Abstract
The interspinous process motion (ISM) method can provide a more accurate assessment of postoperative subaxial cervical fusion than Cobb angle method which is used more commonly in clinical practice. However, the ISM method presents the measurement results in millimeters which cannot be directly compared with the Cobb angle measurement data. We proposed a modified measurement method for cervical functional spinal unit range of motion (FSU ROM) and evaluate its repeatability and reliability in measuring the ROM of the surgical segment after cervical artificial disc replacement surgery. A total of 81 patients who underwent cervical artificial disc replacement surgery in our department were retrospectively reviewed. Postoperative flexion-extension dynamic cervical radiographs were used for the measurement of FSU ROM of the surgical segment. The modified measurement method (M1) and the traditional Cobb angle measurement method (M2) were used. In the comparative analysis, there was no statistically significant difference between the two measurement methods (P > 0.05). Linear correlation study showed significant correlation between the two methods (P < 0.01), with a correlation coefficient of 0.947. Bland–Altman analysis showed the average difference between the two methods was 0.13°, the most of the measured data points fell within the 95% confidence interval. The M1 method demonstrated high intra-observer reliability (ICC = 0.957) and inter-observer reliability (ICC = 0.947). The M2 method showed good intra-observer reliability (ICC = 0.889) and good inter-observer reliability (ICC = 0.874). The M1 method yielded an SEM of 0.64° and an MDC of 1.49° for FSU ROM measurement, while the M2 method resulted in an SEM of 1.14° with an MDC of 2.66°.The modified measurement method for assessing cervical FSU ROM demonstrates satisfactory repeatability and reliability, provide higher measurement precision.
Similar content being viewed by others
Introduction
Measurement of the cervical functional spinal unit range of motion (FSU ROM) is a common method used for the functional assessment of the cervical spine. By measuring FSU ROM, we can assess bony fusion in the surgical segment after cervical fusion surgery1,2. This method can also be used to assess ROM of the affected segment both before and after cervical artificial disc replacement (CTDR) surgery. Flexion-extension radiograph Cobb angle measurement is the primary method for FSU ROM. This method shares the advantage of simple, efficient, and highly accurate, making it the most widely used in clinical practice3. Rhee JM et al. believe that the interspinous process motion (ISM) method can provide a more accurate assessment of postoperative subaxial cervical fusion. They recommend using less than 1-mm motion as the initial modality for determining anterior cervical arthrodesis for both clinical and research applications4. Similarly, for evaluating the functional status of artificial disc after CTDR surgery, ISM can also make precise and reliable assessments5,6. However, the measurement results of the ISM method are in millimeters. Therefore, this method cannot be directly compared with the Cobb angle measurement data which is used more commonly. This study proposed a modified measurement method for cervical FSU ROM. This method measuring the change in the angle between the line connecting spinous process ends and the anterior edge of the vertebral bodies of the upper and lower vertebrae in the responsible segment on dynamic flexion-extension radiographs. Since the spinous process ends are further away from the rotation center of the FSU, the modified method was expected to achieve precision comparable to the ISM, while providing angle values. In clinical practice, the modified method may offer a more accurate assessment of the prosthesis function after CTDR surgery, the intervertebral bone fusion after ACDF surgery, and the stability between vertebrae, by the consensus standards. The modified method is supposed to be preferable to Cobb angle measurement or ISM in those scenarios. In this study, this modified cervical FSU ROM method was compared with the traditional Cobb angle method. its repeatability and reliability were also analyzed.
Materials and methods
Study population
The study protocol was approved and the need for informed consent was waived by the Ethics Committee of Shanghai Changzheng Hospital (Project License No.2024SL027). This study adhered to the principles of the Declaration of Helsinki. Patients who underwent cervical total disc replacement (CTDR) surgery in our department were selected as the subjects for this study. Inclusion criteria: surgical treatment with the Discover artificial disc (Depuy Spine); regular postoperative follow-up; at least 12 months follow-up; postoperative flexion-extension radiographs of the cervical spine taken at our hospital; well-positioned artificial disc prostheses with no complications related to internal fixation; patients without neck pain or severe discomfort in the neck and shoulder. Exclusion criteria: concurrent thoracic or lumbar spine diseases; cervical trauma or fractures during follow-up; congenital and developmental spinal deformities; severe comorbidities or psychiatric conditions.
Postoperative flexion-extension radiographs of the cervical spine were collected. For patients with multiple follow-up visits, the radiographs with the best clarity were selected for the measurement of this study. The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Measure methods
The FSU ROM of the surgical segment was measured by the modified measurement method (M1) and the traditional Cobb angle method (M2) respectively. The AGFA IMPAX system was used for radiological measurements. Two experienced surgeons performed the measurements using both methods independently. Two weeks after the first measurement, a second measurement was conducted under the same conditions.
Traditional Cobb angle method
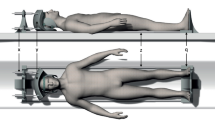
On flexion-extension radiographs of the cervical spine, reference lines are drawn parallel the upper endplate of the upper vertebral body and the lower endplate of the lower vertebral body of the surgical segment. The angles between these two reference lines were measured in both the extension and flexion positions (a positive value for cervical lordosis and a negative value for cervical kyphosis). As shown in Fig. 1.
Cervical FSU ROM measured by Cobb angle method. Along the upper endplate of the upper vertebral body and the lower endplate of the lower vertebral body of the surgical segment, we draw two reference lines. The angles between these two reference lines were measured in both the extension and flexion positions of the cervical spine on the radiographs. The angles formed on the lateral flexion radiographs are flexion angle. The angles formed on the extension radiographs are extension angles. The calculation formula is as follows: \({\text{Cervical FSU ROM = Cobb angle in extension position}} - {\text{Cobb angle in flexion position}}\).
Modified FSU ROM measurement method
On the lateral extension radiographs, drew a straight line from the highest point of the anterior edge of the upper vertebral body of the surgical segment to the end of the spinous process, and another straight line from the lowest point of the anterior edge of the lower vertebral body to the end of its spinous process. The angle between these two lines was the extension angle. Similarly, on the lateral flexion radiographs, draw two identical lines, and the angle between these lines was the flexion angle. As shown in Fig. 2.
Cervical FSU ROM measured by modified method. From the highest point of the anterior edge of the upper vertebral body and the lowest point of the anterior edge of the lower vertebral body to the end of their spinous process respectively, we drew two lines and constituted an angle. The angles formed on the lateral flexion radiographs are flexion angles. Same as the extension angles. The calculation formula is as follows: \({\text{Cervical FSU ROM = extension angle}} - {\text{flexion angle}}\).
Statistical analysis
GPowerWin_3.1.9.7 software (http://www.gpower.hhu.de/) was used for sample size calculation. According to the results of our previous study, the mean difference between the two methods is approximately 1°, with a standard deviation of the difference of about 3°7. The significance level (α) was set at 0.05 (two-sided), and the power (1-β) was set at 0.8. Data analyses were conducted using SPSS 17.0 software (SPSS Inc., USA). The comparison of the two measurement methods was conducted using a paired t-test. Intra-observer reliability and inter-observer reliability were analyzed using the intraclass correlation coefficient (ICC). The ICC values were assessed using the following criteria: 0.90–0.99 indicated high reliability, 0.80–0.89 indicated good reliability, 0.70–0.79 indicated fair reliability, and below 0.69 indicated poor reliability. The reliability of the two measurement methods was assessed using the standard error of measurement (SEM) and the minimum detectable change (MDC). SEM was equal to the square root of the mean square error term (residual) in the ICC variance analysis table. The minimum detectable change at a 90% confidence interval (MDC 90) was calculated using the following formula:
Pearson correlation analysis was used to analyze the correlation between the two measurement methods. Bland–Altman analysis was conducted using GraphPad Prism 6.01 software. P-value < 0.05 was considered statistically significant.
Result
Comparative analysis of general data
This study included a total of 81 patients who underwent CTDR surgery, of which 37 were male and 44 were female, aged between 33 and 55 years, with an average age of 43.1 ± 4.4 years. The patients were grouped based on different ages and genders, and the comparison of the two measurement results was conducted within each group as shown in Table 1. Across all groups, there were no significant differences observed in the results of the two measurement methods (P > 0.05 for all).
Correlation analysis of two measurement methods
There was a significant correlation between the two methods (P < 0.01), with a correlation coefficient of 0.947 (Fig. 3), and a 95% confidence interval (CI) of (0.919, 0.966). Bland–Altman analysis shown the average difference between the two methods was 0.13°, with the distribution of differences close to 0, and the most of measurement data points fell within the 95% CI (Fig. 4).
Intra-observer reliability analysis
The same surgeon used method M1 to measure the FSU ROM on two separate occasions, the ICC was 0.957, with a 95% confidence interval (CI) of (0.934, 0.972), and P < 0.01. This indicates high reliability of intra-observer reliability for the two measurements.
The same surgeon employed method M2 to measure the FSU ROM on two separate occasions, resulting in an ICC of 0.889, with a 95% CI of (0.833, 0.927), and a significance level of P < 0.01. These findings indicate a good intra-observer reliability for the two measurements.
Inter-observer reliability analysis
Two surgeons used method M1 to measure the FSU ROM, the ICC was 0.947, with a 95% CI of (0.918, 0.965), and P < 0.01. This indicates a high reliability of inter-observer reliability among different measurers.
Two surgeons used method M2 to measure the FSU ROM, resulting in an ICC of 0.874, with a 95% CI of (0.811, 0.917), and a significance level of P < 0.01. These findings suggest a good inter-observer reliability among the different measurers.
Reliability analysis of the two measurement methods
The SEM for FSU ROM measured by method M1 is 0.64°, and the MDC is 1.49°. For the traditional method M2, the SEM for FSU ROM measurement is 1.14°, and the MDC is 2.66°, as shown in Table 2.
Discussion
Measurement method for cervical FSU ROM
The assessment of cervical spine motion function is the most routine examination in spine surgery clinical practice8,9,10. The measurement of FSU ROM is used to assess the mobility of a single segment in the cervical spine. In terms of measurement methods, the traditional Cobb angle method remains the mainstream in clinical applications. This method is simple, efficient, and provides high accuracy and reliability for the measurement of the overall ROM of the cervical spine. However, for the measurement of FSU ROM, as the normal ROM of the FSU is about 10 degrees, and even less for the degenerated cervical spine, it proposes a higher requirement for measurement precision. With the innovation and development of digital imaging technology, the use of digital imaging data for measurement through imaging software has become widely applied in clinical practice and offers many advantages such as convenience, efficiency, and high accuracy11,12. Using the Cobb angle method to measure cervical spine ROM, studies have shown that the accuracy of computer-assisted measurement methods is superior to traditional radiograph film measurements, improving measurement precision by about 3°13. In the study by Janusz P et al., traditional cervical Cobb angle measurement had high reliability of intra-observer reliability, but there still existed a measurement standard deviation of 2–3 degrees14.
Errors in imaging measurements were mainly caused by the following reasons: ①Insufficiently standardized patient positioning during X-ray imaging, causing the measured endplates in the image data not to completely overlap in a straight line, affecting the selection of measurement reference lines15; ②Osteophyte formation, which commonly occurs at the anterior or posterior edges of the vertebral bodies during cervical degeneration, while these two locations were key points for choosing markers in cervical ROM measurements, the selection errors of these markers being the direct cause of deviations in measurement results; ③The C7 vertebra was often obscured by the shoulders, making it difficult to draw a line parallel to the lower endplate of C7 vertebra accurately during measurements. These measurement errors, while not significantly affecting the overall ROM of the cervical spine, cannot be ignored for the FSU ROM.
Advantages of the modified measurement method for cervical FSU ROM
The flexion-extension movement of the cervical FSU involves rotational movements of the upper and lower vertebrae around a rotational center. The traditional Cobb angle method involves selecting reference lines parallel to the endplates, with the measurement reference points being the anterior and posterior angles of the vertebrae. While the ISM is based on measuring the distance between the ends of the spinous processes of the upper and lower vertebrae. Since the ends of the spinous processes are farther from the rotational center of the upper and lower vertebrae, they can more significantly reflect the range of movement of the upper and lower vertebrae. Theoretically, when comparing the two methods, the ISM method is more precise and reliable. The modified measurement method used in this study is also based on the range of movement of the spinous process ends. The results of this study demonstrate the superior intra-observer and inter-observer reliability of the modified method compared to the traditional Cobb angle method. Additionally, the modified method primarily relies on the anterior angle of the vertebra and the end of the spinous process as measurement reference points, and the imaging of these two positions is often clearer. Even in some patients’ lateral radiographs where the C7 vertebra may be obscured by the shoulder, the anterior angle of the C7 vertebra and the end of the spinous process are often more easily identifiable. This is another reason why the M1 method yielded significantly lower SEM and MDC values. However, due to the difference in measurement units between the ISM and the modified method, it is inconvenient to compare the two, and further research is needed to explore differences in measurement precision. In addition, related research suggests that the ISM is more suitable for assessing bony fusion in the surgical segment after cervical fusion surgery16. Whether the modified measurement method also has similar advantages remains to be confirmed through further research.
Limitation
This study had several limitations. First, the sample size of this study was only 81 cases, and all patients included in this study were CTDR surgery patients with an age under 55. The bony structures of the cervical spine in this group of patients were clear, with no severe osteophytes or bone spurs that would affect the measurement, making measurement relatively simple. The validity and reliability of M1 for measuring cervical FSU ROM in elderly patients still need to be further explored through larger sample studies. Second, the measurement method had only been applied within our department, and all measurements were assisted by computer imaging software. It was necessary to conduct multi-center validation studies and compare the results from radiograph film measurements. Additionally, the subjects included in this study were all patients who had undergone CTDR. It was necessary to include patients with a variety of diseases in the measurement study to further clarify the applicability of this method.
Conclusion
The modified measurement method for assessing cervical FSU ROM demonstrates satisfactory repeatability and reliability, while also providing higher measurement precision.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Riffitts, M. et al. Functional range of motion of the cervical spine in cervical fusion patients during activities of daily living. J. Biomech. 152, 111528 (2023).
Silva, A. J. C. et al. Improvement and validation of a female finite element model of the cervical spine. J. Mech. Behav. Biomed. 142, 105797 (2023).
He, Z. et al. Assessment of cervical myelopathy risk in ossification of the posterior longitudinal ligament patients with spinal cord compression based on segmental dynamic versus static factors. Neurospine 20, 651–661 (2023).
Rhee, J. M. et al. Radiological determination of postoperative cervical fusion: A systematic review. Spine 40, 974–991 (2015).
Park, S. et al. Feasibility of local bone dust as a graft material in anterior cervical discectomy and fusion. J. neurosurg-spine. 31, 480–485 (2019).
Ballesteros, V. et al. Interspinous motion assessment in anterior cervical discectomy and fusion: Anterior plate versus zero profile implant. Global Spine J. 6, s-0036-1582756-s-1580036-1582756 (2016).
Zhou, J. et al. Preliminary application of a modified imaging measurement method for sagittal range of motion of cervical spine. J. Spinal Surg. 19, 5 (2021).
Wang, H. et al. Quantifying the ranges of relative motions of the intervertebral discs and facet joints in the normal cervical spine. J. Biomech. 112, 110023 (2020).
Fujishiro, T. et al. Significance of flexion range of motion as a risk factor for kyphotic change after cervical laminoplasty. J. Clin. Neurosci. 76, 100–106 (2020).
Sessumpun, K. et al. Characteristics of cervical spine motion in different types of cervical alignment: Kinematic MRI study. Clin. Spine Surg. 31, E239–e244 (2018).
Herrmann, A. M. & Geisler, F. H. A new computer-aided technique for analysis of lateral cervical radiographs in postoperative patients with degenerative disease. Spine 29, 1795–1803 (2004).
Frobin, W., Leivseth, G., Biggemann, M. & Brinckmann, P. Sagittal plane segmental motion of the cervical spine. A new precision measurement protocol and normal motion data of healthy adults. Clin. Biomech. 17, 21–31 (2002).
Wang, C. et al. [Computer-assisted versus traditional Cobb angle measurement on digital radiograph in scoliosis]. Zhonghua Yi Xue Za Zhi. 90, 1300–1303 (2010).
Janusz, P., Tyrakowski, M., Yu, H. & Siemionow, K. Reliability of cervical lordosis measurement techniques on long-cassette radiographs. Eur. Spine J. 25, 3596–3601 (2016).
Yo, K. et al. The reliabilities of several measurement methods of cervical sagittal alignment in cases with cervical spine rotation using X-ray findings in cervical spine disorders. Spine Surg. Relat. Res. 2, 186–196 (2018).
Ham, D. W., Choi, Y. S., Yoo, Y., Park, S. M. & Song, K. S. Measurement of interspinous motion in dynamic cervical radiographs using a deep learning-based segmentation model. J. Neurosurg-spine 39, 329–334 (2023).
Funding
This research was supported by grants from Naval Medical University Research Project (2022MS031). No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Contributions
J.W., H.Z. and B.H., are co-first authors, as they have equal contribution to the original and revised manuscript. J.W. contributed to conceptualization, methodology, software, investigation and writing—original draft. H.Z. contributed to conceptualization, investigation, writing—review & editing. B.H. contributed to formal analysis and investigation. F.Z. contributed to the patients’ data collection. W.Y., H.C. and L.L. contributed to the supervision and direction.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Shanghai Changzheng Hospital (Project License No.2024SL027).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, J., Zhou, H., Hu, B. et al. A modified measurement method for functional spinal unit ROM of cervical spine. Sci Rep 15, 7877 (2025). https://doi.org/10.1038/s41598-025-92658-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92658-6