Abstract
Patients with middle and lower thoracic esophageal carcinoma (TEC) after surgery are prone to develop abdominal lymph node recurrence (LNR). However, questions remain regarding the indications for postoperative abdominal radiotherapy. We aimed to identify the risk factors for abdominal LNR and to develop a dynamic nomogram for predicting abdominal LNR. We reviewed 1004 patients with middle and lower TEC treated with three-field lymph node dissection between January 2010 and December 2020 at two clinical centers. Risk factors for abdominal LNR were identified using least absolute shrinkage and selection operator (LASSO) logistic regression analysis. A dynamic nomogram was then developed. Performance was evaluated using receiver operating characteristic (ROC) curve , calibration curve and decision curve analysis. The rates of abdominal LNR in the training, internal test and external test cohorts were 25.91%, 23.40% and 23.98%, respectively. A dynamic nomogram was developed to predict the abdominal LNR in patients with middle and lower TEC. The main predictors included tumor ___location, pathologic N stage and number of preoperative abdominal LNM. The AUC of the training, internal test, and external test cohorts were 0.767 (95%CI 0.7263–0.8079), 0.763 (95%CI 0.7002–0.8258) and 0.802 (95%CI 0.7419–0.8629), respectively. Furthermore, The calibration curves and DCA analysis indicated a favorable fit and significant clinical applicability of the nomogram. The dynamic nomograms is available at https://prediction-of-abdiminal-lymph-node-metastasis-in-tec.shinyapps.io/DynNomapp/. Tumor ___location, pathologic N stage and number of preoperative abdominal LNM were identified as risk factors for predicting abdominal LNR. The online dynamic nomograms showed good prediction performance and convenient clinical application, which may help clinicians identify patients who require adjuvant abdominal radiotherapy.
Similar content being viewed by others
Introduction
Esophageal carcinoma is a highly aggressive and lethal neoplasm within the gastrointestinal tract,1 with high rates of lymph node involvement. Despite recent advances in three-field lymph node dissection (3-LND),2,3 there has been no significant improvement in survival. The lymph node recurrence (LNR) has been proven to be the most prevalent recurrence pattern.4 Adjuvant radiotherapy has been shown to prevent LNR and improve survival in patients undergoing lymphadenectomy for thoracic esophageal carcinoma (TEC).5,6 However, questions remain on indications for postoperative abdominal radiotherapy. Postoperative abdominal radiotherapy is a complex issue that involved the individualized prediction of abdominal LNR and radiation-related complications.
The rates of abdominal LNR vary significantly among different TEC segments. In upper TECs, the recurrence rates of abdominal lymph nodes were only 0–2.3% in previous studies.7,8 However, abdominal LNRs were observed more frequently in the middle and lower TECs. The recurrence rates in the middle and lower TEC were 7.8%–19.9% and 26.6%–40.8%, respectively.7,8,9,10,11 The abdominal lymph node metastasis was rare in upper TEC, more common in lower TEC, and varied greatly in middle TEC. Given the discernible differences in abdominal LNR among different segments of esophageal carcinoma and the gastrointestinal reactions frequently caused by abdominal radiotherapy, it is necessary and urgent to establish a predictive model of abdominal LNR in patients with middle and lower TEC to offer reference for postoperative radiotherapy.
Nomograms function as powerful tools to facilitate the integration of various parameters and generation of individualized prediction. Some studies12,13,14,15,16 have suggested that nomograms can provide beneficial and accurate prediction of local recurrence, distant metastasis and survival outcomes in esophageal carcinoma. In this study, logistic regression analysis was employed to identify significant predictive factors for abdominal LNR in patients with middle and lower TEC who underwent 3-LND. A nomogram was developed to provide a practical tool for predicting abdominal LNR. By utilizing the nomogram, clinicians can tailor adjuvant treatment strategies, such as postoperative radiotherapy, and surveillance protocols to optimize outcomes.
Materials and methods
Patients
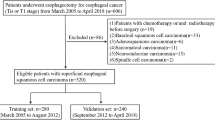
The clinical data of patients with middle and lower thoracic esophageal squamous cell carcinoma (ESCC) treated with complete 3-LND between January 2010 and December 2020 at two clinical centers were included in this retrospective study. This research was approved by the Ethics Committee of the First Hospital of Quanzhou Affiliated to Fujian Medical University, Quanzhou, China. All methods were performed in accordance with the relevant guidelines and regulations. All participants in this study had provided informed consent prior to enrollment. Figure 1 illustrates the patient recruitment pathway. The inclusion criteria were (1) patients who had undergone 3-LND; (2) more than 15 lymph nodes were dissected; (3) patients were followed up every 3–6 months after surgery. The exclusion criteria were (1) patients who had not undergone 3-LND; (2) patients with other types of cancer; (3) patients with palliative resection; (4) patients with incomplete medical records.
Data collection
The following clinical data were collected: sex, age, tumor ___location, Pathologic T stage, N stage, differentiation, lymphatic invasion, vascular invasion, number of preoperative abdominal LNM, weight loss, preoperative chemotherapy, radiotherapy, postoperative chemotherapy and radiotherapy. The data of abdominal LNR were also collected. The TNM staging of esophageal carcinoma was performed according to the 7th edition of the AJCC-TNM staging manual.
Surgical approach
All patients underwent a complete 3—LND. Firstly, in the chest, the esophagus and mediastinal lymph nodes were removed; subsequently, in the abdomen, the left gastric nodes, greater and lesser curvature nodes, parahiatal nodes, splenic hilar nodes and common hepatic nodes were excised; finally, cervical lymph nodes were excised through an incision in the neck. More than 15 lymph nodes were dissected.
Neoadjuvant and adjuvant therapy
Neoadjuvant and adjuvant therapy was conducted according to the adverse prognosis or risk factors for recurrence. The adjuvant chemotherapy (paclitaxel/5-fluorouracil and cisplatin/nedaplatin for 4 to 6 cycles) and/or radiotherapy (50–54 Gy) was conducted after operation. The neoadjuvant chemotherapy (paclitaxel/5-fluorouracil and cisplatin/nedaplatin) and/or radiotherapy (40 Gy) was conducted before operation. The abdominal cavity was not included in the preoperative and postoperative radiotherapy target volumes.
Follow-up
All patients were followed up every 3–6 months in the first year after 3-LND, and every 6–12 months thereafter. Re-examinations included chest and abdominal enhanced CT scans, abdominal Doppler ultrasound examinations, and PET-CT scans if required.
Diagnostic criteria
The determination of abdominal LNR primarily relied on a comprehensive assessment of clinical symptoms, physical examination findings and imaging results. Imaging diagnostic criterion for abdominal LNR was set as follows: lymph nodes were deemed malignant if the transverse diameter of the nodes was larger than 1 cm or there was progressive enlargement of the suspicious lymph nodes. Moreover, the shape of the lymph nodes and uptake of FDG in PET-CT were also taken into account.
Statistical analysis
We identified the cutoff value of age as 55 years for evaluating abdominal LNR by using receiver operating characteristic (ROC) curve analysis and categorized the number of preoperative abdominal lymph node metastases as 0, 1–2 and ≥ 3, according to previous studies.4,8 Then categorical variables were compared using the χ2 test in univariate analysis. For multivariate analysis, we conducted least absolute shrinkage and selection operator (LASSO) logistic regression analysis to identify risk factors of abdominal LNR and constructed a predictive nomogram. The nomogram’s performance was evaluated using ROC curves, calibration curves and decision curve analysis. An dynamic nomogram application was built using Shiny to facilitate their incorporation into the clinical practice. The nomogram model for time of abdominal lymph node recurrence-free was also developed utilizing LASSO-cox analysis. A P value less than 0.05 was considered statistically significant. All statistical analyses were performed using the R software (version 4.4.1).
Results
Patient characteristics
Overall, 1004 eligible patients with ESCC were enrolled in this study, with a median follow up duration of 42.2 months. The original dataset of center1 was divided into a training cohort (n = 548) and an internal test cohort (n = 235) at a ratio of 7:3. In addition, patients of center2 were enrolled as the external test cohort (n = 221). The detailed characteristics are listed in Table 1. There were no statistically significant differences in all variables among the cohorts.
A total of 250 patients presented with abdominal LNR (24.90%). The incidence of abdominal LNR was 25.91%, 23.40% and 23.98% in the training, internal test and external test cohorts, respectively, (Table 2). Over half of the cases across all cohorts had T3 stage tumors (p = 0.948). 149 patients with T3 (27.9%) developed abdominal LNR. The majority of patients were in the N3 category across all cohorts. In patients with pathology of N0, N1, N2, N3, the rates of abdominal LNR were 1.09%, 5.09%, 23.08%, and 40%, respectively. Preoperative abdominal LNMs were found 32.5%, 34.47% and 28.05% in the training, internal test, and external test cohorts, respectively. The rates of abdominal LNR were 5.06% for those with no positive abdominal lymph nodes, 28.47% for 1 to 2 positive nodes, and 46.1% for three or more positive nodes. The abdominal LNR rates of middle and lower TECs were 17.44% and 47.04%, respectively.
Sex, age, tumor differentiation status, lymphatic invasion, vascular invasion, weight loss, preoperative chemotherapy, postoperative chemotherapy and postoperative radiotherapy did not show significant differences, with p-values of 0.855, 0.669, 0.097, 0.478, 0.370, 0.291, 0.370, 0.235, 0.366 and 0.256 respectively. Notably, the presence of preoperative radiotherapy differed significantly among the cohorts (p < 0.001), with more patients in the external test cohort receiving this treatment. This comprehensive analysis provided insights into the baseline characteristics of the patient cohorts, essential for the predictive research conducted in this study.
Development of the nomogram for the prediction of lymph node recurrence
The clinical characteristics between the abdominal LNR and non-abdominal LNR groups were compared. The results showed sex, Pathologic T stage, number of preoperative abdominal lymph node metastases, pathologic N stage, lymphatic invasion and tumor ___location were significantly related to abdominal LNR, while age, differentiation, vascular invasion and weight loss were not related to abdominal LNR.
The candidate predictors were then refined to three key predictors utilizing LASSO analysis with tenfold cross validation. The resultant coefficients are presented in Table 2. The coefficient profile and cross-validated error plot of the LASSO regression model are displayed in Fig. 2. The most regularized and simplest model (based on lambda.1se) comprised three variables (pathologic N stage, Tumor ___location and number of preoperative abdominal LNM) (Fig. 2). The lambda coefficient was 0.06359. The logistic model was finally developed into a dynamic nomogram (Fig. 3) and was available for online access (https://prediction-of-abdiminal-lymph-node-metastasis-in-tec.shinyapps.io/DynNomapp/). Figure 4 shows operation interface of dynamic nomogram on the web page and provides two examples of the dynamic nomograms for abdominal LNR prediction.
The potential predictors selected by the Least Absolute Shrinkage and Selection Operator (LASSO) regression analysis model. (a) Regression coefficient path diagram (1. Pathologic N stage; 2. Tumor ___location; 3. number of preoperative abdominal LNM); (b) Cross verification curve (λ = 0.06359). LNM: abdominal lymph node metastases.
Operation interface of dynamic nomogram on the web page and two examples predicting for abdominal LNR. (a) The risk of abdominal LNR was at 1.88% for a patient with middle TEC, N0 stage, and with 0 positive abdominal lymph nodes. (b) A patient diagnosed with lower TEC, N1 stage, and with 1–2 positive abdominal lymph nodes was at a risk of 17.30%. LNR: lymph node recurrence; TEC: thoracic esophageal carcinoma; LNM: lymph node metastases.
Validation of the nomogram model
The prediction model utilizing the training cohort demonstrated good discrimination, as substantiated by ROC curve analysis. The area under the ROC curve (AUC) for the training, internal test, and external test cohorts were 0.767 (95%CI 0.7263–0.8079), 0.763 (95%CI 0.7002–0.8258) and 0.802 (95%CI 0.7419–0.8629), respectively (Fig. 5).
Figure 6 displays the calibration curves and the decision curve analysis (DCA) curves. The model exhibited excellent concordance between predicted and observed probabilities of abdominal lymph node recurrence (LNR), with no statistically significant differences across three cohorts: the training cohort (R2 = 0.261, Brier score: 0.159, P = 0.998), the internal test cohort (R2 = 0.249, Brier score: 0.152, P = 0.772) and the external test cohort (R2 = 0.306, Brier score: 0.145, P = 0.598). Furthermore, this study demonstrated that the nomogram provided significant net benefits for clinical application. The results indicated that when the patient’s risk threshold was within the range of 5% to 50%, utilizing the nomogram to predict abdominal LNR added more benefit.
The nomogram model for time of abdominal lymph node recurrence-free
The nomogram model for 12-month and 18-month of abdominal lymph node recurrence -free were also developed utilizing LASSO-cox analysis with tenfold cross validation. The most regularized and simplest model (based on lambda.1se) comprised two variables (pathologic N stage and number of preoperative abdominal LNM). The lambda coefficient was 0.11279. The cox model was finally developed into a nomogram (Fig. 7).
Discussion
Although the standard treatment regimen for advanced TEC is neoadjuvant therapy followed by surgery, radiotherapy after surgery remains a common treatment modality in China. Previous studies had considered postoperative radiotherapy as an effective treatment to prevent LNR, and had recommended it, especially in patients with LNM.17,18,19,20 However, a consensus on the indications for postoperative abdominal radiotherapy has not yet been reached. In the past, the delineation of postoperative radiation target volume was primarily according to the patterns of lymphatic spread21,22 and recurrence patterns.7,23 Whether to perform postoperative abdominal radiotherapy has differed among centers.
In the previous study,24,25 the abdominal lymphatic drainage area was not included in the traditional large T-shaped and small T-shaped irradiation field. This might lead to miss invisible tumor cells that would migrate to the abdominal lymphatic drainage area. These cells could continue to proliferate and grow, eventually resulting in abdominal recurrence. Some researchers8,11 argued that the abdominal irradiation should be selectively recommended for patients with lower TEC, as these patients have a high probability of abdominal lymph node metastasis. Abdominal irradiation is a double—edged sword; it can not only eliminate invisible tumor cells, but also lead to severe complications, such as gastrointestinal reactions. Therefore, individualized analysis is critically required for performing abdominal radiotherapy. Consequently, there is an urgent demand for tools that can help clinicians predict abdominal LNR accurately, so that the lymph node region can be individualized and selectively irradiated.
LASSO regression is a powerful and widely-used regression technique that performed variable selection and regularization, thereby enhancing the predictive accuracy of the model. One of the main advantages of LASSO regression is its ability to perform automatic variable selection, which can help identify the most relevant predictors and reduce the complexity of the model. This research method has been considered feasible and effective in previous studies.26,27,28,29 In this study, the main predictive factors identified through LASSO regression analysis included tumor ___location, pathologic N stage and number of preoperative abdominal LNM. These factors will be discussed in more detail in the following analysis.
The abdominal LNR rates of TEC vary greatly among different segments. For patients with middle and lower TEC, abdominal lymph node recurrences were observed more frequently.7,8,9,10 Zhang WC et al.9 reported that the abdominal LNR rate was 13.9% in middle TEC patients and 40.8% in lower TEC patients; Gao et al.11 found the rates to be 19.9% and 36.9%, respectively, in middle and lower TEC patients. In the present study, the rates of abdominal LNR in patients with middle and lower TEC were 17.44% and 47.04%, respectively. The rate of abdominal LNR in patients with lower TEC was significantly higher than that with middle TEC, indicating that lower TEC has a higher risk of abdominal LNR. Du et al.23 also showed tumor cells of lower TEC exhibited a propensity for abdominal metastasis. This phenomenon might be ascribed to disparate LNM mechanisms exhibited by TEC from different segments. The closer proximity of the primary tumor to the abdominal lymphatic drainage area increases the probability of tumor cells metastasis through the lymphatic vessels. These findings underscore that tumor ___location served as a significant risk factor for abdominal LNR.
The stage N of TEC, classified by the number of positive lymph nodes, has been implicated in patient’s prognosis and LNR.30,31,32,33 In Gao et al. studies,11 patients with N2 + 3 pathology exhibited an abdominal lymph node recurrence rate of 76.5%. Hiroshi Miyata et al.'s studies34 also identified nodal status as an independent predictor of abdominal LNR. In our study, the abdominal LNR rates for patients with N0, N1, N2, and N3 pathologies were 1.09%, 5.09%, 23.08%, and 40%, respectively. This result indicates that increasing the number of positive lymph nodes might result in raising the risk of abdominal LNR.
The number of abdominal LNM before operation may serve as a critical factor of abdominal LNR.10 In our study, the abdominal LNR rates were found to be 5.06% for patients without positive abdominal lymph nodes, 28.47% for those with 1 to 2 positive nodes, and 46.1% for those with three or more positive nodes. However, Chen et al.8 reported the metastasis rates of positive abdominal lymph nodes were 22.7%, lower than our study’s 37.76%. This difference may result from several factors. First, our study exclusively included middle and lower TEC patients, who generally have higher recurrence rates than upper TEC patients. Second, our study population had a higher proportion of advanced-stage cancers (T3/T4 and N2/N3), which are linked to increased recurrence risk. Third, variations in surgical techniques and adjuvant therapy protocols across studies may also influence recurrence patterns. Hiroshi Miyata et al. studies34 also noted that the rate of abdominal LNR from esophageal carcinoma was not necessarily low. Overall, previous studies8,10 support that abdominal LNR is related to the number of preoperative abdominal LNM. This may be ascribed to the technical challenges in complete excising nodes in the vicinity of the abdominal aorta, truncus coeliacus and common hepatic artery, leading to residual subclinical lesions and abdominal LNR.
The nomogram developed based on the above three factors was finally assessed through the ROC curve, calibration curve and decision curve analysis. The predictive performance of the nomogram was evaluated using AUCs of 0.767, 0.763, and 0.802 for the training cohort, internal test cohort and external test cohort, respectively. The results demonstrated that the original nomogram maintained its utility in the validation sets, and the calibration curve closely adhering to the ideal curve, indicating concordance between predicted and observed results. The decision curve showed that utilizing a 5%–50% threshold for predicting abdominal LNR achieved a positive net benefit. Therefore, the predictive validity of the nomogram was considered to be both testable and provable. Remarkably, the model performed better in the external testing data than in the training data. This could be due to the following reasons: First, the external test cohort might have had a more homogeneous distribution of key predictors and fewer confounding factors, contributing to better performance. Second, the smaller sample size of the external test cohort could have reduced variability, leading to seemingly better performance metrics (e.g., AUC).
To improved the model stability, we also creatively conducted a time-to-event analysis of abdominal lymph node recurrence-free status at 12-and 18-month intervals. The analysis revealed that preoperative lymph node metastasis and N staging serve as independent predictors of abdominal lymph node recurrence-free survival, underscoring the critical need for stringent postoperative surveillance of abdominal lymph node in these high-risk patient cohorts.
The prediction model for abdominal LNR offers several clinical utilities. First, In our previous study,4 we identified that the LNR at the para-aortic (above the left renal vein), celiac artery, posterior surface of the pancreatic head, and common hepatic artery accounted for 77.94%, 44.11%, 27.94%, and 23.52%, respectively. Based on these findings, we proposed that clinicians consider implementing individualized abdominal radiotherapy targeting these specific regions using the predictive model. This approach not only improves local control rates but also reduces treatment-related adverse reactions, such as nausea and vomiting, improving treatment efficacy and quality of life. Second, the prediction model could assist clinicians in prioritizing patients for intensified post-surgical surveillance, particularly those identified as high-risk for abdominal LNR. This could facilitate earlier detection and management of recurrences. Third, the nomogram provides a quantitative risk assessment that can be used to counsel patients about their individual risk of abdominal LNR to help them make informed treatment decisions.
Our study had several limitations that should be acknowledged. Firstly, The study was a retrospective investigation. It was difficult to standardize quality of the neoadjuvant therapy, surgery and adjuvant therapy at different clinical centers. And, there was no uniform criterion for performing adjuvant abdominal radiotherapy. These might affect the results of neoadjuvant and adjuvant therapy on recurrence. Secondly, there might be potential confounders that were not considered. As the primary aim of the study was to develop the prediction model for abdominal LNR after 3-LND, and this model performed well and showed good discrimination and calibration by using these three parameters. We believed that our nomogram model could be convenient and useful for clinicians to predict of abdominal LNR and to identify which patients need prophylactic abdominal radiotherapy.
Conclusion
Middle and lower TEC patients had a higher incidence of abdominal LNR. Tumor ___location, the pathologic N stage and number of preoperative abdominal LNM were risk factors for predicting abdominal LNR. The online dynamic nomograms showed good prediction performance and convenient clinical application, which provided clinicians with a quantitative tool for deciding which patients should undergo adjuvant abdominal radiotherapy.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Morgan, E. et al. The global landscape of esophageal squamous cell carcinoma and esophageal adenocarcinoma incidence and mortality in 2020 and projections to 2040: New estimates From GLOBOCAN 2020. Gastroenterology 163(3), 649–658 (2022).
Siaw-Acheampong, K. et al. Minimally invasive techniques for transthoracic oesophagectomy for oesophageal cancer: Systematic review and network meta-analysis. BJS Open. 4, 787–803 (2020).
Li, Y. et al. Changes in the recent three decades and survey on the current status of surgical treatment for esophageal cancer in China. Thoracic. Cancer. 15(22), 1705–1713 (2024).
Xu, Z.-C., Su, B.-A., Li, J.-C., Cheng, W.-F. & Chen, J. Pattern of relapse following three-field lymphadenectomy of esophageal carcinoma and related factors predictive of recurrence. Cancer/Radiothérapie 27(3), 189–195 (2023).
Ni, W. et al. Postoperative adjuvant therapy versus surgery alone for stage IIB-III esophageal squamous cell carcinoma: A phase III randomized controlled trial. Oncologist. 26(12), e2151–e2160 (2021).
Deng, W. et al. Postoperative radiotherapy in pathological T2–3N0M0 thoracic esophageal squamous cell carcinoma: Interim report of a prospective, phase III, randomized controlled study. Oncologist. 25(4), e701–e708 (2020).
Cai, W. J. & Xin, P. L. Pattern of relapse in surgical treated patients with thoracic esophageal squamous cell carcinoma and its possible impact on target delineation for postoperative radiotherapy. Radiother. Oncol. 96(1), 104–107 (2010).
Chen, J. et al. Patterns and rates of abdominal lymphatic metastasis following esophageal carcinoma. PLoS ONE 12(10), e0185424 (2017).
Zhang, W. C. et al. Patterns of failure after complete resection of thoracic esophageal squamous cell carcinoma: Implications for postoperative radiation therapy volumes. Chin. J. Radiat. Oncol. 21(1), 38–41 (2012).
Wang, Y. et al. Risk factors and patterns of abdominal lymph node recurrence after radical surgery for locally advanced thoracic esophageal squamous cell cancer. Cancer Manag. Res. 12, 3959–3969 (2020).
Gao, H.-M. et al. Construction of a predictive model of abdominal lymph node metastasis in thoracic esophageal squamous cell carcinoma and preliminary analysis of its effect on target for postoperative radiotherapy. Front. Surg. 16(9), 1039532 (2022).
Huang, Z., Hong, Z., Chen, L. & Kang, M. Nomogram for predicting occult locally advanced esophageal squamous cell carcinoma before surgery. Front. Surg. 9, 917070 (2022).
Wang, J. et al. Factors and a predictive nomogram for lymph node metastasis in superficial esophageal squamous cell carcinoma. World J. Gastroenterol. 29(47), 6138–6147 (2023).
Hu, J. F. et al. Increases prognostic value of clinical-pathological nomogram in patients with esophageal squamous cell carcinoma. Front. Oncol. 14, 997776. https://doi.org/10.3389/fonc.2023.997776 (2023).
Ding, T. et al. A survival prediction nomogram for esophageal squamous cell carcinoma treated with neoadjuvant chemoradiotherapy followed by surgery. Cancer Manag. Res. 9(13), 7771–7782 (2021).
Deng, W. et al. Nomogram to predict overall survival for thoracic esophageal squamous cell carcinoma patients after radical esophagectomy. Ann. Surg. Oncol. 26(9), 2890–2898 (2019).
Chen, J. et al. Number and ___location of positive nodes, postoperative radiotherapy, and survival after esophagectomy with three-field lymph node dissection for thoracic esophageal squamous cell carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 82(1), 475–482 (2012).
Xu, Z. C. & Su, B. A. Comparison of local recurrence patterns of postoperative radiotherapy with surgery alone for esophageal carcinoma patients. IJS Oncol. 6(1), 33–40 (2021).
Li, L. et al. Adjuvant therapeutic modalities following three-field lymph node dissection for stage II/III esophageal squamous cell carcinoma. J. Cancer 8(11), 2051–2059 (2017).
Luo, H. et al. Meta-analysis of survival benefit with postoperative chemoradiotherapy in patients of lymph node positive esophageal carcinoma. Clin. Transl. Oncol. 20(7), 889–898 (2018).
Chen, J. et al. The pattern and prevalence of lymphatic spread in thoracic oesophageal squamous cell carcinoma. Eur. J. Cardio-Thoracic Surg. 36(3), 480–486 (2009).
Hagens, E. R. C. et al. Distribution of lymph node metastases in esophageal carcinoma [TIGER study]: Study protocol of a multinational observational study. BMC Cancer 19(1), 662 (2019).
Rongxu, Du. et al. Postoperative lymphatic recurrence distribution and delineation of the radiation field in lower thoracic squamous cell esophageal carcinomas: A real-world study. Radiat Oncol. 17(1), 47 (2022).
Xiao, Z. F. et al. Influence of number of metastatic lymph nodes on survival of curative resected thoracic esophageal cancer patients and value of radiotherapy: Report of 549 cases. Int. J. Radiat. Oncol. Biol. Phys. 62(1), 82–90 (2005).
Chen, J. et al. Postoperative radiotherapy improved survival of poor prognostic squamous cell carcinoma esophagus. Ann. Thorac. Surg. 90(2), 435–442 (2010).
Tao, Y. et al. Risk factors of lymph node metastasis or lymphovascular invasion for superficial esophageal squamous cell carcinoma: A practical and effective predictive nomogram based on a cancer hospital data. Front. Med. (Lausanne). 17(9), 1038097 (2022).
Tong, Y. et al. A radiomics nomogram for predicting postoperative recurrence in esophageal squamous cell carcinoma. Front Oncol. 13, 1162238 (2023).
Zhu, Y.-T. et al. Developing and validating a predictive model of delivering large-for-gestational-age infants among women with gestational diabetes mellitus. World J. Diabetes 15(6), 1242–1253 (2024).
Ruan, R. et al. A nomogram for predicting lymphovascular invasion in superficial esophageal squamous cell carcinoma. Front. Oncol. 11, 663802 (2021).
Guo, X. et al. Value of nomogram incorporated preoperative tumor volume and the number of postoperative pathologically lymph node metastasis regions on predicting the prognosis of thoracic esophageal squamous cell carcinoma. Cancer Manag. Res. 13, 4619–4631 (2021).
Harada K, Hwang H, Wang X, et al. Frequency and implications of paratracheal lymph node metastases in resectable esophageal or gastroesophageal junction adenocarcinoma. Annals of surgery, 2021, 273 (4): 751-757.
Li, Y. et al. Predicting the value of adjuvant therapy in esophageal squamous cell carcinoma by combining the total number of examined lymph nodes with the positive lymph node ratio. Ann. Surg. Oncol. 26(8), 2367–2374 (2019).
Zhao, Q. et al. Accurate ___location describe and management of lymph node recurrence after esophagectomy for thoracic esophageal squamous cell carcinoma: A retrospective cohort study. Int. J. Surg. 110(6), 3440–3449 (2024).
Miyata, H. et al. Lymph node metastasis and recurrences from esophageal squamous cell carcinoma in patients with previous gastrectomy. Ann. Surg. Oncol. 27(13), 5312–5319 (2020).
Acknowledgements
This study was supported by grants from the Quanzhou Science and Technology Plan Project (2024NY005). This research did not increase the risk and economic burden of patients; the patients’ rights were fully protected; the project design was conducted in line with scientific and ethical principles. The institutional review board approved this project. All participants in this study provided informed written consent prior to enrollment.
Author information
Authors and Affiliations
Contributions
Conception and design: Zhi-Chen Xu; Administrative support:Bao-An Su; Qing-Hua Xu Provision of study materials or patients: Bao-An Su, Jian-cheng Li,Wen-Fang Cheng,Juhui Chen; Collection and assembly of data: Zhi-Chen Xu ; Mingqiang Lin;Meng-Ke Qu Data analysis and interpretation: Zhi-Chen Xu; All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, ZC., Su, BA., Lin, MQ. et al. A dynamic nomogram for predicting abdominal lymph node recurrence in patients with esophageal carcinoma. Sci Rep 15, 13412 (2025). https://doi.org/10.1038/s41598-025-97774-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-97774-x