Abstract
Extracellular vesicles (EVs) transport biomolecules that mediate intercellular communication. We previously showed that EVs contain DNA (EV-DNA) representing the entire genome. However, the mechanism of genomic EV-DNA packaging and its role in cancer remain elusive. We now demonstrate that EV-DNA is predominantly localized on the vesicle surface and associated with uniquely modified and cleaved histones. Moreover, a genome-wide clustered regularly interspaced short palindromic repeats knockout screen revealed that immune developmental pathways and genes, including apoptotic peptidase activating factor 1 (APAF1) and neutrophil cytosolic factor 1 (NCF1), regulate EV-DNA packaging. Furthermore, in colorectal cancer models, uptake of EV-DNA by pre-metastatic liver Kupffer cells (KCs) activated DNA damage responses. This activation rewired KC cytokine production and promoted the formation of tertiary lymphoid structures, thereby suppressing liver metastasis. Conversely, loss of APAF1 decreased EV-DNA packaging and promoted liver metastasis. Importantly, colorectal cancer biopsy EV-DNA secretion could serve as a predictive biomarker for postoperative metastasis. Taken together, our findings indicate that uniquely chromatinized EV-DNA induces antitumor immunity.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
Raw sequencing data can be found on the Sequence Read Archive (PRJNA1072813), including whole-genome sequencing, DNA sequencing for the CRISPR screen and RNA sequencing. The proteomics data were deposited to the ProteomeXchange Consortium through the PRIDE partner repository under dataset identifiers PXD056104 (PTM MS proteomics data of histones from cells and EVs) and PXD056026 (MS proteomics data for HCT116 and MDA-MB-231 EVs). Uncropped western blot images and raw data for all main and extended data figures have been provided in the Source Data files. All other data supporting the findings of this study are available from the corresponding authors on reasonable request. Source data are provided with this paper.
Code availability
No custom code was generated in the course of this study.
References
Zijlstra, A. & Di Vizio, D. Size matters in nanoscale communication. Nat. Cell Biol. 20, 228–230 (2018).
Zhang, H. et al. Identification of distinct nanoparticles and subsets of extracellular vesicles by asymmetric flow field-flow fractionation. Nat. Cell Biol. 20, 332–343 (2018).
Zhang, Q. et al. Transfer of functional cargo in exomeres. Cell Rep 27, 940–954 (2019).
Jeppesen, D. K. et al. Reassessment of exosome composition. Cell 177, 428–445 (2019).
Lucotti, S., Kenific, C. M., Zhang, H. & Lyden, D. Extracellular vesicles and particles impact the systemic landscape of cancer. EMBO J. 41, e109288 (2022).
Costa-Silva, B. et al. Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver. Nat. Cell Biol. 17, 816–826 (2015).
Rodrigues, G. et al. Tumour exosomal CEMIP protein promotes cancer cell colonization in brain metastasis. Nat. Cell Biol. 21, 1403–1412 (2019).
Peinado, H. et al. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat. Med. 18, 883–891 (2012).
Hoshino, A. et al. Tumour exosome integrins determine organotropic metastasis. Nature 527, 329–335 (2015).
Abdouh, M. et al. Exosomes isolated from cancer patients’ sera transfer malignant traits and confer the same phenotype of primary tumors to oncosuppressor-mutated cells. J. Exp. Clin. Cancer Res. 36, 113 (2017).
Clancy, J. W., Sheehan, C. S., Boomgarden, A. C. & D’Souza-Schorey, C. Recruitment of DNA to tumor-derived microvesicles. Cell Rep. 38, 110443 (2022).
Kahlert, C. et al. Identification of double-stranded genomic DNA spanning all chromosomes with mutated KRAS and P53 DNA in the serum exosomes of patients with pancreatic cancer. J. Biol. Chem. 289, 3869–3875 (2014).
Thakur, B. K. et al. Double-stranded DNA in exosomes: a novel biomarker in cancer detection. Cell Res. 24, 766–769 (2014).
Fischer, S. et al. Indication of horizontal DNA gene transfer by extracellular vesicles. PLoS ONE 11, e0163665 (2016).
Lazaro-Ibanez, E. et al. DNA analysis of low- and high-density fractions defines heterogeneous subpopulations of small extracellular vesicles based on their DNA cargo and topology. J. Extracell. Vesicles 8, 1656993 (2019).
Maire, C. L. et al. Genome-wide methylation profiling of glioblastoma cell-derived extracellular vesicle DNA allows tumor classification. Neuro Oncol. 23, 1087–1099 (2021).
Nemeth, A. et al. Antibiotic-induced release of small extracellular vesicles (exosomes) with surface-associated DNA. Sci. Rep. 7, 8202 (2017).
Choi, D. et al. Mapping subpopulations of cancer cell-derived extracellular vesicles and particles by nano-flow cytometry. ACS Nano 13, 10499–10511 (2019).
Fernando, M. R., Jiang, C., Krzyzanowski, G. D. & Ryan, W. L. New evidence that a large proportion of human blood plasma cell-free DNA is localized in exosomes. PLoS ONE 12, e0183915 (2017).
Lazaro-Ibanez, E. et al. Different gDNA content in the subpopulations of prostate cancer extracellular vesicles: apoptotic bodies, microvesicles, and exosomes. Prostate 74, 1379–1390 (2014).
Torralba, D. et al. Priming of dendritic cells by DNA-containing extracellular vesicles from activated T cells through antigen-driven contacts. Nat. Commun. 9, 2658 (2018).
Vagner, T. et al. Large extracellular vesicles carry most of the tumour DNA circulating in prostate cancer patient plasma. J. Extracell. Vesicles 7, 1505403 (2018).
Bernard, V. et al. Circulating nucleic acids are associated with outcomes of patients with pancreatic cancer. Gastroenterology 156, 108–118 (2019).
Yang, S. et al. Detection of mutant KRAS and TP53 DNA in circulating exosomes from healthy individuals and patients with pancreatic cancer. Cancer Biol. Ther. 18, 158–165 (2017).
Choi, J. et al. Detection of circulating KRAS mutant DNA in extracellular vesicles using droplet digital PCR in patients with colon cancer. Front. Oncol. 12, 1067210 (2022).
Cai, J. et al. SRY gene transferred by extracellular vesicles accelerates atherosclerosis by promotion of leucocyte adherence to endothelial cells. Clin. Sci. (Lond.) 129, 259–269 (2015).
Sansone, P. et al. Packaging and transfer of mitochondrial DNA via exosomes regulate escape from dormancy in hormonal therapy-resistant breast cancer. Proc. Natl Acad. Sci. USA 114, E9066–E9075 (2017).
Ghanam, J. et al. Extracellular vesicles transfer chromatin-like structures that induce non-mutational dysfunction of p53 in bone marrow stem cells. Cell Discov. 9, 12 (2023).
Lian, Q. et al. Chemotherapy-induced intestinal inflammatory responses are mediated by exosome secretion of double-strand DNA via AIM2 inflammasome activation. Cell Res. 27, 784–800 (2017).
Kitai, Y. et al. DNA-containing exosomes derived from cancer cells treated with topotecan activate a STING-dependent pathway and reinforce antitumor immunity. J. Immunol. 198, 1649–1659 (2017).
Diamond, J. M. et al. Exosomes shuttle TREX1-sensitive IFN-stimulatory dsDNA from irradiated cancer cells to DCs. Cancer Immunol. Res. 6, 910–920 (2018).
Sisquella, X. et al. Malaria parasite DNA-harbouring vesicles activate cytosolic immune sensors. Nat. Commun. 8, 1985 (2017).
Tsilioni, I. & Theoharides, T. C. Extracellular vesicles are increased in the serum of children with autism spectrum disorder, contain mitochondrial DNA, and stimulate human microglia to secrete IL-1β. J. Neuroinflammation 15, 239 (2018).
Takahashi, A. et al. Exosomes maintain cellular homeostasis by excreting harmful DNA from cells. Nat. Commun. 8, 15287 (2017).
Yokoi, A. et al. Mechanisms of nuclear content loading to exosomes. Sci. Adv. 5, eaax8849 (2019).
Simpson, R. T. Structure of chromatin containing extensively acetylated H3 and H4. Cell 13, 691–699 (1978).
Santos-Rosa, H. et al. Histone H3 tail clipping regulates gene expression. Nat. Struct. Mol. Biol. 16, 17–22 (2009).
Yi, S. J. & Kim, K. Histone tail cleavage as a novel epigenetic regulatory mechanism for gene expression. BMB Rep. 51, 211–218 (2018).
Zhou, P., Wu, E., Alam, H. B. & Li, Y. Histone cleavage as a mechanism for epigenetic regulation: current insights and perspectives. Curr. Mol. Med. 14, 1164–1172 (2014).
Ahn, B. K., Kim, S. H., Paik, S. S. & Lee, K. H. Loss of APAF-1 expression is associated with early recurrence in stage I, II, and III colorectal cancer. Langenbecks Arch. Surg. 401, 1203–1210 (2016).
Pelissier Vatter, F. A. et al. Extracellular vesicle- and particle-mediated communication shapes innate and adaptive immune responses. J. Exp. Med. 218, e20202579 (2021).
Li, J. et al. Tumor cell-intrinsic factors underlie heterogeneity of immune cell infiltration and response to immunotherapy. Immunity 49, 178–193 (2018).
Wang, G. et al. Tumour extracellular vesicles and particles induce liver metabolic dysfunction. Nature 618, 374–382 (2023).
Kasapi, A. & Triantafyllopoulou, A. Genotoxic stress signalling as a driver of macrophage diversity. Cell Stress 6, 30–44 (2022).
Braumüller, H. et al. The cytokine network in colorectal cancer: implications for new treatment strategies. Cells 12, 138 (2022).
Chang, H. W. et al. Mechanism of FACT removal from transcribed genes by anticancer drugs curaxins. Sci. Adv. 4, eaav2131 (2018).
Petitprez, F. et al. B cells are associated with survival and immunotherapy response in sarcoma. Nature 577, 556–560 (2020).
Helmink, B. A. et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature 577, 549–555 (2020).
Cabrita, R. et al. Tertiary lymphoid structures improve immunotherapy and survival in melanoma. Nature 577, 561–565 (2020).
Biller, L. H. & Schrag, D. Diagnosis and treatment of metastatic colorectal cancer: a review. JAMA 325, 669–685 (2021).
Hugen, N., van de Velde, C. J. H., de Wilt, J. H. W. & Nagtegaal, I. D. Metastatic pattern in colorectal cancer is strongly influenced by histological subtype. Ann. Oncol. 25, 651–657 (2014).
Ponten, F., Jirstrom, K. & Uhlen, M. The Human Protein Atlas—a tool for pathology. J. Pathol. 216, 387–393 (2008).
Xiao, W. et al. Roles and clinical significances of ATF6, EMC6, and APAF1 in prognosis of pancreatic cancer. Front. Genet. 12, 730847 (2021).
Zou, H., Henzel, W. J., Liu, X., Lutschg, A. & Wang, X. APAF-1, a human protein homologous to C. elegans CED-4, participates in cytochrome c-dependent activation of caspase-3. Cell 90, 405–413 (1997).
Jagot-Lacoussiere, L. et al. DNA damage-induced nuclear translocation of APAF-1 is mediated by nucleoporin Nup107. Cell Cycle 14, 1242–1251 (2015).
Ferraro, E. et al. APAF1 plays a pro-survival role by regulating centrosome morphology and function. J. Cell Sci. 124, 3450–3463 (2011).
Dillekas, H., Rogers, M. S. & Straume, O. Are 90% of deaths from cancer caused by metastases? Cancer Med. 8, 5574–5576 (2019).
Zeng, D. et al. Immunosuppressive microenvironment revealed by immune cell landscape in pre-metastatic liver of colorectal cancer. Front. Oncol. 11, 620688 (2021).
Kaczanowska, S. et al. Genetically engineered myeloid cells rebalance the core immune suppression program in metastasis. Cell 184, 2033–2052 (2021).
Awad, R. M., De Vlaeminck, Y., Maebe, J., Goyvaerts, C. & Breckpot, K. Turn back the TIMe: targeting tumor infiltrating myeloid cells to revert cancer progression. Front. Immunol. 9, 1977 (2018).
Labani-Motlagh, A., Ashja-Mahdavi, M. & Loskog, A. The tumor microenvironment: a milieu hindering and obstructing antitumor immune responses. Front. Immunol. 11, 940 (2020).
Zhang, Y. & Zhang, Z. The history and advances in cancer immunotherapy: understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell. Mol. Immunol. 17, 807–821 (2020).
Bojmar, L. et al. Extracellular vesicle and particle isolation from human and murine cell lines, tissues, and bodily fluids. STAR Protoc. 2, 100225 (2021).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 25, 402–408 (2001).
Bojmar, L. et al. Protocol for cross-platform characterization of human and murine extracellular vesicles and particles. STAR Protoc. 5, 102754 (2024).
Qian, B. Z. et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature 475, 222–225 (2011).
Kang, W. et al. Multiplex spatial protein detection by combining immunofluorescence with immunohistochemistry. Methods Mol. Biol. 2593, 233–244 (2023).
Liu, Z., Gu, Y., Shin, A., Zhang, S. & Ginhoux, F. Analysis of myeloid cells in mouse tissues with flow cytometry. STAR Protoc. 1, 100029 (2020).
Joung, J. et al. Genome-scale CRISPR–Cas9 knockout and transcriptional activation screening. Nat. Protoc. 12, 828–863 (2017).
Shechter, D., Dormann, H. L., Allis, C. D. & Hake, S. B. Extraction, purification and analysis of histones. Nat. Protoc. 2, 1445–1457 (2007).
Sidoli, S. & Garcia, B. A. Characterization of individual histone posttranslational modifications and their combinatorial patterns by mass spectrometry-based proteomics strategies. Methods Mol. Biol. 1528, 121–148 (2017).
Sidoli, S., Bhanu, N. V., Karch, K. R., Wang, X. & Garcia, B. A.Complete workflow for analysis of histone post-translational modifications using bottom-up mass spectrometry: from histone extraction to data analysis. J. Vis. Exp. 111, e54112 (2016).
Sidoli, S., Simithy, J., Karch, K. R., Kulej, K. & Garcia, B. A. Low resolution data-independent acquisition in an LTQ-Orbitrap allows for simplified and fully untargeted analysis of histone modifications. Anal. Chem. 87, 11448–11454 (2015).
Zhou, Y. et al. Metascape provides a biologist-oriented resource for the analysis of systems-level datasets. Nat. Commun. 10, 1523 (2019).
Bu, D. et al. KOBAS-i: intelligent prioritization and exploratory visualization of biological functions for gene enrichment analysis. Nucleic Acids Res. 49, W317–W325 (2021).
Acknowledgements
We acknowledge the Genomics Resource Core Facility (Weill Cornell Medicine), Electron Microscopy and Histology Core Facility (Weill Cornell Medicine) and Molecular Cytology Core Facility (Memorial Sloan Kettering Cancer Center, MSKCC) for their high-quality service. We also acknowledge support from T. Miller and M. Lima Silva Santos with flow cytometry and cell sorting. We thank members of the Lyden laboratory for insightful discussions. We gratefully acknowledge support from the National Cancer Institute (CA224175 (D.L.), CA210240 (D.L.), CA232093 (D.L.), CA207983 (D.L.), CA169538 (D.L.) and CA218513 (D.L. and H.Z.)), the Malcolm Hewitt Weiner Foundation, the Manning Foundation, the Hartwell Foundation and the Children’s Cancer and Blood Foundation (all to D.L.), the Beth C. Tortolani Foundation, Lerner Foundation, Gitty Leiner Fund, Sussman Family Fund and MSKCC core grant P30 CA008748 (all to J.B.), a Research Assistance for Primary Parents grant from the Mastercard Diversity–Mentorship Collaborative at Weill Cornell Medicine and Worldwide Cancer Research WRC 23-0105 (I.W.), a National Research Foundation of Korea grant funded by the Korean government (MSIT) (2022R1A2C4001879 to H.S.K.), a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI22C0353 and RS-2023-00304686 to H.S.K. and HI19C1330 to D.K.), the Bio & Medical Technology Development Program of the National Research Foundation (NRF) & funded by the Korean government (Ministry of Science and ICT) (2022M3A9F3016364 to H.S.K.), the Hankookilbo Myung-Ho Seung Faculty Research Assistance Program of Yonsei University College of Medicine (6-2023-0172 to H.S.K.), Institute for Project-Y funded by Yonsei University (H.S.K.), a research grant (H.S.K.) funded by the CKDBiO-YONSEI Microbiome Research Center (CYMRC) and the Alchemist Project through the Korean Ministry of Trade, Industry and Energy (20012443 to H.S.K.). The Y.D. Lab is supported by the Josie Robertson Foundation, the Pershing Square Sohn Cancer Research Alliance, the National Institutes of Health (CCSG core Grant No. P30 CA008748, MSK SPORE P50 CA192937 and R35 GM138386), the Parker Institute for Cancer Immunotherapy, the STARR Cancer Alliance award and the Anna Fuller Trust. In addition, the Y.D. lab is supported by W. H. Goodwin, A. Goodwin, the Commonwealth Foundation for Cancer Research and the Center for Experimental Therapeutics at MSKCC. Several illustrations for this manuscript were created with BioRender.com.
Author information
Authors and Affiliations
Contributions
I.W. designed the experimental approach, performed the experimental work, analyzed the data, coordinated the project and wrote the manuscript. Y.S., I.A., L.S., G.C.T., J.H., K.-A.K., D.K., S.D., Y.L., G.A., M.C., T.H., M.Z.T., A.K. and R.M. performed experimental work. K.E.J. performed and analyzed the whole-genome sequencing. Y.D.H., D.H.H., S.P., J.-S.S., M.J., J.Y.P. and M.G.L. provided patient samples. M.V.R., D.Z., J.B. and S.M. generated APAF1 KO in murine cells. S.S. performed and analyzed the PTM MS for histones. K.M. and B.K.T. gave feedback on the project. R.E.S., N.B., I.M. and H.Z. read the manuscript and gave feedback on the project. J.B. and Y.D. designed the experimental approach, read the manuscript and gave feedback on the project. H.S.K. designed the experimental approach, analyzed the data and wrote the manuscript. D.L. coordinated and designed the experimental approach, coordinated the project, interpreted the data and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
D.L. is on the scientific advisory board of Aufbau Holdings. R.E.S. is on the scientific advisory board of Miromatrix and is a speaker and consultant for Alnylam. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks Lei Qi, Janusz Rak and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Inclusion and diversity statement We support inclusive, diverse, and equitable conduct of research.
Extended data
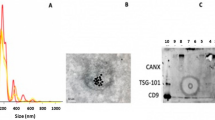
Extended Data Fig. 1 EV-DNA originates from genomic DNA.
(a,b) A549 and K562 EVs were treated with or without DNase 0, and EV-DNA was extracted. (a) EV-DNA was quantified using Qubit3 and normalized to EV protein content. Data are mean ± s.e.m., analyzed using a two-tailed, unpaired Student’s t-test, with n = 4 independent experiments per group. (b) EV-DNA was analyzed using chip-based capillary electrophoresis (Bioanalyzer). The data are representative of n = 3 independent experiments. (c) HCT116 cells were treated with 1 ug/ml puromycin for 24 h to induce apoptosis, with untreated cells as a control. Lysates were prepared from cells and the indicated EVs and analyzed by Western blot using the indicated antibodies. (d) Fragment coverage for paired-end whole genome sequencing (WGS) of EV-DNA (with or without DNase 0) and gDNA in HCT116 and MDA-MB-231 cells. Each box represents one chromosome, and the y-axis shows relative read count abundance along the genome.
Extended Data Fig. 2 APAF1 and NCF1 regulate EV-DNA packaging.
(a-b) EVs were isolated from control and APAF1 KO cells. (a) Mode diameter of EVs by nanoparticle tracking analysis. Data are mean ± s.e.m., analyzed using a two-tailed, unpaired Student’s t-test, with n = 4 independent experiments for HCT116 and n = 3 independent experiments for MDA-MB-231. (b) EVs protein amount (μg) was measured by BCA analysis and normalized to cell number at the time of collection. Data are mean ± s.e.m., analyzed using a two-tailed, unpaired Student’s t-test, with n = 6 independent experiments for HCT116 and n = 5 independent experiments for MDA-MB-231. (c) Venn diagram showing unique and overlapping proteins identified by MS/MS between control and APAF1 KO EVs in each cell line. (d-g) EVs were isolated from control and NCF1 KO cells. (d) Transmission electron microscopy for EVs, representative of n = 3 independent experiments. Scale bar: 200 nm. (e) Mode diameter of EVs by nanoparticle tracking analysis. Data are mean ± s.e.m., analyzed using a two-tailed, unpaired Student’s t-test, with n = 4 independent experiments for HCT116 and n = 3 independent experiments for MDA-MB-231 from independent experiments. (f) EVs protein amount (μg) was measured by BCA analysis and normalized to cell number at the time of collection. Data are mean ± s.e.m., analyzed using a two-tailed, unpaired Student’s t-test, with n = 6 independent experiments for HCT116 and n = 5 independent experiments for MDA-MB-231 from independent experiments. (g) EV-DNA was extracted and quantified using Qubit3, normalized to EV protein content. Data are mean ± s.e.m., analyzed using a two-tailed, unpaired Student’s t-test, with n = 5 independent experiments per group. (h) Genomic DNA and EV-DNA were isolated from HCT116 or MDA-MB-231 cells expressing control or NCF1 KO sgRNAs. qPCR was used to detect sgRNA levels in gDNA and EV-DNA and normalized to control sgRNA sequence in gDNA. Data are mean ± s.e.m., analyzed using a two-tailed, unpaired Student’s t-test, n = 5 independent experiments per group from independent experiments. (i) Validation of APAF1 knockdown in NCF1 KO cell lines, the data represent two independent experiments. (j) EV-DNA was extracted from EVs derived from the indicated cell lines. Data are mean ± s.e.m., analyzed using a two-tailed, unpaired Student’s t-test, with n = 4 independent experiments per group.
Extended Data Fig. 3 Education of NSG mice with HCT116 EVs has no effect on metastasis formation.
(a) Gating strategy for GFP-positive cells. (b-g) NOD.Cg mice were educated 3 times a week for 3 weeks with 10 μg of EVs (Control or APAF1 KO) from HCT116 cells, or PBS, followed by intra-splenically injection of control GFP-Luc-labeled cells (5×104/mouse). Tumors were allowed to grow for 3-4 weeks with continued education. Experiments were performed twice in male and female mice. (b) Schematics of the education experiment. (c) Representative image of tumors in the spleen. (d) Tumor weight in grams. Data are mean ± s.e.m., analyzed by one-way ANOVA (n = 8 mice per Con group, n = 8 mice per PBS group, and n = 9 mice per KO group from n = 2 independent experiments). (e) Representative IVIS images. (f) Quantification of IVIS data. Data are mean ± s.e.m., analyzed by one-way ANOVA (n = 9 mice per Con group, n = 10 mice per KO group, and n = 10 mice per PBS group, from n = 2 independent experiments). (g) One liver lobe per mouse was analyzed by flow cytometry for GFP-positive cells. Data are mean ± s.e.m., one-way ANOVA (n = 9 mice per Con group, n = 11 mice per KO group, and n = 9 mice per PBS group from n = 2 independent experiments). (h-l) NSG mice educated 3 times a week for 3 weeks with 10 µg of EVs (Control or KO) from HCT116 cells, or PBS, were then intra-splenically injected with APAF1 KO cells (5×104/mouse) labeled with GFP-Luc. Tumors were allowed to grow for 3-4 weeks with continued education. The experiment was performed with 5 mice per group from one experiment in female mice. (h) Representative image of tumors in the spleen. (i) Tumor weight in grams. Data are mean ± s.e.m., analyzed by one-way ANOVA, with n = 5 mice per group from one experiment. (j) Representative IVIS images. (k) Quantification of IVIS data. Data are mean ± s.e.m., analyzed by one-way ANOVA, with n = 5 mice per group from one experiment. (l) One liver lobe per mouse was digested and analyzed by flow cytometry for GFP-positive cells. Data are mean ± s.e.m., analyzed by one-way ANOVA, with n = 5 mice per group from one experiment.
Extended Data Fig. 4 Generation of APAF1 KO in murine cancer cells.
(a-f) APAF1 was knocked out in CT26 cells, and EVs were isolated from control and APAF1 KO CT26 cells. (a) Total cell extracts were prepared from WT and APAF1 KO cells, and the lysates were analyzed by Western blot using the indicated antibodies. (b) EVs were analyzed by transition electron microscopy (TEM). Scale bar: 200 nm. (c) Nanoparticle tracking analysis; the histogram represents 3 independent readings per EV sample and cell type. (d) EV protein content was measured using BCA analysis and normalized to the number of cells at the time of collection. Data are mean ± s.e.m., analyzed using a two-tailed, unpaired Student’s t-test, with n = 3 independent experiments per group. (e) EV-DNA was extracted and quantified using Qubit3, normalized to EV protein content. Data are mean ± s.e.m., analyzed by two-tailed, unpaired Student’s t-test, with n = 3 independent experiments per group. (f) EV-DNA was analyzed using chip-based capillary electrophoresis (Bioanalyzer). (g-l) APAF1 was knocked out in KPC cells, and EVs were isolated from control and APAF1 KO KPC cells. (g) Total cell extracts were prepared from WT and APAF1 KO cells, and the lysates were analyzed by Western blot using the indicated antibodies. (h) EVs were visualized by transition electron microscopy. Scale bar: 200 nm. (i) Nanoparticle tracking analysis; the histogram represents 3 independent readings per EV sample and cell type. (j) EV protein content (mg) was measured by BCA analysis and normalized to the number of cells at the time of collection. Data are mean ± s.e.m., analyzed by a two-tailed, unpaired Student’s t-test, with n = 10 per cell type from 5 independent experiments. (k) EV-DNA was extracted and quantified using Qubit3, normalized to protein content. Data are mean ± s.e.m., analyzed by two-tailed, unpaired Student’s t-test, with n = 7 per cell type from 4 independent experiments. (l) EV-DNA was analyzed using chip-based capillary electrophoresis (Bioanalyzer).
Extended Data Fig. 5 Reduced EV-DNA induces pro-tumor programming in KCs.
(a) Gating strategy for immune cell populations in the liver. (b) Percentages of EV+CD31+ cells. Data are mean ± s.e.m., analyzed by one-way ANOVA, with n = 6 mice per group from two independent experiments. (c-d) RNA sequencing analysis of Kupffer cells (KCs) isolated from n = 4 mice per group from two independent experiments after treatment with CT26 control or APAF1 KO EVs. (c) Gene Set Enrichment Analysis (GSEA) of pathways enriched in KCs treated with control or APAF1 KO EVs. (d) Pathway analysis highlighting those pathways upregulated in KCs from mice treated with APAF1 KO EVs compared to control EV-treated mice.
Extended Data Fig. 6 EV-DNA is damaged and induces cytokines secretion from KCs.
(a) Total protein was extracted from HCT116 and CT26 cells and EVs. The extracts (5 μg) were analyzed by Western blot for the indicated proteins. Data are representative of n = 2 independent experiments. (b) Primary KCs were isolated from the livers of naïve mice, plated in 48-well plates, and allowed to adhere for 16-24 hr. The KCs were then treated with the LPS (1 mg/ml) or control EVs (10 µg) for 24 h, after which cytokines secreted in the media were quantified (LegendPlex assay). Data summarize n = 2 independent repeats. (c) Balb/c mice were educated 3 times per week for 3 weeks with 10 µg of EVs (control or APAF1 KO) derived from CT26 cells or PBS. One liver lobe from each mouse was used for flow cytometric analysis of immune cell populations in the liver. Data are mean ± s.e.m., analyzed by one-way ANOVA, with n = 3 mice per group from one experiment. (d) Balb/c mice were educated 3 times per week for 3 weeks with 10 µg of EVs derived from CT26 cells. The liver was extracted and stained for analysis. Left panel: A representative liver section stained with multiplex immunofluorescence, showing B cells (B220, green), T cells (CD3, white), dendritic cells (CD11c, red), and DAPI (blue). Right panel: Following IF imaging, coverslips were removed, and immunohistochemistry staining for vWF was performed. Scale bar: 250 µm. Data represent n = 3 independent experiments.
Supplementary information
Supplementary Tables
Supplementary Table 1: sgRNA sequences and corresponding read counts from the genome-wide CRISPR KO screen. Supplementary Table 2: List of genes ranked by the top 10% of sgRNAs identified from genome-wide CRISPR KO screening in MDA-MB-231, HCT116, A549 and K562 cells. Supplementary Table 3: Pathway analysis of the top candidate genes associated with the regulation or inhibition of EV-DNA packaging, identified from the genome-wide CRISPR screen. Supplementary Table 4: List of 612 genes, 6,410 sgRNA sequences and corresponding read counts obtained from next-generation sequencing of EV-DNA and gDNA. Supplementary Table 5: Gene list ranked by secondary screening in MDA-MB-231 and HCT116 cells. Supplementary Table 6: Top enriched pathways of 612 genes ranked by secondary screening. Supplementary Table 7: Participant characteristics. Supplementary Table 8: Univariate and multivariate Cox regression analyses for disease-free survival. Supplementary Table 9: List of plasmids and primers used in the study. Supplementary Table 10: List of antibodies used in this study.
Source data
Source Data
Supporting blots for main and extended data figures.
Source Data
Raw data for all figures and extended data figures.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wortzel, I., Seo, Y., Akano, I. et al. Unique structural configuration of EV-DNA primes Kupffer cell-mediated antitumor immunity to prevent metastatic progression. Nat Cancer 5, 1815–1833 (2024). https://doi.org/10.1038/s43018-024-00862-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-024-00862-6
This article is cited by
-
Neutrophils secrete exosome-associated DNA to resolve sterile acute inflammation
Nature Cell Biology (2025)
-
Anti-metastatic extracellular vesicles carrying DNA
Nature Cancer (2024)