning, nutrition support, and deciding adjuvant chemotherapy2,7,8,9,10,11,12,13. The post-RT percentage weight loss (pWL) straightforwardly quantitates the toxicity on patient caused by treatment. Despite extensive research found the association between disease progression and pWL during RT, due to the variation of timepoint defined for pWL, results are not consistent enough to give a generalized prediction of patient’s prognosis11,14,15,16,17,18,19,20,21. Recent studies have also found that the reported pWL varied significantly by study times and region, suggesting the pWL is not a specific indicator to characterize a patient’s unique treatment response or predict prognostic outcomes22,23.
Radiation toxicities increase as a process during the treatment but not as an event, and so does the bodyweight changes. However, the pWL only characterizes the difference between initial bodyweight to a single endpoint bodyweight. To date, there is no study that has been working on the association between a series of bodyweight changes during treatment and the prognosis. It is because the patient’s bodyweight is not necessarily recorded in a regular manner for all patients and possibly with missing measurement during the whole treatment. Irregular-time sampling and partially observed data posed two major challenges of analyzing the time-series bodyweight record.
A new family of neural networks has attracted our attention, the Neural Ordinary Differential Equation (Neural ODE), that provides an approximated solution of differential equations with a black-box differential equation solver24. In our case, the model learns to predict the patient’s ‘prognosis by his initial bodyweight and the trajectory of bodyweight changes based on all records during the treatment. Recently a more elegant approach of handling irregular sampled partially observed data is the Neural Controlled Differential Equation (Neural CDE). It takes a continuous time differentiable function as input, that is constructed from the irregular sampled time series data, allowing data to be interpolated from the sampling interval25. This ideally resolves the modeling challenge of bodyweight records.
Based on the observed prognostic value of the pWL in RT, we hypothesize that the patient’s prognosis can also be revealed by his rate of bodyweight change during RT, by considering all bodyweights measured during the treatment interval at once. The purpose of this study is divided into twofold: (i) develop a Predicted Progression Probability (PPP) from the bodyweight series, and (ii) validate its ability in predicting progression and response to adjuvant chemotherapy. This study aims to provide a novel, independent post-RT predictor in terms of the rate of bodyweight change, surrogated to the pWL which is about the amplitude of bodyweight change, for disease progression. On top of that, we also aim to provide decision-guiding of adjuvant chemotherapy on NPC patients after RT by this predictor.
Method and material
Study design and patients
This retrospective study included 624 patients with primary histologically confirmed NPC as the primary tumor who underwent radiotherapy from 2012 to 2018, with their last follow-up between 2014 to 2021 at Hospital A (N = 257) and Hospital B (N = 367). All patients are treated with Intensity-modulated radiation therapy (IMRT) according to their institutional practice, with detailed information provided in Supplementary Note 1a. Demographic information, including staging, sex, age, treatment arm, pretreatment performance status grade (Eastern Cooperative Oncology Group [ECOG]), pretreatment Epstein-Barr virus (EBV) DNA test, body height, and time-series bodyweight data during RT were collected. The EBV DNA test was considered as positive for patient whose either blood EBV DNA load > 20 copy/ng or serum VCA-IgA titer > 1:5 otherwise negative. Patients coexisting with other tumors, M1 stage, and withdrawn treatment during RT were excluded from the study. Most patients’ bodyweight was measured in a weekly manner since the start day of RT but not all, therefore the number of days from RT start to measurement was also collected for each bodyweight record. The percentage weight loss (pWL) of patients was calculated from the last measured bodyweight during the RT period. Samples from Hospital A were regarded as the training cohort for fitting the prediction model and samples from Hospital B were regarded as testing cohort for externally validating the results. The starting time of all survival rate in this study was defined as the end of RT day. Progression-free Survival (PFS) was defined as the time from starting time to either date of disease progression or death from any cause.
Constructing progression prediction probability from time series patient’s record
Suppose the patient’s records were fully observed during the RT treatment but possibly measured at irregular timepoints \(\text{x}=(\left({t}_{0}{\text{x}}_{0}\right),\left({t}_{1}{\text{x}}_{1}\right),\left({t}_{2}{\text{x}}_{2}\right),\dots ,\left({t}_{n}{\text{x}}_{n}\right))\), with \(t_{0} < \cdots < t_{n}\) and each \({t}_{i}\in {\mathbb{R}}\) the timepoint of patient’s records \({\text{x}}_{0}\in {\mathbb{R}}^{\upsilon }\), where \(\upsilon\) is the number of measurements on each record. In our task we had \(\upsilon =5\) corresponding to one-hot sex labels, age (year), body height (m), and bodyweight (kg) measured on each timepoint during RT. Let a controlled system \(\text{\rm X}:\left[{t}_{0},{\text{t}}_{n}\right]\to {\mathbb{R}}^{\upsilon +1}\) to be the natural cubic spine with knots at \({t}_{0}, {t}_{1}, .., {t}_{n}\). Here the patient record \(\text{x}\) was assumed to be an observed discretization of patient’s bodyweight change process during RT, and \(\text{\rm X}\) is the approximation of this underlying process with \({\text{\rm X}}_{{t}_{i}}=({\text{x}}_{i},{t}_{i})\). Noted that the controlled system \(\text{\rm X}\) is not just a bounded variation of patients’ bodyweight during RT but also differentiable, therefore the missing value of patients ’bodyweight can be approximated by interpolation.
Let a neural network \({{L}_{input}}_{\theta }:{\mathbb{R}}^{\upsilon +1}\to {\mathbb{R}}^{\omega }\) that linearly projecting the input to latent state, where \(\omega\) is a hyperparameter that describe the size of the latent state. Let a learnable function \({f}_{\theta }: {\mathbb{R}}^{\omega }\to {\mathbb{R}}^{\omega \times (\upsilon +1)}\) be any neural network that used to equate the changing of latent state variables from \({z}_{{t}_{i}}\) to \({z}_{{t}_{i+1}}\), with the initial latent state \({z}_{{t}_{0}}\) calculated from the first measurements \({{L}_{input}}_{\theta }({t}_{0}{\text{x}}_{0})\). Then, the final latent state can be calculated by integrating the initial latent state to the final latent state:
where \({t}_{n}\) is the measurement time of the final bodyweight record. Lastly, let a sigmoid classifier \({{L}_{output}}_{\theta }:{\mathbb{R}}^{\omega }\to [0, 1]\) to be any neural network that linearly projecting the final latent state variables \({z}_{n}\) to the predicted progression probability (Model architecture and training specifications were provided in Supplementary Note 2).
Preprocessing the clinical variables
Considering only the patient’s bodyweight were changing and measured periodically during the RT, the sex, age and height variables of the patient remained constant. L2 normalization was first performed on these constants to ensure the feature robustness and then copied their values to each bodyweight measurement. For batching samples with different number of measurements before constructing the controlled system, the last measurement \(\left({t}_{n}{\text{x}}_{n}\right)\) was padded forward until all samples in the same batch have the same input length.
Statistical analysis
T-test was used to compare two continuous variables and chi-square test was used to compare categorical variables. The classification performance of the model was indicated by the Receiver Operating Characteristics Curve (ROC curve) with area under the curve (AUC). The prognostic value of PPP for all patients were evaluated in each cohort, additionally with subgroups defined by clinicopathological factors.
Survival curves were generated by Kaplan–Meier method and compared by log-rank test. Univariate and multivariable analyses were performed under Cox regression. The association between the PPP and various clinical factors were assessed by the Cox model. A two-sided p < 0.05 was considered significant. A 95% confidence interval was provided with hazard ratio.
Results
Clinical characteristics
Table 1 lists the detailed characteristics of clinicopathological, bodyweight changes during RT, and progression event after RT of the patients in training (N = 257) and testing (N = 367) cohorts. Of the total 624 patients included in the study, the median (range) age was 54.0 (18–89) years with men (76.9%) as the majority. More than 70% of the patients had an advanced stage NPC, underwent concurrent-chemoradiotherapy (N = 545, 87.3%). 23.3% (N = 146) of the patients received Induction chemotherapy before RT commenced, and 27.9% (N = 174) of the patients received adjuvant chemotherapy after RT. The time series bodyweight of patients was found in seven records during RT in both cohorts corresponding to each week measurement. The number of bodyweight record found, median bodyweight (kg) value, and the median measured time from RT start of each cohort are provided in Table 1. There were 2 (< 1%), 2 (< 1%), 5 (2%), and 5 (2%) missing bodyweight records at the 4th, 5th, 6th and 7th week measurement in training cohort. There were 2 (0.5%), 4 (1%), 36 (9.8%), and 212 (57.8%) missing bodyweight records at the 4th, 5th, 6th and 7th week measurement in testing cohort. The median follow time (std.) was 30.4 (21.5) months in the training cohort and 52.7 (26.0) months in the testing cohort. The percentage of progression happened within 5 years were 22.2% and 30.2% in training and testing cohort, with a median time to event 13.7 months and 13.2 months respectively.
Development and validation the prognostic prediction probability (PPP)
The model was developed by mapping the bodyweight measured at irregular time points during RT to the 5-years progression event label in training cohort. 98% (N = 252) of the training samples have 7 weeks bodyweight records as input, with the area under ROC curve (AUC) of 0.84 (Fig. 1a). The PPP provided a robust prediction to either 1-, 3- or 5-years Progression, with AUC of 0.72, 0.76, 0.75 respectively in testing cohort (N = 367, Fig. 1a). The testing cohort was also divided into sub-cohorts according to the number of bodyweight records found, for evaluating the model’s ability in handling various length measurements. The AUC of testing sub-cohort samples with 7 weeks bodyweight records (N = 155) was 0.76, 6 weeks bodyweight records (N = 176) was 0.73, and 5-weeks bodyweight records (N = 32) was 0.95 as shown in Fig. 1b, suggesting the robustness of model. Additionally, prediction performance showed similar precision in terms of local recurrence (LR), regional recurrence (RR), distant metastasis (DM), and RIP event in the training and testing cohort, respectively (ROC curves in Supplementary Fig. 3). The mean PPP of the progression occurred patients (42% and 40%) was significantly higher than the no progression patients (28% and 31%) for both cohorts shown in Fig. 1c and d (all p < 0.001). However, there was no statistically significant difference of the pWL for progression occurred patients (8.70% and 9.22%) and no progression patients (8.43% and 8.70%) for the training (p = 0.636) and testing cohort (p = 0.295) as shown in Fig. 1e and f.
The Receiver-operating characteristic (ROC) curves of the PPP in predicting disease progression in the training (A) and testing (B) cohort. The distribution of PPP in the training (C) and testing (D) cohort. The distribution of pWL in the training (E) and testing (F) cohort, with p-value of the T-test indicated.
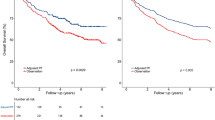
Prognostic value of progression prediction probability
The cut-off of dichotomizing the high-risk groups was PPP > 31.9% according to the highest Youden Index (J = 0.544) in training cohort. The prognostic value of PPP was assessed according to the threshold. For the high-risk groups, the 5-years PFS were 53.1% and 60.5% respectively in training and testing cohort; for the low-risk groups, the 5-years PFS were 82.5% and 97.5% respectively in training and testing cohort. Log-rank test showed significant difference of the progression-free rate in both training (p = 0.002) and testing cohort (p = 0.039), respectively in Fig. 2. Substantial log-rank tests have confirmed that significant difference could also be found in the local recurrence-free survival, regional recurrence-free survival, distant metastasis-free survival, and overall survival of patients stratified by PPP based on the same value (Survival curves in Supplementary Fig. 4).
Univariable and multivariable cox analysis
Univariable Cox regression analysis of the PPP and common clinical risk factors were shown in Table 2. PPP stratification was a significant risk factor for 5-year progression in both training (p < 0.001, HR = 7.32[3.87–13.86]) and testing cohort (p < 0.001, HR = 2.66[1.72–4.11]). In the training cohort, age > 65 (p = 0.038, HR = 1.89[1.03–3.47]), Advanced T stage (p = 0.027, HR = 1.89[1.03–3.47]), and performed induction chemotherapy (p < 0.001, 3.07[1.81–5.21]) was significantly associated with disease progression. In the testing cohort, advanced T stage (p = 0.023, HR = 2.44[1.13–5.24]) and post-RT pWL > 10% (p = 0.044, HR = 1.46[1.01–2.14]) was significantly associated with progression. Multivariable cox regression analysis was performed on the PPP adjusting for clinicopathological variables shown in Table 3. The PPP remained a powerful prognostic factor for predicting the 5-years PFS in training (p < 0.001, HR = 7.82[3.66–16.71]) and testing (p < 0.001, HR = 3.32[1.46–7.58]) cohort. Additional Cox analysis found that the progression rate was significantly higher in male than female in the high-risk PPP group, with hazard ratio of 2.55 (95%CI = 1.08–6.07, p = 0.027) observed in the training cohort and 1.86 (95%CI = 1.10–3.14, p = 0.018) observed in the testing cohort. However, the statistical significance cannot be observed in the low-risk PPP group according to sex (Fig. 3a). Similar results could also be observed with patient who underwent induction chemotherapy before RT, which significantly tended to have a worse prognosis than patients who did not underwent induction chemotherapy, suggesting the independent prognostic value of PPP (Fig. 3b). On the other hand, the post-RT pWL was only marginally significant to PFS in training cohort (p = 0.072, HR = 0.59[0.33–1.04]) and not significant in testing cohort (p = 0.278) under multivariable Cox regression. The partial effects of the covariates PPP and pWL inside the multivariable Cox model (Table 3) were demonstrated respectively Supplementary Plots 5, PPP is more indicative for stratifying progression risk.
Predictive value of PPP for adjuvant chemotherapy response
It was found that adjuvant chemotherapy was associated with an improved prognosis for high-risk PPP group, shown in Fig. 3c, with hazard ratio of 0.41 (95%CI = 0.21–0.78, p = 0.005) found in the training cohort and 0.54 (95%CI = 0.30–0.95, p = 0.030) in the testing cohort. However, the adjuvant chemotherapy did not provide significant prognosis benefit in the low-risk PPP group according to Cox model, for both training (HR = 0.79[0.25–2.53], p = 0.451) and testing cohort (HR = 1.39[0.59–3.28], p = 0.690), respectively.
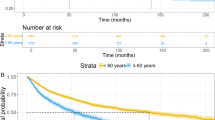
Additional analysis on the rate of bodyweight changes over time
To have a more intuitive understanding of the association between bodyweight dynamics and progression, the rate of bodyweight changes over time (kg/day) within every bodyweight measurement interval of the progression and no progression patients was plotted in Fig. 4. Patients with progression and patients without progression had experienced similar weight loss rate during the first interval (week 1 to 2) and last two intervals (week 5 to 6, week 6 to 7). However, for patients with progression, they tended to have a significantly higher weight loss rate than the non-progressed patient (more negative) during week 2 to 3 (-0.096 vs -0.059, p = 0.011) and week 3 to 4 (-0.157 vs -0.129, p = 0.041). We also observed that the PPP was significantly, positively correlated with a higher weight loss rate from week 1 to week4, but negatively correlated with a higher weight loss rate from week 5 to week 7 (A detailed description table of this weight loss rate was provided in Supplementary Table 6).
Line plots of the rate of patient’s bodyweight change (kg/day) of every bodyweight measurement interval during the RT course. Most patients experienced weight loss during RT (negative value), with orange line reflected the weight loss rates of patient without progression, and blue line reflected the weight loss rates of patient with progression, respectively. A p-value of T-test was provided for comparing the distribution of weight loss rate in each interval.
Discussion
Due to the induced radiation toxicity on upper gastrointestinal tract, a significant pWL after RT is not only common for NPC patients but generally to all head-and-neck (HNC) and lung cancer patients4,17,26,27. Currently, there is limited knowledge about the dynamics changes of bodyweight during RT16. To our best knowledge, we performed the first-of-its-kind study that utilized a series of bodyweight records during RT to estimate the progression probability, and validated the generalizability of this novel predictor to various survival outcomes in an external cohort. Further analysis confirmed the prognostic value of PPP was independent from common clinicopathological factors. More importantly, we found that the PPP could also predict the adjuvant chemotherapy response for all patients in our study cohorts.
Percentage weight loss (pWL) indicates the amplitude of weight loss during RT, is a well-known negative prognostic factor to NPC patients, but might not be specific enough to give an event prediction. Li et al.’s work is the only study we found, that utilized patient’s post-RT pWL to give a mortality prediction, with pWL cut-off at 5.4% yielded a prediction AUC of 0.623 from a cohort of 322 NPC patients28. The pre-treatment BMI is another prognostic indicator focused by previous studies, with most studies found that the higher BMI was associated with longer survival in NPC patients29,30,31,32. However, such pattern has also been frequently observed in other cancer prognosis study, known as the ‘BMI paradox’33. Recent studies had claimed that the BMI is not a creditable predictor in cancer prognosis as it neither distinguish muscle from adipose tissue, nor describe adipose tissue distribution34. Low muscle mass is known to be strongly associated with higher risk of recurrence, treatment-related toxicities, and cancer-specific mortality. As a result, patient with who are overweight have on average higher levels of muscle than their normal-weight counterparts were often found to have better prognosis35. This idea was further supported by He et al. study, which found that the visceral adipose tissue (VAT) was the only independent prognostic body composition factor in locally advanced NPC comparing with BMI, subcutaneous, or intra muscular adipose tissue36. However, these body compositional parameters are less frequently and more complicated to be periodically measured comparing to patient’s bodyweight. Therefore, considering the continuous changes of patient’s body condition during the treatment in this study, the vulnerability of a patient to disease progression can be more reasonably characterized by the rate of bodyweight changes. Here the model treats this prediction task as an initial value problem, that firstly estimated a progression rate based on patient’s initial body records, and further adjust the progression rate based on the change of body record during RT. Despite we did not observe a significant association between pWL and progression outcome (Fig. 1e and f), the rate of bodyweight change indicated by PPP could successfully predict to each progression event and outperformed the previous mortality prediction (Results in Supplementary Fig. 3). In contrast to the pWL defined on a single endpoint day, we incorporated multiple timepoints data to form a continuous rough path, this not only provide richer information for model to learn, the continuously defined dynamics can also naturally incorporate data arrived at any arbitrary times for the ease of validation and implementation on individual patient.
We must notice that the PPP was a projection score not directly from the patient’s bodyweight records, but from the high dimensional latent space manipulated from the patient’s bodyweight records. Although it is hard to directly visualize the association between the bodyweight dynamics and progression risk in terms of PPP, more intuitive ideas can be found when surrogating the PPP with bodyweight loss rate, that is the value of the negative slope of patient’s bodyweight change over time. Interestingly, for the patients with progression, they tended to experience a significantly higher weight loss rate than those who had no progression during the second week to fourth week of RT course (Fig. 4). This phenomenon could be elucidated by previous explanations about the association of weight loss and poor prognosis. Weight loss is a common tool to determine the development of malnutrition, which would weaken several human defense mechanisms thus promoting susceptibility to infection and compromising the response to malignancy15,16,17,18. Therefore, an early detection of high weight loss rate may indicate a more vigorous systemic inflammatory happened inside body, that this induced physiologic alternation was found to facilitate tumor development, invasion, and metastasis37,38. Here, we would like to highlight the rate of bodyweight changes during RT might be more indicative (Supplementary Plots 5) and informative for evaluating a patient’s prognosis, compared with the amplitude of bodyweight change during RT (pWL).
Another hypothetical explanation of the correlation between PPP and disease progression is tackled from the physiological changes of NPC during relapse. Recurrent NPC is defined as tumor relapse after achieving complete remission with RT, and further invade locally, regionally, and systemically39. NPC is an exquisitely radio-sensitive tumor, that the radio-resistance development of NPC during radiation course was identified as the main culprit of tumor recurrence40. Specifically, the epithelial-to-mesenchymal transition (EMT) process of tumor cell was proved to be strongly associated with the radio-resistance development and disease progression of NPC41. During EMT, tumor cell will switch its metabolic pathway from mitochondrial oxidative phosphorylation to cytosolic glycolysis, consuming tremendous amount of energy to support growth and creating immunosuppressive tumor microenvironment to evade immunity42,43. The EMT process was also known as the fundamental of NPC metastasis and responsible for the poor response to monoclonal antibodies used in chemotherapy44. Therefore, it is reasonable to hypothesize that the body immune system is keep acting against the radio-resistance development of tumor cell during RT, to prevent energy reserves consumed for tumor growth. Patient who failed to counteract against the systemic burden created by tumor EMT would experience a higher degree and rate of bodyweight loss during RT. This hypothesis could explain our observation that patient who had disease progression were experienced a higher bodyweight loss rate during week 2–4 than patient without disease progression. The rate (acceleration/deceleration) of body compositional changes during treatment might be worth to be investigated with the prognosis of NPC patients.
The additional courses of adjuvant cisplatin-fluorouracil (PF) aim to prevent disease recurrence by eradicating microscopic cancer cells. However, patients usually exhibit poor nutritional status by the end of RT course, managing toxicities associated with this regimen is challenging45. Therefore, the efficacy of the adjuvant chemotherapy (AC) remained controversial for its benefit in controlling locally advanced NPC46,47,48. The benefit of AC was suggested to be proportional to the risk of residual disease persisting after definitive treatment, supported by retrospective reports in which patients with N3 stage were often found to be beneficial from AC, but not in other N stages47,49. Here the PPP may be more valuable than N stage as a stratification factor for determining AC regimen, considering its predictive ability to all survival outcomes is came from the post-RT evaluation of patient’s bodyweight. Additionally, the significant survival benefits of AC regimen compared to non-AC regimen found in the high-PPP patients but not the low-PPP patients could be explained by the correlation between rate of bodyweight changes over time and the PPP values (Supplementary Table 6). Under Pearson correlation test, the PPP was found to be positively correlated with the weight loss rate at the first four weeks during the RT course, while it was negatively correlated with the weight loss rate at the last two weeks before RT end. That is, patients with mild bodyweight loss rate at the end of RT are more likely to be classified as high-PPP (PPP > 0.316) compared to patients with high bodyweight loss rate at the end of RT. Thus, these high-PPP patients tend to have a better body condition to overcome the additional compliances caused by AC, whereas low-PPP patients do not, as they experienced a higher magnitude of weight loss rate at the end of treatment than the first few weeks of RT course.
The main limitation of this study is the retrospective nature, that we could only consider the bodyweight changes during the radiation course from the available data. Indeed, there are many useful biomarkers that characterize the patient’s condition and are continuously monitored during RT, examples of Epstein-Barr Virus (EBV) level, liver-renal functions, and various blood profiles. The model can process these irregular-time measured variables, possibly allowing a more generalized prediction performance. We address this by using an independent cohort with larger sample size to validate the prediction reproducibility. The demographic bias of two study cohorts also posed limitation onto this study. Patient underwent either RT-alone, CCRT, with or without neoadjuvant chemotherapy were considered as a single cohort for modelling and analysis. Chemotherapy is known to add extra systemic burden on patient during or before the radiation course. Common acute complications including nausea, vomiting, and sore mouth will further dampen the patient’s swallowing ability, that susceptibly lead to higher weight loss. The extra toxicities of chemotherapeutic agent are not considered in this study. On top of that, all patients included from two hospitals were southern Chinese. Dietary habits, cultural, and psychological factors varied regionally and ethnically, which would affect the degree of patient’s weight loss and the willingness of eating during RT. The prediction reliability of model may be reduced if abovementioned factors of testing samples were significantly different from the study’s sample. Another limitation is the selection bias of clinicians, that the decision about AC was not randomized in this study. Although we observed the predictive ability of PPP in adjuvant chemotherapy response from two cohorts, further confirmation should be assessed in prospective, randomized clinical trials in diverse populations.
Conclusion
In conclusion, we utilized a new deep learning model architecture and demonstrated its ability in modeling time-series bodyweight records to predict progression. The predictive and prognostic ability of the rate of bodyweight change during RT is prominent, and outperformed the amplitude of bodyweight change (pWL). Apart from bodyweight, many of the clinical variables are also intrinsically changing in dynamics and being recorded as series. We would like to highlight the temporality of these clinical data may potentially provide a more precise and generable association to the study endpoint.
Data availability
Research data and code are stored in an institutional repository and will be shared upon request to the corresponding author.
References
Sun, X.-S., Li, X.-Y., Chen, Q.-Y., Tang, L.-Q. & Mai, H.-Q. Future of radiotherapy in nasopharyngeal carcinoma. Br. J. Radiol. 92, 20190209 (2019).
Platek, M. E. et al. Pretreatment weight status and weight loss among head and neck cancer patients receiving definitive concurrent chemoradiation therapy: Implications for nutrition integrated treatment pathways. Support. Care Cancer 21, 2825–2833 (2013).
Johnston, C. A., Keane, T. J. & Prudo, S. M. Weight loss in patients receiving radical radiation therapy for head and neck cancer: A prospective study. J. Parenter. Enter. Nutr. 6, 399–492 (1982).
Langius, J. A. et al. Radiotherapy on the neck nodes predicts severe weight loss in patients with early stage laryngeal cancer. Radiother. Oncol. 97, 80–85 (2010).
Ottosson, S., Zackrisson, B., Kjellén, E., Nilsson, P. & Laurell, G. Weight loss in patients with head and neck cancer during and after conventional and accelerated radiotherapy. Acta Oncol. 52, 711–718 (2013).
Qiu, C., Yang, N., Tian, G. & Liu, H. Weight loss during radiotherapy for nasopharyngeal carcinoma: A prospective study from Northern China. Nutr. Cancer 63, 873–879 (2011).
Lin, A. et al. Metabolic abnormalities associated with weight loss during chemoirradiation of head-and-neck cancer. Int. J. Radiat. Oncol. Biol. Phys. 63, 1413–1418 (2005).
Kubrak, C. et al. Clinical determinants of weight loss in patients receiving radiation and chemoirradiation for head and neck cancer: A prospective longitudinal view. Head Neck 35, 695–703 (2013).
Collins, M. M., Wight, R. G. & Partridge, G. Nutritional consequences of radiotherapy in early laryngeal carcinoma. Ann. R. Coll. Surg. Engl. 81, 376–381 (1999).
Larsson, M., Hedelin, B., Johansson, I. & Athlin, E. Eating problems and weight loss for patients with head and neck cancer: A chart review from diagnosis until one year after treatment. Cancer Nurs. 28 (2005).
Petruson, K. M., Silander, E. M. & Hammerlid, E. B. Quality of life as predictor of weight loss in patients with head and neck cancer. Head Neck 27, 302–310 (2005).
Ehrsson, Y. T., Langius-Eklöf, A. & Laurell, G. Nutritional surveillance and weight loss in head and neck cancer patients. Support. Care Cancer 20, 757–765 (2012).
Lam, S.-K., Zhang, Y., Zhang, J., Li, B., Sun, J., Liu, C. Y.-T. et al. Multi-organ omics-based prediction for adaptive radiation therapy eligibility in nasopharyngeal carcinoma patients undergoing concurrent chemoradiotherapy. Front. Oncol. 11 (2022).
Cho, Y.-W. et al. Prediction of posttreament significant body weight loss and its correlation with disease-free survival in patients with oral squamous cell carcinomas. Nutr. Cancer 65, 417–423 (2013).
Langius, J. A. E. et al. Critical weight loss is a major prognostic indicator for disease-specific survival in patients with head and neck cancer receiving radiotherapy. Br. J. Cancer 109, 1093–1099 (2013).
Jin, Y.-N. et al. The prognostic value of weight loss during radiotherapy among patients with nasopharyngeal carcinoma: A large-scale cohort study. BMC Cancer 22, 505 (2022).
Zeng, Q. et al. Critical weight loss predicts poor prognosis in nasopharyngeal carcinoma. BMC Cancer 16, 169 (2016).
Du, X.-J. et al. Value of the prognostic nutritional index and weight loss in predicting metastasis and long-term mortality in nasopharyngeal carcinoma. J. Transl. Med. 13, 364 (2015).
Nourissat, A. et al. Predictors of weight loss during radiotherapy in patients with stage I or II head and neck cancer. Cancer 116, 2275–2283 (2010).
Shen, L.-J., Chen, C., Li, B.-F., Gao, J. & Xia, Y.-F. High weight loss during radiation treatment changes the prognosis in under-/normal weight nasopharyngeal carcinoma patients for the worse: A retrospective analysis of 2433 cases. PLoS One 8, e68660 (2013).
Nazari, V., Pashaki, A. S. & Hasanzadeh, E. The reliable predictors of severe weight loss during the radiotherapy of head and neck cancer. Cancer Treat. Res. Commun. 26, 100281 (2021).
Han, P., Lee, S. H., Noro, K., Haller, J. W., Nakatsugawa, M., Sugiyama, S. et al. Improving early identification of significant weight loss using clinical decision support system in lung cancer radiation therapy. JCO Clin. Cancer Inform. 944–952 (2021).
Jager-Wittenaar, H. et al. Malnutrition in patients treated for oral or oropharyngeal cancer–prevalence and relationship with oral symptoms: An explorative study. Support Care Cancer 19, 1675–1683 (2011).
Chen, R. T. Q., Rubanova, Y., Bettencourt, J. & Duvenaud, D. Neural ordinary differential equations (2018).
Kidger, P., Morrill, J., Foster, J. & Lyons, T. Neural controlled differential equations for irregular time series (2020).
Abu Zaid, Z. et al. Weight loss in post-chemoradiotherapy head and neck cancer patients. Nutrients 14, 548 (2022).
Kiss, N., Isenring, E., Gough, K. & Krishnasamy, M. The prevalence of weight loss during (chemo)radiotherapy treatment for lung cancer and associated patient- and treatment-related factors. Clin. Nutr. 33, 1074–1080 (2014).
Li, G. et al. Vicious circle of acute radiation toxicities and weight loss predicts poor prognosis for nasopharyngeal carcinoma patients receiving intensity modulated radiotherapy. J. Cancer 8, 832–838 (2017).
Sun, X.-S. et al. Patterns of failure and survival trends in 3,808 patients with stage II nasopharyngeal carcinoma diagnosed from 1990 to 2012: A large-scale retrospective cohort study. Cancer Res. Treat. 51, 1449–1463 (2019).
Lin, X., Wang, B., Zheng, F., Fei, Z. & Chen, C. Prognostic relevance of change in body mass index in patients with nasopharyngeal carcinoma undergoing volumetric modulated arc therapy: A retrospective study. Cancer Control 29, 10732748221126936 (2022).
Jin, X. et al. Pretreatment body mass index (BMI) as an independent prognostic factor in nasopharyngeal carcinoma survival: A systematic review and meta-analysis. Nutr. Cancer 74, 3457–3467 (2022).
Du, Y. et al. Body mass index and body shape before treatment and nasopharyngeal carcinoma prognosis: A population-based patient cohort study in southern China. Int. J. Cancer 153, 290–301 (2023).
Strulov Shachar, S. & Williams, G. R. The obesity paradox in cancer-moving beyond BMI. Cancer Epidemiol. Biomark. Prev. 26, 13–16 (2017).
Caan, B. J., Cespedes Feliciano, E. M. & Kroenke, C. H. The importance of body composition in explaining the overweight paradox in cancer—counterpoint. Cancer Res. 78, 1906–1912 (2018).
Huang, P.-Y. et al. Pretreatment body mass index as an independent prognostic factor in patients with locoregionally advanced nasopharyngeal carcinoma treated with chemoradiotherapy: Findings from a randomised trial. Eur. J. Cancer 49, 1923–1931 (2013).
He, W.-Z. et al. Association of body composition with survival and inflammatory responses in patients with non-metastatic nasopharyngeal cancer. Oral Oncol. 108, 104771 (2020).
Mantovani, A., Allavena, P., Sica, A. & Balkwill, F. Cancer-related inflammation. Nature 454, 436–444 (2008).
Muliawati, Y., Haroen, H. & Rotty, L. W. A. Cancer anorexia—cachexia syndrome. Acta Med. Indones. 44, 154–162 (2012).
Li, J.-X., Lu, T.-X., Huang, Y. & Han, F. Clinical characteristics of recurrent nasopharyngeal carcinoma in high-incidence area. Sci. World J. 2012, 719754 (2012).
Zhang, J., Hu, Z., Horta, C. A. & Yang, J. Regulation of epithelial-mesenchymal transition by tumor microenvironmental signals and its implication in cancer therapeutics. Semin. Cancer Biol. 88, 46–66 (2023).
Tan, L. L. Y. & Chua, M. L. K. Discovering biomarkers of radioresistance in a radiosensitive cancer: A clinical paradox in nasopharyngeal carcinoma. Ann. Transl. Med. 8, 1284–1284 (2020).
Fedele, M., Sgarra, R., Battista, S., Cerchia, L. & Manfioletti, G. The epithelial-mesenchymal transition at the crossroads between metabolism and tumor progression. Int. J. Mol. Sci. 23, 800 (2022).
Hsu, P. P. & Sabatini, D. M. Cancer cell metabolism: Warburg and beyond. Cell 134, 703–707 (2008).
Bai, Y., Sha, J., Okui, T., Moriyama, I., Ngo, H. X., Tatsumi, H. et al. The epithelial-mesenchymal transition influences the resistance of oral squamous cell carcinoma to monoclonal antibodies via its effect on energy homeostasis and the tumor microenvironment. Cancers 13 (2021).
Chen, Y.-P. et al. Nasopharyngeal carcinoma. Lancet 394, 64–80 (2019).
Lee, V. H. et al. Management of nasopharyngeal carcinoma: Is adjuvant therapy needed?. J. Oncol. Pract. 14, 594–602 (2018).
Chen, J., Liu, T., Sun, Q. & Jin, T. Comparison of the efficacy between concurrent chemoradiotherapy with or without adjuvant chemotherapy for stage II nasopharyngeal carcinoma. Medicine 99, e20443 (2020).
Miao, J. et al. Adjuvant capecitabine following concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal carcinoma. JAMA Oncol. 8, 1776 (2022).
Tsai, M.-H. et al. Improved overall survival is associated with adjuvant chemotherapy after definitive concurrent chemoradiotherapy for N3 nasopharyngeal cancer. Sci. Rep. 12, 13390 (2022).
Acknowledgements
We would like to thank the radiation oncology department of Queen Elizabeth Hospital, Hong Kong, and the radiation oncology department of Queen Mary Hospital, Hong Kong for providing valuable clinical and radiotherapy data.
Funding
This research was partly supported by research grants of Shenzhen Basic Research Program (JCYJ20210324130209023), Shenzhen-Hong Kong-Macau S&T Program (Category C) (SGDX20201103095002019), Mainland-Hong Kong Joint Funding Scheme (MHKJFS) (MHP/005/20), Project of Strategic Importance Fund (P0035421) and Projects of RISA (P0043001) from The Hong Kong Polytechnic University.
Author information
Authors and Affiliations
Contributions
J.S. as the first author is contributed to the conceptualization of methodology, statistical analysis, and manuscript writing. S.K.E.L., J.Z., X.T., F.K.L., C.W.Y., J.C.C., V.H.L., and Y.S. are contributed to the data collection, data curation, and manuscript writing. J.C. as the corresponding author contributed to the study initiation, organization, and manuscript writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
AI and AI-assisted technologies were not used in the writing process of the manuscript. This study was performed in accordance with the STROBE guidelines. The use of data was approved by the Research Ethics Committee (Kowloon Central/Kowloon East), reference number KC/KE-18-0085/ER-1, and the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB), reference number UW20-827.
Informed consent
Due to the retrospective nature of the study, the Institutional Review Board of the University of Hong Kong and the Research Ethics Committee (Kowloon Central/Kowloon East) waived the need of obtaining informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, J., Lam, S.k.E., Teng, X. et al. Predicting disease progression from the rate of bodyweight change in nasopharyngeal carcinoma patient during radiotherapy. Sci Rep 15, 7490 (2025). https://doi.org/10.1038/s41598-025-88810-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-88810-x