Abstract
Early identification and management of asymptomatic carotid plaques can reduce the risk of cardiovascular and cerebrovascular events. This study aimed to explore the factors that affect carotid plaques in the Northern Chinese population and construct a nomogram for risk assessment to identify high-risk populations for carotid artery plaques. A cross-sectional study on cardiovascular factors was conducted in Shijingshan District, Beijing, from January 2022 and August to September 2023, targeting individuals aged 18 years and above. Carotid plaques were assessed via carotid ultrasound. LASSO regression was used for feature selection, logistic regression was employed to analyze risk factors, and a risk assessment nomogram was also developed.. The performance was evaluated using the area under the receiver operating characteristic curve (AUC), and the calibration was assessed through the Hosmer‒Lemeshow goodness-of-fit test. The study included a total of 828 subjects, with 558 in the normal group and 270 in the carotid plaque group. Thirty-three risk factors were included in the LASSO regression analysis as independent variables for screening. The results of the adjusted multiple logistic regression analysis show that age (OR = 6.81, 95% CI:4.371–10.758), unmarried marital status (OR = 3.475, 95% CI: 1.927–6.554), current smoking (OR = 2.318, 95% CI: 1.519–3.553), hypertension history (OR = 1.794, 95% CI: 1.123–2.860), dyslipidemia history (OR = 1.920, 95% CI: 1.149–3.215), systolic blood pressure (SBP) (OR = 1.014, 95% CI: 1.004–1.024), GLU (OR = 1.135, 95% CI: 1.017–1.272), and malondialdehyde (MDA) (OR = 1.014, 95% CI: 1.003–1.025) were associated with an increased risk of carotid plaques.In contrast, higher education levels were associated with a lower risk of carotid plaques, with education level (3) (OR = 0.436, 95% CI: 0.208–0.917) and education level (4) (OR = 0.348, 95% CI: 0.170–0.718) indicating a protective association. The constructed nomogram Risk assessment had an AUC of 0.850 (95% CI: 0.823–0.877) and demonstrated good calibration (χ2 = 13.973, P = 0.08246). By integrating age, education level, marital status, current smoking, hypertension history, dyslipidemia history, SBP, GLU and MDA, we developed a high-performance nomogram for assessment., which may be helpful for the early detection and prevention of carotid plaques in the general population. Further studies may be useful to validate the applicability in different regions and populations.
Similar content being viewed by others
Introduction
Carotid plaques are strongly associated with the development of cardiovascular diseases (CVD)1 and represent a localized manifestation of atherosclerosis. Their presence increases the risk of coronary artery disease (CAD)2, myocardial infarction3, and ischemic stroke4,5,6. In China, CVD remains the leading cause of mortality, surpassing cancer and other major diseases7 with the incidence of coronary heart disease and ischemic stroke continuing to rise8,9. Early identification and intervention for carotid plaques are crucial in reducing the risk of cardiovascular and cerebrovascular events.Studies suggest that carotid plaques, particularly in asymptomatic and preclinical stages, may exhibit distinct biological and genetic characteristics10,11. However, despite carotid ultrasound being the standard method for detecting plaques, it is not widely utilized in routine screening, leading to potential missed diagnoses12. Therefore, developing a reliable risk assessment tool is essential for identifying high-risk individuals and enabling timely intervention.This study aims to establish a simple and practical risk assessment for carotid plaques by integrating LASSO regression with logistic regression, facilitating early risk assessment in the general population.
Materials and methods
Study design
The study is a cross-sectional study. The survey was carried out in the Apple Orchard and Wulituo communities of Shijingshan district, Beijing, in January 2022 and from August to September 2023. Residents over 18 years old in these two communities were selected as study subjects using a cluster sampling method. In this study, trained staff conducted surveys on all participants and collected basic information, such as age, sex, height, weight, and waist circumference, as well as information on smoking, drinking, physical activity, and dietary habits, through questionnaires and physical examinations. Doppler ultrasound technology was used to measure the bilateral carotid intima‒media thickness and the presence of plaques. Fasting venous blood samples were taken to measure superoxide dismutase (SOD) activity, glutathione peroxidase 3 (GPX3) levels, malondialdehyde (MDA) levels, oxidized low-density lipoprotein (oxLDL) levels, and paraoxonase-1 (PON1) levels. The purpose of this cross-sectional study was to understand the status of carotid plaques in the general population through community surveys. On the basis of the data from the cross-sectional study, we aimed to identify risk factors associated with carotid plaques and to establish an assessment tool that visually and quantitatively represents the contribution of these risk factors. All participants signed written informed consent before the survey, and the study was approved by the ethics committee of Fuwai Hospital, and informed consent was obtained from all participants involved in the study. All procedures followed were in accordance with the ethical standards of the responsible committee and with the Helsinki Declaration.
Study subjects
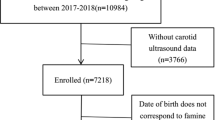
This cross-sectional study included a total of 828 participants, including 415 males and 413 females. The research plan initially included 1105 participants; however, owing to personal circumstances, a total of 158 participants failed to participate in the survey, resulting in a response rate of 85.70%. Furthermore, owing to insufficient variable information, an additional 119 individuals were excluded from the analysis(Fig. 1). All participating patients provided written informed consent and expressed their willingness to actively take part in the study.
Data collection
The variables in this study were selected based on their potential associations with carotid plaque formation and cardiovascular health. All the subjects underwent questionnaire surveys, physical examinations, laboratory tests, and carotid ultrasound examinations. The questionnaire collected basic information such as age, sex, medical history, smoking, drinking status, physical activity, dietary habits, and sleep duration. Smoking was defined as having smoked at least 20 packs of cigarettes in a lifetime and currently smoking. Drinking was defined as consuming at least one alcoholic beverage per week in the past month. A family history of cardiovascular disease was defined as having parents with hypertension, hyperlipidemia, diabetes, coronary heart disease, or stroke. The definition of hypertension includes: 1) a history of hypertension; 2) Take antihypertensive medication in the past two weeks; And/or 3) the average systolic blood pressure measured three times is ≥ 140 mmHg or the diastolic blood pressure is ≥ 90 mmHg. The definition of dyslipidemia includes: 1) previously diagnosed by a hospital and currently taking lipid-lowering drugs (such as statins and betas); 2) And/or abnormal fasting blood lipid testing. Nutrition data were assessed by evaluating the intake frequency of vegetables, fruits, meat, fish, and fried foods over the past month, with the average daily intake (g/day) calculated. Sleep time was determined based on participants’ reported average sleep duration on weekdays and weekends, from which the overall daily average sleep time (min/d) was derived. The height, weight, waist circumference, blood pressure, and heart rate were measured during the physical examination.Body mass index was calculated as weight divided by the square of height (kg/m2). Height was measured to the nearest 0.5 cm using a standard right-angle device and a fixed measuring tape while participants were barefoot. Weight was measured using the OMRON body fat and weight measurement device (V-Body HBF-371, OMRON) while participants wore light clothing. After resting for 5 min, blood pressure was measured three times at the heart level on the right arm using the OMRON HBP-1300 professional portable blood pressure monitor (OMRON), with 30-s intervals between measurements, in the presence of an observer. The average of the three readings was used for analysis.
Morning fasting elbow venous blood samples were collected. After standing for 30 min, the samples were centrifuged at 3000 rpm for 20 min to extract serum from the top layer, which was then stored at -80 °C until laboratory testing. Commercial kits were used to measure SOD activity (Human SOD Kit, Jiancheng Bioengineering Institute) and PON1 (Human PON1 ELISA Kit, Abcam), GPX3 (Human GPX3 ELISA Kit), and oxLDL (Human oxLDL ELISA Kit, Elabscience) levels. The MDA content was detected via the TBA spectrophotometric method (MDA Detection Kit, Jiancheng Bioengineering Institute). Total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), and fasting plasma glucose(FPG) were measured via a Beckman Coulter AU5811 automatic biochemical analyzer and reagents (USA).
Carotid artery ultrasound examination was performed using a color Doppler ultrasound diagnostic device (ACUSON Sequoia Silver). The subject was placed in a supine position, with clothing adjusted to fully expose the neck and head for examination. When one side was examined, the head was turned to the opposite side to ensure full exposure of the neck vessels. The common carotid artery and carotid sinus were scanned sequentially, and the intima-media thickness (IMT) was measured at the far wall of the distal common carotid artery (CCA), 1 cm proximal to the bifurcation, at end-diastole on both sides. A plaque is defined as a focal structure that invades at least 0.5 mm into the arterial lumen, 50% of the surrounding IMT, or an IMT > 1.5 mm13. Carotid ultrasound results were classified into two categories: the absence of plaque in all carotid arteries was considered normal, and the presence of a plaque in any carotid artery was considered carotid plaque.
Statistical analysis
All the statistical analyses were performed via SAS version 9.4 or R version 4.4.1. The 828 subjects were divided into normal and carotid plaque groups. Normally distributed measurements are presented as the means ± standard deviations and were compared between groups via t tests. Nonnormally distributed data are presented as medians and quartiles, and the Wilcoxon rank-sum test was used for group comparisons. Categorical variables are expressed as percentages and were compared via the chi-square test or Fisher’s exact test. LASSO regression analysis was employed to select feature variables and adjust for potential confounders in logistic regression. The assessment ability was evaluated using the area under the receiver operating characteristic (ROC) curve (AUC), and calibration was assessed via the Hosmer–Lemeshow test.. A two-sided P value < 0.05 was considered statistically significant.
Results
Characteristics of the participants in the cross-sectional study
This study included a total of 828 subjects, with 558 in the normal group and 270 in the carotid plaque group. There were statistically significant differences between the normal group and the carotid plaque group in terms of age, education level, marital status, current smoking rate, hypertension history, diabetes history, dyslipidemia history, daily intake of meat, moderate and above physical activity time, static behavior time, sleep time, SBP, DBP, heart rate, WC(Waist Circumference), Glu, GPX3, MDA, oxLDL, and PON1 (P < 0.05). The detailed data can be found in Table 1.
Feature selection via lasso regression
Further analysis of the risk factors for carotid artery plaques was conducted. Carotid artery plaques were treated as the dependent variable, and 33 risk factors in this group were included as independent variables for screening using LASSO regression. Using Lambda 1-se as the selection criterion for the final equation (λ = 0.03268302), eleven variables with nonzero coefficients were ultimately selected: Age, Education level, Marital status, Current smoking, Hypertension history, Dyslipidemia history, SBP, GLU, GPX3, MDA and oxLDL(Figs. 2 (a) and 2 (b)).
(a) LASSO regression coefficient path diagram. The 33 independent variables included in Lasso regression for variable screening are as follows: Gender, Age, Education level, Primary school and below, Ethnicity, Marital status, Current smoking, Current drinking, Hypertension history, Dyslipidemia history, Diabetes history, Vegetables, Fruit, Meat, Fried food, Moderate or above physical activity time, Static behavior time, Sleep time, BMI(Body Mass Index), SBP(Systolic Blood Pressure), DBP(Diastolic Blood Pressure), Heart rate, WC (Waist Circumference), TC (Total Cholesterol), LDL-C (Low-Density Lipoprotein Cholesterol), HDL-C(High-Density Lipoprotein Cholesterol), TG(Triglycerides), Glu(Glucose), GPX3(Glutathione Peroxidase 3), SOD(Superoxide Dismutase), MDA (Malondialdehyde), oxLDL (Oxidized Low-Density Lipoprotein), and PON1(Paraoxonase-1). (b) Cross validation diagram. Using LASSO regression analysis, eleven risk factors were selected (Age, Education level, Marital status, Current smoking, Hypertension history, Dyslipidemia history, SBP, GLU, GPX3, MDA and oxLDL). Two vertical lines were drawn at the optimal score according to the minimum standard (left dashed line) and the 1-s.e. standard (right blue line). Lambda 1-se was used as the selection criterion for the final equation.
Development of the assessment approach
Using the eleven characteristic variables selected by LASSO regression as independent variables and carotid plaque as the dependent variable, logistic regression analysis was performed. The results are shown in Table 2. The results of the adjusted multiple logistic regression analysis show that age (OR = 6.81, 95% CI:4.371–10.758), unmarried marital status (OR = 3.475, 95% CI: 1.927–6.554), current smoking (OR = 2.318, 95% CI: 1.519–3.553), hypertension history (OR = 1.794, 95% CI: 1.123–2.860), dyslipidemia history (OR = 1.920, 95% CI: 1.149–3.215), SBP (OR = 1.014, 95% CI: 1.004–1.024), GLU (OR = 1.135, 95% CI: 1.017–1.272), and MDA (OR = 1.014, 95% CI: 1.003–1.025) were associated with an increased risk of carotid plaques (P < 0.05).In contrast, higher education levels were associated with a lower risk of carotid plaques, with education level (3) (OR = 0.436, 95% CI: 0.208–0.917) and education level (4) (OR = 0.348, 95% CI: 0.170–0.718) indicating a protective association(P < 0.05).
Therefore, incorporating the above nine independent assessment factors, a nomogram for assessment the risk of carotid plaques in a cross-sectional study population is shown in Fig. 3.
Carotid artery plaque risk chart. The risk factors for the nomogram of carotid plaque risk include Age, Education level, Marital status, Current smoking, Hypertension history, Dyslipidemia history, SBP, GLU and MDA. Variable assignment: Age (1 = Age < 60, 2 = Age≧60, Use 1 as a reference), Education level (1 = Primary school and below, 2 = Middle school, 3 = High school/vocational school, 4 = College/bachelor’s degree or above, Use 1 as a reference), Marital status(0 = Married, 1 = Others, Use 0 as a reference), current smoking (0 = Not smoking, 1 = smoking, Use 0 as a reference), Hypertension history (0 = No, 1 = Yes, Use 0 as a reference), Dyslipidemia history (0 = No, 1 = Yes, Use 0 as a reference).
Evaluation of assessment performance
The ROC curve of the nomogram showed an AUC of 0.850 (95% CI: 0.823–0.877), as shown in Fig. 4a. The Hosmer–Lemeshow goodness-of-fit test indicated good calibration (χ2 = 13.973, P = 0.08246). The calibration curve of the nomogram for assessment carotid plaque risk also demonstrated excellent consistency (Fig. 4(b)). In summary, the nomogram exhibits strong performance in risk stratification.
(a) ROC validation of the carotid artery plaque risk assessment chart. The y-axis represents the true positive rate of risk factors. The x-axis represents the false positive rate of risk factors. (b) Calibration curves of the carotid plaque risk nomogram. The y-axis represents the actual diagnosis of carotid plaques, whereas the x-axis represents the risk of carotid plaques. The “ideal” line is the calibration curve, and the "bias-corrected" line represents a correction made to the ideal curve. A curve that is closer to the diagonal dashed line indicates better performance.
Discussion
To understand and assess the formation of carotid plaques in the general population, we utilized LASSO regression and logistic regression analysis to identify nine independent risk factors: age, education level, marital status, current smoking, hypertension history, dyslipidemia history, SBP, GLU and MDA. On the basis of these factors, we constructed a nomogram assessment tool and evaluated via the area under the receiver operating characteristic curve (AUC). The results revealed that the AUC was 0.850 (95% CI: 0.823–0.877), indicating high discriminatory performance. Moreover, the analysis demonstrated good calibration (χ2 = 13.973, P = 0.08246), further validating its reliability.
The findings of this study indicate that age is an important risk factor for carotid plaque formation. Compared with the healthy population, individuals with carotid plaques are generally older. Other studies also indicate that the detection rate of carotid plaques significantly increases with age. The aging process leads to changes in the morphology and function of carotid arteries, which in turn induces the formation of plaques14,15. Compared with that in younger individuals, the risk of carotid plaques is greater in elderly individuals, which may be related to changes in lipid metabolism, reduced vascular elasticity, and enhanced inflammatory responses in elderly individuals. Age is an important risk factor for carotid plaques and involves multiple factors, such as unhealthy lifestyles16, genetics, and disease states17. Therefore, monitoring and managing carotid artery health should be strengthened for the elderly population, especially those with unhealthy habits or specific clinical conditions.
The present study demonstrated that the smoking rate in the carotid plaque group was significantly higher than that in the normal group, indicating that smoking is a significant risk factor for carotid plaque formation. A study by Kiriyama18 also indicated that even after adjusting for age, sex, and other established cardiovascular risk factors, the incidence of high-risk plaques remained significantly higher in smokers than in non-smokers. The effects of smoking extend beyond the quantity of carotid plaque; they also influence its composition. Research has suggested that smoking increases the expression of inflammatory markers and tissue-destructive enzymes in carotid plaques, which may contribute to plaque instability and an increased risk of cardiovascular events19. Furthermore, smoking is linked to the density of carotid plaques. Current smokers are more likely to have high-density calcified plaques or low-density soft plaques, which are more prone to rupture20. Consequently, smoking can be considered an independent risk factor for plaque formation. Therefore, smoking cessation is crucial for preventing and reducing carotid plaque formation.
The study found that educational level and marital status are both associated with the risk of carotid plaques, consistent with findings from other studies21. Individuals with higher education levels have a lower risk, possibly due to healthier lifestyles, better disease management skills, and greater access to healthcare. In contrast, those with lower education levels are more likely to smoke22,23, engage in less physical activity, and have poorer chronic disease management, accelerating the progression of atherosclerosis.Additionally, the study found that unmarried individuals have a higher risk of carotid plaques, which may be related to insufficient social support, a higher prevalence of unhealthy lifestyles, and weaker health management abilities. Previous studies24 have shown that unmarried individuals have poorer cardiovascular health. Married individuals, supported by their partners, are more likely to adopt healthy behaviors, such as maintaining a balanced diet, exercising regularly, and undergoing routine health check-ups. In contrast, unmarried individuals may have higher smoking rates, poorer dietary habits, and lower medical adherence. These findings suggest the need to strengthen health education and screening for individuals with lower education levels and those who are unmarried, raising awareness of disease prevention and optimizing prevention strategies to reduce the risk of cardiovascular diseases and improve long-term health outcomes.This study found that GLU (blood glucose levels) is associated with the risk of carotid plaque, consistent with previous research25. Hyperglycemia may promote atherosclerosis through oxidative stress, inflammation, and endothelial dysfunction. Studies have shown26 that individuals with diabetes and prediabetes have a higher risk of carotid atherosclerosis. Since this study did not include a history of diabetes, The association of GLU levels may be independent of a diabetes diagnosis, suggesting that even in non-diabetic individuals, elevated blood glucose may increase the risk of plaque formation.It is essential to strengthen blood glucose management through lifestyle interventions and medication while ensuring regular monitoring to identify high-risk individuals early and optimize intervention strategies to reduce cardiovascular risk.This study identified a history of hypertension as a risk factor for carotid plaque formation. Research27 has shown that individuals with hypertension face a significantly higher risk of developing carotid plaques, with the severity of hypertension positively correlated with plaque formation. Prolonged exposure to high blood pressure damages the arterial intima, facilitating lipid deposition and plaque development. Hypertension may contribute to plaque formation through multiple mechanisms, including promoting inflammation28, altering vascular wall mechanics 29, and affecting blood pressure stability. Notably, increased blood pressure variability, particularly in systolic blood pressure (SBP), is linked to carotid plaque formation 14. Our findings also highlight the strong association between elevated SBP and carotid plaques. High SBP induces turbulent blood flow at arterial bifurcations, increasing shear stress and endothelial damage, thereby promoting plaque development30,31. Sustained hypertension triggers vascular remodeling, leading to arterial wall thickening and lumen narrowing, further contributing to plaque progression. Additionally, microvascular damage caused by high SBP results in local hypoxia, enhancing lipid and inflammatory cell deposition in the arterial wall32. The findings of the study conducted by Xie30 and colleagues indicated that individuals with high SBP had a significantly higher incidence of newly formed carotid plaques and an increased risk over the next ten years.In summary, hypertension history and elevated SBP are closely linked to carotid plaque formation. Effective management and monitoring of hypertensive patients and individuals with high SBP are crucial in reducing the risk of carotid plaques and preventing related complications.
The results of this study demonstrated that a history of dyslipidemia was a risk factor for carotid plaque formation. Research has shown that LDL-C is an important risk factor of carotid plaques, with elevated levels increasing the risk33,34. while HDL-C helps transport cholesterol and reduces plaque formation35. Research has shown that reduced HDL-C levels are associated with an increased risk of carotid plaques. Certain subtypes of HDL-C, such as HDL-3, may be better of carotid disease36. Additionally, the ratio of LDL-C to HDL-C (LDL-C/HDL-C) is an independent risk factor for unstable carotid plaques (a high LDL-C/HDL-C ratio accelerates the occurrence of carotid plaques)37,38. Additionally, TG, TC, and non-HDL-C are also linked to a higher plaque risk39. In this study, no significant differences were observed in TC, LDL-C, and HDL-C levels between the healthy and plaque groups, and lipid indicators were not found to be associated with plaque risk. This may be due to interventions taken by individuals with dyslipidemia after becoming aware of their condition, leading to improved baseline lipid levels. These findings indirectly emphasize the importance of comprehensive lipid management in reducing the risk of carotid plaques.
This study found significant differences in GPX3, MDA, oxLDL, and PON1 levels between healthy individuals and those with carotid plaques, with MDA levels closely associated with an increased risk of carotid plaques. Oxidative stress refers to an imbalance between the production and clearance of reactive oxygen species (ROS) in the body, leading to cellular and tissue damage. In cardiovascular diseases, ROS participate in pathological processes through various mechanisms, such as altering endothelial cell function and promoting the formation and progression of atherosclerotic plaques40. This study further directly confirmed the correlation between MDA and carotid plaques, providing new insights for the prevention and treatment of carotid atherosclerosis. Additionally, PON1 protects low-density lipoprotein from oxidation through its antioxidant effects, and its activity is negatively correlated with IMT41,42. A decrease in PON1 activity may be associated with an increased susceptibility to plaque formation. Although GPX3 and oxLDL were not ultimately identified as risk-associated factors for carotid plaques, their close association with carotid plaques was still demonstrated to some extent, laying the foundation for further research.
In this study, participants with longer durations of moderate or above physical activity and shorter sedentary time showed a higher prevalence of carotid plaques. This may be due to the cumulative nature of carotid plaque formation, which reflects past lifestyle and health conditions rather than just current activity patterns. The cross-sectional design also precludes causal inference, raising the possibility of reverse causation—individuals at higher risk may have increased physical activity and reduced sedentary time for health management. Moreover, the type, intensity, and consistency of activity may be more relevant than duration alone, warranting further exploration.
By analyzing the relationships between these nine independent factors and carotid plaques, we can gain a deeper understanding of plaque formation mechanisms and provide scientific evidence for early prevention and intervention. An increase in age and SBP, along with current smoking, hypertension history, dyslipidemia history, and elevated GLU and MDA levels, directly or indirectly contributes to arterial wall damage and lipid deposition, promoting plaque formation. Additionally, variations in education level and marital status may influence health awareness, lifestyle choices, and access to healthcare, further affecting carotid plaque risk. Our study has significant clinical implications. Identifying these independent factors enables healthcare professionals to detect high-risk individuals earlier and implement targeted preventive measures. For instance, individuals with a history of hypertension, dyslipidemia, or elevated GLU and oxidative stress markers (such as MDA) may benefit from more frequent monitoring for carotid plaque progression. Early interventions, including lifestyle modifications and medical treatments, can be tailored to these high-risk individuals, potentially reducing the incidence of cardiovascular and cerebrovascular diseases. By developing a nomogram that incorporates these risk factors, individualized carotid plaque risk assessment in clinical practice can be enhanced, enabling personalized prevention and treatment strategies, improving patient outcomes, and ultimately reducing cardiovascular events and healthcare costs. Future research should explore additional potential risk factors and validate this approach across diverse populations to further optimize carotid plaque assessment and prevention.
Strengths and limitations
Our study analyzed a broad range of variables, including data from traditional questionnaires, physical exams, laboratory tests, carotid ultrasound examinations, and oxidative stress markers, providing a comprehensive analysis. The inclusion of oxidative stress markers is a key strength of this study, offering new insights into their role in carotid plaque formation.However, several limitations should be considered. First, the cross-sectional design prevents us from establishing causal relationships between risk factors and carotid plaque formation, highlighting the need for future prospective cohort studies. Second, while LASSO regression was used to identify the most relevant risk factors, some potentially important factors, such as a history of diabetes, were not included in the final selection. This may be due to their relatively low contribution, collinearity with other variables, or limited statistical power given the sample size.Third, the exclusion of some participants due to personal reasons or insufficient data may have introduced selection bias. Although LASSO regression helps control for confounding factors, it cannot completely eliminate bias, and future research should focus on optimizing sample selection. Fourth, our study population was drawn from a specific geographic region (northern China), so the generalizability of these findings to other regions remains uncertain. Larger sample sizes and studies in diverse populations are needed to validate these results.Finally, while our analys demonstrated high discriminative ability and good calibration within the study population, it has not been externally validated. This limits our ability to assess its generalizability and robustness across different populations. Future studies should incorporate independent datasets from diverse populations for external validation to further enhance the reliability .
Conclusions
In conclusion, this study identified nine independent risk factors for carotid plaque and developed a high-performance nomogram assessment tool. The analysis contributes to the early detection and prevention of carotid plaques, ultimately improving patient prognosis and reducing healthcare costs. Future research with a larger sample size and validation across different regions and populations may be necessary to further enhance early detection and intervention strategies for carotid plaques.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to restrictions imposed by the ethics committee. However, they may be made available from the corresponding author upon reasonable request.
References
Wyman, R. A. et al. Ultrasound-detected carotid plaque as a predictor of cardiovascular events. Vasc. Med. 11(2), 123–130 (2006).
Gaĭgalaĭte, V. et al. Association between structure of atherosclerotic plaques in carotid arteries and myocardial infarction. Kardiologiia 53(9), 21–25 (2013).
Zhang, Y. et al. Association between the triglyceride-glucose index and carotid plaque incidence: A longitudinal study. Cardiovasc. Diabetol. 21(1), 244 (2022).
Liu, J. et al. Deep learning based on carotid transverse B-mode scan videos for the diagnosis of carotid plaque: a prospective multicenter study. Eur. Radiol. 33(5), 3478–3487 (2023).
Finn, C. et al. The Association between Carotid Artery Atherosclerosis and Silent Brain Infarction: A Systematic Review and Meta-analysis. J. Stroke Cerebrovasc. Dis. 26(7), 1594–1601 (2017).
Min W. U., Xiao-Yan X., Jian Y., et al. Correlation of acute ischemic cerebral infarction with carotid atherosclerosis plaque. J Postgrad Med, (2009).
HEALTH T W C O T A R O C, CHINA D I. Interpretation of the Annual Report on Cardiovascular Health and Diseases in China 2022 [J]. Cardiology Discovery, 4(1): 58–80. (2024)
Wang, Z. et al. Summary of the 2022 Report on Cardiovascular Health and Diseases in China. Chin. Med. J. (Engl) 136(24), 2899–2908 (2023).
Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019 [J]. Lancet Neurol, 20(10): 795–820 (2021)
Spence, J. D. Technology Insight: Ultrasound measurement of carotid plaque–patient management, genetic research, and therapy evaluation. Nat. Clin. Pract. Neurol. 2(11), 611–619 (2006).
Rundek, T. et al. Carotid plaque, a subclinical precursor of vascular events: The Northern Manhattan Study. Neurology 70(14), 1200–1207 (2008).
Wu, D. et al. An accurate and explainable ensemble learning method for carotid plaque prediction in an asymptomatic population. Comput. Methods Programs Biomed. 221, 106842 (2022).
Touboul P J, Hennerici M G, Meairs S, et al. Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011 [J]. Cerebrovasc Dis, 34(4): 290–296 (2012)
Liu, A. et al. Carotid atherosclerosis is associated with hypertension in a hospital-based retrospective cohort. Int. J. Clin. Exp. Med. 8(11), 21932–21938 (2015).
Garg, S., Kashikar, S. V. & Phatak, S. Colour Doppler Evaluation of Extracranial Carotid Arteries: A Clinical and Radiological Correlation. J. Clin. Diagn. Res. https://doi.org/10.7860/JCDR/2016/15426.7130 (2016).
Redgrave, J. N., Lovett, J. K. & Rothwell, P. M. Histological features of symptomatic carotid plaques in relation to age and smoking: The oxford plaque study. Stroke 41(10), 2288–2294 (2010).
Yamagami, K. et al. Abstract TP129: Aging is Associated with Vulnerability of Carotid Plaques in Patients With Type 2 Diabetes Mellitus. Stroke https://doi.org/10.1161/str.47.suppl_1.tp129 (2016).
Kiriyama, H. et al. Effect of cigarette smoking on carotid artery atherosclerosis: A community-based cohort study. Heart Vessels. 35(1), 22–29 (2020).
Kangavari, S. et al. Smoking increases inflammation and metalloproteinase expression in human carotid atherosclerotic plaques. J. Cardiovasc. Pharmacol. Ther. 9(4), 291–298 (2004).
Yang, D. et al. Cigarette Smoking and Carotid Plaque Echodensity in the Northern Manhattan Study. Cerebrovasc. Dis. 40(3–4), 136–143 (2015).
Dienhart, C. et al. Including educational status may improve cardiovascular risk calculations such as SCORE2. Front. Cardiovasc. Med. 11, 1345277 (2024).
Nang, E. E. et al. Association of Television Viewing Time with Body Composition and Calcified Subclinical Atherosclerosis in Singapore Chinese. PLoS ONE 10(7), e0132161 (2015).
Redondo-Bravo, L. et al. Does Socioeconomic Status Influence the Risk of Subclinical Atherosclerosis?: A Mediation Model. J. Am. Coll. Cardiol. 74(4), 526–535 (2019).
Paalanen, L. et al. Inequalities by education and marital status in the co-occurrence of cardiovascular risk factors in Finland persisted between 1997–2017. Sci. Rep. 10(1), 9123 (2020).
Bjarnason, T. A. et al. Oral glucose tolerance test predicts increased carotid plaque burden in patients with acute coronary syndrome. PLoS ONE 12(8), e0183839 (2017).
Jiang, Z. Z. et al. A High Triglyceride-Glucose Index Value Is Associated With an Increased Risk of Carotid Plaque Burden in Subjects With Prediabetes and New-Onset Type 2 Diabetes: A Real-World Study. Front. Cardiovasc. Med. 9, 832491 (2022).
Su, T. C. et al. Hypertension status is the major determinant of carotid atherosclerosis: A community-based study in Taiwan. Stroke 32(10), 2265–2271 (2001).
Hashimoto, H. et al. Relationship between C-reactive protein and progression of early carotid atherosclerosis in hypertensive subjects. Stroke 35(7), 1625–1630 (2004).
Beaussier, H. et al. Carotid plaque, arterial stiffness gradient, and remodeling in hypertension. Hypertension 52(4), 729–736 (2008).
Gaoqiang, X. et al. OS 17–01 Relationship of baseline blood pressure with 10 years progression of carotid atherosclerosis. J. Hypertens. 34, e221–e221 (2016).
Frank, H. et al. Effect of shear stress on vascular inflammation and plaque development. Curr. Opin. Lipidol. 18(5), 527–533 (2007).
Silver, A. E. & Vita, J. A. Shear-stress-mediated arterial remodeling in atherosclerosis: too much of a good thing?. Circulation 113(24), 2787–2789 (2006).
Grønholdt, M. L. M. Ultrasound and lipoproteins as predictors of lipid-rich, rupture-prone plaques in the carotid artery. Arterioscler. Thromb. Vasc. Biol. 19(1), 2–13 (1999).
Tada, H. et al. Coronary Artery and Carotid Artery Plaques in Patients With Heterozygous Familial Hypercholesterolemia. JACC Adv. 2(8), 100594 (2023).
Li, Z. et al. Low-/high-density lipoprotein cholesterol ratio and carotid plaques in patients with coronary heart disease: A Chinese cohort study. Lipids Health Dis. 20(1), 144 (2021).
Kim, D. S. et al. HDL-3 is a superior predictor of carotid artery disease in a case-control cohort of 1725 participants. J. Am. Heart Assoc. 3(3), e000902 (2014).
Liu, H. et al. Relationship of the Low-Density Lipoprotein Cholesterol/High-Density Lipoprotein Cholesterol Ratio with a Vulnerable Plaque in Patients with Severe Carotid Artery Stenosis: A Case-Control Study in the Han Chinese Population. Curr. Neurovasc. Res. 19(2), 160–170 (2022).
Wu, Z. et al. Serum LDL-C/HDL-C ratio and the risk of carotid plaques: A longitudinal study. BMC Cardiovasc. Disord. 22(1), 501 (2022).
Wu, J. et al. Association between non-high-density lipoprotein cholesterol levels and asymptomatic vulnerable carotid atherosclerotic plaques. Eur. J. Neurol. 26(12), 1433–1438 (2019).
Senoner, T. & Dichtl, W. Oxidative Stress in Cardiovascular Diseases: Still a Therapeutic Target?. Nutrients 11(9), 2090 (2019).
Harangi, M. et al. Association between human paraoxonase 1 activity and intima-media thickness in subjects under 55 years of age with carotid artery disease. Cerebrovasc. Dis. 25(1–2), 122–128 (2008).
Gungor, O. et al. The associations between serum paraoxonase 1 activity and carotid atherosclerosis in renal transplant patients. Clin. Nephrol. 80(3), 198–202 (2013).
Acknowledgements
We would like to thank all the medical staff who participated in this study for their time and dedication. Moreover, we would like to express our gratitude to all the research subjects who participated in this study.
Funding
The study was supported by the National Natural Science Foundation of China (81973117).
Author information
Authors and Affiliations
Contributions
Authors’ Contributions KY prepared the draft manuscript and statistically analyzed the data. LZ designed the concept of the study. LC, and CJ provided guidance on the study design and editing. YH, JS, LD, YY, YT, TX, ML and ZW effectively worked for the data collection. LZ critically reviewed/edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yuan, K., Li, C., Chu, J. et al. The study on risk assessment of carotid plaques in the Northern Chinese population based on LASSO regression. Sci Rep 15, 16391 (2025). https://doi.org/10.1038/s41598-025-99723-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-99723-0