Abstract
Introduction
The 2023 nomenclature defined criteria for steatotic liver disease (SLD), including metabolic dysfunction-associated SLD (MASLD), alcohol-associated liver disease (ALD), and the overlapping MASLD/ALD (MetALD). We aimed to assess racial and ethnic disparities in the SLD prevalence among United States (US) adults based on this new nomenclature.
Methods
We undertook a cross-sectional study employing the 2017–2018 National Health and Nutrition Examination Survey (NHANES) database. We identified SLD according to a controlled attenuation parameter ≥288 dB/m, liver stiffness ≥7.2 kPa, or elevated aminotransferase levels. Alcohol use thresholds were established according to the updated SLD definition. We estimated prevalences using the complex design of the NHANES survey. Multivariable logistic regressions with complex design weights were employed.
Results
A total of 5532 individuals are included. The mean age is 45.4 years, and 50.9% are women. The adjusted estimated prevalence of MASLD is 42.4% (95% CI: 41.1–43.8%), MetALD 1.7% (95% CI: 1.3–2.0%), and ALD 0.6% (95% CI: 0.3–0.8%). Hispanics exhibit a higher prevalence of SLD, but there are no significant differences in advanced fibrosis prevalence due to SLD among racial/ethnic groups. In MASLD, men, individuals aged 40–64 and ≥65 years, Hispanics, those with health insurance, higher BMI, diabetes, hypertension, hypertriglyceridemia, and low high-density lipoprotein (HDL) cholesterol or use of lipid-lowering agents are independently associated with a higher risk, while Blacks have the lowest risk. In MetALD, men and higher BMI are independently associated with a higher risk of MetALD in adjusted multivariable analysis. In ALD, the adjusted multivariable analysis shows that only health insurance is independently associated with a lower ALD risk.
Conclusions
MASLD prevalence is high in the US, especially in men, older individuals, and Hispanics. MetALD and ALD prevalence was substantial but could be underestimated.
Plain language summary
This study aims to estimate the prevalence of different types of fatty liver disease, in which excess fat occurs in the liver. A particular type of fatty liver disease that is not caused by excess alcohol consumption affects 42.4% of adults in the USA, with men, older adults, and Hispanics being more likely to have this form of liver disease. People with health insurance are less likely to have liver disease caused by excess alcohol consumption. These results highlight the importance of targeted prevention efforts in people with a higher risk of developing liver disease. Future public health strategies should focus on reducing risk factors and providing equitable healthcare access.
Similar content being viewed by others
Introduction
Steatotic liver diseases (SLD), mainly metabolic dysfunction-associated steatotic liver disease (MASLD) (previously known as non-alcoholic fatty liver disease –NAFLD–) and alcohol-associated liver disease (ALD) are the leading causes of chronic liver disease globally, including in the United States (US)1,2. MASLD is associated with metabolic diseases, reaching an estimated prevalence of 65% in overweight patients, 90% in morbidly obese patients, and up to 70% in patients with type 2 diabetes mellitus (T2DM)3,4. However, prior evidence has demonstrated that moderate alcohol use could also interact with overweight/obesity, insulin resistance, T2DM, and genetic background, increasing the risk for chronic liver disease4. For example, a study using the United Kingdom (UK) Biobank found that those obese with excessive alcohol use and homozygous variant patatin-like phospholipase ___domain-containing protein 3 (PNPLA3) I148M carriers had a supramultiplicative risk of cirrhosis compared to those without the genetic variant5. Thus, since genetic variants had different distributions globally, potential regional differences in susceptibility to the development and the severity of SLD could be observed among different populations6.
A global consensus in 2023 established diagnostic criteria for MASLD, ALD, and the intersection between both diseases (MetALD)7. The new definition acknowledges the contribution of alcohol use in the development and progression of chronic liver disease, with specific thresholds of alcohol use for each diagnosis. Thus, MASLD is defined by liver steatosis in the presence of metabolic dysfunction, while MetALD is based on alcohol use ranging between 140–350 g/week in women and 210–420 g/week in men. Based on this definition, a recent study conducted in the US estimated the SLD prevalence at 34.2%, being MASLD at 31.3%, MetALD at 2.8%, and ALD at 0.1%8. Although MASLD prevalence was similar to prior estimates for NAFLD in countries such as the US8,9,10 and Brazil11, estimates of ALD could significantly decrease at the expense of a MetALD diagnosis.
In recent decades, significant disparities have been reported among individuals previously diagnosed with NAFLD and ALD prior to the nomenclature change in 202312,13,14. For example, a systematic review including 34 studies evidenced that MASLD prevalence was highest in Hispanics, intermediate in non-Hispanic (NH) whites, and lowest in Blacks15. However, they did not identify differences in terms of liver fibrosis among race/ethnicity. Another study assessing ALD in the US evidenced that men and Hispanic race were associated with harmful alcohol use, while in those admitted due to ALD, women, and Hispanic race were associated with increased risk of acute-on-chronic liver failure (ACLF)16. Since the new definition was released in 2023 with MetALD as a new clinical entity, information about its prevalence and potential disparities has been scarce worldwide. Therefore, this study aimed to identify the potential disparities in the SLD prevalence among American adults according to the new SLD definitions, including MASLD, MetALD, and ALD7. The adjusted estimated prevalence was high in the US, at 42.4% for MASLD, 0.6% for ALD, and 1.7% for MetALD in individuals aged over 15 years old. Although the five criteria for metabolic dysfunction were independently associated with SLD, only increased waist circumference and excess weight, abnormal glucose metabolism, and arterial hypertension were associated with a higher risk of advanced fibrosis. Potential disparities were observed in the SLD spectrum, with SLD prevalence notably higher in men (MASLD and MetALD), Hispanic race/ethnicity (MASLD), and those without health insurance (ALD).
Methods
Study design and participants
We used the 2017–2018 National Health and Nutrition Examination Survey (NHANES) dataset, a cross-sectional nationally representative survey of the non-institutionalized US population, including in-person interviews and health examinations in mobile examination centers. The 2017–2018 NHANES overall response rate was 51.9% for interviews and 48.8% for examinations. The NHANES survey includes a comprehensive assessment of sociodemographic and clinical data, where information regarding race/ethnicity, comorbidities, and levels of alcohol use are self-reported by survey participants. The NHANES database is publicly available and can be accessed at the following website: https://www.cdc.gov/nchs/nhanes/index.htm. The NHANES study was approved by the National Center for Health Statistics Research Ethics Review Board, and all participants provided informed consent to participate in the NHANES dataset. Since this study was conducted using anonymized public data, it was considered exempt from additional institutional review board approval.
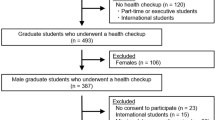
We included individuals aged over 15 years old who had data on liver stiffness measurement (LSM). Thus, we excluded 2958 participants aged under 15 years old and 764 without LSM assessment. We recorded self-reported sociodemographic data, including sex, education level (categorized as some high school, high school or some college, and college), health insurance, and race/ethnicity. Specifically, we classified individuals of NH white descent as “white”, individuals of NH Black descent as “Black/African American”, individuals of NH Asian descent as “Asian”, and individuals of other racial and ethnic backgrounds as “Other.” Mexican American and other Hispanic individuals were combined into a single category called “Hispanic”. We also registered levels of alcohol use, body mass index (BMI), T2DM prevalence, hypertension prevalence, and dyslipidemia prevalence. We identified SLD according to the presence of a controlled attenuation parameter (CAP) ≥ 288 dB/m17, an abnormal LSM ≥ 7.2 kPa (as a single value of abnormal LSM)18, or elevated liver enzyme levels (aspartate aminotransferase [AST] or alanine aminotransferase [ALT] >25 U/L in women and >35 U/L in men) in conjunction with other clinical parameters related to metabolic dysfunction, alcohol intake, and race/ethnicity19. This approach was designed to better capture the natural history of SLD, including those with significant fibrosis or steatohepatitis at the moment of the assessment, respectively. In particular, thresholds for AST and ALT were based on prior studies on SLD19,20,21,22. For MASLD and MetALD, we included those with at least 1 out of 5 cardiometabolic criteria, as per the 2023 consensus definition7. MASLD was identified based on alcohol use <140 g/week in women and <210 g/week in men; MetALD 140–350 g/week in women and 210–420 g/week in men; and ALD > 350 g/week in women and >420 g/week in men in the past 12 months, and after excluding hepatitis B and C chronic infections. Fibrosis was assessed using the median LSM, with significant fibrosis (F2) ≥ 8.2 kPa, advanced fibrosis (F3) ≥ 9.7 kPa, and cirrhosis (F4) ≥ 13.6 kPa23. In MASLD, we identified individuals with metabolic dysfunction-associated (MASH) steatohepatitis using a FibroScan-AST (FAST) score using a validated cut-off ≥0.35 (with a sensitivity of 90% to identify those with NAFLD activity score ≥4 and fibrosis stage ≥2 in liver biopsy)24. Also, we defined abnormal glucose metabolism as fasting glucose ≥100 mg/dL or 2-h post-load glucose levels ≥140 mg/dL, glycated hemoglobin ≥5.7%, T2DM, or treatment for T2DM, while increased adiposity and excess weight were described as a BMI ≥ 25 kg/m2 (23 kg/m2 in Asian) or elevated waist circumference (>94 cm for men >80 cm in women)7.
Statistical analysis
Our primary objective was the MASLD, MetALD, and ALD prevalence among different races and ethnicities in the US. The secondary objectives were the overall MASLD, MetALD, and ALD prevalence, and the prevalence of advanced liver fibrosis and the liver fibrosis stage among the different conditions. A sensitivity analysis was performed, identifying SLD based on CAP ≥ 288 dB/m or LSM ≥ 7.2 kPa exclusively. For the sensitivity analysis, we excluded the assessment of AST and ALT to avoid inclusion of patients with other potential causes of abnormal liver tests that can not be assessed in the NHANES database, including drug-induced liver injury (DILI), autoimmune hepatitis, Wilson’s disease, among others. We also made models to estimate prevalence by race/ethnicity, adjusting by age and sex. In addition, we built multivariable logistic regressions with appropriate complex design weights to estimate prevalence differences by sex, age, race/ethnicity, level of education, insurance, BMI, prediabetes and T2DM prevalence, and hypertension prevalence. We also estimated the SLD prevalence in those 15–39 years old and explored the odds ratio of the different metabolic dysfunction criteria in the diagnosis of SLD and the progression of liver fibrosis.
We assessed the distribution of data using visual methods, including histograms and kernel density estimates, due to the complex survey design. We estimated mean age and standard error (SE) using the complex design of the NHANES survey. Data non-normally distributed data was described as median and interquartile range. We estimated prevalences using the complex design of the NHANES survey, including the proportion and the 95% confidence interval (95% CI). We used logistic regression with appropriate complex design weights to estimate associations between variables and the prevalences of MASLD, MetALD, and ALD. When we assessed the performance of metabolic dysfunction criteria, we aggregated metabolic risk factors into five criteria, including: 1. Increased waist circumference, overweight or obesity; 2. prediabetes glucose intolerance, and T2DM; 3. Hypertension; 4. Hypertriglyceridemia; and 5. Low HDL cholesterol or use of lipid-lowering agents, to increase statistical power. Those variables that resulted significantly in the univariate analyses (p-value < 0.05) were used to adjust multivariable analyses using stepwise selection. A p-value < 0.05 indicated statistical significance (Stata version 18.0 [StataCorp]). The Pontificia Universidad Católica de Chile (Santiago, Chile) institutional review board granted the study exempt status in 2023.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Baseline characteristics and Ethnicity/Race
A total of 5532 out of 9254 individuals were included. The estimated mean age was 45.4 (SE: 0.6) years old and 50.9% were women (Table 1). In the overall population, 61.5% were NH white, 11.4% Black/African American, 16.4% Hispanic, 5.7% Asian, and 5.0% had other races/ethnicities. Around 87.5% of participants fulfilled at least 1 of 5 cardiometabolic criteria: 73.2% were overweight/obese or had increased adiposity, 52.4% had abnormal fasting glucose or diabetes, 43.1% had hypertension, 32.1% had hypertriglyceridemia, and 37.2% low high-density lipoprotein (HDL) cholesterol or used lipid-lowering agents. In addition, the estimated T2DM unadjusted prevalence was 11.1%, and 28.7% had metabolic syndrome. Table 1 summarizes the main characteristics of individuals with MASLD, MetALD, and ALD. In particular, individuals with ALD tend to be younger and predominantly men.
Hispanic individuals had a higher overweight or obesity prevalence than NH whites (78.8% versus 69.2%, p < 0.0001) (Supplementary Table 1). Also, Asians exhibited a higher T2DM prevalence than NH whites (13.7% versus 10.7%, p = 0.039). In the case of hypertension, Black/African American individuals showed a higher prevalence than NH whites (52.1% versus 43.7%, p = 0.002), while Hispanics had a lower prevalence (35.9% versus 43.7%, p = 0.023). Black/African Americans also showed a lower frequency of hypertriglyceridemia and low HDL cholesterol or use of lipid-lowering agents than NH whites (16.0% versus 33.2%, p < 0.0001; and 31.5% versus 37.2%, p = 0.041, respectively). Supplementary Table 1 summarizes all the baseline characteristics according to race/ethnicity.
Assessment of steatotic liver disease
Based on unadjusted estimates, the prevalence of liver steatosis was 33.1%, while 3.1% of participants had significant fibrosis, 3.2% advanced fibrosis, and 3.0% cirrhosis. The 40.8% (95% CI: 38.5%–43.2%) of the participants met the criteria of MASLD, 2.1% (95% CI: 1.6%–2.9%) of MetALD, and 0.9% (95% CI: 0.7%–1.2%) of ALD (Table 2). In individuals aged 15–39 years old, 29.8% (95% CI: 27.2%–32.6%) met the criteria of MASLD, 1.7% (95% CI: 1.0%–2.9%) of MetALD, and 1.1% (95% CI: 0.6%–1.8%) of ALD. Among those with MASLD, the unadjusted prevalence of suspected metabolic dysfunction-associated steatohepatitis (MASH) at risk was 13.3% (95% CI: 11.3%–15.2%). In addition, around 0.2% (95% CI: 0.1%–0.4%) of individuals had cryptogenic steatosis, while 0.2% (95% CI: 0.1%–0.4%) had chronic hepatitis B and 1.0% (95% CI: 0.4%–2.0%) hepatitis C virus infection. A total of 8.6% of people were lean MASLD and 16.3% lean MetALD, while 76.9% of ALD patients were overweight/obese. In sensitivity analyses, the estimated MASLD prevalence was 34.2% (95% CI: 31.9%–36.6%), MetALD 1.7% (95% CI: 1.2%–2.3%), and ALD 0.6% (95% CI: 0.4%–0.9%) (Fig. 1). A total of 20.1% of participants with MASLD had at least significant fibrosis, while 13.9% and 9.8% of patients with MetALD and ALD had a fibrosis stage ≥F2, respectively (Fig. 1).
Estimations include a the prevalence according to the pre-specified criteria, and b the prevalence obtained in the sensitivity analysis. Thresholds for fibrosis staging were based on liver stiffness measurements, including significant fibrosis (F2) ≥ 8.2 kPa, advanced fibrosis (F3) ≥ 9.7 kPa, and cirrhosis (F4) ≥ 13.6 kPa23. Sensitivity analysis identified steatotic liver disease based on CAP ≥ 288 dB/m or LSM ≥ 7.2 kPa exclusively. The numerical data used to plot this figure is available in Supplementary Data 2.
MASLD prevalence was higher in men, individuals aged 40–64 and ≥65 years old, of Hispanic ethnicity, with any health insurance, higher BMI, T2DM, hypertension, hypertriglyceridemia, and low HDL cholesterol or use of lipid-lowering agents (Table 3). A multivariable analysis adjusted by significant variables from the univariate analysis showed that men (odds ratio [OR] 1.30, 95% CI: 1.05–1.61; p = 0.019), individuals aged 40–64 (OR 1.69, 95% CI: 1.42–2.02; p < 0.0001) and ≥65 years old (OR 1.57, 95% CI: 1.13–2.19; p = 0.011), Hispanics (OR 1.49, 95% CI: 1.11–2.01; p = 0.012), those with health insurance (OR 1.46, 95% CI: 1.02–2.08; p = 0.039) higher BMI (OR 1.16, 95% CI: 1.14–1.18; p < 0.0001), T2DM (OR 1.92, 95% CI: 1.37–2.70; p = 0.001), hypertension (OR 1.46, 95% CI: 1.11–1.92; p = 0.010), hypertriglyceridemia (OR 1.75, 95% CI: 1.46–2.09; p < 0.0001), and low HDL cholesterol or use of lipid-lowering agents (OR 1.34, 95% CI: 1.04–1.74; p = 0.029) were independently associated with a higher odds of MASLD (Table 3). In the same multivariate analysis, Black/African Americans showed lower odds of MASLD compared to NH whites (OR 0.62; 95%: 0.48–0.81; p = 0.002).
MetALD was more frequent in men and those with higher BMI, while it was lower in Asians. A multivariable analysis adjusted by sex, ethnicity, and BMI showed that men (OR 2.37, 95% CI: 1.30–4.32; p = 0.008) and higher BMI (OR 1.02, 95% CI: 1.00–1.04; p = 0.031) were independently associated with higher odds of MetALD (Table 3). Finally, in the case of ALD, this condition was more frequently observed in men, those aged ≥65 years old, and low HDL cholesterol or use of lipid-lowering agents, but its prevalence was lower in those with a higher level of education and health insurance (Table 3). In a multivariable analysis, only individuals with health insurance (OR 0.41, 95% CI: 0.17–0.95; p = 0.040) were independently associated with lower ALD prevalence (Table 3).
We also estimated the prevalence according to race/ethnicity in models adjusted by age and sex. Thus, the adjusted standardized prevalence of SLD was 45.1% (95% CI: 43.7–46.5%), with 42.4% (95% CI: 41.1–43.8%) for MASLD, 1.7% (95% CI: 1.3–2.0%) for MetALD, and 0.6% (95% CI: 0.3–0.8%) for ALD. In MASLD, the adjusted prevalence of MASH at risk was 12.7% (95% CI: 10.8%–14.5%). In these models, only Hispanic ethnicity was associated with a higher risk of SLD for all ages (Fig. 2a). However, there were no significant differences in the odds of advanced fibrosis (Fig. 2b) or MASH at risk among racial/ethnic groups compared to NH whites (Black: OR 0.94, 95% CI: 0.59–1.49, p = 0.766; Hispanic: OR 1.22, 95% CI: 0.78–1.93, p = 0.356; Asian: OR 1.05, 95% CI: 0.70–1.59, p = 0.797).
Metabolic dysfunction criteria and risk of liver disease
In the study cohort, 26.8% of individuals had normal weight, 1.7% had increased adiposity with normal weight, 31.1% were overweight, and 40.3% had obesity. There was a dose-dependent relationship between abnormal weight and the SLD risk (increased adiposity, OR 2.86, 95% CI: 1.36–5.98, p = 0.009; overweight, OR 4.30, 95% CI: 3.45–5.36, p < 0.0001; obesity, OR 16.04, 95% CI: 12.25–21.01, p < 0.0001) (Fig. 3a). Similarly, abnormal glucose metabolism also exhibited a dose-dependent SLD risk (abnormal fasting glucose or prediabetes OR 2.49, 95% CI: 2.08–2.97, p < 0.0001; and T2DM OR 7.13, 95% CI: 5.71–8.90, p < 0.0001) (Fig. 3b). In terms of fibrosis, obesity, but no increased adiposity nor overweight was associated with a higher risk of advanced fibrosis (obesity OR 8.89, 95% CI: 3.46–22.88, p < 0.0001) (Fig. 3c). Finally, abnormal glucose metabolism showed a dose-dependent association with advanced fibrosis (abnormal fasting glucose or prediabetes OR 1.81, 95% CI: 1.26–2.61, p = 0.003; and T2DM OR 7.01, 95% CI: 4.08–12.05, p < 0.0001) (Fig. 3d). Supplementary Table 2 summarizes the main frequency of cardiometabolic risk factors among race/ethnicities. In terms of metabolic dysfunction, all five criteria were associated with a lower risk of SLD, advanced fibrosis, and cirrhosis (Supplementary Data 1). A multivariable analysis adjusted by significant variables from the univariate analysis showed that abnormal weight, glucose metabolism, and hypertension have the highest odds of SLD (Supplementary Data 1). Also, only abnormal weight (OR 3.05, 95% CI: 1.04–8.94; p = 0.043), abnormal glucose metabolism (OR 1.69, 95% CI: 1.04–2.73; p = 0.036), and hypertension (OR 2.20, 95% CI: 1.37–3.53; p = 0.003) were independently associated with advanced fibrosis. Finally, only hypertension (OR 2.72, 95% CI: 1.54–4.80; p = 0.002) was independently associated with cirrhosis (Supplementary Data 1).
a SLD prevalence according to the presence of excess weight; b SLD prevalence according to abnormal glucose metabolism and type 2 diabetes mellitus (T2DM); c advanced fibrosis prevalence according to the presence of excess weight; and d advanced fibrosis prevalence according to abnormal glucose metabolism and T2DM. We defined abnormal glucose metabolism as fasting glucose ≥100 mg/dL, or 2-hour post-load glucose levels ≥140 mg/dL, glycated hemoglobin ≥5.7%, T2DM, or treatment for T2DM, while increased adiposity and excess weight were described as a BMI ≥ 25 kg/m² (≥23 kg/m² in Asian populations) or elevated waist circumference (>94 cm for men and >80 cm for women). Error bars represent the 95% confidence interval from estimations using the complex design of the survey. The numerical data used to plot this figure is available in Supplementary Data 2.
Discussion
In this study, we estimated high adjusted SLD prevalence in the US between 2017–2018, with 45.1% for SLD, 42.4% for MASLD, 1.7% for MetALD, and 0.6% for ALD in individuals aged over 15 years old. This high burden may contribute to numerous health-related consequences, including cardiovascular disease, cirrhosis, primary liver cancer, and other neoplasms25,26. Individuals identified as Hispanic had a higher prevalence of SLD compared to other race/ethnic groups, but there were no significant differences in the prevalence of advanced fibrosis due to SLD among racial and ethnic groups. Men and individuals of Hispanic race/ethnicity evidenced a higher risk of MASLD, exhibiting potential disparities in these populations, while Blacks had a lower risk. Although MetALD was more frequent in men, with higher BMI, but lower in Asians, there were no differences among races/ethnicities in the multivariable analysis. ALD was more frequent in men, those with lower levels of education, and those without health insurance.
Our results showed that Hispanics were at higher risk of MASLD in the US, which is consistent with previously published data27. However, important differences have been observed in the Hispanic population living in the US according to their country of origin28. In addition, Hispanics could exhibit a higher risk of MASH15. Differences in SLD among races and ethnicities could be driven by genetic susceptibility, socioeconomic factors, unhealthy lifestyles, and dietary patterns4,15,29. In terms of genetic background, the variant I148M of the PNPLA3 gene is the most studied genetic polymorphism30, which has been robustly associated with susceptibility to steatosis, steatohepatitis, fibrosis, and hepatocellular carcinoma in MASLD and ALD4. Interestingly, this gene variant is twice as common in Hispanics compared to other populations31,32. BMI is also higher in Hispanics compared to other ethnicities, as well as other metabolic risk factors such as T2DM, arterial hypertension, visceral obesity, and dyslipidemia33. In addition, the dietary pattern of Hispanics living in the US is often based on a carbohydrate-rich diet, including tortillas, beans, and rice, especially among Puerto Rican, Dominican, and Mexican populations34. Healthy food is expensive for people living in low-income households, while cheaper food could be easier to obtain but tends to have higher levels of added sugars and saturated fat, increasing the risk of MASLD and MetALD. A recent study assessing food security in the US demonstrated that Blacks and Hispanics have a higher prevalence of food insecurity35. However, NH whites with MASLD had lower diet quality scores with greater food insecurity compared to other races/ethnicities. Finally, Blacks had a lower risk of MASLD despite having higher rates of hypertension and obesity than Hispanics living in the US36. These differences have been attributed to a lower amount of visceral fat and lower prevalence of high-risk genetic variants in African Americans37; however, more data are required to elucidate these differences. In this study, we also observed that having health insurance was associated with a higher risk of MASLD. Previous studies, particularly those examining multiple chronic conditions, have documented a higher prevalence of chronic diseases in insured populations, especially among those with public health insurance38. This finding may be influenced by socioeconomic or lifestyle factors that were not accounted for in the models, and further research is needed to clarify this potential association.
Alcohol misuse and drinking patterns could also influence the natural history of SLD, especially MetALD and ALD. In the case of ALD, no race/ethnicity was independently associated with ALD. However, those who are most socially disadvantaged (no health insurance and lower education levels) exhibited higher ALD prevalence, which is in line with the alcohol-harm paradox where people of low socioeconomic status tend to experience disproportionately greater alcohol-related harm than those of high socioeconomic status, even when the amount of alcohol consumption is the same or less than those with higher income39. NH whites have a higher alcohol use compared to other races/ethnicities40. However, binge drinking is more frequently observed in American Indians and Hispanics, while heavy drinking and alcohol use disorder (AUD) is higher in American Indians41. In Hispanic women, the population-based Hispanic Community Health Study/ Study of Latinos (HCHS/SOL) showed that alcohol use was commonly associated with younger age, greater acculturation, having greater than high school education, and being employed full-time predicted current drinking. In the case of Hispanic men, socioeconomic indicators, being employed full time (versus retired), and having a lower income predicted alcohol use42. Also, AUD prevalence could be higher in Puerto Ricans and Mexican Americans compared to South/Central and Cuban Americans41.
Around 54.1% of the American population consumes alcohol, with a rising AUD prevalence ranging from 8.5% to 12.7% in the US43. Also, 90% of heavy drinkers will develop steatosis, and around 12% of these patients with AUD will have advanced fibrosis or cirrhosis44. Therefore, MetALD and ALD prevalence could be even higher than the estimates obtained. The underestimation could be due to recall bias, selection bias, and underreporting of alcohol use45. Also, alcohol intake thresholds are ill-defined and can overlap with ALD. Prior evidence has suggested that lower levels of alcohol use can induce liver disease4,46,47,48. Metabolic dysfunction was also frequent in the US population using the 1 out of 5 criteria (87.5% of the overall population). However, only increased adiposity, abnormal glucose metabolism, and arterial hypertension were independently associated with advanced fibrosis. These relationships were also dose-dependent, suggesting the need to better identify the phenotypes among MASLD and MetALD patients. Major and minor criteria could highlight the role of obesity, T2DM, and arterial hypertension over dyslipidemia and other criteria. Also, a standardized method to quantify alcohol use in clinical practice (i.e. validated questionnaires and alcohol biomarkers) is urgently needed, as well as the exposure to alcohol over time. Further studies should also be conducted to determine the best threshold to determine MetALD and to provide stricter recommendations in terms of alcohol abstinence and pharmacological therapies to individuals with dual etiology.
Since alcohol use and metabolic dysfunction are the leading drivers of SLD49, strategies to enforce the World Health Organization SAFER initiative and other relevant alcohol-related public health policies could contribute to decreasing the incidence of SLD50,51. Although several European countries have demonstrated that pricing policies can be effective in decreasing alcohol use, a national plan on alcohol addressing racial and ethnic disparities and strategies to increase access to screening, brief interventions, and treatment (especially in populations with lower access to the healthcare system) could strongly impact in the natural history of SLD51. Other public health policies targeting obesity, T2DM, arterial hypertension, dyslipidemia, the registry of the burden of SLD, and efforts to raise awareness can also contribute to tackling this huge problem2,52. In particular, it is necessary to identify patients at risk early on, develop standardized approaches to non-invasive testing, and establish effective and personalized treatment and care, coupled with societal interventions53,54. These objectives should be coordinated with the medical and research community beyond hepatology and other key clinical stakeholders, such as endocrinologists and primary care physicians, to public health and policy, with WHO and key governmental entities to decrease poor liver health outcomes due to alcohol use and metabolic dysfunction55.
Due to its nature, this study has some limitations. First, it is based on observational data that could have been affected by misclassification. Also, we did not have a liver biopsy to confirm the diagnosis. As aforementioned, all clinical information and levels of alcohol use were self-reported, which could contribute to lower estimates of MetALD and ALD prevalence and misclassification45,56. In particular, drinking patterns are unknown, and estimation of weekly alcohol use could significantly vary. There are multiple CAP and LSM cutoffs validated, which could vary the estimations of SLD prevalence. Also, we do not have information about the length of time of alcohol use and metabolic dysfunction-associated comorbidities. Although the new evidence proposes the diagnosis of MetALD based on the presence of 1 out of 5 criteria, current data does not support that alcohol interacts with hypertension or dyslipidemia in the same way as overweight or T2DM to develop chronic liver disease in the long term. In fact, alcohol misuse can cause arterial hypertension and dyslipidemia, thereby resulting in the misclassification of patients. Although we excluded individuals with hepatitis B and hepatitis C virus infection, we did not have information about less prevalent conditions that could develop hepatic steatosis, including drug-induced liver injury, hemochromatosis, Wilson’s disease, familial hypobetalipoproteinemia, liposomal acid lipase deficiency, among others. Finally, the low number of individuals in some ethnic groups can be difficult to compare with individuals with advanced fibrosis, especially in MetALD and ALD. Therefore, although rates of MetALD and ALD seem lower compared to MASLD, a high clinical suspicion of alcohol use should be held in individuals with metabolic dysfunction. The use of alcohol biomarkers and reassessment of metabolic dysfunction after three months of alcohol abstinence could facilitate the identification of these three entities and avoid misclassification.
In conclusion, this study illustrates the high prevalence of SLD in the US. Potential disparities were identified in the natural history of SLD, with MASLD independently associated with men and Hispanic race/ethnicity, MetALD with men and a higher BMI, and ALD with a lower educational level and absence of medical insurance. Prospective studies using precise alcohol use quantification, including standardized assessments and alcohol biomarkers, are necessary to better estimate the burden of MetALD and ALD.
Data availability
The datasets generated and analyzed during the current study and used for the creation of figures are publicly available in the United States on the website: https://www.cdc.gov/nchs/nhanes/index.htm. The numerical data used to plot Figs. 1 and 3 are available in Supplementary Data 2.
References
Younossi, Z. M., Wong, G., Anstee, Q. M. & Henry, L. The global burden of liver disease. Clin. Gastroenterol. Hepatol. 21, 1978–1991 (2023).
Díaz, L. A. et al. The establishment of public health policies and the burden of non-alcoholic fatty liver disease in the Americas. Lancet Gastroenterol. Hepatol. https://doi.org/10.1016/S2468-1253(22)00008-5 (2022).
En Li Cho, E. et al. Global prevalence of non-alcoholic fatty liver disease in type 2 diabetes mellitus: an updated systematic review and meta-analysis. Gut 72, 2138–2148 (2023).
Díaz, L. A., Arab, J. P., Louvet, A., Bataller, R. & Arrese, M. The intersection between alcohol-related liver disease and nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. https://doi.org/10.1038/s41575-023-00822-y (2023).
Kim, H.-S. et al. Synergistic Associations of PNPLA3 I148M Variant, Alcohol Intake, and Obesity With Risk of Cirrhosis, Hepatocellular Carcinoma, and Mortality. JAMA Netw Open 5, e2234221 (2022).
Díaz, L. A. et al. Liver diseases in Latin America: current status, unmet needs, and opportunities for improvement. Curr. Treat. Options Gastroenterol. 20, 261–278 (2022).
Rinella, M. E. et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. Hepatology https://doi.org/10.1097/HEP.0000000000000520 (2023).
Lee, B. P., Dodge, J. L. & Terrault, N. A. National prevalence estimates for steatotic liver disease and sub-classifications using consensus nomenclature. Hepatology https://doi.org/10.1097/HEP.0000000000000604 (2023).
Ciardullo, S., Carbone, M., Invernizzi, P. & Perseghin, G. Exploring the landscape of steatotic liver disease in the general US population. Liver Int. 43, 2425–2433 (2023).
Kalligeros, M. et al. Prevalence of steatotic liver disease (MASLD, MetALD and ALD) in the United States: NHANES 2017-2020. Clin. Gastroenterol. Hepatol. https://doi.org/10.1016/j.cgh.2023.11.003 (2023).
Perazzo, H., Pacheco, A. G., Griep, R. H. & Collaborators. Changing from NAFLD through MAFLD to MASLD: Similar prevalence and risk factors in a large Brazilian cohort. J. Hepatol. https://doi.org/10.1016/j.jhep.2023.08.025 (2023).
Cotter, T. G. et al. Racial and ethnic disparities in liver transplantation for alcohol-associated liver diseases in the United States. Transplantation https://doi.org/10.1097/TP.0000000000004701 (2023).
Anouti, A. et al. Racial and ethnic disparities in alcohol-associated liver disease in the United States: a systematic review and meta-analysis. Hepatol. Commun. 8, e0409 (2024).
Ayares, G. et al. Racial and ethnic disparities in the natural history of alcohol-associated liver disease in the United States. Liver Int. https://doi.org/10.1111/liv.16023 (2024).
Rich, N. E. et al. Racial and ethnic disparities in nonalcoholic fatty liver disease prevalence, severity, and outcomes in the United States: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 16, 198–210.e2 (2018).
Singal, A. K. et al. Alcohol-associated liver disease in the United States is associated with severe forms of disease among young, females and Hispanics. Aliment. Pharmacol. Ther. 54, 451–461 (2021).
Caussy, C. et al. Optimal threshold of controlled attenuation parameter with MRI-PDFF as the gold standard for the detection of hepatic steatosis. Hepatology 67, 1348–1359 (2018).
Foucher, J. et al. Diagnosis of cirrhosis by transient elastography (FibroScan): a prospective study. Gut 55, 403–408 (2006).
Wong, T., Dang, K., Ladhani, S., Singal, A. K. & Wong, R. J. Prevalence of alcoholic fatty liver disease among adults in the United States, 2001-2016. JAMA 321, 1723–1725 (2019).
Degertekin, B. et al. Determination of the upper limits of normal serum alanine aminotransferase (ALT) level in healthy Turkish population. Hepatol. Forum 1, 44–47 (2020).
Lee, J. K. et al. Estimation of the healthy upper limits for serum alanine aminotransferase in Asian populations with normal liver histology. Hepatology 51, 1577–1583 (2010).
Chang, Y., Ryu, S., Sung, E. & Jang, Y. Higher concentrations of alanine aminotransferase within the reference interval predict nonalcoholic fatty liver disease. Clin. Chem. 53, 686–692 (2007).
Eddowes, P. J. et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology 156, 1717–1730 (2019).
Newsome, P. N. et al. FibroScan-AST (FAST) score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis: a prospective derivation and global validation study. Lancet Gastroenterol. Hepatol. 5, 362–373 (2020).
Rumgay, H. et al. Global burden of primary liver cancer in 2020 and predictions to 2040. J. Hepatol. 77, 1598–1606 (2022).
Duell, P. B. et al. Nonalcoholic fatty liver disease and cardiovascular risk: a scientific statement from the American Heart Association. Arterioscler. Thromb. Vasc. Biol. 42, e168–e185 (2022).
Setiawan, V. W. et al. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: the multiethnic cohort. Hepatology 64, 1969–1977 (2016).
Kallwitz, E. R. et al. Prevalence of suspected nonalcoholic fatty liver disease in Hispanic/Latino individuals differs by heritage. Clin. Gastroenterol. Hepatol. 13, 569–576 (2015).
Rieman-Klingler, M. C., Jung, J., Tesfai, K., Loomba, R. & Non, A. L. Integrating genetic and socioeconomic data to predict the progression of nonalcoholic fatty liver disease. Am. J. Biol. Anthropol. 184, e24979 (2024).
Wang, J. et al. Association of genetic risk score with NAFLD in an ethnically diverse cohort. Hepatol. Commun. 5, 1689–1703 (2021).
Pinto Marques Souza de Oliveira, C., Pinchemel Cotrim, H. & Arrese, M. Nonalcoholic fatty liver disease risk factors in Latin American populations: current scenario and perspectives. Clin. Liver Dis. 13, 39–42 (2019).
Pontoriero, A. C. et al. Influence of ethnicity on the distribution of genetic polymorphisms associated with risk of chronic liver disease in South American populations. BMC Genet. 16, 93 (2015).
Vidal, T. M., Williams, C. A., Ramoutar, U. D. & Haffizulla, F. Type 2 diabetes mellitus in Latinx populations in the United States: a culturally relevant literature review. Cureus 14, e23173 (2022).
Mora, N. & Golden, S. H. Understanding cultural influences on dietary habits in Asian, Middle Eastern, and Latino patients with type 2 diabetes: a review of current literature and future directions. Curr. Diab. Rep. 17, 126 (2017).
Kardashian, A., Dodge, J. L. & Terrault, N. A. Racial and ethnic differences in diet quality and food insecurity among adults with fatty liver and significant fibrosis: a U.S. population-based study. Aliment. Pharmacol. Ther. 56, 1383–1393 (2022).
Saab, S., Manne, V., Nieto, J., Schwimmer, J. B. & Chalasani, N. P. Nonalcoholic fatty liver disease in Latinos. Clin. Gastroenterol. Hepatol. 14, 5–12 (2016).
Wagenknecht, L. E. et al. Association of PNPLA3 with non-alcoholic fatty liver disease in a minority cohort: the Insulin Resistance Atherosclerosis Family Study. Liver Int. 31, 412–416 (2011).
Boersma, P., Black, L. I. & Ward, B. W. Prevalence of multiple chronic conditions among US Adults, 2018. Prev. Chronic Dis. 17, E106 (2020).
Probst, C., Kilian, C., Sanchez, S., Lange, S. & Rehm, J. The role of alcohol use and drinking patterns in socioeconomic inequalities in mortality: a systematic review. Lancet Public Health 5, e324–e332 (2020).
Chartier, K. & Caetano, R. Ethnicity and health disparities in alcohol research. Alcohol Res. Health 33, 152–160 (2010).
Vaeth, P. A. C., Wang-Schweig, M. & Caetano, R. Drinking, alcohol use disorder, and treatment access and utilization among U.S. racial/ethnic groups. Alcohol. Clin. Exp. Res. 41, 6–19 (2017).
Castañeda, S. F. et al. Alcohol use, acculturation and socioeconomic status among Hispanic/Latino men and women: The Hispanic Community Health Study/Study of Latinos. PLoS One 14, e0214906 (2019).
Grant, B. F. et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 74, 911–923 (2017).
Vannier, A. G. L. et al. Incidence and progression of alcohol-associated liver disease after medical therapy for Alcohol Use Disorder. JAMA Netw Open 5, e2213014 (2022).
Staufer, K. et al. Ethyl glucuronide in hair detects a high rate of harmful alcohol consumption in presumed non-alcoholic fatty liver disease. J. Hepatol. https://doi.org/10.1016/j.jhep.2022.04.040. (2022)
Liu, B., Balkwill, A., Reeves, G., Beral, V. & Million Women Study Collaborators. Body mass index and risk of liver cirrhosis in middle aged UK women: prospective study. BMJ 340, c912 (2010).
Åberg, F., Helenius-Hietala, J., Puukka, P., Färkkilä, M. & Jula, A. Interaction between alcohol consumption and metabolic syndrome in predicting severe liver disease in the general population. Hepatology 67, 2141–2149 (2018).
Decraecker, M. et al. Long-term prognosis of patients with alcohol-related liver disease or non-alcoholic fatty liver disease according to metabolic syndrome or alcohol use. Liver Int. 42, 350–362 (2022).
Israelsen, M., Torp, N., Johansen, S., Thiele, M. & Krag, A. MetALD: new opportunities to understand the role of alcohol in steatotic liver disease. Lancet Gastroenterol. Hepatol. 8, 866–868 (2023).
Díaz, L. A. et al. Impact of public health policies on alcohol-associated liver disease in Latin America: an ecological multinational study. Hepatology 74, 2478–2490 (2021).
Díaz, L. A. et al. Association between public health policies on alcohol and worldwide cancer, liver disease and cardiovascular disease outcomes. J. Hepatol. https://doi.org/10.1016/j.jhep.2023.11.006. (2023)
Lazarus, J. V. et al. The global NAFLD policy review and preparedness index: Are countries ready to address this silent public health challenge? J. Hepatol. 76, 771–780 (2022).
Lazarus, J. V. et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nat. Rev. Gastroenterol. Hepatol. 19, 60–78 (2022).
Lazarus, J. V. et al. A global research priority agenda to advance public health responses to fatty liver disease. J. Hepatol. https://doi.org/10.1016/j.jhep.2023.04.035 (2023).
Allen, A. M., Younossi, Z. M., Diehl, A. M., Charlton, M. R. & Lazarus, J. V. Envisioning how to advance the MASH field. Nat. Rev. Gastroenterol. Hepatol. https://doi.org/10.1038/s41575-024-00938-9 (2024).
Danpanichkul, P., Suparan, K., Kim, D. & Wijarnpreecha, K. What is new in metabolic dysfunction-associated steatotic liver disease in lean individuals: from bench to bedside. J. Clin. Med. 13, 278 (2024).
Acknowledgements
Jeffrey V. Lazarus acknowledges support to ISGlobal from the grant CEX2018-000806-S funded by MCIN/AEI/10.13039/501100011033 and the ´Generalitat de Catalunya´ through the CERCA Program, outside of the submitted work. Ramón Bataller is recipient of NIAAA U01AA021908 and U01AA020821. Rohit Loomba receives funding support from NCATS (5UL1TR001442), NIDDK (U01DK061734, U01DK130190, R01DK106419, R01DK121378, R01DK124318, P30DK120515), NHLBI (P01HL147835), John C Martin Foundation (RP124) and NIAAA (U01AA029019). Marco Arrese receives support from the Chilean government through the Fondo Nacional de Desarrollo Científico y Tecnológico (FONDECYT 1241450).
Author information
Authors and Affiliations
Contributions
L.A.D. and J.P.A. conceived and designed the study; L.A.D. and E.F.L. collected the data, and contributed to data analysis and interpretation; L.A.D., E.F.L., J.V.L., and J.P.A. performed the final analysis and drafted the manuscript. All the authors participated in drafting the article and revising it critically for important intellectual content. All the authors approved the final version of the version submitted.
Corresponding author
Ethics declarations
Competing interests
Rohit Loomba serves as a consultant to Aardvark Therapeutics, Altimmune, Arrowhead Pharmaceuticals, AstraZeneca, Cascade Pharmaceuticals, Eli Lilly, Gilead, Glympse Bio, Inipharma, Intercept, Inventiva, Ionis, Janssen Inc., Lipidio, Madrigal, Neurobo, Novo Nordisk, Merck, Pfizer, Sagimet, 89 bio, Takeda, Terns Pharmaceuticals and Viking Therapeutics. Rohit Loomba has stock options in Sagimet biosciences. In addition, his institution received research grants from Arrowhead Pharmaceuticals, Astrazeneca, Boehringer-Ingelheim, Bristol-Myers Squibb, Eli Lilly, Galectin Therapeutics, Gilead, Intercept, Hanmi, Intercept, Inventiva, Ionis, Janssen, Madrigal Pharmaceuticals, Merck, Novo Nordisk, Pfizer, Sonic Incytes and Terns Pharmaceuticals. Rohit Loomba is a co-founder of LipoNexus Inc. Other authors declare that they have no conflicts of interest.
Peer review
Peer review information
Communications Medicine thanks Pedro Ochoa-Allemant and Zaki Sherif for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Díaz, L.A., Lazarus, J.V., Fuentes-López, E. et al. Disparities in steatosis prevalence in the United States by Race or Ethnicity according to the 2023 criteria. Commun Med 4, 219 (2024). https://doi.org/10.1038/s43856-024-00649-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-024-00649-x