Abstract
Obstructive sleep apnea (OSA) is characterized by pharyngeal collapse, hypoxia, and hypercapnia. However, the impact of coronary heart disease (CHD) severity on OSA development has been rarely explored. This study aimed to evaluate the correlation between CHD severity and OSA incidence. This retrospective cohort study was conducted using the National Health Insurance Research Database (NHIRD). Patients with CHD were categorized into three groups: those with severe CHD who underwent percutaneous coronary intervention (PCI), those with CHD without PCI, and those receiving medical treatment. The primary outcome was the development of OSA at least six months after CHD onset. Cox proportional hazards regression was used to calculate the adjusted hazard ratio (aHR) and 95% confidence interval (CI) for OSA across the different CHD groups. A total of 5,193 and 8,313 OSA events were recorded in the CHD-PCI and CHD groups, respectively. After adjusting for multiple confounders, the incidence of OSA was significantly higher in the CHD-PCI group than in the CHD group (aHR: 1.267, 95% CI: 1.220–1.315, P = 0.0135). Subgroup analyses showed that the association between severe CHD with PCI and OSA was more pronounced in older CHD patients (P < 0.05). The cumulative incidence of both OSA and severe OSA was significantly higher in the CHD-PCI group than in the CHD group (both P < 0.001). Severe CHD requiring PCI is associated with a higher incidence of subsequent OSA compared to mild CHD. This association is particularly significant in patients older than 70 years.
Similar content being viewed by others
Introduction
Coronary heart disease (CHD) is characterized by coronary artery stenosis and the resulting ischemic condition of the myocardium, which is increasingly prevalent in developing countries1,2. CHD affects both sexes and carries a significant mortality rate, with women experiencing worse outcomes than their male counterparts3. The chronic form of CHD can be managed with medical treatments, including antiplatelet and lipid-lowering medications4,5. In more advanced cases, such as multivessel disease or chronic total occlusions, percutaneous coronary intervention (PCI) is performed to restore vascular perfusion6,7.
Previous studies have shown that CHD affects multiple organ systems beyond the heart and coronary arteries8,9. CHD is associated with metabolic syndrome due to chronic inflammation and insulin resistance10. Additionally, acute coronary syndrome has been observed in 8% of patients with Behçet’s disease11. CHD has also been linked to changes in choroidal vascularity in the eye12, and patients with advanced periodontitis have a higher risk of developing CHD, likely due to systemic inflammatory responses13.
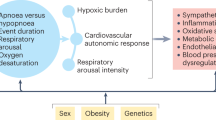
Obstructive sleep apnea (OSA) is characterized by pharyngeal collapse, hypoxia, and hypercapnia14. Known risk factors for OSA include age, male sex, and obesity14. The relationship between OSA and CHD has been investigated, with studies suggesting a positive correlation between the two conditions15,16. However, while prior research has examined the association between CHD and OSA development, the impact of CHD severity on OSA remains largely unexplored. Given the shared pathophysiological mechanisms between CHD and OSA17, it is plausible that higher CHD severity may be associated with more frequent OSA episodes.
This study aimed to evaluate the correlation between CHD severity—based on PCI status—and the subsequent development of OSA and severe OSA using data from the National Health Insurance Research Database (NHIRD) in Taiwan. Several known risk factors for OSA were included in the multivariate analysis.
Materials and methods
Data source
This study adhered to the Declaration of Helsinki (1964) and its subsequent amendments. Ethical approval was obtained from both the National Health Insurance Administration of Taiwan and the Institutional Review Board of Chung Shan Medical University Hospital (project code: CS2-23044). The requirement for written informed consent was waived by both organizations. The National Health Insurance Research Database (NHIRD) contains comprehensive insurance records from Taiwan’s National Health Insurance system, covering over 23 million individuals from January 1, 2000, to December 31, 2020. The NHIRD dataset includes International Classification of Diseases Ninth Revision (ICD-9) and Tenth Revision (ICD-10) diagnostic codes, as well as patient demographics (age, sex, education level, and residential area), imaging and laboratory examination records, medical department classifications, procedure and surgical codes, and Anatomical Therapeutic Chemical (ATC) classification system codes for medications.
Patient selection
This was a retrospective cohort study. Participants were defined as having CHD once they met the following criteria: (1) receipt of CHD diagnoses according to the ICD-9 and ICD-10 codes from 2014 to 2019; (2) the arrangement of complete blood cell count, white blood cell differentiation count, cholesterol, triglyceride, high-density lipoprotein, low-density lipoprotein, and electrocardiogram exams before the CHD diagnosis; and (3) the patients had visited the internal medicine, family medicine, or cardiovascular departments for at least two months. The index date of this study was defined as the date of 6 months after CHD diagnosis. In addition, the following exclusion criteria were adopted: (1) missing demographics; (2) death before the index date; (3) age less than 20 years old or more than 100 years old; (4) CHD diagnosis found in less than two outpatient department visits; (5) index date earlier than 2015 or later than 2019; and (6) OSA developed before the index date. To compare CHD severity, patients were categorized into two groups: those who received only medical treatment and those who underwent PCI. PCI was used as an indicator of severe CHD, as it is typically performed in patients with multivessel disease, as noted in previous literature18. However, the ACS-related and elective PCIs cannot be separated in the NHIRD which could interfere our analysis. Each CHD patient with PCI was matched to two CHD patients receiving medical treatment. PSM was performed using the PROC PSMATCH procedure in SAS software, with the propensity score estimated through logistic regression. The following baseline covariates were included: year of CHD diagnosis, index year, age, sex, economic status, hypertension, diabetes mellitus, hyperlipidemia, cerebrovascular disease, and peripheral vascular disease. A 1:2 nearest neighbor greedy matching approach with a caliper width of 0.01 was applied to ensure comparability between groups. A caliper of 0.01 was chosen as it effectively minimized covariate imbalances without excessively reducing the matched sample size. Balance between matched groups was assessed using the absolute standardized mean difference (ASD), with a threshold of < 0.1 considered indicative of a well-balanced distribution. Following matching, 296,544 individuals were assigned to the CHD-PCI group and 593,088 to the CHD group. The patient selection process is illustrated in Fig. 1.
Primary outcome
The primary outcome was an OSA episode, according to the following criteria: (1) receipt of OSA-related ICD-9 and ICD-10 diagnostic codes, (2) arrangement of polysomnography before the date of OSA diagnosis according to the related procedure codes, and (3) OSA diagnosis made by a chest physician, neurologist, or otolaryngologist. Severe OSA was defined as OSA based on the above criteria and OSA-related nasal, pharyngeal, and laryngeal surgeries. In addition, only OSA events that appeared after the index date were considered the outcome achievement. The patients in this research were followed until the occurrence of an OSA episode, and were withdrawn from the Taiwan National Health Insurance program or the deadline of the NHIRD, which indicates December 31, 2020.
Demographic and systemic confounders
To minimize confounding effects on OSA development, multivariable analyses were adjusted for the following demographic and clinical factors: age, sex, economic status, hypertension, diabetes mellitus, hyperlipidemia, cerebrovascular disease, peripheral vascular disease, and medication use (systemic corticosteroids, aspirin, clopidogrel, direct-acting oral anticoagulants, statins, and warfarin). The presence of these conditions and medications was determined using insurance codes from the NHIRD. To ensure adequate exposure duration for confounders to influence OSA development, only systemic diseases or medications that persisted for at least two years before the index date were included in the analysis.
Statistical analysis
All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). Descriptive statistics were used to compare demographic characteristics, systemic diseases, and medication prescriptions between groups. The ASD was used to assess variable distributions, with values > 0.1 considered indicative of significant differences. Cox proportional hazard regression was conducted to estimate adjusted hazard ratios (aHR) and 95% confidence intervals (CI) for OSA and severe OSA between the two groups. The model accounted for demographic factors, systemic diseases, and medication use. The proportional hazards assumption was verified for the comparison of OSA risk between the CHD and CHD-PCI groups. Kaplan–Meier survival curves were generated to illustrate the cumulative incidence of OSA and severe OSA, and the log-rank test was used to compare differences between the CHD and CHD-PCI groups. For subgroup analyses, CHD patients were stratified by age and sex, and Cox proportional hazard regression was performed again to assess the incidence of OSA and severe OSA within different subgroups. Additionally, an interaction test was conducted to examine variations in aHR and 95% CI across CHD subgroups. Statistical significance was set at P < 0.05, while P < 0.0001 was reported as P < 0.0001 in this study.
Results
The baseline characteristics of the CHD-PCI and CHD groups are summarized in Table 1. A total of 118,412 patients (39.93%) in the CHD-PCI group and 235,387 patients (39.69%) in the CHD group were aged > 70 years, with no significant differences in age distribution between groups (ASD = 0.0015). The number of male patients was identical in both groups: 192,915 (65.05%) in the CHD-PCI group and 385,830 (65.05%) in the CHD group (ASD = 0.0000). Similarly, no significant differences were observed in economic status, systemic diseases, or medication use between groups following the PSM process (all ASD < 0.1) (Table 1).
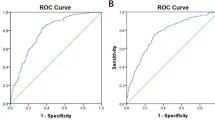
After the follow-up period, 5,193 and 8,313 OSA events were recorded in the CHD-PCI and CHD groups, respectively (Table 2). The incidence of OSA was significantly higher in the CHD-PCI group than in the CHD group, even after adjusting for all potential confounders (aHR: 1.267, 95% CI: 1.220–1.315, P = 0.0135) (Table 2). Regarding severe OSA, 373 and 618 severe OSA events were documented in the CHD-PCI and CHD groups, respectively (Table 2). Multivariate analysis confirmed a significantly higher incidence of severe OSA in the CHD-PCI group compared to the CHD group (aHR: 1.215, 95% CI: 1.058–1.396, P = 0.0211) (Table 2). The cumulative incidence of OSA and severe OSA for both groups is illustrated in Figs. 2 and 3, respectively. The Kaplan–Meier curves demonstrate significantly higher cumulative incidences of both OSA and severe OSA in the CHD-PCI group compared to the CHD group (both P < 0.001).
In subgroup analyses, CHD patients who underwent PCI exhibited a significantly higher incidence of both OSA and severe OSA across nearly all age subgroups (P < 0.05). Furthermore, the association between severe CHD with PCI and both OSA and severe OSA was more pronounced in older CHD patients than in younger patients with severe CHD (P = 0.0035 and 0.0327, respectively) (Table 3).
Discussion
This study demonstrated that severe CHD requiring PCI is associated with a higher incidence of OSA compared to CHD patients who did not undergo PCI. Notably, this association was more pronounced in individuals aged > 70 years, and the correlation strengthened over time.
Epidemiologically, CHD is a prevalent condition worldwide, with an annual incidence of 1.7%1. In certain populations, such as Finnish males, the incidence of CHD can reach 37% over a 20-year follow-up, with a CHD-related mortality rate of approximately 15%19. Similarly, OSA is highly prevalent, affecting approximately 4% of males in the U.S. and 7.5% in India20. OSA is also associated with reduced quality of life and emotional distress21. Given that both CHD and OSA significantly impact public health, understanding their interplay is crucial14,22.
The pathophysiological mechanisms underlying CHD and OSA share several common pathways, beyond their associations with dyslipidemia and hypertension17,23,24,25. CHD is characterized by elevated inflammatory cytokines, including C-reactive protein (CRP), interleukins, and tumor necrosis factor-alpha (TNF-α), which are involved in all stages of atherosclerosis progression9,26,27. Notably, inflammation plays a key role in OSA as well, as patients with severe OSA exhibit higher levels of interleukins and CRP compared to those with mild OSA25,28. Additionally, hypoxia and oxidative stress, common features in CHD, also contribute to OSA pathophysiology, leading to vascular damage and increased production of reactive oxygen species (ROS)25,29,30. Given these shared mechanisms, it is plausible that CHD not only increases the risk of OSA but that higher CHD severity further amplifies this risk. Our findings support this hypothesis in an Asian population, emphasizing the need for further investigation.
Previous studies have highlighted the bidirectional relationship between CHD and OSA, where OSA increases the risk of CHD, and vice versa. However, few studies have examined whether CHD severity influences OSA incidence. Our study provides preliminary evidence supporting this link, demonstrating that CHD severity may be an independent risk factor for subsequent OSA development, even after adjusting for known OSA risk factors such as age, sex, hypertension, and metabolic diseases14. Consequently, CHD severity may be an independent risk factor for subsequent OSA development. The severity of OSA can alter the development of CHD-related morbidity, in which moderate-to-severe OSA is an independent predisposing factor for major adverse cardiovascular events31. Patients who received continuous positive airway pressure treatment showed a lower risk of cardiovascular events32. Compared to the OSA-to-CHD association in a previous study, our study further demonstrated that CHD severity can also affect the risk of OSA. Although PCI itself may contribute to some respiratory stress33, the effect was rather short-term in previous publications, and we may only regard PCI as a severity index in the current study. The cumulative incidence analyses further demonstrated the significant higher risk of developing OSA in the CHD patients with PCI management than the CHD patients without PCI management.
In subgroup analyses, the relationship between CHD severity and OSA was most pronounced in patients aged ≥ 70 years. This finding remained significant after adjusting for systemic diseases and medical factors, suggesting that older adults may be particularly vulnerable to the OSA-inducing effects of severe CHD. Age is a well-established risk factor for OSA, and males are more susceptible to OSA-related complications than females16,20. However, women may also experience similar OSA symptoms, including snoring and daytime hypersomnolence, but are often underdiagnosed34. Some studies have reported a higher prevalence of OSA in women (50%) compared to men (37%)35, further emphasizing the importance of screening in at-risk populations. Accordingly, we believe that the higher risk of OSA development in females with severe CHD observed in this study, which contradicts previous findings20, may be due to the historical underestimation of OSA in females. In fact, only 40% of females at high risk for OSA have been diagnosed with the condition36. Another possible explanation is that females generally tend to seek medical assistance more frequently than males, regardless of disease type37. As a result, they may be more likely to consult a physician for OSA-related symptoms. Given these findings, our results suggest that older CHD patients, particularly those with severe disease, should be routinely evaluated for OSA.
The current study has several limitations. First, as it relies on claims data rather than actual medical records, certain important clinical details—such as laboratory results for CHD, cardiac imaging findings, PCI procedure details, therapeutic outcomes of PCI, recurrence of coronary artery stenosis after PCI, exact CHD diagnosis timing, and sociodemographic variables including body mass index, smoking status, and alcohol consumption—are unavailable. Additionally, key OSA-related data, including polysomnography results, apnea-hypopnea index values, self-paid surgical procedures or devices used for OSA treatment, treatment outcomes, and recurrence of OSA, cannot be accessed. To define severe OSA, we used the presence of nasal, pharyngeal, and laryngeal surgeries related to OSA, as polysomnography data and apnea-hypopnea index values are not available in the Taiwan NHIRD. However, this approach may limit the accuracy of severe OSA classification, as not all patients with severe OSA undergo surgery; some may opt for self-paid continuous positive airway pressure (CPAP) therapy instead. The absence of self-paid OSA treatments, including CPAP and weight-loss surgery, from the NHIRD dataset further limits our ability to comprehensively assess treatment outcomes. Additionally, CHD patients undergoing PCI may have more frequent healthcare visits, increasing the likelihood of OSA detection and potentially introducing detection bias. Another limitation is the exclusion of obesity from our multivariate analysis, despite its well-established role as a risk factor for both CHD and OSA. In clinical practice, ICD-9 and ICD-10 codes for obesity are infrequently recorded by physicians, making it difficult to include this variable, which may have led to residual confounding. As mentioned in the Methods section, ACS-related and elective PCIs cannot be distinguished because cardiac imaging and medical records are not available in the NHIRD system. Additionally, the precision of CHD severity assessment in this study may be limited, which could affect the overall integrity of our results. Finally, as nearly all participants in this study were Han Taiwanese, the findings may not be generalizable to other ethnic populations, limiting the study’s external validity.
In conclusion, severe CHD requiring PCI is associated with a higher risk of subsequent OSA, independent of other known risk factors. This association is stronger in patients aged ≥ 70 years and increases over time. Given these findings, CHD patients, particularly those with severe disease, should be screened for OSA to prevent long-term complications. Future large-scale, prospective studies are warranted to further explore the impact of CHD severity on OSA treatment outcomes and the potential bidirectional relationship between these two conditions.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Xie, Q., Huang, J., Zhu, K. & Chen, Q. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with coronary heart disease and type 2 diabetes mellitus: cumulative meta-analysis. Clin. Cardiol. 44, 899–906 (2021).
Zhu, K. F., Wang, Y. M., Zhu, J. Z., Zhou, Q. Y. & Wang, N. F. National prevalence of coronary heart disease and its relationship with human development index: A systematic review. Eur. J. Prev. Cardiol. 23, 530–543 (2016).
Khamis, R. Y., Ammari, T. & Mikhail, G. W. Gender differences in coronary heart disease. Heart 102, 1142–1149 (2016).
Al-Lamee, R. K., Nowbar, A. N. & Francis, D. P. Percutaneous coronary intervention for stable coronary artery disease. Heart 105, 11–19 (2019).
Almeida, S. O. & Budoff, M. Effect of Statins on atherosclerotic plaque. Trends Cardiovasc. Med. 29, 451–455 (2019).
Hoole, S. P. & Bambrough, P. Recent advances in percutaneous coronary intervention. Heart 106, 1380–1386 (2020).
Banning, A. P. et al. Percutaneous coronary intervention in the UK: recommendations for good practice 2015. Heart 101 (Suppl 3), 1–13 (2015).
Wang, S. B. et al. A spectrum of retinal vasculature measures and coronary artery disease. Atherosclerosis 268, 215–224 (2018).
Wirtz, P. H. & von Känel, R. Psychological stress, inflammation, and coronary heart disease. Curr. Cardiol. Rep. 19, 111 (2017).
Rana, J. S., Nieuwdorp, M., Jukema, J. W. & Kastelein, J. J. Cardiovascular metabolic syndrome - an interplay of, obesity, inflammation, diabetes and coronary heart disease. Diabetes Obes. Metab. 9, 218–232 (2007).
Vural, U., Kizilay, M. & Aglar, A. A. Coronary involvement in Behçet’s disease: what are its risks and prognosis?? (Rare cases and literature Review). Braz J. Cardiovasc. Surg. 34, 749–758 (2019).
Seo, W. W., Yoo, H. S., Kim, Y. D., Park, S. P. & Kim, Y. K. Choroidal vascularity index of patients with coronary artery disease. Sci. Rep. 12, 3036 (2022).
Priyamvara, A. et al. Periodontal inflammation and the risk of cardiovascular disease. Curr. Atheroscler Rep. 22, 28 (2020).
Jordan, A. S., McSharry, D. G. & Malhotra, A. Adult obstructive sleep Apnoea. Lancet 383, 736–747 (2014).
Yeghiazarians, Y. et al. Obstructive sleep apnea and cardiovascular disease: A scientific statement from the American heart association. Circulation 144, e56–e67 (2021).
Mehra, R. Sleep apnea and the heart. Cleve Clin. J. Med. 86, 10–18 (2019).
Gonzaga, C., Bertolami, A., Bertolami, M., Amodeo, C. & Calhoun, D. Obstructive sleep apnea, hypertension and cardiovascular diseases. J. Hum. Hypertens. 29, 705–712 (2015).
Faro, D. C. et al. Complete percutaneous coronary revascularization in acute coronary syndromes with multivessel coronary disease: A systematic review. JACC Cardiovasc. Interv. 16, 2347–2364 (2023).
Voutilainen, A., Brester, C., Kolehmainen, M. & Tuomainen, T. P. Epidemiological analysis of coronary heart disease and its main risk factors: are their associations multiplicative, additive, or interactive? Ann. Med. 54, 1500–1510 (2022).
Punjabi, N. M. The epidemiology of adult obstructive sleep apnea. Proc. Am. Thorac. Soc. 5, 136–143 (2008).
Batool-Anwar, S. et al. Impact of continuous positive airway pressure (CPAP) on quality of life in patients with obstructive sleep apnea (OSA). J. Sleep. Res. 25, 731–738 (2016).
Dalen, J. E., Alpert, J. S., Goldberg, R. J. & Weinstein, R. S. The epidemic of the 20(th) century: coronary heart disease. Am. J. Med. 127, 807–812 (2014).
Shaya, G. E., Leucker, T. M., Jones, S. R., Martin, S. S. & Toth, P. P. Coronary heart disease risk: Low-density lipoprotein and beyond. Trends Cardiovasc. Med. 32, 181–194 (2022).
Harrington, R. A. Targeting inflammation in coronary artery disease. N Engl. J. Med. 377, 1197–1198 (2017).
Arnaud, C., Bochaton, T., Pépin, J. L. & Belaidi, E. Obstructive sleep Apnoea and cardiovascular consequences: pathophysiological mechanisms. Arch. Cardiovasc. Dis. 113, 350–358 (2020).
Li, H. et al. Inflammatory biomarkers of coronary heart disease. Front. Biosci. (Schol Ed). 10, 185–196 (2018).
Liu, Y. et al. Systemic immune-inflammation index predicts the severity of coronary stenosis in patients with coronary heart disease. Coron. Artery Dis. 32, 715–720 (2021).
Popadic, V. et al. Correlation of dyslipidemia and inflammation with obstructive sleep apnea severity. Front. Pharmacol. 13, 897279 (2022).
Sarwar, N., Thompson, A. J. & Di Angelantonio, E. Markers of inflammation and risk of coronary heart disease. Dis. Markers. 26, 217–225 (2009).
Vitulano, N. et al. Obstructive sleep apnea and heart disease: the biomarkers point of view. Front. Biosci. (Schol Ed). 5, 588–599 (2013).
Jia, S. et al. Obstructive sleep apnea is associated with severity and long-term prognosis of acute coronary syndrome. J. Geriatr. Cardiol. 15, 146–152 (2018).
McEvoy, R. D. et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl. J. Med. 375, 919–931 (2016).
Su, H. M. et al. Acute respiratory distress syndrome after early successful primary percutaneous coronary intervention therapy in acute myocardial infarction: a case report. Kaohsiung J. Med. Sci. 21, 78–83 (2005).
Quintana-Gallego, E. et al. Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients. Respir Med. 98, 984–989 (2004).
Franklin, K. A. & Lindberg, E. Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J. Thorac. Dis. 7, 1311–1322 (2015).
Kapsimalis, F. & Kryger, M. Sleep breathing disorders in the U.S. Female population. J. Womens Health (Larchmt). 18, 1211–1219 (2009).
Wang, Y., Hunt, K., Nazareth, I., Freemantle, N. & Petersen, I. Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open. 3, e003320 (2013).
Funding
This research was funded by Chung Shan Medical University Hospital, Taiwan, grant number CSH-2023-C-038.
Author information
Authors and Affiliations
Contributions
KHT, YTL, CHH, and SFY designed and conceptualized the study. CWL, JYH and SFY are responsible for the statistical analyses. KHT, YTL, CYL, JYH, CHH, and SFY are responsible for the manuscript draft. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by both the National Health Insurance Administration of Taiwan and Institutional Review Board of Chung Shan Medical University Hospital (Project code: CS2-23044).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ting, KH., Lu, YT., Lin, CW. et al. The severity of coronary heart disease and the incidence and severity of following obstructive sleep apnea: a population-based cohort study. Sci Rep 15, 12539 (2025). https://doi.org/10.1038/s41598-025-97516-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-97516-z