Abstract
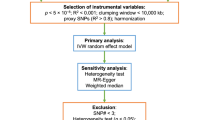
Obesity is a major risk factor for Coronavirus disease (COVID-19) severity; however, the mechanisms underlying this relationship are not fully understood. As obesity influences the plasma proteome, we sought to identify circulating proteins mediating the effects of obesity on COVID-19 severity in humans. Here, we screened 4,907 plasma proteins to identify proteins influenced by body mass index using Mendelian randomization. This yielded 1,216 proteins, whose effect on COVID-19 severity was assessed, again using Mendelian randomization. We found that an s.d. increase in nephronectin (NPNT) was associated with increased odds of critically ill COVID-19 (OR = 1.71, P = 1.63 × 10-10). The effect was driven by an NPNT splice isoform. Mediation analyses supported NPNT as a mediator. In single-cell RNA-sequencing, NPNT was expressed in alveolar cells and fibroblasts of the lung in individuals who died of COVID-19. Finally, decreasing body fat mass and increasing fat-free mass were found to lower NPNT levels. These findings provide actionable insights into how obesity influences COVID-19 severity.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
GWAS summary statistics for each trait are available as follows:
BMI (https://portals.broadinstitute.org/collaboration/giant/).
Plasma proteome from the deCODE study (https://www.decode.com/summarydata/).
COVID-19 outcomes (https://www.covid19hg.org/results/r7/).
GTEx Portal v.8 (https://gtexportal.org/home/datasets/).
Plasma proteome from BQC19 (https://www.mcgill.ca/genepi/mcg-covid-19-biobank). Access to the data of BQC19 can be obtained upon approval of requests via bqc19.ca.
Cis-pQTLs of each study are available in the corresponding publications’ supplementary materials26,27,28.
Body fat percentage, body fat mass and fat-free mass GWASs are available at IEU OpenGWAS project with accession IDs ukb-b-8909, ukb-b-19393 and ukb-b-13354, respectively (https://gwas.mrcieu.ac.uk/).
scRNA-seq data of COVID-19 lung autopsy samples are available at the Single-Cell Portal under accession ID SCP1052 (https://singlecell.broadinstitute.org/single_cell/). CADD-scores v.1.6 can be accessed at https://cadd.gs.washington.edu/score.
Genotype data from the 1000 Genomes Project is available at https://www.internationalgenome.org/data.
Source data are provided with this paper.
Code availability
We used R v.4.1.2 (https://www.r-project.org/), TwoSampleMR v.0.5.6 (https://mrcieu.github.io/TwoSampleMR/), snappy v.1.0 (https://gitlab.com/richards-lab/vince.forgetta/snappy), coloc v.5.1.0 (https://chr1swallace.github.io/coloc/), FINEMAP R package v.1.4, Seurat v.4.0.6 (https://satijalab.org/seurat/), PLINK v.1.9 (http://pngu.mgh.harvard.edu/purcell/plink/) and GCTA fastGWA v.1.93.3 (https://yanglab.westlake.edu.cn/software/gcta/). Custom codes are available on GitHub (https://github.com/satoshi-yoshiji/TwostepMR_obesity_COVID/).
References
Johns Hopkins University. COVID-19 Global Map https://coronavirus.jhu.edu/map.html (2022).
COVID-19 Host Genetics Initiative. Mapping the human genetic architecture of COVID-19. Nature 600, 472–477 (2021).
Stefan, N., Birkenfeld, A. L., Schulze, M. B. & Ludwig, D. S. Obesity and impaired metabolic health in patients with COVID-19. Nat. Rev. Endocrinol. 16, 341–342 (2020).
Foulkes, A. S. et al. Understanding the link between obesity and severe COVID-19 outcomes: causal mediation by systemic inflammatory response. J. Clin. Endocrinol. Metab. 107, e698–e707 (2021).
Zickler, M. et al. Replication of SARS-CoV-2 in adipose tissue determines organ and systemic lipid metabolism in hamsters and humans. Cell. Metab. 34, 1–2 (2022).
Goudswaard, L. J. et al. Effects of adiposity on the human plasma proteome: observational and Mendelian randomisation estimates. Int. J. Obes. 45, 2221–2229 (2021).
Zaghlool, S. B. et al. Revealing the role of the human blood plasma proteome in obesity using genetic drivers. Nat. Commun. 12, 1279 (2021).
Filbin, M. R. et al. Longitudinal proteomic analysis of severe COVID-19 reveals survival-associated signatures, tissue-specific cell death, and cell–cell interactions. Cell. Rep. Med. 2, 100287 (2021).
Skrivankova, V. W. et al. Strengthening the reporting of observational studies in epidemiology using Mendelian randomization. JAMA 326, 1614 (2021).
Skrivankova, V. W. et al. Strengthening the reporting of observational studies in epidemiology using Mendelian randomisation (STROBE-MR): explanation and elaboration. BMJ 375, n2233 (2021).
Ponsford, M. J. et al. Cardiometabolic traits, sepsis, and severe COVID-19: a Mendelian randomization investigation. Circulation 142, 1791–1793 (2020).
Luo, S., Liang, Y., Wong, T. H. T., Schooling, C. M. & Au Yeung, S. L. Identifying factors contributing to increased susceptibility to COVID-19 risk: a systematic review of Mendelian randomization studies. Int. J. Epidemiol. 51, 1088–1105 (2022).
Zhou, S. et al. A Neanderthal OAS1 isoform protects individuals of European ancestry against COVID-19 susceptibility and severity. Nat. Med. 27, 659–667 (2021).
Gaziano, L. et al. Actionable druggable genome-wide Mendelian randomization identifies repurposing opportunities for COVID-19. Nat. Med. 27, 668–676 (2021).
Bovijn, J., Lindgren, C. M. & Holmes, M. V. Genetic variants mimicking therapeutic inhibition of IL-6 receptor signaling and risk of COVID-19. Lancet Rheumatol. 2, e658–e659 (2020).
Klaric, L. et al. Mendelian randomisation identifies alternative splicing of the FAS death receptor as a mediator of severe COVID-19. Preprint at medRxiv https://doi.org/10.1101/2021.04.01.21254789 (2021).
Niemi, M. E. K., Daly, M. J. & Ganna, A. The human genetic epidemiology of COVID-19. Nat. Rev. Genet. 23, 533–546 (2022).
Pietzner, M. et al. ELF5 is a potential respiratory epithelial cell-specific risk gene for severe COVID-19. Nat. Commun. 13, 4484 (2022).
RECOVERY Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 397, 1637–1645 (2021).
Holmes, M. V., Richardson, T. G., Ference, B. A., Davies, N. M. & Davey Smith, G. Integrating genomics with biomarkers and therapeutic targets to invigorate cardiovascular drug development. Nat. Rev. Cardiol. 18, 435–453 (2021).
Manousaki, D., Mokry, L. E., Ross, S., Goltzman, D. & Richards, J. B. Mendelian Randomization Studies Do Not Support a Role for Vitamin D in Coronary Artery Disease. Circ. Cardiovasc. Genet. 9, 349–356 (2016).
Jiang, X. et al. Circulating vitamin D concentrations and risk of breast and prostate cancer: a Mendelian randomization study. Int. J. Epidemiol. 48, 1416–1424 (2019).
Meng, X. et al. Phenome-wide Mendelian-randomization study of genetically determined vitamin D on multiple health outcomes using the UK Biobank study. Int. J. Epidemiol. 48, 1425–1434 (2019).
Manson, J. E. et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N. Engl. J. Med. 380, 33–44 (2019).
Yengo, L. et al. Meta-analysis of genome-wide association studies for height and body mass index in ∼700000 individuals of European ancestry. Hum. Mol. Genet. 27, 3641–3649 (2018).
Ferkingstad, E. et al. DECODE: Large-scale integration of the plasma proteome with genetics and disease. Nat. Genet. 53, 1712–1721 (2021).
Pietzner, M. et al. Synergistic insights into human health from aptamer- and antibody-based proteomic profiling. Nat. Commun. 12, 6822 (2021).
Emilsson, V. et al. Co-regulatory networks of human serum proteins link genetics to disease. Science 361, 769–773 (2018).
Lawlor, D. A., Harbord, R. M., Sterne, J. A. C., Timpson, N. & Davey Smith, G. Mendelian randomization: Using genes as instruments for making causal inferences in epidemiology. Stat. Med. 27, 1133–1163 (2008).
Bowden, J., Davey Smith, G. & Burgess, S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 44, 512–525 (2015).
Swerdlow, D. I. et al. Selecting instruments for Mendelian randomization in the wake of genome-wide association studies. Int. J. Epidemiol. 45, 1600–1616 (2016).
Zhang, J. et al. Plasma proteome analyses in individuals of European and African ancestry identify cis-pQTLs and models for proteome-wide association studies. Nat. Genet. 54, 593–602 (2022).
Staley, J. R. et al. PhenoScanner: a database of human genotype-phenotype associations. Bioinformatics 32, 3207–3209 (2016).
Tsukui, T. et al. Collagen-producing lung cell atlas identifies multiple subsets with distinct localization and relevance to fibrosis. Nat. Commun. 11, 1920 (2020).
Xie, T. et al. Single-cell deconvolution of fibroblast heterogeneity in mouse pulmonary fibrosis. Cell Rep. 22, 3625–3640 (2018).
Obeidat, M. E. et al. Molecular mechanisms underlying variations in lung function: a systems genetics analysis. Lancet Respir. Med. 3, 782–795 (2015).
Bhatt, S. P. et al. Discriminative accuracy of FEV1:FVC thresholds for COPD-related hospitalization and mortality. JAMA 321, 2438–2447 (2019).
Davies, N. M., Holmes, M. V. & Davey Smith, G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ 362, k601 (2018).
Holmes, M. V., Ala-Korpela, M. & Smith, G. D. Mendelian randomization in cardiometabolic disease: challenges in evaluating causality. Nat. Rev. Cardiol. 14, 577–590 (2017).
Au Yeung, S. L., Li, A. M., He, B., Kwok, K. O. & Schooling, C. M. Association of smoking, lung function and COPD in COVID-19 risk: a two-step Mendelian randomization study. Addiction 117, 2027–2036 (2022).
Lawlor, D. A., Tilling, K. & Davey Smith, G. Triangulation in aetiological epidemiology. Int. J. Epidemiol. 45, 1866–1886 (2016).
Kircher, M. et al. A general framework for estimating the relative pathogenicity of human genetic variants. Nat. Genet. 46, 310–315 (2014).
Saferali, A. et al. Characterization of a COPD-associated NPNT functional splicing genetic variant in human lung tissue via long-read sequencing. Preprint at medRxiv https://doi.org/10.1101/2020.10.20.20203927 (2020).
Shrine, N. et al. New genetic signals for lung function highlight pathways and chronic obstructive pulmonary disease associations across multiple ancestries. Nat. Genet. 51, 481–493 (2019).
Sakornsakolpat, P. et al. Genetic landscape of chronic obstructive pulmonary disease identifies heterogeneous cell-type and phenotype associations. Nat. Genet. 51, 494–505 (2019).
GTEx Consortium. The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science 369, 1318–1330 (2020).
Delorey, T. M. et al. COVID-19 tissue atlases reveal SARS-CoV-2 pathology and cellular targets. Nature 595, 107–113 (2021).
Woolf, B., Zagkos, L. & Gill, D. TwoStepCisMR: a novel method and R package for attenuating bias in cis-Mendelian randomization analyses. Genes 13, 1541 (2022).
Burgess, S., Daniel, R. M., Butterworth, A. S., Thompson, S. G. & Consortium, E. P.-I. Network Mendelian randomization: using genetic variants as instrumental variables to investigate mediation in causal pathways. Int. J. Epidemiol. 44, 484–495 (2015).
Relton, C. L. & Davey Smith, G. Two-step epigenetic Mendelian randomization: a strategy for establishing the causal role of epigenetic processes in pathways to disease. Int. J. Epidemiol. 41, 161–176 (2012).
Sanderson, E., Spiller, W. & Bowden, J. Testing and correcting for weak and pleiotropic instruments in two-sample multivariable Mendelian randomization. Stat. Med. 40, 5434–5452 (2021).
Brandenberger, R. et al. Identification and characterization of a novel extracellular matrix protein nephronectin that is associated with integrin α8β1 in the embryonic kidney. J. Cell Biol. 154, 447–458 (2001).
Morimura, N. et al. Molecular cloning of POEM: a novel adhesion molecule that interacts with α8β1 integrin. J. Biol. Chem. 276, 42172–42181 (2001).
Inagaki, F. F. et al. Nephronectin is upregulated in acute and chronic hepatitis and aggravates liver injury by recruiting CD4-positive cells. Biochem. Biophys. Res. Commun. 430, 751–756 (2013).
Kon, S., Honda, M., Ishikawa, K., Maeda, M. & Segawa, T. Antibodies against nephronectin ameliorate anti-type II collagen-induced arthritis in mice. FEBS Open Bio. 10, 107–117 (2020).
O’Rourke, R. W. & Lumeng, C. N. Pathways to severe COVID-19 for people with obesity. Obesity 29, 645–653 (2021).
Strunz, M. et al. Alveolar regeneration through a Krt8+ transitional stem cell state that persists in human lung fibrosis. Nat. Commun. 11, 3559 (2020).
Xie, T. et al. Mesenchymal growth hormone receptor deficiency leads to failure of alveolar progenitor cell function and severe pulmonary fibrosis. Sci. Adv. 7, eabg6005 (2021).
Stiegler, P. & Cunliffe, A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. 36, 239–262 (2006).
Jastreboff, A. M. et al. Tirzepatide once weekly for the treatment of obesity. N. Engl. J. Med. 387, 205–216 (2022).
Heise, T. et al. Effects of subcutaneous tirzepatide versus placebo or semaglutide on pancreatic islet function and insulin sensitivity in adults with type 2 diabetes: a multicentre, randomised, double-blind, parallel-arm, phase 1 clinical trial. Lancet Diabetes Endocrinol. 10, 418–429 (2022).
Garvey, W. T. et al. Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial. Nat. Med. 28, 2083–2091 (2022).
Blundell, J. et al. Effects of once-weekly semaglutide on appetite, energy intake, control of eating, food preference and body weight in subjects with obesity. Diabetes Obes. Metab. 19, 1242–1251 (2017).
Pi-Sunyer, X. et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N. Engl. J. Med. 373, 11–22 (2015).
Grannell, A. et al. Liraglutide does not adversely impact fat-free mass loss. Obesity 29, 529–534 (2021).
Richardson, T. G., Fang, S., Mitchell, R. E., Holmes, M. V. & Davey Smith, G. Evaluating the effects of cardiometabolic exposures on circulating proteins which may contribute to severe SARS-CoV-2. eBioMedicine 64, 103228 (2021).
Locke, A. E. et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 518, 197–206 (2015).
Pihlajamaki, J. et al. Expression of the splicing factor gene SFRS10 is reduced in human obesity and contributes to enhanced lipogenesis. Cell Metab. 14, 208–218 (2011).
Zhao, X. et al. FTO-dependent demethylation of N6-methyladenosine regulates mRNA splicing and is required for adipogenesis. Cell Res. 24, 1403–1419 (2014).
Roundtree, I. A., Evans, M. E., Pan, T. & He, C. Dynamic RNA modifications in gene expression regulation. Cell 169, 1187–1200 (2017).
Kim, M., Lee, C. & Park, J. Extracellular matrix remodeling facilitates obesity-associated cancer progression. Trends Cell Biol. 32, 825–834 (2022).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife 7, e34408 (2018).
Purcell, S. et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. 81, 559–575 (2007).
The 1000 Genomes Project Consortium. A global reference for human genetic variation. Nature 526, 68–74 (2015).
Deeks, J. J. et al. in Cochrane Handbook for Systematic Reviews of Interventions 2nd edn (eds Higgins, J. P. T. et al.) Ch. 10 (The Cochrane Collaboration, 2019).
Hemani, G., Bowden, J. & Davey Smith, G. Evaluating the potential role of pleiotropy in Mendelian randomization studies. Hum. Mol. Genet. 27, R195–R208 (2018).
Burgess, S., Bowden, J., Fall, T., Ingelsson, E. & Thompson, S. G. Sensitivity analyses for robust causal inference from mendelian randomization analyses with multiple genetic variants. Epidemiology 28, 30–42 (2017).
Pierce, B. L., Ahsan, H. & Vanderweele, T. J. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int. J. Epidemiol. 40, 740–752 (2011).
Giambartolomei, C. et al. Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. PLoS Genet. 10, e1004383 (2014).
Benner, C. et al. FINEMAP: efficient variable selection using summary data from genome-wide association studies. Bioinformatics 32, 1493–1501 (2016).
Huffman, J. E. et al. Multi-ancestry fine mapping implicates OAS1 splicing in risk of severe COVID-19. Nat. Genet. 54, 125–127 (2022).
Leek, J. T., Johnson, W. E., Parker, H. S., Jaffe, A. E. & Storey, J. D. The sva package for removing batch effects and other unwanted variation in high-throughput experiments. Bioinformatics 28, 882–883 (2012).
Hao, Y. et al. Integrated analysis of multimodal single-cell data. Cell 184, 3573–3587 (2021).
Carter, A. R. et al. Understanding the consequences of education inequality on cardiovascular disease: Mendelian randomisation study. BMJ 365, l1855 (2019).
Grant, A. J. & Burgess, S. Pleiotropy robust methods for multivariable Mendelian randomization. Stat. Med. 40, 5813–5830 (2021).
Vabistsevits, M. et al. Deciphering how early life adiposity influences breast cancer risk using Mendelian randomization. Commun. Biol. 5, 337 (2022).
Yoshiji, S. et al. Causal associations between body fat accumulation and COVID-19 severity: a Mendelian randomization study. Front. Endocrinol. 13, 899625 (2022).
Cichonska, A. et al. metaCCA: summary statistics-based multivariate meta-analysis of genome-wide association studies using canonical correlation analysis. Bioinformatics 32, 1981–1989 (2016).
Acknowledgements
We thank the COVID-19 Host Genetics Initiative for providing the latest summary statistics for COVID-19 outcomes. We acknowledge S. Wang, T. Khosroheidari, L. Cuddeback, W. Schwarzmann and D. Denmark at SomaLogic for constructive discussions. We acknowledge Biorender (biorender.com) for providing materials used to create the illustrative diagram. The Richards research group is supported by the Canadian Institutes of Health Research (grants 365825, 409511, 100558 and 169303), the McGill Interdisciplinary Initiative in Infection and Immunity (MI4), the Lady Davis Institute of the Jewish General Hospital, the Jewish General Hospital Foundation, the Canadian Foundation for Innovation, the National Institutes of Health Foundation, Genome Quebec, the Public Health Agency of Canada, McGill University, Cancer Research UK (grant no. C18281/A29019) and the Fonds de Recherche Quebec Santé (FRQS). J.B.R. is supported by an FRQS Mérite Clinical Research Scholarship. The support from Calcul Quebec and Compute Canada is acknowledged. TwinsUK is funded by the Welcome Trust, the Medical Research Council, the European Union, the National Institute for Health Research-funded BioResource and the Clinical Research Facility and Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust in partnership with King’s College London. S.Y. is supported by the Japan Society for the Promotion of Science. T.L. is supported by a Vanier Canada Graduate Scholarship, an FRQS doctoral training fellowship and a McGill University Faculty of Medicine Studentship. G.B.-L. is supported by scholarships from the FRQS, the Canadian Institutes of Health Research and Quebec’s Ministry of Health and Social Services. Y.C. is supported by an FRQS doctoral training fellowship and the Lady Davis Institute/TD Bank Studentship Award. M.H. is supported by grants from the SciLifeLab/Knut and Alice Wallenberg national COVID-19 research program (KAW 2020.0182 and KAW 2020.0241), the Swedish Heart-Lung Foundation (20210089, 20190639 and 20190637) and the Swedish Society of Medicine (SLS-938101). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conception and design was the responsibility of S.Y. and J.B.R. Methodology was overseen by S.Y., T.L. and J.B.R. Data analysis was performed by S.Y., T.L., J.D.S.W., C.-Y.S. and J.B.R. Visualization was conducted by S.Y. and T.L. Writing of the original draft was carried out by S.Y. Review and editing was carried out by S.Y., G.B.-L., T.L., J.D.S.W., C.-Y.S., T.N., D.R.M., Y.C., K.L., M.H., Y.I., Z.A., S.L., N.D., C.D., M.V., C.T., X.X., M.B., F.S., L.L., H.M.M., M.A., J.A., V.M., N.J.T., H.Z., S.Z., V.F., Y.F. and J.B.R.
Corresponding author
Ethics declarations
Competing interests
J.B.R. has served as an advisor to GlaxoSmithKline and Deerfield Capital. The institution of J.B.R. has received investigator-initiated grant funding from Eli Lilly, GlaxoSmithKline and Biogen for projects unrelated to this research. J.B.R. is the CEO of 5 Prime Sciences (www.5primesciences.com), which provides research services for biotech, pharma and venture capital companies for projects unrelated to this research. T.L. and V.F. are employees of 5 Prime Sciences. T.N. has received speaking fees from Boehringer Ingelheim and AstraZeneca regarding the projects unrelated to this research. The other authors declare no competing interests.
Peer review
Peer review information
Nature Metabolism thanks Shiu Lun Ryan Au Yeung and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Yanina-Yasmin Pesch, in collaboration with the Nature Metabolism team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Information.
Supplementary Tables
Supplementary Tables 1–22.
Source data
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data Fig. 8
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoshiji, S., Butler-Laporte, G., Lu, T. et al. Proteome-wide Mendelian randomization implicates nephronectin as an actionable mediator of the effect of obesity on COVID-19 severity. Nat Metab 5, 248–264 (2023). https://doi.org/10.1038/s42255-023-00742-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s42255-023-00742-w
This article is cited by
-
Evaluating metabolome-wide causal effects on risk for psychiatric and neurodegenerative disorders
BMC Medicine (2025)
-
Mendelian randomization analysis of blood metabolites and immune cell mediators in relation to GVHD and relapse
BMC Medicine (2025)
-
Investigating the potential of oxidative stress-related gene as predictive markers in idiopathic pulmonary fibrosis
Scientific Reports (2025)
-
Multiomic insight into the involvement of cell aging related genes in the pathogenesis of endometriosis
Scientific Reports (2025)
-
A cross-tissue transcriptome-wide association study identified susceptibility genes for age-related macular degeneration
Scientific Reports (2025)