Abstract
Current guidelines recommend hepatocellular carcinoma (HCC) surveillance for at-risk individuals, including individuals with hepatitis B virus infection. However, the performance and survival benefits of annual screening have not been evaluated through multicenter prospective studies in a Chinese population. Between 2017 and 2021, we included 14,426 participants with hepatitis B surface antigen seropositivity in an annual HCC screening study in China using a multicenter prospective design with ultrasonography and serum alpha-fetoprotein. After four rounds of screening and follow-up, the adjusted hazard ratios of death after correction for lead-time and length-time biases for screen-detected cancers at the prevalent and incident rounds were 0.74 (95% confidence interval = 0.60–0.91) and 0.52 (95% confidence interval = 0.40–0.68), respectively. A meta-analysis demonstrated that HCC screening was associated with improved survival after adjusting for lead-time bias. Our findings highlight the ‘real-world’ feasibility and effectiveness of annual HCC screening in community settings for the early detection of HCC and to improve survival.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated for the current study are not publicly available due to Chinese legal restrictions (Data Security Law of the People’s Republic of China), the willingness of other researchers and current ethical approval, but are available from the corresponding author (W.C.) upon reasonable request. All data from the systematic review and meta-analysis have been included in the main text and its source data files. All other data supporting the findings of this study are available from the corresponding author upon reasonable request. Source data are provided with this paper.
Code availability
All custom code used for these analyses is publicly available at https://github.com/ChangfaXia/HCCScreen/ without any restrictions. This includes the code for the meta-analysis, sojourn time estimation and bias correction, as appropriate. For the data analysis, R v.4.1.3 was used with base packages and the following additional packages: survival, ggplot2 and msm.
Change history
11 September 2023
A Correction to this paper has been published: https://doi.org/10.1038/s43018-023-00648-2
References
Rumgay, H. et al. Global, regional and national burden of primary liver cancer by subtype. Eur. J. Cancer 161, 108–118 (2022).
Zeng, H. et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Global Health 6, e555–e567 (2018).
Singal, A. G. et al. Hepatocellular carcinoma screening associated with early tumor detection and improved survival among patients with cirrhosis in the US. Am. J. Med. 130, 1099–1106 (2017).
Korean Liver Cancer Association, National Cancer Center. 2018 Korean Liver Cancer Association-National Cancer Center Korea Practice Guidelines for the management of hepatocellular carcinoma. Korean J. Radiol. 20, 1042–1113 (2019).
Galle, P. R. et al. EASL Clinical Practice Guidelines: management of hepatocellular carcinoma. J. Hepatol. 69, 182–236 (2018).
Marrero, J. A. et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 68, 723–750 (2018).
Omata, M. et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol. Int. 11, 317–370 (2017).
He, J. et al. China guideline for liver cancer screening (2022, Beijing). J. Clin. Hepatol. 38, 1739–1758 (2022).
Méndez-Sánchez, N. et al. Latin American Association for the Study of the Liver (LAASL) clinical practice guidelines: management of hepatocellular carcinoma. Ann. Hepatol. 13, S4–S40 (2014).
Poon, D. et al. Management of hepatocellular carcinoma in Asia: consensus statement from the Asian Oncology Summit 2009. Lancet Oncol. 10, 1111–1118 (2009).
Ronot, M. et al. Hepatocellular carcinoma surveillance with ultrasound-cost-effectiveness, high-risk populations, uptake. Br. J. Radiol. 91, 20170436 (2018).
Poustchi, H. et al. Feasibility of conducting a randomized control trial for liver cancer screening: is a randomized controlled trial for liver cancer screening feasible or still needed? Hepatology 54, 1998–2004 (2011).
Villanueva, A. Hepatocellular carcinoma. N. Engl. J. Med. 380, 1450–1462 (2019).
Zhang, B.-H., Yang, B.-H. & Tang, Z.-Y. Randomized controlled trial of screening for hepatocellular carcinoma. J. Cancer Res. Clin. Oncol. 130, 417–422 (2004).
Chen, J.-G. et al. Screening for liver cancer: results of a randomised controlled trial in Qidong, China. J. Med. Screen 10, 204–209 (2003).
Singal, A. G., Pillai, A. & Tiro, J. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med. 11, e1001624 (2014).
Kemp, W., Pianko, S., Nguyen, S., Bailey, M. J. & Roberts, S. K. Survival in hepatocellular carcinoma: impact of screening and etiology of liver disease. J. Gastroenterol. Hepatol. 20, 873–881 (2005).
Wong, G. L. et al. Surveillance programme for hepatocellular carcinoma improves the survival of patients with chronic viral hepatitis. Liver Int. 28, 79–87 (2008).
Bae, H. et al. Effectiveness of hepatocellular carcinoma surveillance and an optimal surveillance interval: nationwide cohort of Korea. Yonsei Med. J. 62, 758–766 (2021).
Kwon, J. W. et al. The impact of national surveillance for liver cancer: results from real-world setting in Korea. Gut Liver 14, 108–116 (2020).
van Meer, S. et al. Surveillance for hepatocellular carcinoma is associated with increased survival: results from a large cohort in the Netherlands. J. Hepatol. 63, 1156–1163 (2015).
Piñero, F. et al. Surveillance for hepatocellular carcinoma: does the place where ultrasound is performed impact its effectiveness? Dig. Dis. Sci. 64, 718–728 (2019).
Toyoda, H. et al. Impact of surveillance on survival of patients with initial hepatocellular carcinoma: a study from Japan. Clin. Gastroenterol. Hepatol. 4, 1170–1176 (2006).
Choi, D. T. et al. Hepatocellular carcinoma screening is associated with increased survival of patients with cirrhosis. Clin. Gastroenterol. Hepatol. 17, 976–987 (2019).
Taura, N. et al. Clinical benefits of hepatocellular carcinoma surveillance: a single-center, hospital-based study. Oncol. Rep. 14, 999–1003 (2005).
Ando, E. et al. Surveillance program for early detection of hepatocellular carcinoma in Japan: results of specialized department of liver disease. J. Clin. Gastroenterol. 40, 942–948 (2006).
Tanaka, H. et al. Surveillance of hepatocellular carcinoma in patients with hepatitis C virus infection may improve patient survival. Liver Int. 26, 543–551 (2006).
Kuo, Y. H. et al. Hepatocellular carcinoma surveillance and appropriate treatment options improve survival for patients with liver cirrhosis. Eur. J. Cancer 46, 744–751 (2010).
Tong, M. J. et al. Surveillance for hepatocellular carcinoma improves survival in Asian-American patients with hepatitis B: results from a community-based clinic. Dig. Dis. Sci. 55, 826–835 (2010).
Noda, I. et al. Regular surveillance by imaging for early detection and better prognosis of hepatocellular carcinoma in patients infected with hepatitis C virus. J. Gastroenterol. 45, 105–112 (2010).
El-Serag, H. B. et al. Effectiveness of AFP and ultrasound tests on hepatocellular carcinoma mortality in HCV-infected patients in the USA. Gut 60, 992–997 (2011).
Edenvik, P. et al. Application of hepatocellular carcinoma surveillance in a European setting. What can we learn from clinical practice? Liver Int. 35, 1862–1871 (2015).
Nusbaum, J. D. et al. The effect of hepatocellular carcinoma surveillance in an urban population with liver cirrhosis. J. Clin. Gastroenterol. 49, e91–95 (2015).
Thein, H. H. et al. Improved survival in patients with viral hepatitis-induced hepatocellular carcinoma undergoing recommended abdominal ultrasound surveillance in Ontario: a population-based retrospective cohort study. PLoS ONE 10, e0138907 (2015).
Wu, C. Y. et al. Association between ultrasonography screening and mortality in patients with hepatocellular carcinoma: a nationwide cohort study. Gut 65, 693–701 (2016).
Mittal, S. et al. Effectiveness of surveillance for hepatocellular carcinoma in clinical practice: a United States cohort. J. Hepatol. 65, 1148–1154 (2016).
Chaiteerakij, R. et al. Surveillance for hepatocellular carcinoma reduces mortality: an inverse probability of treatment weighted analysis. Ann. Hepatol. 16, 421–429 (2017).
Tong, M. J. et al. Long-term survival after surveillance and treatment in patients with chronic viral hepatitis and hepatocellular carcinoma. Hepatol. Commun. 1, 595–608 (2017).
Hong, T. P. et al. Surveillance improves survival of patients with hepatocellular carcinoma: a prospective population-based study. Med. J. Aust. 209, 348–354 (2018).
Lang, S. et al. Hepatocellular carcinoma surveillance with liver imaging is not associated with improved survival. Scand. J. Gastroenterol. 55, 222–227 (2020).
Haq, M. I. et al. Effect of hepatocellular carcinoma surveillance programmes on overall survival in a mixed cirrhotic UK population: a prospective, longitudinal cohort study. J. Clin. Med. 10, 2770 (2021).
Ji, M. et al. Mass screening for liver cancer: results from a demonstration screening project in Zhongshan City, China. Sci. Rep. 8, 12787 (2018).
Yeh, Y.-P. et al. Evaluation of abdominal ultrasonography mass screening for hepatocellular carcinoma in Taiwan. Hepatology 59, 1840–1849 (2014).
Chinese Society of Hepatology, Chinese Medical Association. Consensus on secondary prevention of primary liver cancer (2021 version) [article in Chinese]. Zhonghua Gan Zang Bing Za Zhi 29, 216–226 (2021).
Xiang, X. et al. Distribution of tumor stage and initial treatment modality in patients with primary hepatocellular carcinoma. Clin. Transl. Oncol. 19, 891–897 (2017).
Kapidzic, A. et al. Attendance and yield over three rounds of population-based fecal immunochemical test screening. Am. J. Gastroenterol. 109, 1257–1264 (2014).
Yousaf-Khan, U. et al. Final screening round of the NELSON lung cancer screening trial: the effect of a 2.5-year screening interval. Thorax 72, 48–56 (2017).
Horeweg, N. et al. Detection of lung cancer through low-dose CT screening (NELSON): a prespecified analysis of screening test performance and interval cancers. Lancet Oncol. 15, 1342–1350 (2014).
Nathani, P. et al. Hepatocellular carcinoma tumour volume doubling time: a systematic review and meta-analysis. Gut 70, 401–407 (2021).
Steele, R. J. et al. Interval cancers in a FOBT-based colorectal cancer population screening programme: implications for stage, gender and tumour site. Gut 61, 576–581 (2012).
Hardcastle, J. D. et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet 348, 1472–1477 (1996).
van der Vlugt, M. et al. Interval colorectal cancer incidence among subjects undergoing multiple rounds of fecal immunochemical testing. Gastroenterology 153, 439–447 (2017).
An, C. et al. Growth rate of early-stage hepatocellular carcinoma in patients with chronic liver disease. Clin. Mol. Hepatol. 21, 279–286 (2015).
Wang, J.-H. et al. Hepatocellular carcinoma surveillance at 4- vs. 12-month intervals for patients with chronic viral hepatitis: a randomized study in community. Am. J. Gastroenterol. 108, 416–424 (2013).
Bruix, J. & Sherman, M. Management of hepatocellular carcinoma: an update. Hepatology 53, 1020–1022 (2011).
Su, F. et al. Screening is associated with a lower risk of hepatocellular carcinoma-related mortality in patients with chronic hepatitis B. J. Hepatol. 74, 850–859 (2021).
Sheena, B. S. et al. Global, regional, and national burden of hepatitis B, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 7, 796–829 (2022).
Wang, M. et al. Contribution of hepatitis B virus and hepatitis C virus to liver cancer in China north areas: experience of the Chinese National Cancer Center. Int. J. Infect. Dis. 65, 15–21 (2017).
von Elm, E. et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335, 806–808 (2007).
Chinese Society of Ultrasound in Medicine, Oncology Intervention Committee of Chinese Research Hospital Society & National Health Commission Capacity Building and Continuing Education Expert Committee on Ultrasonic Diagnosis. Guideline for ultrasonic diagnosis of liver diseases [article in Chinese]. Zhonghua Gan Zang Bing Za Zhi 29, 385–402 (2021).
Bureau of Medical Administration & National Health and Family Planning Commission of the People’s Republic of China. Diagnosis, management, and treatment of hepatocellular carcinoma (V2017) [article in Chinese]. Zhonghua Gan Zang Bing Za Zhi 25, 886–895 (2017).
Edge, S. B. & Compton, C. C. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann. Surg. Oncol. 176, 1471–1474 (2010).
Duffy, S. W. et al. Correcting for lead time and length bias in estimating the effect of screen detection on cancer survival. Am. J. Epidemiol. 168, 98–104 (2008).
Jackson, C. Multi-state models for panel data: the msm package for R. J. Stat. Softw. 38, 1–28 (2011).
Akwiwu, E. U. et al. A progressive three-state model to estimate time to cancer: a likelihood-based approach. BMC Med. Res. Methodol. 22, 179 (2022).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339, b2700 (2009).
Schuch, F. B. et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am. J. Psychiatry 175, 631–648 (2018).
Acknowledgements
This study was supported by the National Natural Science Foundation of China (81974492 and 82273721), the Innovation Fund for Medical Sciences of the Chinese Academy of Medical Sciences (2021-I2M-1-066) and the Sanming Project of Medicine in Shenzhen (SZSM201911015). The funders had no role in study design, data collection, data analysis, data interpretation, writing of the final manuscript or the decision to publish. We gratefully acknowledge the cooperation of all involved staff affiliated with cancer registries and the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Contributions
H. Zeng, C.Q. and W.C. designed the study and interpreted the data. H. Zeng wrote the first draft of the manuscript. C.X. and M.C. had primary responsibility for applying the analytical methods to produce estimates and create the figures and tables. H. Zeng and M.C. had primary responsibility for seeking, extracting and cleaning the data. C.Q., D.W., K.C., Z.Z., S.Z., J.Z., H.D., X.Q., S.D., Y.C., Z.S., H.D., Q.L. and H. Zhao conducted the technical implementation and monitored the clinical conduct of the study. M.C. and R.F. carried out the systematic review and meta-analysis. J.M., J.S.J., X.Z., X.Y. and F.S. provided critical feedback on the methods or results. W.C., H. Zeng and C.Q. had full access to all the data in the study. All authors reviewed the final manuscript draft and agreed with its content and conclusions.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks Jörn Schattenberg and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 The flowchart of the study.
a, The flowchart of the HCC screening cohort. b, The flowchart of the systematic review and meta-analysis.
Extended Data Fig. 2 Detection rates and early-detection rates of HCC.
a, Detection rate for all participants (n = 327 patients). b, Detection rate for men (n = 239 patients). c, Detection rate for women (n = 88 patients). d, Early-detection rate for all participants (n = 327 patients). e, Early-detection rate for men (n = 239 patients). f, Early-detection rate for women (n = 88 patients). g, Detection rates in cirrhotic and non-cirrhotic participants (n = 327 patients).
Extended Data Fig. 3 Subgroup analyses of screening effectiveness.
a, Stage-specific survival for screen-detected cancers with known stage at diagnosis (n = 323 patients). b, Association between screening and effectiveness of overall survival. Data are displayed as the hazard ratio ±95% CI (screening group n = 327 patients, control group n = 1,446 patients).
Extended Data Fig. 4 Sensitivity analyses of the meta-analysis.
a, Influence analysis by exclusion of one study at a time. Data are displayed as the hazard ratio ±95% CI (n = 27 studies). b, Influence analysis by exclusion of one study adjusted for lead-time bias at a time. Data are displayed as the hazard ratio ±95% CI (n = 13 studies). c, Funnel plot for assessment of publication bias (n = 28 studies). Data are displayed as the hazard ratio and standard error of log hazard ratio.
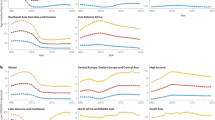
Extended Data Fig. 5 Subgroup analyses of the meta-analysis.
a, Subgroup analysis by screening interval (A). interval <12 months & ≥12 months. (B) interval <12 months alone. (C). interval ≥12 months alone. b, Subgroup analysis by etiology of HCC (A). HBV only. (B). HCV only. (C). HBV/HCV. Data are displayed as the hazard ratio ± 95% CI (n = 28 studies).
Supplementary information
Supplementary Tables
Supplementary Tables 1–9.
Source data
Source Data Fig. 1
Data for the screening performance of the HCC screening cohort.
Source Data Fig. 2
Survival data in patients with HCC with or without screening.
Source Data Fig. 3
Data for the forest plot showing the pooled estimates. a, Survival. b, Survival adjusted for lead-time bias.
Source Data Extended Data Fig.1
Data for the flowchart. a, Flowchart of the HCC screening cohort. b, Flowchart of the systematic review and meta-analysis.
Source Data Extended Data Fig. 2
Data for the detection and early detection rates of HCC. a, Detection rate for all participants. b, Detection rate for men. c, Detection rate for women. d, Early detection rate for all participants. e, Early detection rate for men. f, Early detection rate for women. g, Detection rates in participants with and without cirrhosis.
Source Data Extended Data Fig. 3
Data for the subgroup analyses of screening effectiveness. a, Stage-specific survival for patients with screen-detected cancers with known stage at diagnosis. b, Association between screening and effectiveness of overall survival.
Source Data Extended Data Fig. 4
Data for the sensitivity analyses of the meta-analysis. a, Influence analysis by exclusion of one study at a time. b, Influence analysis by exclusion of one study at a time, adjusted for lead-time bias. c, Funnel plot to assess publication bias.
Source Data Extended Data Fig. 5
Data for the subgroup analyses of the meta-analysis. a, Subgroup analysis according to screening interval. Interval <12 months and ≥12 months (A). Interval <12 months alone (B). Interval ≥12 months alone (C). b, Subgroup analysis according to the etiology of HCC. HBV only (A). HCV only (B). HBV/HCV (C).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zeng, H., Cao, M., Xia, C. et al. Performance and effectiveness of hepatocellular carcinoma screening in individuals with HBsAg seropositivity in China: a multicenter prospective study. Nat Cancer 4, 1382–1394 (2023). https://doi.org/10.1038/s43018-023-00618-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-023-00618-8
This article is cited by
-
Lenvatinib and tislelizumab versus atezolizumab and bevacizumab in combination with TAE-HAIC for unresectable hepatocellular carcinoma with high tumor burden: a multicenter retrospective cohort study
Cancer Immunology, Immunotherapy (2025)
-
Identification of the entosis-related prognostic signature and tumour microenvironment in hepatocellular carcinoma on the basis of bioinformatics analysis and experimental validation
Clinical and Experimental Medicine (2025)
-
[68Ga]Ga-PSMA-617 PET/MRI for imaging patients suspected of hepatocellular carcinoma
European Journal of Nuclear Medicine and Molecular Imaging (2025)
-
PD-L1+ neutrophils induced NETs in malignant ascites is a potential biomarker in HCC
Cancer Immunology, Immunotherapy (2024)