Abstract
Sepsis is a severe systemic inflammatory response, and sepsis-associated acute kidney injury (SA-AKI) is one of its most common complications. The pan-immune inflammation value (PIV), a novel inflammatory index, is designed to comprehensively reflect the status of systemic immune and inflammatory responses. However, the relationship between PIV and short-term clinical outcomes in SA-AKI patients remains unclear. This study was a retrospective analysis of SA-AKI patients from the MIMIC-IV database. The Boruta algorithm was used to identify key features predicting short-term mortality in SA-AKI patients. The relationships between ln (PIV) and all-cause mortality at 28 days and 90 days were assessed via multivariate Cox proportional hazards regression, subgroup analysis, sensitivity analysis, restricted cubic spline (RCS) modelling, and Kaplan‒Meier (K–M) survival analysis. A total of 4369 patients were included in the study, of whom 57.0% were male. Boruta analysis indicated that ln (PIV) was an important clinical feature. The results of multivariable Cox regression analysis revealed a positive correlation between ln (PIV) and mortality risk at both 28 days and 90 days (HR [95% CI] = 1.057 [1.009, 1.106], P = 0.019; HR [95% CI] = 1.075 [1.032, 1.120], P < 0.001). The RCS model revealed a nonlinear relationship between ln (PIV) and mortality at 28 and 90 days, with a critical threshold of 6.72. Above this threshold, a higher ln (PIV) was associated with increased mortality risk at both time points; sensitivity analyses confirmed that this association remained significant after specific patients were excluded. Subgroup analyses revealed that ln (PIV) significantly affected short-term mortality in diabetic patients (P < 0.05). Ln (PIV) is closely associated with short-term mortality in ICU patients with SA-AKI, suggesting its potential application in early risk assessment and clinical intervention.
Similar content being viewed by others
Introduction
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection1. Despite advances in understanding its pathophysiology, mechanisms, and treatment, the incidence and mortality of sepsis have decreased only slightly in recent years2. Sepsis remains a leading cause of death and critical illness worldwide3. Acute kidney injury (AKI) is particularly common among its complications. Studies have shown that more than 50% of AKI cases are associated with sepsis4,5,6. Sepsis-associated acute kidney injury (SA-AKI) is closely linked to adverse clinical outcomes, including prolonged hospital stays, increased cardiovascular event risks, and elevated mortality rates7,8. Given these severe consequences, the early identification of patients at risk for SA-AKI, followed by timely and appropriate interventions, is crucial for preventing further renal damage and improving patient prognosis.
Although commonly used scoring systems assist in identifying the prognosis of sepsis patients, their effectiveness remains suboptimal. Furthermore, many of these systems include an excessive number of indicators, making them cumbersome to use, especially in clinical settings with limited medical resources, such as the emergency department. Therefore, finding a routinely available index for the early identification of high-risk sepsis patients with poor prognoses remains crucial. A prominent feature of sepsis is the early dysregulation of systemic inflammation and the immune response. In recent years, indicators related to inflammation and immune status analyses, particularly those that can accurately predict the risk of adverse outcomes in sepsis patients, have shown significant potential9.
Recently, a novel index known as the pan-immune-inflammation value (PIV), which integrates neutrophil, platelet, monocyte, and lymphocyte counts, has garnered increasing attention. PIV is considered a comprehensive of systemic inflammation and immune status and has been identified as a key indicator of the host immune response10,11. Elevated PIV values are associated with poor prognosis in a variety of conditions, including hypertension, malignancy, vasculitis, and sepsis12,13,14,15,16. In light of these findings, it seems reasonable to hypothesize that PIV may be associated with 28-day mortality in patients with SA-AKI. However, no previous studies have specifically addressed this potential link. Therefore, the aim of this study was to explore the relationship between PIV and 28-day mortality in patients with SA-AKI.
Methods
Data source
This study is based on the publicly available MIMIC-IV database (Version 2.2)17,18, a critical care database developed by the Complex Systems Monitoring Group at Beth Israel Deaconess Medical Center (BIDMC) in Boston, Massachusetts. The dataset includes comprehensive records of over 50,000 patients admitted between 2008 and 2019. Since the database is anonymous and deidentified, the BIDMC Institutional Review Board approved the waiver of informed consent and authorized the use of the data for research purposes. Data extraction was performed by the corresponding author, Heping Xu, who was granted access to the database after completing the CITI Program online training (Record ID: 59,568,270).
Definitions
The PIV was calculated as [neutrophil count (103/mm3) × platelet count (103/mm3) × monocyte count (103/mm3)/lymphocyte count (103/mm3)]12. Sepsis was diagnosed according to the Sepsis-3 criteria and required a Sequential Organ Failure Assessment (SOFA) score of 2 or higher. Septic shock was defined as sepsis with a lactate level greater than 2.0 mmol/L and the need for vasopressor support1. Acute kidney injury (AKI) is defined according to the KDIGO guidelines, which include either an increase in serum creatinine (SCr) of ≥ 0.3 mg/dL within 48 h from baseline or urine output < 0.5 mL/kg/h for at least 6 hours19. Baseline serum creatinine is defined as the lowest serum creatinine level within the 7 days prior to admission and serves as a reference for KDIGO staging20. SA-AKI is defined as the new onset of AKI within 7 days of hospital admission in a patient with sepsis21.
Participants
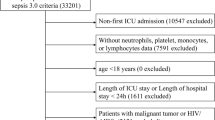
Participants diagnosed with SA-AKI were included in the study. The exclusion criteria were as follows: (a) non-first ICU admission; (b) absence of neutrophil, platelet, monocyte, or lymphocyte count data on the first day of ICU admission, as the calculation of PIV is essential; (c) age < 18 years; (d) ICU or hospital stay of less than 24 h; and (e) a history of chronic kidney disease. A total of 4369 patients with SA-AKI were included in the final analysis. The study flow chart of the population is shown in Fig. 1.
Outcome
The primary endpoint was 28-day all-cause mortality, whereas the secondary endpoint was all-cause mortality at 90 days.
Data extraction
This study utilized PostgreSQL software to extract a dataset from the MIMIC-IV, which included comprehensive demographic and clinical variables such as age, sex, ethnicity, weight, history of myocardial infarction, congestive heart failure, chronic pulmonary disease, diabetes, and cerebrovascular disease. It also includes initial SOFA scores, the Simplified Acute Physiology Score II (SAPS II), and the Charlson Comorbidity Index. The recorded vital signs included systolic and diastolic blood pressure, mean arterial pressure, heart rate, respiratory rate, temperature, and pulse oximetry readings. The laboratory parameters included white blood cell count, haemoglobin, platelet count, anion gap, bicarbonate, chloride, glucose, sodium, potassium, creatinine, blood urea nitrogen, calcium, prothrombin time, albumin, neutrophils, platelets, monocytes, and lymphocytes. The monitored clinical outcomes included septic shock, renal replacement therapy (RRT), invasive mechanical ventilation, in-hospital mortality, and mortality at 28 and 90 days. The ICU length of stay and total hospital stay were also recorded.
Statistical analysis
In this study, owing to the skewed distribution of PIV, a natural logarithm transformation (ln (PIV)) was applied before analysis. Continuous variables are expressed as the means (standard deviations) or medians (interquartile ranges), whereas categorical variables are presented as percentages. The baseline characteristics across different ln (PIV) categories were assessed via chi-square tests for categorical data, one-way analysis of variance (ANOVA) for normally distributed continuous data, and the Kruskal‒Wallis H test for nonnormally distributed continuous data.
To identify key features that predict short-term mortality in SA-AKI patients, we employed the Boruta algorithm to assess the significance of ln (PIV) as a predictor. This algorithm determines feature importance by comparing the Z value of each real feature with the maximum Z value of its corresponding "shadow feature." If a feature’s Z value is significantly greater than the maximum Z value of the shadow feature across multiple independent tests, it is marked as “important” (green area); otherwise, it is marked as “unimportant” (red area) and excluded from the feature selection process. The default parameters for the Boruta algorithm include a significance level of P = 0.01 and a maximum of 100 iterations22.
To explore the relationship between ln (PIV) and short-term all-cause mortality in SA-AKI patients, multivariable Cox proportional hazards regression analysis was performed. The assumption of multicollinearity was also evaluated by calculating the variance inflation factor (VIF). A VIF greater than 5 was considered indicative of multicollinearity between independent variables23. The Boruta algorithm identified 25 important features, including ln (PIV). Four models were developed, each adjusted stepwise: Model 1 was the unadjusted baseline model; Model 2 adjusted for age, sex, ethnicity, and weight-related variables; Model 3 further adjusted for cerebrovascular disease, SBP, heart rate, respiratory rate, temperature, SpO2, the Charlson comorbidity index, SOFA score, SAPSII score, septic shock, invasive ventilation, and RRT; and Model 4, based on Model 3, additionally adjusted for white blood cell count, haemoglobin, anion gap, calcium, blood urea nitrogen, potassium, creatinine, prothrombin time, glucose, and albumin. Subgroup analyses were conducted on the basis of age (< 65 and ≥ 65 years), sex, ethnicity, history of myocardial infarction, congestive heart failure, cerebrovascular disease, chronic pulmonary disease, diabetes, invasive ventilation, and septic shock.
Sensitivity analyses included Cox proportional hazards regression, excluding patients with myocardial infarction or cerebrovascular disease, to further validate the results. To ensure the robustness of the findings, patients whose ICU stay was less than 2 days were also excluded. To determine the nonlinear relationship between ln (PIV) and short-term mortality in SA-AKI patients, restricted cubic spline curves were plotted. Kaplan‒Meier survival analysis was used to compare the survival rates of SA-AKI ICU patients stratified by ln (PIV) and assess the impact of ln (PIV) on short-term mortality in SA-AKI patients. All the data analyses were performed via R version 4.2.1 and Stata version 18.0. Statistical tests were two-sided, and a P value of less than 0.05 was considered statistically significant.
Ethics approval
MIMIC-IV is an anonymized public database approved by the institutional review boards of the Massachusetts Institute of Technology (MIT) and Beth Israel Deaconess Medical Center (BIDMC). The requirement for informed consent was waived because of the thorough anonymization and deidentification of all patient information in the database.
Results
Baseline characteristics
This study included a total of 4369 patients with SA-AKI, as illustrated in Table 1. The baseline characteristics of the study population, stratified by the ln (PIV) index, are presented. The mean age of the patients was 65.2 years (SD = 16.1), with 57.0% of the participants being male and 65.2% Caucasian. The 28-day and 90-day mortality rates were 20.3% and 26.0%, respectively. Compared with patients with a ln (PIV) index ≤ 6.72, those with higher ln (PIV) values presented significantly increased rates of body weight, congestive heart failure, chronic lung disease, and invasive ventilation. Higher ln (PIV) levels were also associated with higher SAPSII scores, heart rates, respiratory rates, white blood cell (WBC) counts, and blood urea nitrogen (BUN) levels, as well as longer intensive care unit (ICU) stays and total hospital stays. Patients with higher ln (PIV) values had significantly higher 28-day and 90-day mortality rates than did those with lower ln (PIV) values.
Boruta algorithm
We applied the Boruta algorithm to identify features associated with 28-day and 90-day mortality in patients with SA-AKI, as shown in Fig. 2. In the Boruta analysis, variables in the green area were classified as important features, whereas those in the red area were considered irrelevant. The results revealed that when the Boruta algorithm was used, 25 important features were selected, with ln (PIV) consistently identified as a significant predictor of both 28-day and 90-day mortality risk.
Feature selection for predicting short-term mortality risk via the Boruta algorithm. The horizontal axis represents the name of each variable, and the vertical axis represents the Z value of each variable. The box plot shows the Z value of each variable during model calculation. The green boxes represent important variables, and the red boxes represent unimportant variables. SBP, systolic blood pressure; DBP, diastolic blood pressure; MBP, mean blood pressure; SpO2, pulse oxygen saturation; MI, myocardial infarction; CHF, congestive heart failure; CD, cerebrovascular disease; CPD, chronic pulmonary disease; RRT, renal replacement therapy; CCI, Charlson comorbidity index; SOFA, Sequential Organ Failure Assessment score; SAPS II, simplified acute physiology score II; WBC, white blood cell; BUN, blood urea nitrogen; PT, prothrombin time.
Association between ln (PIV) and short-term mortality
The relationships between ln (PIV) and 28-day and 90-day mortality are presented in Table 2. The ln (PIV) index was categorized into two groups for analysis. Four Cox proportional hazards regression models were constructed to evaluate the independent effect of ln (PIV) on mortality in ICU patients with SA-AKI. The results indicated that higher ln(PIV) values were associated with an increased risk of 28-day all-cause mortality in SA-AKI patients (Model 1: hazard ratio [HR] = 1.141, 95% confidence interval [CI] 1.088–1.196, P < 0.001; Model 2: HR = 1.125, 95% CI 1.073–1.180, P < 0.001; Model 3: HR = 1.088, 95% CI 1.041–1.138, P < 0.001; Model 4: HR = 1.057, 95% CI 1.009–1.106, P = 0.019). A similar trend was observed for 90-day all-cause mortality.
Additionally, we analysed ln (PIV) as a categorical variable. Compared with patients in the lower ln(PIV) group (ln[PIV] ≤ 6.72), those in the higher ln(PIV) group presented an increased risk of 28-day mortality (Model 1: HR = 1.667, 95% CI 1.421–1.955, P < 0.001; Model 2: HR = 1.592, 95% CI 1.357–1.869, P < 0.001; Model 3: HR = 1.479, 95% CI 1.257–1.738, P < 0.001; Model 4: HR = 1.343, 95% CI 1.137–1.588, P < 0.001). A similar pattern was observed in the association between ln (PIV) and 90-day all-cause mortality.
Restricted cubic spline
We used restricted cubic spline regression to assess the shape of the relationship between ln (PIV) and mortality risk and to establish a threshold for ln (PIV). The results indicated that, after adjusting for confounding factors, there was a nonlinear relationship between ln (PIV) and 28-day and 90-day all-cause mortality in SA-AKI patients (P < 0.05). Specifically, when ln (PIV) was less than 6.72, no significant association was found between ln (PIV) and 28-day or 90-day all-cause mortality [HR (95% CI) = 0.921 (0.840, 1.009), P = 0.077; HR (95% CI) = 0.931 (0.859, 1.008), P = 0.078]. In contrast, when ln (PIV) exceeded 6.72, a positive correlation was observed between ln (PIV) and both 28-day mortality and 90-day mortality [HR (95% CI) = 1.090 (1.005, 1.205), P = 0.023; HR (95% CI) = 1.141 (1.045, 1.247), P = 0.003], as shown in Fig. 3.
Kaplan‒Meier analysis
Patients were categorized into two groups on the basis of the ln(PIV) index (T1: ≤ 6.72, T2: > 6.72), and Kaplan‒Meier survival analysis was used to assess the 28-day and 90-day mortality rates in SA-AKI patients. As shown in Fig. 4, the survival curve for the T2 subgroup was significantly lower than that for the T1 subgroup (log-rank test, P < 0.0001), suggesting that higher ln (PIV) levels at admission are associated with increased short-term mortality risk.
Subgroup analysis
To explore potential clinical heterogeneity, we conducted interaction and stratified analyses (Fig. 5). We assessed the relationships between ln (PIV) and 28-day and 90-day mortality in different subgroups of SA-AKI patients stratified by age (< 65 years and ≥ 65 years), sex, ethnicity, history of myocardial infarction, congestive heart failure, cerebrovascular disease, chronic pulmonary disease, diabetes, invasive ventilation, and septic shock. Significant interaction effects were observed only in the diabetes subgroup (P < 0.05) for both 28-day and 90-day mortality. No significant interactions were found in the other subgroups. The results indicated that, in the diabetes subgroup, higher ln (PIV) levels were associated with an increased risk of short-term mortality.
Effect size of ln (PIV) on short-term mortality in prespecified and exploratory subgroups. The effect size was adjusted for age, sex, ethnicity, weight, cerebrovascular disease, Charlson comorbidity index, SOFA score, SAPSII score, septic shock, invasive ventilation, RRT, SBP, heart rate, respiratory rate, temperature SpO2, white blood cell count, haemoglobin, anion gap, potassium, blood urea nitrogen, calcium, creatinine, prothrombin time, glucose and albumin, with the exception of the subgroup variable.
Sensitivity analysis
The results of the sensitivity analysis are presented in Table 3. After patients with a history of myocardial infarction were excluded, the hazard ratios (HRs) for 28-day and 90-day mortality were 1.078 (95% CI 1.024–1.134) and 1.095 (95% CI 1.047–1.145), respectively. After excluding patients with cerebrovascular disease, the HRs for 28-day and 90-day mortality were 1.056 (95% CI: 1.004–1.110) and 1.071 (95% CI 1.024–1.120), respectively. Additionally, after patients with an ICU stay of less than 2 days were excluded, the HRs for 28-day and 90-day mortality remained consistent at 1.058 (95% CI 1.009–1.108) and 1.077 (95% CI 1.033–1.1230), respectively. We also analysed ln PIV) as a categorical variable on the basis of tertiles, and the associations between ln PIV and 28-day and 90-day mortality in SA-AKI patients remained stable.
Discussion
In this study, we first analysed the relationship between PIV and 28-day mortality in patients with SA-AKI. The results revealed that higher ln (PIV) values were significantly associated with increased 28-day all-cause mortality in SA-AKI patients, and this relationship remained significant after adjusting for multiple confounders. Furthermore, we found a distinct nonlinear relationship between ln (PIV) and 28-day mortality. Specifically, when ln (PIV) exceeded 6.72, the risk of death increased sharply, whereas below this threshold, the difference in mortality risk was not statistically significant. Kaplan‒Meier survival analysis further confirmed this finding, showing that patients with high ln (PIV) values (T3 group) had significantly higher mortality rates. Sensitivity analyses demonstrated the robustness of this conclusion across different subgroups, suggesting that ln (PIV) could serve as an independent predictor of short-term mortality in SA-AKI patients. These findings provide a novel perspective for risk assessment and prevention strategies in SA-AKI patients.
In contrast to previous studies that focused on the application of PIV in cancer and cardiovascular events, limited research has explored the relationship between PIV and SA-AKI. Giovanni Fuca et al. first proposed PIV as a new systemic inflammatory marker in 2020 and reported that PIV could predict survival outcomes in patients with metastatic colorectal cancer12. Similarly, studies on locally advanced head and neck squamous cell carcinoma (HNSCC) have indicated that higher PIV values are associated with poorer overall survival and disease-free survival, suggesting that PIV may serve as a prognostic marker for HNSCC24. Bektas Murat et al. reported that PIV demonstrated good prognostic value for all-cause mortality at one month and one year in patients with STEMI (ST-elevation myocardial infarction) and was positively correlated with long-term all-cause and cardiovascular mortality in hypertensive patients25. Although these studies have confirmed the prognostic value of PIV in cancer and cardiovascular diseases, the role of PIV in sepsis and SA-AKI has not received much attention. Xu HB et al. reported that PIV was significantly associated with short-term mortality risk in sepsis patients, suggesting that PIV may have applications in the prognostic assessment of sepsis and SA-AKI patients9. Our study further supports this view, showing that higher PIV values are associated with higher short-term mortality, and the potential of ln (PIV) as an independent prognostic factor warrants further attention.
Sepsis, a critical illness involving immune and inflammatory responses, is one of the major causes of AKI26. The occurrence of sepsis involves complex immune and inflammatory responses, and PIV, a novel index, has gradually attracted increasing attention in the clinic12. By combining the neutrophil, platelet, monocyte, and lymphocyte counts, PIV reflects the systemic immune and inflammatory status of the body27,28. In sepsis, neutrophil counts increase, but their antimicrobial functions are often suppressed, leading to reduced pathogen clearance and an increased risk of secondary infections29. Monocytes play an important role in immune responses, and their numbers and functions change during sepsis30,31. Platelets are involved in haemostasis and can modulate inflammation through interactions with immune cells32. In sepsis, lymphocyte apoptosis, particularly that of T cells, increases, leading to immune suppression and an impaired response to infections33,34. Therefore, elevated PIV reflects abnormal systemic immune and inflammatory responses, which may affect the occurrence and mortality risk of SA-AKI through several mechanisms: (1) Immune and inflammatory dysregulation: the systemic inflammatory response triggered by sepsis may exacerbate acute kidney injury. Elevated PIV suggests immune dysfunction or an excessive inflammatory response, which can aggravate kidney damage and increase mortality risk1. (2) Neutrophil dysfunction: Despite the increased neutrophil count in sepsis, antimicrobial functions, such as antibacterial activity and delayed apoptosis, are often suppressed, leading to decreased pathogen clearance and an increased risk of secondary infections. The increase in neutrophils in PIV may reflect this dysfunction and thereby exacerbate AKI35. (3) Platelet function: Platelet activation and aggregation in sepsis can lead to microvascular thrombosis, resulting in tissue ischaemia and organ damage. Elevated platelet counts in PIV may indicate their role in inappropriate immune responses, thereby increasing the risk of organ failure and death36. (4) Lymphocyte apoptosis and immune suppression: Increased lymphocyte apoptosis, particularly of T cells, in sepsis leads to immune suppression, impairing the ability to respond effectively to secondary infections and aggravating kidney injury. The changes in lymphocytes in PIV may reflect the degree of immune suppression, influencing the occurrence and mortality risk of SA-AKI37. (5) Microvascular injury and organ failure: Sepsis-induced microvascular injury and increased permeability result in oedema, haemodynamic instability, and inadequate organ perfusion. The cells in PIV, particularly neutrophils and platelets, may be involved in this microvascular injury, and as the kidneys are highly perfused organs, they are particularly susceptible to microvascular dysfunction, thereby exacerbating SA-AKI and increasing mortality risk38.
Although our study suggests that ln (PIV) is an important predictor of 28-day mortality in SA-AKI patients, there are several limitations. First, the retrospective design limits the establishment of causal relationships. Although we performed multivariable adjustments and subgroup analyses, potential confounding factors may still influence the results. Moreover, this study collected data only within the first 24 h of admission, including blood cell counts (lymphocytes, neutrophils, platelets, and monocytes). Missing PIV data may impact the accuracy of the results. We assessed only the baseline ln (PIV) and did not consider the impact of its dynamic changes on patient outcomes. Finally, this study was conducted at a single centre, and future multicentre studies are needed to further validate the utility of ln (PIV) as a prognostic biomarker, particularly its application in high-risk populations and its underlying mechanisms, providing more targeted guidance for clinical treatment decisions.
Conclusion
In conclusion, this cohort study revealed that a higher ln (PIV) is closely associated with increased 28-day all-cause mortality in patients with SA-AKI. These findings suggest that ln (PIV) may serve as a potential index for early risk assessment, but further research is needed to validate the results.
Data availability
The data used in this study are third-party data from the MIMIC-IV v2.2 database. These data are publicly available from PhysioNet (https://mimic.physionet.org/) upon registration and completion of the required training in human subjects research, specifically the CITI program. The authors confirm that they did not have any special access privileges to these data that others would not have.
References
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA-J. Am. Med. Assoc. 315, 801 (2016).
Rhee, C. et al. Incidence and trends of sepsis in us hospitals using clinical vs claims data, 2009–2014. JAMA-J. Am. Med. Assoc. 318, 1241 (2017).
Evans, L. et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intens. Care Med. 47, 1181 (2021).
Hoste, E. A. et al. Epidemiology of acute kidney injury in critically ill patients: The multinational AKI-EPI study. Intens. Care Med. 41, 1411 (2015).
Bagshaw, S. M., George, C. & Bellomo, R. Early acute kidney injury and sepsis: A multicentre evaluation. Crit. Care 12, R47 (2008).
Uchino, S. et al. Acute renal failure in critically ill patients: A multinational, multicenter study. Jama-J. Am. Med. Assoc. 294, 813 (2005).
Wiersema, R. et al. Two subphenotypes of septic acute kidney injury are associated with different 90-day mortality and renal recovery. Crit. Care 24, 150 (2020).
Schuler, A. et al. The impact of acute organ dysfunction on long-term survival in sepsis. Crit. Care Med. 46, 843 (2018).
Xu, H. B. et al. Association between admission pan-immune-inflammation value and short-term mortality in septic patients: a retrospective cohort study. Sci. Rep.-Uk 14, 15205 (2024).
Yang, X. C. et al. Prognostic value of pan-immune-inflammation value in colorectal cancer patients: A systematic review and meta-analysis. Front. Oncol. 12, 1036890 (2022).
Wu, B. et al. The relationship between the pan-immune-inflammation value and long-term prognoses in patients with hypertension: National health and nutrition examination study, 1999–2018. Front. Cardiovasc. Med. 10, 1099427 (2023).
Fucà, G. et al. The Pan-Immune-Inflammation Value is a new prognostic biomarker in metastatic colorectal cancer: results from a pooled-analysis of the Valentino and TRIBE first-line trials. Br. J. Cancer 123, 403 (2020).
Guven, D. C. et al. The association between the pan-immune-inflammation value and cancer prognosis: A systematic review and meta-analysis. Cancers 14, 2675 (2022).
Lee, L. E. et al. Pan-immune-inflammation value at diagnosis independently predicts all-cause mortality in patients with antineutrophil cytoplasmic antibody-associated vasculitis. Clin. Exp. Rheumatol. 39(Suppl 129), 88 (2021).
Corti, F. et al. The Pan-Immune-Inflammation Value in microsatellite instability-high metastatic colorectal cancer patients treated with immune checkpoint inhibitors. Eur. J. Cancer 150, 155 (2021).
Ligorio, F. et al. The pan-immune-inflammation-value predicts the survival of patients with human epidermal growth factor receptor 2 (HER2)-positive advanced breast cancer treated with first-line Taxane-Trastuzumab-Pertuzumab. Cancers 13, 1964 (2021).
Johnson, A. et al. MIMIC-IV, a freely accessible electronic health record dataset. Sci. Data 10, 1 (2023).
Goldberger, A. L. et al. PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals. Circulation 101, E215 (2000).
Kellum, J. A. & Lameire, N. Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Crit. Care 17, 204 (2013).
Xu, H. et al. L-shaped association between triglyceride-glucose body mass index and short-term mortality in ICU patients with sepsis-associated acute kidney injury. Front. Med.-Lausanne 11, 1500995 (2024).
Zarbock, A. et al. Sepsis-associated acute kidney injury: consensus report of the 28th acute disease quality initiative workgroup. Nat. Rev. Nephrol. 19, 401 (2023).
Degenhardt, F., Seifert, S. & Szymczak, S. Evaluation of variable selection methods for random forests and omics data sets. Brief. Bioinform. 20, 492 (2019).
Xu, H., Liu, Y., Niu, H., Wang, H. & Zhan, F. Impact of body mass index on mortality outcomes in intensive care patients with Staphylococcus aureus sepsis: A retrospective analysis. PLoS ONE 19, e308471 (2024).
Guven, D. C. et al. The association between pan-immune-inflammation value and survival in head and neck squamous cell carcinoma. Eur. Arch. Otorhinol. 280, 2471 (2023).
Murat, B., Murat, S., Ozgeyik, M. & Bilgin, M. Comparison of pan-immune-inflammation value with other inflammation markers of long-term survival after ST-segment elevation myocardial infarction. Eur. J. Clin. Invest. 53, e13872 (2023).
Kuperminc, E., Heming, N., Carlos, M. & Annane, D. Corticosteroids in ARDS. J. Clin Med 12, 3340 (2023).
Agnello, L. et al. The value of a complete blood count (CBC) for sepsis diagnosis and prognosis. Diagnostics 11, 1881 (2021).
Farkas, J. D. The complete blood count to diagnose septic shock. J. Thorac. Dis. 12, S16 (2020).
Chen, J. & Wei, H. Immune Intervention in Sepsis. Front. Pharmacol. 12, 718089 (2021).
Zhang, F. et al. Pan-immune-inflammation value is associated with poor prognosis in patients undergoing peritoneal dialysis. Ren. Fail. 45, 2158103 (2023).
Girndt, M., Trojanowicz, B. & Ulrich, C. Monocytes in uremia. Toxins 12, 340 (2020).
Dewitte, A. et al. Blood platelets and sepsis pathophysiology: A new therapeutic prospect in critically [corrected] ill patients?. Ann. Intens. Care 7, 115 (2017).
Grailer, J. J., Fattahi, F., Dick, R. S., Zetoune, F. S. & Ward, P. A. Cutting edge: Critical role for C5aRs in the development of septic lymphopenia in mice. J. Immunol. 194, 868 (2015).
Zahorec, R. Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl. Med. J. 102, 5 (2001).
Islam, M. M. et al. Immunoadjuvant therapy in the regulation of cell death in sepsis: Recent advances and future directions. Front. Immunol. 15, 1493214 (2024).
Leung, G. & Middleton, E. A. The role of platelets and megakaryocytes in sepsis and ARDS. J. Physiol.-Lond. 602, 6047 (2024).
Wang, Z., Zhang, W., Chen, L., Lu, X. & Tu, Y. Lymphopenia in sepsis: a narrative review. Crit. Care 28, 315 (2024).
Vincent, J. L. & De Backer, D. Microvascular dysfunction as a cause of organ dysfunction in severe sepsis. Crit. Care 9(Suppl 4), S9 (2005).
Acknowledgements
We thank the MIMIC-IV database for providing the original study data.
Funding
This work was supported by the Hainan Provincial Natural Science Foundation of China. Project 823RC560. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization, Methodology, Formal Analysis H.P.X., X.Y.C. and Y.H.O.; Visualization, Investigation, H.N. and X.W.C.; Writing—Original Draft, H.P.X., X.Y.C. and Y.H.O.; Writing—Review & Editing, P.H. and H.N.; Funding acquisition H.P.X.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
The submitted manuscript has been read and approved by all the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, H., Cai, X., Niu, H. et al. Association of PIV value with early mortality in ICU patients with sepsis-associated acute kidney injury from the MIMIC IV database. Sci Rep 15, 11212 (2025). https://doi.org/10.1038/s41598-025-96320-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96320-z