Abstract
Osteoarthritis (OA) is a chronic degenerative joint disease with an increasing global burden, particularly among the working-age population. This study aims to analyze the temporal trends in OA burden by age and sex globally from 1990 to 2021, focusing on incidence, prevalence, and disability-adjusted life years (DALYs) rates, and to predict future trends. Using data from the Global Burden of Disease (GBD) database, which includes 204 countries and regions, we stratified the findings by the sociodemographic index (SDI). Age-standardized rates were used to calculate the estimated annual percentage change (EAPC) with corresponding 95% confidence intervals (95% CI). Additionally, a Bayesian Age-Period-Cohort (BAPC) model was employed to project future OA trends up to 2040.The results revealed a consistent increase in the global OA burden over the study period. Between 1990 and 2021, the number of OA cases in the working-age population increased from 16,420,160 to 35,494,218, representing a growth rate of 116.16%. Over the same period, prevalence and DALYs rose by 123.11% and 125%, respectively. Global age-standardized incidence rate (ASIR), prevalence rate (ASPR), and DALYs rate (ASDR) exhibited continuous upward trends, with annual percentage changes of 0.387%, 0.431%, and 0.46%, respectively. Notably, East Asia demonstrated the highest EAPC, reflecting a rapid rise in OA burden, while high-income North America exhibited minimal changes, indicating a relatively stable trend. Countries such as Equatorial Guinea, Mongolia, and Armenia also experienced significant increases in EAPC, underscoring emerging regional challenges.Further socioeconomic analysis highlighted disparities in OA burden. A significant positive correlation was observed between ASIR, ASPR, ASDR, and SDI. While low-SDI countries exhibited lower OA burdens, metrics were substantially higher in high-SDI countries. From 1990 to 2021, the gap between countries with the highest and lowest SDIs widened, underscoring growing global health inequalities. Projections based on the BAPC model suggest that by 2040, the incidence and prevalence of OA will continue to rise, with the number of cases expected to reach 38,800,395, particularly driven by notable increases among women.These findings highlight the urgent need for developing targeted public health strategies to mitigate the effect of OA on the working-age population and promote global health equity.
Similar content being viewed by others
Osteoarthritis (OA) is a chronic degenerative joint disorder characterized by the progressive degeneration of articular cartilage, osteophyte formation at the joint margins, and pathological changes in subchondral bone, leading to clinical manifestations such as joint pain, stiffness, and restricted mobility1. Predominantly affecting the hip, knee, and hand joints, OA may also involve other articular structures2. The associated pain and functional limitations not only markedly reduce patients’ quality of life but also impose significant socioeconomic burdens on families and society3. Epidemiological data indicate that OA affects more than 300 million individuals worldwide, with disproportionately higher incidence and prevalence observed in middle-aged and elderly populations. With the aging of the global population and increasing obesity rates, the OA burden as a public health concern is increasing, warranting more comprehensive studies to address this worsening challenge4.
The Organisation for Economic Co-operation and Development (OECD) defines the working-age population (WAP) as individuals aged 15 to 645,6. With global demographic shifts, rising dependency ratios, and other market trends, the health issues of the working-age population (WAP) are becoming increasingly crucial for future societal well-being. In particular, the burden of certain diseases has profound implications for this population. Although OA primarily affects middle-aged and elderly individuals, recent studies have revealed a rising incidence of OA among younger working-age groups. This shift indicates that OA is no longer solely a concern for the elderly.For the working-age population, joint health issues not only impact individual labor productivity but also place an additional strain on healthcare resources7,8. As the backbone of socioeconomic development, the health of working-age individuals, especially their joint health, directly affects their work capacity, efficiency, and economic earnings. The prevalence of OA further influences societal economic vitality and mental well-being9,10. Therefore, preventing and alleviating OA in the working-age population is not only essential for individual long-term quality of life but is also closely linked to sustainable social development. However, to date, no study has systematically examined the burden of arthritis in the working-age population.
Although extensive research has been conducted on vulnerable populations, particularly the elderly, epidemiological studies specifically targeting working-age individuals with OA remain limited11. Currently, there is a lack of comprehensive, long-term global studies examining the prevalence patterns of OA in this demographic. To address this gap, this study systematically investigates the burden of OA among working-age individuals by analyzing Global Burden of Disease (GBD) data from 1990 to 2021. We evaluated incidence, prevalence, and disability-adjusted life years (DALYs), with a particular emphasis on the influence of age, sex distribution, and socioeconomic factors. The findings aim to provide valuable insights for clinicians, epidemiologists, and health policymakers, facilitating the optimization of healthcare resource allocation and the development of more effective public health strategies.
Methods
Overview
The GBD study, led by the Institute for Health Metrics and Evaluation at the University of Washington, has emerged as a critical tool for analyzing global epidemiological data since its inception in 1990.The GBD study offers comprehensive data on disease incidence, prevalence, and DALYs for various countries and regions, classified by age and sex; this helps nations understand the prevalence and burden of different diseases12. In the latest GBD 2021 study, researchers comprehensively analyzed the trends for 371 diseases and injuries worldwide, assessing 87 attributable risk factors across 204 countries and regions. These data provide essential evidence for countries to formulate public health policies and optimize the allocation of healthcare resources13.Detailed information regarding GBD 2021 and its methodology has been documented in relevant literature. All GBD 2021 data are publicly accessible online at the following links: https://vizhub.healthdata.org/gbd-compare/ and https://vizhub.healthdata.org/gbd-results/.
Data
We conducted a secondary analysis based on publicly available data from GBD 2021. The GBD 2021 study, carried out by the Institute for Health Metrics and Evaluation (IHME), integrates all available data to provide consistent information on the burden of diseases, injuries, and risk factors, as well as the latest global, regional, and national estimates14. All data have undergone rigorous standardization and quality control. Since this study uses publicly available data and does not involve the collection or processing of personally identifiable information, no additional ethical approval is required. The GBD study has been approved by the University of Washington’s Institutional Review Board and adheres to all relevant ethical guidelines and data protection regulations.
In the GBD 2021 study, OA includes cases affecting the hip, knee, hand, and other joints. In this study, we utilized data from GBD 2021, which has been described in detail in previous publications15,16. Specifically, GBD 2021 provides a comprehensive and systematic assessment of age- and sex-specific mortality rates, 288 causes of death, 371 diseases and injuries, and 88 risk factors across 204 countries and territories (including subnational estimates for 21 countries and territories) from 1990 to 2021.The osteoarthritis data obtained from GBD 2021 cover the prevalence, incidence, and years lived with disability (YLDs) across 204 countries and territories and 54 regions. In GBD 2021, osteoarthritis is defined as symptomatic OA in the hip, knee, hand, or other joints confirmed by radiographic examination using the Kellgren-Lawrence grading system—grade 2 (definite osteophytes and joint space narrowing) or grade 3–4 (multiple moderate osteophytes, definite joint space narrowing with deformity and sclerosis)17,18,19—and associated with pain for at least one month in the past 12 months. Disability weights, ranging from 0 (perfect health) to 1 (death), were used to represent the severity of health loss due to osteoarthritis. The disability weights in GBD 2021 were derived from data collected through open-access online surveys. YLDs for osteoarthritis were calculated by multiplying the prevalence of each sequela category by its corresponding disability weight.
Sociodemographic index (SDI)
The SDI is a composite measure developed by the GBD research team to evaluate the socioeconomic status of regions. This index integrates per capita income, education levels, and fertility rates into a single value ranging from 0 to 1, reflecting the socioeconomic development of regions or countries and its impact on health outcomes20,21. Typically, a higher SDI value indicates better socioeconomic conditions, which are often associated with improved health outcomes, including lower disease burdens and longer life expectancy. Based on SDI scores, regions are divided into five quantiles: low, low-middle, middle, middle-high, and high. This classification not only facilitates comparisons of health disparities across different regions globally but also reveals the profound effect of socioeconomic background on health status. Through this categorization, researchers can comprehensively analyze health challenges in regions with poor socioeconomic conditions and develop targeted public health strategies to improve global health inequalities.
Data analysis
To conduct data analysis, the structure of the dataset was first determined, and the number and proportion of the prevalence, incidence, and DALYs of OA in working-age individuals were calculated at the global, regional, and national levels. Age-standardized rates (ASRs) were calculated according to global standards22. Specifically, each ASR (per 100,000 population) was calculated as follows:\(\:\text{A}\text{S}\text{R}=\frac{{\sum\:}_{i=1}^{A}\:{a}_{i}{w}_{i}}{{\sum\:}_{i=1}^{A}\:{w}_{i}}\times\:\text{100,000}\).where αi refers to the age-specific rate in the ith age group, wi represents the population number (or weight) of the corresponding ith age subgroup in the population selected as the reference standard, and A signifies the number of age groups.The maps in this study were all generated using R software version 4.4.3 (https://www.r-project.org/).
Subsequently, detailed data on cases and deaths globally, nationally, and regionally were collected for the year, employing rigorous statistical methods to track OA trends in working-age individuals, represented by the estimated annual percentage change (EAPC)23. The EAPC was calculated as follows: 100 × [exp(β) − 1], using a linear regression model for computing the 95% confidence interval (CI). An EAPC value with a 95% CI > 0 indicated an increasing trend, whereas a value with a 95% CI < 0 indicated a reducing trend. Other scenarios suggested that the ASR remains relatively stable over time.
To investigate the influencing factors for EAPC, Pearson’s correlation analyses were performed using R software (available for download at: https://www.r-project.org/). The association between EAPCs and ASR was assessed for 1990, as well as that between EAPCs and the Human Development Index (HDI) for 2021, producing stratified statistical maps24,25. Furthermore, using Pearson’s correlation coefficients, the relationship between the SDI and OA indicators was explored in working-age individuals to evaluate the strength and direction of their linear relationships across different geographic regions.
Decomposition analysis can help determine the additive contributions of factor differences in two populations to the disparities in their overall values26. By disaggregating the incidence, prevalence, and DALYs of OA within the working-age population based on age structure, population growth, and epidemiological changes, the contribution of each component to the cumulative impact can be quantified.
Frontier analysis was conducted to establish a benchmark for the OA burden in working-age individuals and to compare disparities among countries and regions in controlling this burden27. The “effective difference,” reflecting the gap between the current OA burden of each country and its potential minimum burden, adjusted according to SDI, was calculated.
Finally, the Bayesian Age-Period-Cohort (BAPC) model was adopted for predicting OA trends in working-age individuals up to 2030. This model combines past data and probability distributions, accounting for age, time, and cohort effects, allowing the estimation of future global OA burden patterns28.
Results
Global and regional distributions of osteoarthritis in Working-Age individuals in 2021
In 2021, the age-standardized incidence rate (ASIR), age-standardized prevalence rate (ASPR) and age-standardized disability-adjusted life years (ASDR) of OA were 653.375 cases (95% UI: 513.361–808.53), 5,989.794 cases (95% UI: 5,081.139–6,933.053), and 208.001 cases (95% UI: 99.073–416.366) per 100,000 population among working-age individuals globally, respectively. To further determine differences between regions, we categorized the data based on the SDI. We observed that regions with high SDI exhibited the highest ASIR, ASPR, and ASDR [751.852 cases/100,000 (95% UI: 591.624–930.182), 6,717.88 cases/100,000 (95% UI: 5731.583–7766.293), and 236.74 cases/100,000 (95% UI: 113.023–475.948), respectively]. In contrast, countries with low SDI exhibited the lowest ASIR, ASPR, and ASDR [530.864 cases/100,000 (95% UI: 416.784–658.089), 4,765.156 cases/100,000 (95% UI: 4047.096–5526.431), and 162.175 cases/100,000 (95% UI: 77.67–324.3), respectively]. Collectively, these findings suggest that countries and regions with higher economic development levels frequently face a higher disease burden. Specific data supporting these observations are presented in Supplementary Table 1.
From a regional perspective, the OA burden was the most pronounced in high-income North America, high-income Asia Pacific, and East Asia. Supplementary Table 1 comprehensively summarize the data. At the national level, the top 10 countries with the highest ASIR, ASPR, and ASDR in 2021 were primarily developed nations, including South Korea, the United States, and Singapore. This trend indicates that OA poses significant health risks and socioeconomic burdens for working-age individuals in these countries. Supplementary Fig. 1 and Supplementary Table 2 detail the specific findings.
Among the global working-age population, the ASIR in 2021 was 537.143 cases/100,000 (95% UI: 536.866–537.419) for males, whereas it was 768.641 cases/100,000 (95% UI: 768.312–768.970) for females. Regarding prevalence, the ASPR was 4,937.233 cases/100,000 (95% UI: 4,936.397–4,938.069) for males compared with 7,020.759 cases/100,000 (95% UI: 7,019.773–7,021.745) for females. In terms of mortality, the ASDR was 171.027 cases/100,000 (95% UI: 170.872–171.183) for males compared with 244.172 cases/100,000 (95% UI: 243.988–244.356) for females. Overall, the incidence, prevalence, and mortality rates were higher in females than in males, underscoring the significant influence of sex differences on the OA burden.Supplementary Tables 3 and Supplementary Figs. 2 − 5 provide detailed results.
In addition to sex differences, age is also an essential factor affecting the disease burden. Age distribution analysis revealed that among individuals under 50, high-income North America exhibited the highest ASIR, ASPR, and ASDR. However, with an increase in age, the ASIR, ASPR, and ASDR for those over 50 reached their peak in high-income Asia Pacific. Figure 1, Supplementary Fig. 6, and Supplementary Table 4 provide detailed results. These findings indicate that the OA burden is not only associated with regional economic development but is also significantly influenced by age and sex.
Temporal trends of osteoarthritis in Working-Age individuals from 1990 to 2021
In 2021, the number of OA cases reached 35,494,218 (95% UI: 27,880,492–43,932,657) among working-age individuals worldwide; this indicates a significant increase of 116.16% compared with 16,420,160 cases in 1990 (95% UI: 12,947,929–20,366,629). In terms of prevalence, the number of OA cases among working-age increased from 147,223,784 in 1990 (95% UI: 125,053,457–170,708,574) to 329,092,356 in 2021 (95% UI: 279,266,465–380,772,052), indicating a growth rate of 123.11%. Furthermore, the number of OA-induced DALYs was 11,430,526 (95% UI: 22,870,436–5,445,291) among the global working-age population in 2021, an increase of 125% from 5,078,433 in 1990 (95% UI: 10,198,128–2,427,263). Between 1990 and 2021, the ASIR, ASPR, and ASDR of the global working-age population were significantly increased, with annual percentage change (EAPC) values of 0.387 (95% CI: 0.356–0.418), 0.431 (95% CI: 0.388–0.474), and 0.46 (95% CI: 0.413–0.506), respectively. Supplementary Table 1 provide specific results.
Between 1990 and 2021, the number of OA cases among global working-age males increased from 8,093,701 (95% UI: 8,085,456–8,101,946) to 13,815,145 (95% UI: 13,804,966–13,825,324). For females, it increased from 11,283,587 (95% UI: 11,273,865–11,293,309) to 19,502,817 (95% UI: 19,490,789–19,514,845). Furthermore, the prevalence increased from 74,219,869 (95% UI: 74,194,755–74,244,984) to 126,984,119 (95% UI: 126,953,298–127,014,941) among males and from 102,303,951 (95% UI: 102,274,593–102,333,310) to 178,138,587 (95% UI: 178,102,384–178,174,790) among females. In addition, DALYs increased from 2,556,383 (95% UI: 2,551,731–2,561,035) to 4,398,769 (95% UI: 4,393,038–4,404,501) among males and from 3,533,052 (95% UI: 3,527,604–3,538,500) to 6,195,403 (95% UI: 6,188,656–6,202,150) among females. Since 1990, there has been a global increase in ASIR, ASPR, and ASDR for OA among working-age males and females. The EAPC for males was 0.467 (95% CI: 0.381–0.552), 0.486 (95% CI: 0.419– 0.553), and 0.478 (95% CI: 0.411–0.545), respectively; in contrast, it was 0.355 (95% CI: 0.294–0.416), 0.343 (95% CI: 0.302–0.383), and 0.345 (95% CI: 0.305–0.384), respectively, for females. Supplementary Tables 3 and Supplementary Figs. 2–5 provide detailed results.
In terms of incidence, the overall incidence of OA remained stable across all age groups among the working-age population globally. However, a slight upward trend was noted in the 40–44 and 50–54 age groups. Prevalence also exhibited a stable trend; however, a significant increase was noted in the 50–64 age group. DALYs slightly increased across all age groups and SDI levels, particularly in the 50–64 age group, in which the increase was more pronounced. Figure 1, Supplementary Fig. 6, and Supplementary Table 4 collectively present a comprehensive summary of the findings.
SDI analysis revealed that regions with medium SDI exhibited the highest EAPC for incidence, prevalence, and DALYs, with values of 0.542 (95% CI: 0.493–0.59), 0.559 (95% CI: 0.503–0.615), and 0.599 (95% CI: 0.541–0.657), respectively. In contrast, regions with high SDI exhibited the lowest EAPC, recorded at 0.255 (95% CI: 0.207–0.303), 0.313 (95% CI: 0.263–0.363), and 0.334 (95% CI: 0.276–0.392), respectively. Geographically, East Asia exhibited the highest EAPC for incidence, prevalence, and DALYs, with values of 0.673 (95% CI: 0.574–0.773), 0.675 (95% CI: 0.569–0.781), and 0.721 (95% CI: 0.613–0.83), respectively. In contrast, high-income North America (EAPC = 0.102, 95% CI: −0.052 to 0.255) was the region with the lowest incidence, and Central Sub-Saharan Africa exhibited the lowest prevalence and DALYs, with EAPC values of 0.107 (95% CI: 0.051–0.164) and 0.14 (95% CI: 0.08–0.201), respectively. Supplementary Fig. 7 provides detailed results.
Significant differences were noted in EAPC among working-age individuals with OA across different countries. Equatorial Guinea exhibited the highest global incidence (1.176, 95% CI: 1.104–1.249), prevalence (1.280, 95% CI: 1.202–1.358), and DALYs (1.349, 95% CI: 1.305–1.482). In contrast, the Democratic Republic of the Congo recorded the lowest incidence (− 0.033, 95% CI: −0.107 to 0.040) and DALYs (− 0.019, 95% CI: −0.110 to 0.071), whereas Singapore recorded the lowest prevalence (0.074, 95% CI: 0.061–0.086). Figure 2 provides specific results.
Decomposition analysis
The contribution patterns of population growth, aging, and epidemiological changes to the ASIR, ASPR, and ASDR of OA in working-age individuals are similar across the globe, five SDI regions, and 21 GBD regions, as well as among different gender populations. Overall, with a few exceptions, these three factors have led to an increase in ASIR, ASPR, and ASDR for osteoarthritis, with population growth being the primary driver of the rising burden of this disease. Specifically, aging has been associated with a decrease in ASIR, ASPR, and ASDR for OA in working-age individuals in the Low SDI, Central Sub-Saharan Africa, Eastern Sub-Saharan Africa, and Western Sub-Saharan Africa regions.
Moreover, population growth, aging, and epidemiological changes have all contributed to the increasing burden of disease globally and in other regions, see Fig. 3 for detail. Notably, population growth has had the most significant impact on the increases in ASIR (190.47%), ASPR (190.28%), and ASDR (190.66%) in North Africa and the Middle East, while it has had the least impact on the increases in ASIR (2.752%), ASPR (2.781%), and ASDR (2.797%) in Central Europe. Epidemiological changes have contributed most significantly to the increases in ASIR (33.047%), ASPR (35.136%), and ASDR (36.062%) in North Africa and the Middle East, while having the least impact on the increases in ASIR (7.247%), ASPR (5.08%), and ASDR (5.789%) in Eastern Europe.
Additionally, aging has contributed most significantly to the increases in ASIR (26.718%), ASPR (39.768%), and ASDR (40.165%) in Central Latin America, while having the least impact on the increases in ASIR (3.902%), ASPR (3.929%), and ASDR (3.839%) in Eastern Europe and Central Asia, respectively. Detailed results of the specific contributions of these three factors to the burden of disease can be in Supplementary Table 5 .
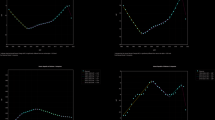
Health inequality analysis
The Slope Index of Inequality (SII) indicated that the gap in incidence, prevalence, and DALYs of OA increased from 339.169 (95% CI: 299.194–379.144), 3314.082 (95% CI: 2909.786–3718.377), and 118.872 (95% CI: 104.644–133.1) in 1990 to 584.079 (95% CI: 545.728–622.43), 6253.758 (95% CI: 5800.124–6707.392), and 223.258 (95% CI: 207.091–239.425) in 2021 in working-age individuals between countries with the highest and lowest SDI. This indicates that countries with a higher SDI bear a disproportionate health burden, a trend particularly pronounced in populous countries such as China and India. Between 1990 and 2021, the global incidence, prevalence, and DALYs increased with the growth of SDI. By 2021, these indicators were higher than those in 1990, reflecting a deterioration in overall health status. In addition, the Concentration Index (CI) of relative gradient inequality increased from 0.146 (95% CI: 0.132–0.16), 0.159 (95% CI: 0.144–0.175), and 0.167 (95% CI: 0.151–0.183) in 1990 to 0.169 (95% CI 0.157–0.18), 0.19 (95% CI 0.177–0.203), and 0.196 (95% CI: 0.183–0.209) in 2021, respectively. This change further reveals an increase in OA-related health inequalities in working-age individuals. Figure 4 and Supplementary Table 6 provide specific results.
.Health inequality regression and concentration curves for Osteoarthritis in Working-Age Individuals by incidence, prevalence, and DALYs. (A) Health inequality regression curves for incidence; (B) Concentration curves for incidence; (C) Health inequality regression curves for prevalence; (D) Concentration curves for prevalence; (E) Health inequality regression curves for DALYs; (F) Concentration curves for DALYs.
Trends of osteoarthritis in Working-Age individuals from 1990 to 2040
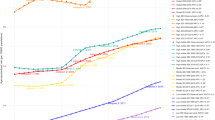
Based on BAPC predictions, the incidence, prevalence, and DALYs of OA will significantly increase over the coming decades in working-age individuals, with the growth rate among females generally exceeding that of males. In particular, the overall incidence is projected to increase from approximately 19,377,288 cases in 1990 to 38,800,395 cases by 2040. Among these, the number of male cases is expected to increase from 8,093,701 to 16,585,970, whereas female cases are projected to increase from 11,283,587 to 22,214,425, indicating a slightly higher growth rate for females. Moreover, the ASIR may increase from approximately 593 cases per 100,000 in 1990 to approximately 667 cases per 100,000 in 2040. The ASIR for males may increase from 489 cases per 100,000 to approximately 550 cases per 100,000; in contrast, the increase for females is more pronounced, increasing from 697 cases per 100,000 in 1990 to nearly 756 cases per 100,000 in 2040.
In terms of prevalence, the total number of cases is projected to increase from 176,523,820 in 1990 to 362,785,075 in 2040. Besides, the number of male cases may increase from 74,219,869 to 154,236,478, whereas female cases may increase from 102,303,951 to 208,548,597, with the growth rate of females continuously increasing slightly faster than that of males. In addition, the predicted ASPR may increase from approximately 5,407 cases per 100,000 in 1990 to approximately 6,249 cases per 100,000 in 2040. The ASPR for males may increase from 4,492 cases per 100,000 to approximately 5,123 cases per 100,000. In contrast, the ASPR for females may increase from 6,328 cases per 100,000 in 1990 to approximately 7,105 cases per 100,000 in 2040.
Regarding DALYs, the total may increase from 6,089,435 in 1990 to 12,454,232 in 2040. DALYs may increase from 2,556,383 to 5,308,574 for males and from 3,533,052 to 7,145,658 for females. Meanwhile, the predicted ASDR indicated that the overall ASDR will increase from approximately 186 cases per 100,000 in 1990 to approximately 214 cases per 100,000 in 2040. The ASDR may increase from 154 cases per 100,000 to approximately 176 cases per 100,000 for males. In contrast, the increase is even more substantial for females, increasing from 218 cases per 100,000 in 1990 to 243 cases per 100,000 in 2040. Overall, from 1990 to 2040, the incidence, prevalence, and DALYs of OA, as well as the age-standardized rates, will increase significantly, particularly among females. This trend suggests that the global health burden will continuously increase, particularly for the female population, with notable increases in ASIR, ASPR, and ASDR. Figure 5 and Supplementary Table 7 provide detailed results, indicating the trends in these data.
Correlation analysis between SDI and ASR of health burden indicators
In this study, we analyzed the relationship between the SDI and ASIR, ASPR, and ASDR to reveal the effect of economic and social development levels on global health burden. Analysis at the overall, regional, and national levels revealed a significant positive correlation between ASIR and SDI (R = 0.663, P < 0.001). Furthermore, a significant positive correlation was observed between ASPR and SDI (R = 0.681, P < 0.001) and similarly between ASDR and SDI (R = 0.702, P < 0.001). Figure 6 illustrates the results.
When examining OA indicators in the working-age population across 21 regions, we observed subtle correlations with the SDI. In particular, the correlation between ASIR and SDI was neutral (R = 0.561, P < 0.001), whereas ASPR exhibited a stronger positive correlation (R = 0.574, P < 0.001), with both reaching statistical significance. In contrast, the association between ASDR and SDI was weaker (R = 0.598, P < 0.001), indicating that ASDR significantly increases with higher SDI. Supplementary Fig. 8 illustrates detailed results.
In 2021, national-level data indicated a gradual increase in the ASIR of OA in working-age individuals with rising SDI, exhibiting a significant positive association (R = 0.65, P < 0.001). However, when SDI exceeded 0.8, a downward trend in ASIR was observed. Meanwhile, ASPR also increased with increasing SDI (R = 0.71, P < 0.001); however, when SDI surpassed 0.6, the relationship between ASPR and SDI exhibited a declining trend. In addition, ASDR exhibited a strong positive relationship with SDI (R = 0.69, P < 0.001); however, when SDI exceeded 0.75, ASDR rapidly decreased. Supplementary Fig. 9 illustrates the results.
Pearson correlation analysis between SDI quantiles and age-standardized rates (ASRs) for Osteoarthritis in Working-Age Individuals in 1990 and 2021. (A) The relationship between the SIR and the SDI, (B) The relationship between the ASPR and the SDI, (C) The relationship between the ASDR and the SDI.
Frontier analysis
The frontier refers to the leading countries or regions in the field of OA in working-age individuals, which demonstrate the lowest disease burden based on their SDI. Effective disparity denotes the gap between a country’s or region’s actual burden and the theoretical burden predicted based on its SDI. A significant effective disparity suggests potential unrealized opportunities for health improvement based on the position within the development spectrum. We utilized the incidence and SDI of OA in working-age individuals from 2021 to estimate the effective disparity for each country and region. South Korea, Brunei, Singapore, the United States, and Japan were identified as the five countries or regions with the largest effective disparity in incidence (effective disparity range: 396.001–448.43). In contrast, Burundi, Madagascar, Cambodia, Niger, and Somalia were identified as the five countries or regions with the smallest effective disparity in incidence (range: 6.401–18.274).
For the prevalence of OA in working-age individuals in 2021 and their SDI, South Korea, the United States, Brunei, Singapore, and Taiwan were identified as the five countries or regions with the largest effective disparity (effective disparity range: 3500.365–3873.693). In contrast, Afghanistan, Burundi, Madagascar, Niger, and Somalia were identified as the five countries or regions with the smallest effective disparity in prevalence (range: 184.894–574.911). When analyzing the DALYs for OA in working-age individuals in 2021 and their SDI, South Korea, Singapore, Brunei, the United States, and Taiwan were identified as the five countries or regions with the largest effective disparity in DALYs (effective disparity range: 128.475–145.212). In contrast, Burundi, Madagascar, Afghanistan, Niger, and Somalia were identified as the five countries or regions with the smallest effective disparity in DALYs (range: 6.401–18.274). Detailed results supporting these findings are presented in Fig. 7 and Supplementary Table 8.
Discussion
In this study, we analyzed the changes in the incidence, prevalence, and DALYs of OA in the global working-age population from 1990 to 2021. During the study period, we noted a significant increase in OA cases, rising from 16,420,160 to 35,494,218, representing an increase of 116.16%. During the same period, the prevalence and DALYs increased by 123.11% and 125%, respectively. These data reflect a sharp escalation in the OA health burden on the working-age population over the past few decades, as evidenced by the rising case numbers and declining quality of life. First, the upward trends in ASIR, ASPR, and ASDR are consistent with previous research findings29,30. Multiple factors contribute to the increasing OA burden. The accelerated aging of the global population, particularly an increase in middle-aged and older groups, has notably increased the incidence and prevalence of OA among the working-age population, particularly in individuals aged 50–64, where the OA burden has become particularly pronounced31. In addition, the global obesity epidemic is a vital factor for the rising prevalence of OA because obesity not only increases joint load but also promotes OA progression via chronic low-grade inflammation32,33. Furthermore, changes in modern work environments, including prolonged sitting, repetitive joint strain, and poor posture, have resulted in sustained joint stress, increasing the risk of OA among the working-age population34.
Sex differences in OA incidence are also significant; this is crucial for understanding the epidemiological characteristics of OA. Studies have revealed that female workers have a higher incidence and prevalence of OA when compared with their male counterparts; this is consistent with previous research findings35,36. This may be associated with fluctuations in estrogen levels37,38, decreased bone density39, and higher obesity rates40. Socioeconomic factors and lifestyle differences may also contribute to women facing more joint stress in their occupations41. Subsequently, the rising burden of OA not only reflects demographic shifts and lifestyle changes but also underscores global inadequacies in preventing and managing OA. To address this trend, strengthening public health interventions and policy support is urgently warranted to promote weight management, healthy lifestyles, and improved occupational safety measures.
Regional analysis revealed that East Asia has the highest EAPC in OA incidence, prevalence, and DALYs globally. This trend may be owing to several factors, including a rapid increase in the elderly population42, accelerated urbanization43, and improvements in healthcare systems44. In contrast, high-income regions in North America exhibited the lowest EAPC values for incidence. Despite the persistent OA burden, the growth rate is slower, primarily owing to well-established public health systems and early preventive measures45. Moreover, the EAPC values were the lowest for prevalence and DALYs in sub-Saharan Africa globally, possibly reflecting the absence of healthcare resources and inadequate disease burden statistics46.
At the national level, countries such as Equatorial Guinea, Mongolia, Armenia, Ethiopia, and Thailand exhibited the highest EAPC values; this is closely associated with the high-intensity physical activities undertaken by workers in these nations47. Meanwhile, Iceland, Denmark, the Netherlands, and Singapore exhibited relatively low EAPC values, reflecting effective measures in preventing and controlling OA in these areas48. Notably, the low EAPC values in the Democratic Republic of the Congo and Zimbabwe do not necessarily indicate a lighter OA burden. The lower values may be associated with inadequate health monitoring systems, limited medical resources, and an underestimation of the actual OA burden49.
The SII indicates that from 1990 to 2021, the gap in the incidence, prevalence, and DALYs of OA among the working-age population between the highest and lowest SDI countries has significantly widened. This trend suggests that the disparity in OA-related health burden between high- and low-SDI countries is continuously expanding. Meanwhile, these health indicators have generally increased with SDI growth worldwide, reflecting an escalating OA burden among the working-age population, particularly in highly populated countries.In high-SDI countries, several factors have contributed to the continuous rise in OA burden. Population aging50, lifestyle changes51, and improved medical detection rates52are key drivers. Additionally, the increasing prevalence of obesity and declining levels of physical activity have further exacerbated the spread of OA53.In contrast, low-SDI countries face greater challenges in addressing OA burden. Limited medical resources and inadequate capacity for early screening and intervention have led to more severe OA cases and a higher DALY burden54. Moreover, a higher proportion of the low-income population engages in physically demanding labor, which further increases the risk of OA47.Global economic development has also played a significant role in shaping OA-related health burdens. Shifts in dietary patterns, accelerated industrialization and urbanization, and the unequal distribution of medical resources and technologies have exacerbated health inequalities. This issue is particularly pronounced in densely populated countries such as China and India43.Therefore, future strategies should focus on comprehensive measures to address these challenges. Enhancing early OA screening and intervention, increasing public health awareness, promoting healthy lifestyles, and advancing the equitable distribution of medical resources are critical steps. These efforts will help reduce health inequalities between and within countries while effectively mitigating OA’s impact on the working-age population.
Based on BAPC predictions, the incidence, prevalence, and DALYs of OA may significantly increase in the global working-age population in the coming decades, with growth rates for females generally exceeding those for males. This trend is primarily attributed to population aging, increasing obesity rates, and increased occupational risks, particularly among working-age individuals, where the prevalence of OA continues to increase. Notably, women experience a more significant OA growth rate owing to differences in joint anatomy, alignment, muscle strength, hormonal influences, obesity, and genetics55. This phenomenon worsens the global health burden of OA, particularly highlighted by imbalanced growth in female populations, presenting new challenges for global public health. This underscores the need for global health governance to pay more attention to the specific needs of women in managing chronic diseases such as OA to ensure more equitable health outcomes and mitigate future economic and social pressures. Although projections indicate the rising incidence, prevalence, and DALYs of OA, uncertainties remain regarding future trends. These uncertainties may be owing to advances in medical technology, changes in public health policies, fluctuations in socioeconomic conditions, and improvements in early diagnosis and treatment capabilities. Therefore, when formulating public health strategies, considering these potential variations is essential to effectively address future health challenges and ensure the flexibility and efficacy of these strategies.
In this study, we investigated the relationship between the SDI and OA burden in the working-age population. We noted that the incidence, prevalence, and DALYs of OA are obviously higher in high SDI regions than in low SDI regions. This disparity reflects the complex relationship between economic development and disease burden. Despite some success in public health policies, early screening, and medical resource allocation in high SDI regions, the challenges posed by population aging and unhealthy lifestyles (such as sedentary behavior and obesity) continuously pose a heavy OA burden. In contrast, low SDI regions face the dual challenges of limited medical resources and lagging economic development. Meanwhile, the CI has increased to varying degrees from 1990 to 2021, further revealing the worsening of OA-related health inequalities OA among the working-age population. Although health burdens are heavier in high SDI countries, health inequalities are worsening in low SDI countries; this reflects that these regions possess insufficient capacity to prevent and manage OA. Notably, in China and India, the two most populous countries globally, changes in OA health burden have profound implications for global health inequities. Because these two nations are experiencing rapid economic growth, environmental pollution, lifestyle changes, and increased population aging, the incidence and related health burden of OA have significantly increased among the working-age population56,57. This not only highlights the complex relationship between economic development and health burden but also emphasizes the need to consider the socioeconomic backgrounds, sex differences, and aging effects of various regions when formulating targeted health policies and interventions. Subsequently, to address the escalating health inequalities related to OA among working-age individuals, countries must adopt more detailed and comprehensive health intervention measures. Public health policies should focus on promoting healthy lifestyles, early diagnosis, and long-term management to alleviate the OA burden on the working-age population. Overall, these study findings provide important evidence for policy-making and lay the groundwork for future health management and intervention strategies across countries with different levels of economic development.
Frontier analysis based on the SDI and ASRs of OA in the working-age population provided critical insights into the global OA trends between 1990 and 2021. With an increase in the SDI, the OA burden also exhibited an overall upward trend among the working-age population (measured by incidence, prevalence, and DALYs). However, data from 2021 reveal significant disparities among countries. For example, while countries such as South Korea, Singapore, and Brunei exhibit high SDIs, their OA prevalence remains relatively high, placing them far from the optimal frontier. In contrast, low SDI countries such as Burundi and Madagascar exhibit relatively low OA burdens. This highlights the complexity of OA outcomes in the working-age population, indicating that although SDI is important, factors such as population aging, lifestyle, working conditions, and healthcare service accessibility also play essential roles in shaping OA trends among the workforce. To address this challenge, countries should develop targeted public health policies that prioritize improvements in working conditions, healthy lifestyle promotion, and chronic disease management to lower the OA burden in the working-age population and enhance overall health levels.
Despite these findings, our study still has some limitations. First, the potential for misdiagnosis, overlooked cases, and loss of documentation—stemming from inadequate medical infrastructure in underdeveloped countries—may result in the underestimation of OA in working-age individuals in the GBD study. Second, the raw data used in the GBD study originates from diverse countries, resulting in inconsistencies in data quality. For example, differences in OA measurement can result in disease misclassifications, complicating comparisons across populations. Although GBD collaborators perform data cleaning, correction, and advanced statistical modeling techniques to address these challenges, the reliance on modeled data presents an additional limitation, particularly at the national level, where the number of countries providing actual data is often restricted. Third, recognizing the inherent lag in GBD estimates is essential; they are based on past trends and covariates. To enhance the robustness of disease burden estimates and improve the accuracy of related studies, international collaboration, refined disease diagnostic criteria—especially in underdeveloped nations—and more efficient health data collection from various sources at the national level are warranted. The GBD database primarily compiles information from national and regional reports and publications rather than directly from national health authorities. This approach may raise concerns regarding data completeness, timeliness, and quality, particularly in low-income regions. Despite these limitations, the GBD study possesses notable strengths. First, comprehensive analyses—such as descriptive statistics, trend assessments, decomposition studies, health inequality evaluations, and predictive modeling—have significantly advanced our understanding of OA epidemiology. Therefore, our study establishes a robust foundation for the development of public health policies and the allocation of medical resources on a global scale.
OA represents a major public health challenge, particularly impacting the labor force, and poses significant socioeconomic challenges due to its adverse effects on productivity, employment, and overall economic stability.The OA burden has been increasing, with notable increases in incidence and prevalence among working-age individuals, particularly older adults and women. This trend is largely driven by demographic changes, including population growth and aging, which may further escalate OA cases in the future. Moreover, disparities associated with SDI have widened, with higher SDI countries bearing a higher OA burden among the labor force. Moreover, our findings emphasize the urgent need for targeted strategies addressing the unique challenges posed by OA in this demographic. Effectively managing OA within the labor force requires prioritizing interventions that enhance access to early diagnosis, promote a healthy lifestyle, and increase public awareness about the condition. By implementing individualized healthcare approaches and focusing on community engagement, policymakers can improve resource allocation and ultimately enhance the quality of life of those with OA, while decreasing its economic effect on the workforce. Lastly, a comprehensive and multifaceted strategy is essential to address the complexities of managing OA and to ensure improved outcomes for individuals affected by this debilitating condition.
Data availability
Data used for the analyses are publicly available from the Institute of Health Metrics and Evaluation (http://www.healthdata.org/; http://ghdx.healthdata.org/gbd-results-tool). For the datasets used and/or analyzed, and the codes used during the current study, please contact the corresponding author at [email protected] (Huanan Li) on reasonable request.
References
Abramoff, B., Caldera, F. E. & Osteoarthritis Pathology, diagnosis, and treatment options. Med. Clin. North. Am. 104 (2), 293–311. https://doi.org/10.1016/j.mcna.2019.10.007 (2020).
Hunter, D. J., March, L. & Chew, M. Osteoarthritis in 2020 and beyond: a lancet commission. Lancet 396 (10264), 1711–1712. https://doi.org/10.1016/S0140-6736(20)32230-3 (2020).
Zhao, T. et al. Cross-sectional and Temporal differences in health-related quality of life of people with and without osteoarthritis: a 10-year prospective study. Rheumatol. (Oxford). 60 (7), 3352–3359. https://doi.org/10.1093/rheumatology/keaa787 (2021).
Safiri, S. et al. Global, regional and National burden of osteoarthritis 1990–2017: a systematic analysis of the global burden of disease study 2017. Ann. Rheum. Dis. 79 (6), 819–828. https://doi.org/10.1136/annrheumdis-2019-216515 (2020).
Song, Y. et al. Trends and cross-country inequality in the incidence of GI cancers among the working-age population from 1990 to 2021: a global burden of disease 2021 analysis. Gut Published Online Dec. 31https://doi.org/10.1136/gutjnl-2024-333932 (2024).
Chen, J. et al. Global, regional, and National epidemiology of visual impairment in Working-Age individuals, 1990–2019. JAMA Ophthalmol. 142 (1), 25–32. https://doi.org/10.1001/jamaophthalmol.2023.5617 (2024).
Zhao, X. et al. Clinical, humanistic, and economic burden of osteoarthritis among noninstitutionalized adults in the united States. Osteoarthr. Cartil. 27 (11), 1618–1626. https://doi.org/10.1016/j.joca.2019.07.002 (2019).
Kotlarz, H., Gunnarsson, C. L., Fang, H. & Rizzo, J. A. Osteoarthritis and absenteeism costs: evidence from US National survey data. J. Occup. Environ. Med. 52 (3), 263–268. https://doi.org/10.1097/JOM.0b013e3181cf00aa (2010).
Glyn-Jones, S. et al. Osteoarthr. Lancet ;386(9991):376–387. doi:https://doi.org/10.1016/S0140-6736(14)60802-3 (2015).
Berkovic, D., Ayton, D., Briggs, A. M. & Ackerman, I. N. The financial impact is depressing and anxiety inducing: A qualitative exploration of the personal financial toll of arthritis. Arthritis Care Res. (Hoboken). 73 (5), 671–679. https://doi.org/10.1002/acr.24172 (2021).
Hawker, G. A. & King, L. K. The burden of osteoarthritis in older adults. Clin. Geriatr. Med. 38 (2), 181–192. https://doi.org/10.1016/j.cger.2021.11.005 (2022).
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396 (10258), 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet 403 (10440), 2133–2161. https://doi.org/10.1016/S0140-6736(24)00757-8 (2024).
Murray, C. J. & Lopez, A. D. Measuring the global burden of disease. N Engl. J. Med. 369 (5), 448–457. https://doi.org/10.1056/NEJMra1201534 (2013).
Peery, A. F. et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the united States: update 2024. Gastroenterol. Published Online Febr. 4 https://doi.org/10.1053/j.gastro.2024.12.029 (2025).
He, C., Lu, S., Yu, H., Sun, Y. & Zhang, X. Global, regional, and National disease burden attributable to high systolic blood pressure in youth and young adults: 2021 global burden of disease study analysis. BMC Med. 23 (1), 74. https://doi.org/10.1186/s12916-025-03918-1 (2025). Published 2025 Feb 6.
Ho-Pham, L. T. et al. Prevalence of radiographic osteoarthritis of the knee and its relationship to self-reported pain. PLoS One. ;9(4):e94563. Published 2014 Apr 10. (2014). https://doi.org/10.1371/journal.pone.0094563
KELLGREN, J. H. & LAWRENCE, J. S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 16 (4), 494–502. https://doi.org/10.1136/ard.16.4.494 (1957).
Kohn, M. D., Sassoon, A. A. & Fernando, N. D. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin. Orthop. Relat. Res. 474 (8), 1886–1893. https://doi.org/10.1007/s11999-016-4732-4 (2016). Epub 2016 Feb 12. PMID: 26872913; PMCID: PMC4925407.
Zou, J. et al. Distributions and trends of the global burden of COPD attributable to risk factors by SDI, age, and sex from 1990 to 2019: a systematic analysis of GBD 2019 data. Respir Res. 23 (1), 90. https://doi.org/10.1186/s12931-022-02011-y (2022). Published 2022 Apr 11.
GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021 [published correction appears in Lancet. ;402(10408):1132. doi: 10.1016/S0140-6736(23)02044-5]. Lancet. 2023;402(10397):203–234. (2023). https://doi.org/10.1016/S0140-6736(23)01301-6
Hankey, B. F. et al. Partitioning linear trends in age-adjusted rates [published correction appears in Cancer Causes Control. ;11(3):288]. Cancer Causes Control. 2000;11(1):31–35. (2000). https://doi.org/10.1023/a:1008953201688
Deng, Y. et al. Epidemiological trends of tracheal, bronchus, and lung cancer at the global, regional, and National levels: a population-based study. J. Hematol. Oncol. 13 (1), 98. https://doi.org/10.1186/s13045-020-00915-0 (2020). PMID: 32690044; PMCID: PMC7370495.
Lv, B. et al. Epidemiological trends of subarachnoid hemorrhage at global, regional, and National level: a trend analysis study from 1990 to 2021. Mil Med. Res. 11 (1), 46. https://doi.org/10.1186/s40779-024-00551-6 (2024). PMID: 38992778; PMCID: PMC11241879.
Wang, F., Ma, B., Ma, Q. & Liu, X. Global, regional, and National burden of inguinal, femoral, and abdominal hernias: a systematic analysis of prevalence, incidence, deaths, and dalys with projections to 2030. Int. J. Surg. 110 (4), 1951–1967. https://doi.org/10.1097/JS9.0000000000001071 (2024). Published 2024 Apr 1.
Chen, X. et al. Evolving trends and burden of inflammatory bowel disease in Asia, 1990–2019: A comprehensive analysis based on the global burden of disease study. J. Epidemiol. Glob Health. 13 (4), 725–739 (2023). Epub 2023 Sep 1. PMID: 37653213; PMCID: PMC10686927.
Xie, Y. et al. Analysis of the global burden of disease study highlights the global, regional, and National trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 94 (3), 567–581. https://doi.org/10.1016/j.kint.2018.04.011 (2018).
Møller, B. et al. Prediction of cancer incidence in the nordic countries: empirical comparison of different approaches. Stat. Med. 22 (17), 2751–2766. https://doi.org/10.1002/sim.1481 (2003).
Cui, A. et al. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine https://doi.org/10.1016/j.eclinm.2020.100587 (2020). 29–30:100587. Published 2020 Nov 26.
Song, M. et al. A comparison of the burden of knee osteoarthritis attributable to high body mass index in China and globally from 1990 to 2019. Front. Med. (Lausanne). 10, 1200294. https://doi.org/10.3389/fmed.2023.1200294 (2023). Published 2023 Aug 23.
Boettiger, D. C. et al. Projected impact of population aging on non-communicable disease burden and costs in the Kingdom of Saudi Arabia, 2020–2030. BMC Health Serv. Res. 23 (1), 1381. https://doi.org/10.1186/s12913-023-10309-w (2023). PMID: 38066590; PMCID: PMC10709902.
Swain, S., Sarmanova, A., Coupland, C., Doherty, M. & Zhang, W. Comorbidities in osteoarthritis: A systematic review and Meta-Analysis of observational studies. Arthritis Care Res. (Hoboken). 72 (7), 991–1000. https://doi.org/10.1002/acr.24008 (2020).
Nedunchezhiyan, U. et al. Obesity, inflammation, and immune system in osteoarthritis. Front. Immunol. 13, 907750. https://doi.org/10.3389/fimmu.2022.907750 (2022). Published 2022 Jul 4.
Hulshof, C. T. J. et al. The effect of occupational exposure to ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases: A systematic review and meta-analysis from the WHO/ILO joint estimates of the Work-related burden of disease and injury. Environ. Int. 150, 106349. https://doi.org/10.1016/j.envint.2020.106349 (2021).
Bruder, A. M., Haberfield, M. J., O’Brien, M. J. M. & Kemp, J. L. Women are disproportionately impacted by knee and hip osteoarthritis: why does this happen and how can we address it? Br. J. Sports Med. 58 (14), 756–757. https://doi.org/10.1136/bjsports-2024-108688 (2024). Published 2024 Jul 1.
Laitner, M. H., Erickson, L. C. & Ortman, E. Understanding the impact of sex and gender in osteoarthritis: assessing research gaps and unmet needs. J. Womens Health (Larchmt). 30 (5), 634–641. https://doi.org/10.1089/jwh.2020.8828 (2021).
Roman-Blas, J. A., Castañeda, S., Largo, R. & Herrero-Beaumont, G. Osteoarthritis associated with estrogen deficiency. Arthritis Res Ther. ;11(5):241. doi: 10.1186/ar2791. Epub 2009 Sep 21. PMID: 19804619; PMCID: PMC2787275. (2009).
Srikanth, V. K. et al. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthr. Cartil. 13 (9), 769–781. https://doi.org/10.1016/j.joca.2005.04.014 (2005).
de Matos, O. et al. Relationship between postural changes, osteoarthritis and bone mineral density in postmenopausal women. Gynecol. Endocrinol. 38 (11), 983–987. https://doi.org/10.1080/09513590.2022.2126454 (2022).
Blagojevic, M., Jinks, C., Jeffery, A. & Jordan, K. P. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthr. Cartil. 18 (1), 24–33. https://doi.org/10.1016/j.joca.2009.08.010 (2010).
Messing, K., Stock, S. R. & Tissot, F. Should studies of risk factors for musculoskeletal disorders be stratified by gender? Lessons from the 1998 Québec Health and Social Survey [published correction appears in Scand J Work Environ Health. ; 35(5):400]. Scand J Work Environ Health. 2009;35(2):96–112. (2009). https://doi.org/10.5271/sjweh.1310
Muraki, S. et al. Prevalence of radiographic knee osteoarthritis and its association with knee pain in the elderly of Japanese population-based cohorts: the ROAD study. Osteoarthr. Cartil. 17 (9), 1137–1143. https://doi.org/10.1016/j.joca.2009.04.005 (2009).
Tang, X. et al. The prevalence of symptomatic knee osteoarthritis in China: results from the China health and retirement longitudinal study. Arthritis Rheumatol. 68 (3), 648–653. https://doi.org/10.1002/art.39465 (2016).
Liu, Y. et al. Prevalence and associated factors of knee osteoarthritis in a rural Chinese adult population: an epidemiological survey. BMC Public. Health. 16, 94. https://doi.org/10.1186/s12889-016-2782-x (2016). Published 2016 Jan 30.
Cao, F. et al. Trends and cross-country inequalities in the global burden of osteoarthritis, 1990–2019: A population-based study. Ageing Res. Rev. 99, 102382. https://doi.org/10.1016/j.arr.2024.102382 (2024).
Bija, M. D. et al. Patterns of knee osteoarthritis in a hospital setting in sub-Saharan Africa. Clin. Rheumatol. 34 (11), 1949–1953. https://doi.org/10.1007/s10067-014-2702-3 (2015).
Veenhof, C., Huisman, P. A., Barten, J. A., Takken, T. & Pisters, M. F. Factors associated with physical activity in patients with osteoarthritis of the hip or knee: a systematic review. Osteoarthr. Cartil. 20 (1), 6–12. https://doi.org/10.1016/j.joca.2011.10.006 (2012).
Puts, M. T., Deeg, D. J., Hoeymans, N., Nusselder, W. J. & Schellevis, F. G. Changes in the prevalence of chronic disease and the association with disability in the older Dutch population between 1987 and 2001. Age Ageing. 37 (2), 187–193. https://doi.org/10.1093/ageing/afm185 (2008).
Green, A. Zimbabwe post-Mugabe era: reconstructing a health system. Lancet 391 (10115), 17–18. https://doi.org/10.1016/S0140-6736(18)30007-2 (2018).
Zhang, Y. & Jordan, J. M. Epidemiology of osteoarthritis [published correction appears in Clin Geriatr Med. ;29(2):ix]. Clin Geriatr Med. 2010;26(3):355–369. (2013). https://doi.org/10.1016/j.cger.2010.03.001
Hunter, D. J., Bierma-Zeinstra, S. & Osteoarthritis Lancet ;393(10182):1745–1759. doi:https://doi.org/10.1016/S0140-6736(19)30417-9 (2019).
Guermazi, A., Roemer, F. W. & Hayashi, D. Imaging of osteoarthritis: update from a radiological perspective. Curr. Opin. Rheumatol. 23 (5), 484–491. https://doi.org/10.1097/BOR.0b013e328349c2d2 (2011).
Vina, E. R. & Kwoh, C. K. Epidemiology of osteoarthritis: literature update. Curr. Opin. Rheumatol. 30 (2), 160–167. https://doi.org/10.1097/BOR.0000000000000479 (2018).
Woolf, A. D. & Pfleger, B. Burden of major musculoskeletal conditions. Bull. World Health Organ. 81 (9), 646–656 (2003).
Segal, N. A., Nilges, J. M. & Oo, W. M. Sex differences in osteoarthritis prevalence, pain perception, physical function and therapeutics. Osteoarthr. Cartil. 32 (9), 1045–1053. https://doi.org/10.1016/j.joca.2024.04.002 (2024).
Long, H. et al. Burden of osteoarthritis in China, 1990–2017: findings from the global burden of disease study 2017. Lancet Rheumatol. 2 (3), e164–e172. https://doi.org/10.1016/S2665-9913(19)30145-69 (2020).
Pal, C. P., Singh, P., Chaturvedi, S., Pruthi, K. K. & Vij, A. Epidemiology of knee osteoarthritis in India and related factors. Indian J. Orthop. 50 (5), 518–522. https://doi.org/10.4103/0019-5413.189608 (2016).
Funding
This work was supported by grants from the National Natural Science Foundation of China (82060871) and Jiangxi Province 2024 Science and Technology Special Funds (20243BCE51009).The funders had no role in the study design or in the collection, analysis, and interpretation of the data, writing of the report, or decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
W.M. and H.C. conceived and designed the study. X.C. downloaded the data. W.M. analyzed the data, while H.C. contributed to the interpretation of the results. Q.Y. was responsible for data visualization. W.M. and H.C. drafted the original manuscript, and H.L. revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
Weiwei Ma, Honggu Chen, Qipeng Yuan, Xiaoling Chen, and Huanan Li declare that they have no conflict of interest.
Ethical approval
This study does not require ethical approval, as it does not involve human participants, personal data, or animal subjects. All data utilized in this research are publicly available and de-identified, thus exempting it from the need for ethical review.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, W., Chen, H., Yuan, Q. et al. Global, regional, and national epidemiology of osteoarthritis in working-age individuals: insights from the global burden of disease study 1990–2021. Sci Rep 15, 7907 (2025). https://doi.org/10.1038/s41598-025-91783-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-91783-6
Keywords
This article is cited by
-
Global trends and hotspots in robot-assisted arthroplasty: a CiteSpace-based bibliometric and visualized analysis
Journal of Robotic Surgery (2025)