Abstract
Acrolein (Acr) is a common volatile toxic substance excreted by the kidneys. There are no studies that specifically look at the effects of Acr on kidney function. This study was designed to investigate the relationship between Acr and kidney damage. A cross-sectional study of data (n = 4951) from the 2011–2018 National Health and Nutrition Examination Survey (NHANES) was conducted. Participants’ urinary Acr concentration, estimated glomerular filtration rate (eGFR), and urinary albumin to creatinine ratio (UACR) were recorded based on laboratory tests. The number of participants with chronic kidney disease (CKD) was counted. Urinary Acr concentration was divided into quartiles. The association of urinary Acr with CKD and eGFR was investigated using multivariate linear regression, multivariate logistic regression, and smooth curve fitting. Subgroup analyses, interaction tests and sensitivity analyses were used to examine the independence of the Acr-CKD and Acr-eGFR associations in the population. In 4951 participants, urinary Acr concentration was positively associated with CKD risk and negatively associated with eGFR. In the fully adjusted model, each log2Acr increase of one unit was associated with a 6% increased risk of CKD (OR = 1.06, 95% CI 1.01, 1.13) and a 0.54 mL/min/1.73 m2 decrease in eGFR (β = − 0.54, 95% CI − 0.95, − 0.13). For categorical log2Acr, for each log2Acr increase of one unit, the risk of CKD was 29% higher in the Q4 group than in the Q1 group (OR = 1.29, 95% CI 1.01, 1.64), while eGFR was 1.9 mL/min/1.73 m2 lower in the Q4 group than in the Q1 group (β = − 1.90, 95% CI − 3.65, − 0.14). Smooth curve fitting confirmed urinary Acr’s nonlinear positive and negative correlations with CKD and eGFR. According to subgroup analyses, sensitivity analyses and interaction tests, the confounding variables did not affect the independent correlations of urinary Acr with CKD and eGFR. Our study found that Acr exposure was significantly associated with kidney damage. Our study provides a new piece of research evidence to support a link between the volatile toxic substance Acr and a decline in kidney function.
Similar content being viewed by others
Introduction
Acrolein (Acr) is a toxic environmental contaminant that enters the human body through food and the respiratory tract. As a poisonous alpha, beta-unsaturated aldehyde, Acr is highly reactive and a potent irritant. Acr has a wide range of sources; it is not only emitted into the air from the combustion of fossil fuels, tobacco, plastics, and wood but is also formed during the heating of carbohydrates, fats, and amino acids in foods1. Of the many sources, the total amount of Acr inhaled through cigarettes exceeds that of all other sources combined2. The total amount of Acr produced in conventional cigarettes has been estimated to vary between 18.3 ug and 98.2 ug/cigarette3. Acr in cigarette smoke comes from the combustion of glycerol and carbohydrates, mainly carbohydrates. Stevens et al. found that cigarettes with 16% added sucrose could result in the release of up to 215 ug/cigarette of Acr4. Acr is highly water soluble. Upon entering the body, Acr rapidly binds to glutathione in liver cells to form a conjugate, which is then converted to N-acetyl-S-(3-hydroxypropyl)-l-cysteine (3HPMA) and N-acetyl-S-(2-carboxyethyl)-l-cysteine (CEMA) by n-acetylation and enzymatic cleavage in the kidneys, after which it is excreted in the urine as a secondary metabolite5.
Acr, a ubiquitous volatile toxic substance, is receiving increasing attention for its threat to human health. Recent research has linked Acr to a variety of diseases. As a respiratory irritant, Acr can cause pulmonary edema, acute lung injury, and chronic obstructive pulmonary disease. Inhalation of Acr through the respiratory tract can cause a number of reactions, including disruption of the integrity of the blood-gas barrier of the alveolar tissue, triggering an inflammatory response, production of large amounts of mucus, enlargement of the alveoli, and genetic mutations, ultimately leading to disease6. Increased Acr intake also affects the ability of endothelial cells to transport glucose, increasing the risk of developing type I and II diabetes7. In addition, Acr has been causally linked to multiple sclerosis8, cancer9, Alzheimer’s disease10, and cardiovascular disease11. High levels and prolonged exposure to Acr have raised public health concerns.
Chronic kidney disease (CKD) is now a public health problem that cannot be ignored and consumes a large amount of public health resources. It is estimated that more than 10% of the world’s population is currently diagnosed with CKD, and the trend is increasing year by year12. CKD disease is primarily characterized by structural and functional abnormalities of the kidneys that persist for more than three months13. There are many causes of CKD; congenital urinary tract disorders, infections, and glomerular disease are the leading causes of CKD in children14. In adult patients, hypertension, diabetes, infections, glomerulonephritis, and the use of nephrotoxic drugs are thought to be strongly associated with the development of CKD15,16. Environmental exposure and the ingestion of toxic substances are particularly prominent causes of kidney dysfunction. Studies have shown that exposure to the heavy metal nickel is strongly associated with decreased kidney function and the development of CKD17. Exposure to airborne organophosphate pesticides increases susceptibility to kidney damage and CKD risk18. Airborne particulate pollutants (PM2.5) have also been shown to decrease glomerular filtration rate and contribute to the development of CKD19. Previous studies have found that plasma Acr concentrations are up to six times higher in people with uremia than in normal people, and found that Acr concentrations are associated with the severity of CKD20. Sindhu also noted that it may not be spermine that acts as a uremic toxin in CKD patients, but rather Acr, an oxidized metabolite of spermine21. In a mouse model of diabetic nephropathy, Acr was also found to cause kidney fibrosis22. The unknown association between Acr, a specific and common volatile toxicant, and renal dysfunction piqued our interest. By elucidating the relationship between Acr exposure and kidney injury, it will help improve the ability to predict the effects of Acr exposure on kidney function.
In this cross-sectional study, we evaluated potential associations between Acr exposure and participants’ kidney function using data from the National Health and Nutrition Examination Survey (NHANES, 2011–2018). This provides valuable epidemiologic evidence for the association between Acr exposure and renal dysfunction. Importantly, more optimized and accurate public health solutions can be provided by articulating the relationship between the two. For the convenience of description, in this article, Acr refers to the amount of acrolein excreted in the urine. In this study, we hypothesized that participants with higher urinary Acr concentrations would have a higher risk of CKD compared to participants with lower urinary Acr concentrations.
Materials and methods
Study description and data inclusion
NHANES data from 2011 to 2018 were used for this study. NHANES is a cross-sectional survey of the U.S. civilian noninstitutionalized population conducted on 2-year cycles. Because NHANES uses a complex, stratified, multistage probabilistic cluster sampling design to assess participants’ health and nutritional status, its sample is representative. NHANES consists of five major modules: demographic information, diet, examination data, laboratory data, and questionnaire data. The National Center for Health Statistics (NCHS) Research Ethics Review Board has overseen and approved the data collection process. All participants provided written consent and were replaced by a unique serial number that identifies the specific NHANES program module in which the participant is participating. Detailed research procedures and information are publicly available at www.cdc.gov/nchs/nhanes/.
NHANES data for 39,156 participants from 4 cycles (2011–2012, 2013–2014, 2015–2016, 2017–2018) were included in this study because these four cycles contained complete Acr data. Details of each of the data modules are given in the following sections. Demographic information: sex, age, race, education level, and marital status. Examination data: body mass index (BMI). Laboratory data: CEMA, 3HPMA, urine creatinine, urine albumin, urine albumin to creatinine ratio (UACR), serum creatinine, alanine aminotransferase (ALT), aspartate aminotransferase (AST). Questionnaire: smoking status, drinking status, hypertension, diabetes, coronary heart disease (CHD), angina, stroke. Inclusion criteria: (1) Complete available CEMA and 3HPMA data. (2) Non-missing data on age, sex, race, and serum creatinine. (3) Complete UACR data. Exclusion criteria: (1) Demographic data that could not be used for analysis, such as “refused,” “missing,” and “don’t know.” (2) Missing or incomplete data on smoking status, drinking status, hypertension, diabetes, CHD, angina, and stroke in examination and questionnaire data.
Research variables
The exposure variable was urinary Acr metabolites. Acr is composed of two metabolic products, CEMA and 3HPMA. CEMA and 3HPMA are coded as “URXCEM” and “URXHPM,” respectively, in the Laboratory Data module. In NHANES 2011–2018, urinary concentrations of Acr metabolites were measured by ultra performance liquid chromatography coupled with electrospray tandem mass spectrometry (UPLC-ESI/MSMS) in mobile examination centers for determination23. After conversion to moles, the sum of CEMA and 3HPMA concentrations was used as the total urinary Acr concentration24. Owing to the skewed distribution (right-skewed) of the urinary Acr concentration, the data were log-transformed (log2) before analysis to bring the data closer to normal distribution for the accuracy of the results2. The outcome variable was CKD. The determination method of CKD is estimated glomerular filtration rate (eGFR) ≤ 60 mL/min/1.73 m2 or UACR ≥ 30.0 mg/g17. We used the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula, which is calculated as eGFR = 175 × standardized Scr−1.154 * age−0.203 * 1.212 [if black] * 0.742 [if female], and the unit is mL/min/1.73 m2 of body surface area25. Urinary albumin and urinary creatinine were measured by fluorescence immunoassay and Roche Cobas 6000 analyzer, respectively. Serum creatinine was measured using an enzymatic method in a Roche Cobas 6000 analyzer. Serum creatinine is converted to glycine and hydrogen peroxide under the action of creatininase, creatinase, and sarcosine oxidase. Hydrogen peroxide under the action of peroxidase can produce colored products (546 nm wavelength). In addition, we also included the continuous variable eGFR as an outcome variable in this study.
Covariates
The NHANES classification standard was used to classify some covariates as categorical variables. Sex is categorized as male and female. Race is categorized as Mexican American, other Hispanic, non-Hispanic white, non-Hispanic black, and other races. There are three categories for education levels: below high school, high school, and above high school. Three types of marital status are distinguished: never married, married/Living with partner, and divorced/separated/widowed. Regarding drinking status, participants were categorized as yes or no based on the question, "ever have 4/5 or more drinks every day? Participants’ smoking status was defined as yes if they had smoked at least 100 cigarettes in their lifetime and no if they had smoked less than 100 cigarettes. Lastly, the NHANES questionnaire classification criteria were used to classify CHD, angina, stroke, diabetes, and hypertension as yes or no. All covariate collection and measurement procedures are publicly available at http://www.cdc.gov/nchs/nhanes/.
Statistical analysis
All analyses were performed under the Centers for Disease Control and Prevention (CDC) guidelines. Because NHANES uses a complex stratified multistage sampling design, we applied appropriate sampling weights to minimize data variability during the analysis. R software (version 4.3.1, http://www.R-project.org) and EmpowerRCH software (version 4.1, www. empowerstats.com; X&Y Solutions, Inc., Boston MA) were used throughout the study for statistical analyses and image generation. Continuous variables are expressed as mean ± standard deviation; categorical variables are expressed as percentages. Acr was divided into quartile groups (Q1-Q4) from low to high concentrations to assess baseline characteristics of the study population. The statistical methods of weighted t-test and weighted chi-squared test were used to evaluate differences in baseline characteristics between groups after grouping Acr by quartiles. Three models in our construction. Multivariate logistic regression analysis assessed the association between Acr and the categorical variable CKD. To evaluate the relationship between Acr and eGFR, we performed multivariate linear regression analysis with eGFR as a continuous variable. Model 1 does not adjust for covariates. Model 2 adjusts for sex, age, and race. Model 3 (fully adjusted model) was further adjusted for education, marital status, BMI, ALT, AST, smoking status, drinking status, hypertension, diabetes, CHD, angina, and stroke based on model 2. We also analyzed the relationship between kidney dysfunction and Acr excretion by multivariate linear regression. Smooth curve fitting helped further discover potential correlations between Acr and CKD, eGFR. Subgroup analyses were used to assess the heterogeneity of the Acr-CKD relationship and the Acr-eGFR relationship among populations of different sex, age (< 60 and ≥ 60 years), race, marital status, BMI (< 18.5, 18.5–24.9, 25.0–29.9, ≥ 30), hypertension, and diabetes. In different subgroups (sex, age, race, marital status, BMI, hypertension, and diabetes), we use interaction tests to determine whether the interaction between Acr and CKD, eGFR is independent of these variables and remains stable across subgroups. It means that these variables affect the relationship between Acr and CKD, eGFR when P < 0.05. Sensitivity analyses were performed for stratification such as hypertension and diabetes. The criterion for statistical significance was set at a two-tailed P < 0.05.
Results
Baseline characteristics of participants
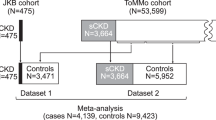
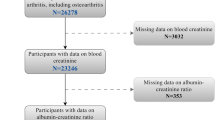
In total, 4951 eligible participants have been recruited between 2011 and 2018. The detailed research process is shown in Fig. 1. First, we excluded 28,636 participants with missing data on acrolein. Next, we excluded 2748 participants with missing data on eGFR and UACR. Participants with missing data on education, marital status, BMI, ALT, AST, drinking status, smoking status, hypertension, diabetes, CHD, angina, and stroke were next excluded, for a total of 2821 participants. The final inclusion was 4951 participants, all ≥ 20 years of age. On average, those participating were 47.40 (16.58) years old. 52.60% of them were men and 47.40% were women. The non-Hispanic white population was 68.34%. The concentration ranges of Q1–Q4 log2Acr were Q1: − 4.00 to 0.22 (≤ -0.22), Q2: − 0.22 to 0.74 (≤ 0.74), Q3: 0.74 to 1.73 (≤ 1.73), Q4: 1.73 to 7.18 (≤ 7.18), respectively. All participants’ mean eGFR and mean UACR were 89.15 (23.02) mL/min/1.73 m2 and 29.93 (209.63) mg/g, respectively. Of these, 14.97% of participants were diagnosed with CKD. Participants in the highest log2Acr group were more likely to have hypertension, diabetes, CHD, stroke, high ALT, high AST, and high urinary creatinine than those in the lowest log2Acr group (all P < 0.05). In addition, participants with higher log2Acr were more likely to be male, married/living with partner, non-Hispanic white, and generally had higher education and BMI (Table 1). Mean (SD) for age, eGFR, UACR.
Association of Acr with CKD and eGFR
The findings of multivariate logistic regression analysis and multivariate linear regression analysis for log2Acr-CKD and log2Acr-eGFR are displayed in Table 2. OR = 1, indicating that Acr is not associated with CKD. OR > 1, indicating that Acr exposure promotes CKD. OR < 1, indicating that Acr exposure inhibits CKD. β = 0 indicates that Acr has no correlation with eGFR. β > 0 indicates that Acr exposure increases eGFR. β < 0 indicates that Acr exposure decreases eGFR. The results showed that higher levels of log2Acr were associated with an increased risk of CKD and a reduced eGFR in all three models. In model 3, each 1-unit increase in continuous log2Acr was associated with a 6% increased risk of developing CKD (OR = 1.06, 95% CI 1.01,1.13). The risk of CKD increased with increasing log2Acr concentration compared to the lowest log2Acr concentration group (Q1). For each 1-unit increase in log2Acr, the risk of CKD in the Q4 group with the highest log2Acr concentration was 29% higher than the risk of CKD in the Q1 group (OR = 1.29, 95% CI 1.01, 1.64), P for trend 95% CI 1.01, 1.15; P = 0.0336. On the other hand, there was a negative correlation between log2Acr and eGFR. In model 3, for each 1-unit increase in continuous log2Acr, participants’ mean eGFR decreased by 0.54 mL/min/1.73 m2 (β = − 0.54, 95% CI − 0.95, − 0.13). In the categorical log2Acr, eGFR decreased with increasing log2Acr concentration compared to the lowest log2Acr concentration group (Q1). For each 1-unit increase in log2Acr, the eGFR of the Q4 group with the highest log2Acr concentration was 1.9 mL/min/1.73 m2 lower than that of the Q1 group with the lowest concentration (β = − 1.90, 95% CI − 3.65, − 0.14), P for trend 95% CI − 1.07, − 0.10; P = 0.0180. The results in Supplementary Table 1 show that kidney dysfunction was not significantly correlated with Acr excretion in model 3 (P > 0.05).
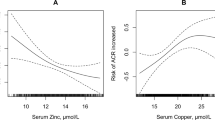
In addition, after adjustment for all covariates, we performed generalized model smoothing curve fitting analyses for log2Acr-CKD and log2Acr-eGFR (Fig. 2A,B). We found that log2Acr correlated positively with CKD and negatively with eGFR. The smoothed curve fitting results provide further evidence of the correlation described above.
Subgroup analysis
Based on the population factors of sex, age, race, marital status, BMI, hypertension, and diabetes, we performed subgroup analyses and interaction tests to examine the extent to which the associations of Acr with CKD and eGFR were stable in the general population and to identify possible population-specific settings. Our study shows that the correlation of Acr with CKD and eGFR varies modestly among the above population factors. In Married/Living with partner, there was a significant positive correlation between Acr and CKD (p < 0.05). Acr showed a valid positive association with CKD in all subgroups except age < 60 years, other Hispanic, other race, never married, divorced/separated/widowed, BMI < 18.5 kg/m2, and BMI ≥ 30 kg/m2, although not statistically significant (p > 0.05) (Fig. 3) For the relationship between Acr and eGFR, we observed a significant negative correlation between Acr and eGFR in age ≥ 60 years (p < 0.05). Acr showed a valid negative correlation with eGFR in all subgroups except non-Hispanic whites, BMI < 18.5 kg/m2, BMI ≥ 30 kg/m2, and diabetic patients, although not statistically significant (p > 0.05) (Fig. 4). The interaction tests of Acr with CKD and eGFR showed the same results. Acr’s independent correlations with CKD and eGFR were unaffected by these variables, as evidenced by the non-significant interactions for each of the subgroups (all P for interaction > 0.05).
Sensitivity analyses
Figures 5A,B show the sensitivity analysis curves for log2Acr-CKD in hypertension and diabetes stratification. Tables 3 and 4 show the results of threshold effects for log2Acr-CKD after stratification by hypertension and diabetes. The above results show that there is a significant positive correlation between log2Acr and CKD before inflection point (p < 0.05).
Discussion
In this cross-sectional study of 4951 participants, we observed an association between Acr and kidney damage. As we hypothesized, Acr exposure detected in urine was associated with impaired renal function. Urine Acr exposure levels were positively associated with CKD risk and negatively associated with eGFR. We confirm their relationship through regression modeling as well as smooth curve fitting. In model 3, the CKD risk and eGFR increased and decreased, respectively, with increasing log2Acr concentration compared with the lowest log2Acr concentration group (Q1). Moreover, this associated effect size was most pronounced in the group with the highest log2Acr concentration (Q4). Pre-existing kidney dysfunction does not affect Acr metabolism or excretion. The results of the smoothed curve fitting also corroborated the nonlinear positive and negative correlations between Acr exposure and CKD risk as well as eGFR. The stratification variables of age, sex, race, marital status, BMI, hypertension, and diabetes did not affect the association between Acr exposure and CKD risk and eGFR. Although the above results suggest that Acr exposure was significantly associated with kidney damage, we cannot establish a causal relationship.
Previous studies have shown that Acr, a highly toxic unsaturated aldehyde, can damage a wide range of tissues and organs when introduced into the body. The toxicity mechanism of Acr to the human body can be divided into two aspects: direct mechanism and indirect mechanism5. Direct mechanisms include the induction of DNA and protein cohesion and the damage of cell membranes. Indirect mechanisms such as induction of oxidative, pro-inflammatory, immune dysregulation, mitochondrial, and endoplasmic reticulum stress. Acr affects cellular physiological processes by targeting amino acid residues of important physiological significance, such as the sulfhydryl, imidazole, and amino groups26. Acr has carcinogenic properties manifested by the induction of interstrand cross-links in the double strands of DNA, DNA–protein cross-links, and the formation of Acr-DNA adducts27,28. This not only interferes with normal gene expression but can also cause critical genes to become mutated. For example, the accumulation of Acr adducts in mitochondria increases the high mutation rate in neurodegenerative diseases29. As another example, high levels of Acr-DNA adducts have been found in cancers of the lung, urothelium, and liver30,31,32. In addition, Acr can generate toxic reactive oxygen species such as superoxide radicals and hydroxyl radicals and diffuse into cellular tissues, leading to lipid peroxidation of proteins, enzymes, and DNA33. Acr exposure can cause dysplasia, necrosis, and metaplasia of respiratory epithelial cells in rats, as well as hemorrhage, ulceration, and cellular hyperplasia of the gastrointestinal mucosa, as reported by Faroon et al.34. On the whole, Acr damages tissue cells and affects normal physiological metabolism in multiple ways.
Acr, an environmental pollutant from a wide range of sources, especially from cigarettes, has now been found to be associated with a number of diseases. A study of 2027 participants by Feroe et al. found that elevated levels of urinary Acr metabolites were significantly associated with an increased risk of diabetes and decreased insulin sensitivity24. A study of 9536 participants by Lei et al.35 also found that the concentration of Acr metabolites was significantly higher in the urine of patients with rheumatoid arthritis than in the normal group and that there was a significant positive correlation with the risk of rheumatoid arthritis. Acr specifically by what way damage kidney? And that got us thinking. In a mouse model of nephropathy, Acr can induce modification changes in pyruvate kinase M2 and translocate it from the cytoplasm to the nucleus, causing aberrant activation of the HIF-1α pathway; activated HIF-1α induces cellular metabolism toward glycolysis, causing mitochondrial dysfunction and ultimately renal tubular injury and exacerbation of renal fibrosis36. In addition, in mouse models of ischemia–reperfusion, Acr was found to cause proximal renal tubular cell death and upregulate the expression of genes associated with renal fibrosis37,38. A strong link between the development of CKD and oxidative stress in the kidney has been demonstrated in relevant studies. Because of the frequent oxidative reactions of renal mitochondria, the kidney is an extremely metabolically active organ that is very sensitive to changes in oxidative stress39. Oxidative stress has been shown to contribute to the increased secretion of multiple inflammatory mediators by affecting the normal function of renal vascular endothelial cells, which is key to renal function impairment and CKD progression40. In the majority of cases, Acr is metabolized via glutathione. Excessive exposure to Acr causes glutathione levels to drop, which disrupts the body’s endogenous antioxidant defenses and causes oxidative stress41,42. Sen et al.43 found that sulforaphane inhibited Acr-mediated oxidative stress and inflammatory response and reduced glutathione consumption by upregulating the expression of Nrf-2 in peripheral blood mononuclear cells. Urinary Acr is an essential marker of oxidative stress; according to Taki et al.44 urinary Acr levels decreased significantly after renal function improvement in CKD patients treated with an oral adsorbent (Kremezin). In addition, Aihara et al.37 noted that exposure to Acr during acute kidney injury caused by tubular cell death may exacerbate acute kidney injury by promoting ischemia–reperfusion events. In summary, with the above analysis, we believe the association between Acr exposure and renal impairment in this study is reliable. Our work provides valuable evidence on the relationship between urinary Acr exposure and kidney damage and helps to provide reliable information for developing and implementing relevant programs.
However, the limitations of our work still warrant our attention. First, because all of the data in this work were derived from the NHANES database, the association between Acr and decreased kidney function may be more applicable to the general U.S. population. Second, since the renal function indicators were derived from the participants’ single urine sample, the repeated urine test results may represent the participants’ renal function status more. Third, other factors that may affect kidney function, such as diet, medication use, and physical activity, were not taken into account. Fourth, eGFR is estimated from serum creatinine combined with a specific formula and can be affected by a variety of factors such as muscle mass, age, diet, medications, etc.45 The study of the relationship between Acr and decreased kidney function is cross-sectional evidence. Although it is helpful in verifying the hypothesis and searching for evidence, it still lacks the ability to infer causality between the two.
Conclusion
This study found that Acr exposure was associated with decreased kidney function. Acr exposure was positively associated with CKD risk and negatively associated with eGFR. Nevertheless, further studies are needed to validate these findings and to unearth the pathological mechanisms of Acr-induced kidney damage.
Data availability
All NHANES data for this study are publicly available and can be found here: https://wwwn.cdc.gov/nchs/nhanes.
Abbreviations
- Acr:
-
Acrolein
- NHANES:
-
National Health and Nutrition Examination Survey
- NCHS:
-
National Center for Health Statistics
- eGFR:
-
Estimated glomerular filtration rate
- UACR:
-
Urinary albumin to creatinine ratio
- CKD:
-
Chronic kidney disease
- 3HPMA:
-
N-Acetyl-S-(3-hydroxypropyl)-l-cysteine
- CEMA:
-
N-Acetyl-S-(2-carboxyethyl)-l-cysteine
- BMI:
-
Body mass index
- CHD:
-
Coronary heart disease
References
Hikisz, P. & Jacenik, D. Diet as a source of acrolein: Molecular basis of aldehyde biological activity in diabetes and digestive system diseases. Int. J. Mol. Sci. 24(7), 6579 (2023).
Alwis, K. U., deCastro, B. R., Morrow, J. C. & Blount, B. C. Acrolein exposure in U.S. tobacco smokers and non-tobacco users: NHANES 2005–2006. Environ. Health Perspect. 123(12), 1302–1308 (2015).
Roemer, E. et al. Chemical composition, cytotoxicity and mutagenicity of smoke from US commercial and reference cigarettes smoked under two sets of machine smoking conditions. Toxicology 195(1), 31–52 (2004).
Stevens, J. F. & Maier, C. S. Acrolein: Sources, metabolism, and biomolecular interactions relevant to human health and disease. Mol. Nutr. Food Res. 52(1), 7–25 (2008).
Moghe, A. et al. Molecular mechanisms of acrolein toxicity: relevance to human disease. Toxicol. Sci. Off. J. Soc. Toxicol. 143(2), 242–255 (2015).
Bein, K. & Leikauf, G. D. Acrolein: A pulmonary hazard. Mol. Nutr. Food Res. 55(9), 1342–1360 (2011).
O’Toole, T. E. et al. Acrolein decreases endothelial cell migration and insulin sensitivity through induction of let-7a. Toxicol. Sci. Off. J. Soc. Toxicol. 140(2), 271–282 (2014).
Tully, M. & Shi, R. New insights in the pathogenesis of multiple sclerosis–role of acrolein in neuronal and myelin damage. Int. J. Mol. Sci. 14(10), 20037–20047 (2013).
Matilde Marques, M. et al. Carcinogenicity of acrolein, crotonaldehyde, and arecoline. Lancet Oncol. 22(1), 19–20 (2021).
Lopachin, R. M., Gavin, T. & Barber, D. S. Type-2 alkenes mediate synaptotoxicity in neurodegenerative diseases. Neurotoxicology 29(5), 871–882 (2008).
DeJarnett, N. et al. Acrolein exposure is associated with increased cardiovascular disease risk. J. Am. Heart Assoc. 3(4), e000934 (2014).
Eckardt, K. U. et al. Evolving importance of kidney disease: from subspecialty to global health burden. Lancet (London, England) 382(9887), 158–169 (2013).
Navaneethan, S. D. et al. KDOQI US commentary on the KDIGO 2024 clinical practice guideline for the evaluation and management of CKD. American J. Kidney Diseases Off. J. Natl. Kidney Found. 85(2), 135–176 (2025).
Harambat, J., van Stralen, K. J., Kim, J. J. & Tizard, E. J. Epidemiology of chronic kidney disease in children. Pediatr. Nephrol. (Berlin, Germany) 27(3), 363–373 (2012).
Romagnani, P. et al. Chronic kidney disease. Nat. Rev. Disease Primers 3, 17088 (2017).
Guo, X., Huang, M., Yang, D. & Luo, Z. Expression and clinical significance of plasma miR-223 in patients with diabetic nephropathy. Int. J. Endocrinol. 2023, 9663320 (2023).
Nan, Y., Yang, J., Ma, L., Jin, L. & Bai, Y. Associations of nickel exposure and kidney function in U.S. adults, NHANES 2017–2018. J. Trace Elem. Med. Biol. Organ Soc. Miner. Trace Elem. (GMS) 74, 127065 (2022).
Lv, J. et al. National temporal trend for organophosphate pesticide DDT exposure and associations with chronic kidney disease using age-adapted eGFR model. Environ. Int. 169, 107499 (2022).
Bowe, B. et al. Particulate matter air pollution and the risk of incident CKD and progression to ESRD. J. Am. Soc. Nephrol. JASN 29(1), 218–230 (2018).
Gugliucci, A. et al. Acrolein inactivates paraoxonase 1: Changes in free acrolein levels after hemodialysis correlate with increases in paraoxonase 1 activity in chronic renal failure patients. Clin. Chim. Acta 384(1–2), 105–112 (2007).
Sindhu, K. K. Uremic toxins: Some thoughts on acrolein and spermine. Renal Fail. 38(10), 1755–1758 (2016).
Kuo, C. W. et al. Pyruvate kinase M2 modification by a lipid peroxidation byproduct acrolein contributes to kidney fibrosis. Front. Med. 10, 1151359 (2023).
Alwis, K. U., Blount, B. C., Britt, A. S., Patel, D. & Ashley, D. L. Simultaneous analysis of 28 urinary VOC metabolites using ultra high performance liquid chromatography coupled with electrospray ionization tandem mass spectrometry (UPLC-ESI/MSMS). Analytica Chim. Acta 750, 152–160 (2012).
Feroe, A. G., Attanasio, R. & Scinicariello, F. Acrolein metabolites, diabetes and insulin resistance. Environ. Res. 148, 1–6 (2016).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Internal Med. 150(9), 604–612 (2009).
Bui, L. C. et al. Acrolein, an α, β-unsaturated aldehyde, irreversibly inhibits the acetylation of aromatic amine xenobiotics by human arylamine N-acetyltransferase 1. Drug Metab. Disposition Biol. Fate Chem. 41(7), 1300–1305 (2013).
Tang, M. S. et al. Acrolein induced DNA damage, mutagenicity and effect on DNA repair. Molecular Nutr. Food Res. 55(9), 1291–1300 (2011).
Voulgaridou, G. P., Anestopoulos, I., Franco, R., Panayiotidis, M. I. & Pappa, A. DNA damage induced by endogenous aldehydes: Current state of knowledge. Mutat. Res. 711(1–2), 13–27 (2011).
Kasiviswanathan, R., Minko, I. G., Lloyd, R. S. & Copeland, W. C. Translesion synthesis past acrolein-derived DNA adducts by human mitochondrial DNA polymerase γ. J. Biol. Chem. 288(20), 14247–14255 (2013).
Park, S. L. et al. Quantitation of DNA adducts resulting from acrolein exposure and lipid peroxidation in oral cells of cigarette smokers from three racial/ethnic groups with differing risks for lung cancer. Chem. Res. Toxicol. 35(10), 1914–1922 (2022).
Hong, J. H. et al. Acrolein contributes to urothelial carcinomas in patients with chronic kidney disease. Urol. Oncol. 38(5), 465–475 (2020).
Kawai, Y., Furuhata, A., Toyokuni, S., Aratani, Y. & Uchida, K. Formation of acrolein-derived 2’-deoxyadenosine adduct in an iron-induced carcinogenesis model. J. Biol. Chem. 278(50), 50346–50354 (2003).
Jeelani, R. et al. Cyclophosphamide and acrolein induced oxidative stress leading to deterioration of metaphase II mouse oocyte quality. Free Radic. Biol. Med. 110, 11–18 (2017).
Faroon, O. et al. Acrolein health effects. Toxicol. Ind. Health 24(7), 447–490 (2008).
Lei, T., Qian, H., Yang, J. & Hu, Y. The exposure to volatile organic chemicals associates positively with rheumatoid arthritis: A cross-sectional study from the NHANES program. Front. Immunol. 14, 1098683 (2023).
Li, S. Y. et al. Aldehyde dehydrogenase 2 preserves kidney function by countering acrolein-induced metabolic and mitochondrial dysfunction. JCI Insight 9(19), e179871 (2024).
Aihara, S., Torisu, K., Hirashima, Y., Kitazono, T. & Nakano, T. Acrolein produced during acute kidney injury promotes tubular cell death. Biochem. Biophys. Res. Commun. 666, 137–145 (2023).
Liu, C. et al. A new LKB1 activator, piericidin analogue S14, retards renal fibrosis through promoting autophagy and mitochondrial homeostasis in renal tubular epithelial cells. Theranostics 12(16), 7158–7179 (2022).
Honda, T., Hirakawa, Y. & Nangaku, M. The role of oxidative stress and hypoxia in renal disease. Kidney Res. Clin. Pract. 38(4), 414–426 (2019).
Zhang, S., Tang, H., Zhou, M. & Pan, L. Sexual dimorphism association of combined exposure to volatile organic compounds (VOC) with kidney damage. Environ. Res. 258, 119426 (2024).
Rahman, I. & Adcock, I. M. Oxidative stress and redox regulation of lung inflammation in COPD. Eur. Respir. J. 28(1), 219–242 (2006).
Ansari, M. A., Keller, J. N. & Scheff, S. W. Protective effect of pycnogenol in human neuroblastoma SH-SY5Y cells following acrolein-induced cytotoxicity. Free Radic. Biol. Med. 45(11), 1510–1519 (2008).
Qin, W. S., Deng, Y. H. & Cui, F. C. Sulforaphane protects against acrolein-induced oxidative stress and inflammatory responses: Modulation of Nrf-2 and COX-2 expression. Arch. Med. Sci. AMS 12(4), 871–880 (2016).
Taki, K. & Niwa, T. Indoxyl sulfate-lowering capacity of oral sorbents affects the prognosis of kidney function and oxidative stress in chronic kidney disease. J. Renal Nutr. Off. J. Council Renal Nutr. Natl. Kidney Found. 17(1), 48–52 (2007).
van der Velde, M., Bakker, S. J., de Jong, P. E. & Gansevoort, R. T. Influence of age and measure of eGFR on the association between renal function and cardiovascular events. Clin. J. Am. Soc. Nephrol. CJASN 5(11), 2053–2059 (2010).
Acknowledgements
We thank the National Center for Health Statistics of the Centers for Disease Control staff for designing, collecting, and collating the NHANES data and creating the public database.
Funding
This work was supported by the Guangxi Medical and Health Appropriate Technology Development and Extension and Application Project (grant/award number: S2021094).
Author information
Authors and Affiliations
Contributions
Conceptualization, X.P.; data curation, J.M.; formal analysis, J.M. and Y.L.; methodology, J.M. and Y.C.; software, Y.C., and W.L.; supervision, X.P.; writing—original draft, J.M., Y.L., and X.P.; writing—review and editing, J.M., Y.L. and X.P.; visualization, Y.C., Y.Z., and W.L.; All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This research analyzed de-identified information downloaded from the National Health and Nutrition Examination Survey public database. The National Center for Health Statistics Ethics Review Committee granted ethics approval. All methods were carried out in accordance with relevant guidelines and regulations (declaration of Helsinki). All individuals provided written informed consent before participating in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, J., Lu, Y., Cai, Y. et al. Acrolein exposure associated with kidney damage: a cross‑sectional study. Sci Rep 15, 8682 (2025). https://doi.org/10.1038/s41598-025-93698-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93698-8