Abstract
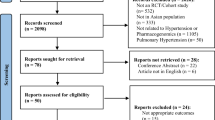
Hypertension is the biggest and most prevalent risk factor for cardiovascular diseases. Depression is the most common psychiatric illness worldwide. Many studies have linked the development of new depression to the use of antihypertensive drugs. This meta-analysis was done to ascertain the relationship. Using standard reporting techniques a literature search was undertaken in Pubmed from inception till 10 May 2024. The risk bias assessment was done using the ROBINS-I tool. Data for the odds ratio were combined using Revman 5.4 using a random or fixed effects model. Our analysis found a significant association between beta blockers and calcium channel blockers use and the risk of developing new depression. Results for other classes of antihypertensives were not significant. The findings highlight the importance of taking into account the potential psychiatric side effects of antihypertensive drugs in people with hypertension. Physicians should stay vigilant and screen their patients for these conditions regularly.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
The search strategy can be found in Supplementary File 1. All other data can be obtained from the corresponding author upon reasonable request.
References
Raič M. Depression and heart diseases: leading health problems. Psychiatr Danub. 2017;4:770–7.
Li Z, Li Y, Chen L, Chen P, Hu Y. Prevalence of depression in patients with hypertension: a systematic review and meta-analysis. Medicine. 2015;94:e1317.
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–50.
Malhi GS, Mann JJ. Depression. Lancet Lond Engl. 2018;392:2299–312.
Johannessen L, Strudsholm U, Foldager L, Munk-Jørgensen P. Increased risk of hypertension in patients with bipolar disorder and patients with anxiety compared to background population and patients with schizophrenia. J Affect Disord. 2006;95:13–7.
Kretchy IA, Owusu-Daaku FT, Danquah SA. Mental health in hypertension: assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int J Ment Health Syst. 2014;8:25.
Fan B, Zhao JV. Genetic proxies for antihypertensive drugs and mental disorders: mendelian randomization study in European and East Asian populations. BMC Med. 2024;22:6.
Tanase DM, Gosav EM, Radu S, Ouatu A, Rezus C, Ciocoiu M, et al. Arterial hypertension and interleukins: potential therapeutic target or future diagnostic marker? Int J Hypertens. 2019;2019:3159283.
Cruickshank JM. The role of beta-blockers in the treatment of hypertension. Adv Exp Med Biol. 2017;956:149–66.
Beers MH, Passman LJ. Antihypertensive medications and depression. Drugs. 1990;40:792–9.
Nasr SJ, Crayton JW, Agarwal B, Wendt B, Kora R. Lower frequency of antidepressant use in patients on renin-angiotensin-aldosterone system modifying medications. Cell Mol Neurobiol. 2011;31:615–8.
Agustini B, Mohebbi M, Woods RL, McNeil JJ, Nelson MR, Shah RC, et al. The association of antihypertensive use and depressive symptoms in a large older population with hypertension living in Australia and the United States: a cross-sectional study. J Hum Hypertens. 2020;34:787–94.
Kessing LV, Rytgaard HC, Ekstrøm CT, Torp-Pedersen C, Berk M, Gerds TA. Antihypertensive drugs and risk of depression: a nationwide Population-Based Study. Hypertens Dallas Tex 1979. 2020;76:1263–79.
Cao YY, Xiang X, Song J, Tian YH, Wang MY, Wang XW, et al. Distinct effects of antihypertensives on depression in the real-world setting: a retrospective cohort study. J Affect Disord. 2019;259:386–91.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing riskof-bias assessments. Res Syn Meth. 2021;12:55–61.
Cornell JE, Mulrow CD, Localio R, Stack CB, Meibohm AR, Guallar E, et al. Random-effects meta-analysis of inconsistent effects: a time for change. Ann Intern Med. 2014;160:267–70.
Review Manager (RevMan) [Computer program]. Version 5.4. The Cochrane Collaboration, 2020
Haddaway NR, Page MJ, Pritchard CC, McGuinness LA. PRISMA2020: an R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst Rev. 2022;18:e1230.
Zill P, Baghai TC, Schüle C, Born C, Früstück C, Büttner A, et al. DNA methylation analysis of the Angiotensin Converting Enzyme (ACE) gene in major depression. PLOS ONE. 2012;7:e40479.
Bornand D, Reinau D, Jick SS, Meier CR. β-blockers and the risk of depression: a Matched Case-Control Study. Drug Saf. 2022;45:181–9.
Verbeek DEP, van Riezen J, de Boer RA, van Melle JP, de Jonge P. A review on the putative association between beta-blockers and depression. Heart Fail Clin. 2011;7:89–99.
Poirier L, Tobe SW. Contemporary use of β-blockers: clinical relevance of subclassification. Can J Cardiol. 2014;30:S9–15.
Riemer TG, Villagomez Fuentes LE, Algharably EAE, Schäfer MS, Mangelsen E, Fürtig MA, et al. Do β-blockers cause depression? Hypertension. 2021;77:1539–48.
Li Y, Fan Y, Sun Y, Alolga RN, Xiao P, Ma G. Antihypertensive drug use and the risk of depression: a systematic review and network meta-analysis. Front Pharmacol. 2021;12:777987.
Chauquet S, Zhu Z, O’Donovan MC, Walters JTR, Wray NR, Shah S. Association of antihypertensive drug target genes with psychiatric disorders: a mendelian Randomization Study. JAMA Psychiatry. 2021;78:623–31.
Du XL, Martinez J, Yamal JM, Simpson LM, Davis BR. The 18-year risk of cancer, angioedema, insomnia, depression, and erectile dysfunction in association with antihypertensive drugs: post-trial analyses from ALLHAT-Medicare linked data. Front Cardiovasc Med. 2023;10:1272385.
Lee JM, Choi S, Jeong S, Son JS, Park SJ, Chang J, et al. Distinct effects of angiotensin converting enzyme inhibitors and angiotensin receptor blockers on major depressive disorder: a nationwide cohort study. Asian J Psychiatry. 2023;81:103436.
Shaw RJ, Mackay D, Pell JP, Padmanabhan S, Bailey DS, Smith DJ. The relationship between antihypertensive medications and mood disorders: analysis of linked healthcare data for 1.8 million patients. Psychol Med. 2021;51:1183–91.
van Sloten TT, Souverein PC, Stehouwer CD, Driessen JH. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers and risk of depression among older people with hypertension. J Psychopharmacol Oxf Engl. 2022;36:594–603.
Van de Velde S, Bracke P, Levecque K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc Sci Med 1982. 2010;71:305–13.
Boal AH, Smith DJ, McCallum L, Muir S, Touyz RM, Dominiczak AF, et al. Monotherapy with major antihypertensive drug classes and risk of hospital admissions for mood disorders. Hypertens Dallas Tex 1979. 2016;68:1132–8.
Feng L, Tan CH, Merchant RA, Ng TP. Association between depressive symptoms and use of HMG-CoA reductase inhibitors (statins), corticosteroids and histamine H(2) receptor antagonists in community-dwelling older persons: cross-sectional analysis of a population-based cohort. Drugs Aging. 2008;25:795–805.
Gammoh O, Bjørk MH, Al Rob OA, AlQudah AR, Hani AB, Al-Smadi A. The association between antihypertensive medications and mental health outcomes among Syrian war refugees with stress and hypertension. J Psychosom Res. 2023;168:111200.
Gerstman BB, Jolson HM, Bauer M, Cho P, Livingston JM, Platt R. The incidence of depression in new users of beta-blockers and selected antihypertensives. J Clin Epidemiol. 1996;49:809–15.
Johansen A, Holmen J, Stewart R, Bjerkeset O. Anxiety and depression symptoms in arterial hypertension: the influence of antihypertensive treatment. the HUNT study, Norway. Eur J Epidemiol. 2012;27:63–72.
Michal M, Wiltink J, Lackner K, Wild PS, Zwiener I, Blettner M, et al. Association of hypertension with depression in the community: results from the Gutenberg Health Study. J Hypertens. 2013;31:893–9.
Ringoir L, Pedersen SS, Widdershoven JWMG, Pouwer F, Keyzer JML, Romeijnders AC, et al. Beta-blockers and depression in elderly hypertension patients in primary care. Fam Med. 2014;46:447–53.
Simonson W, Han LF, Davidson HE. Hypertension treatment and outcomes in US nursing homes: results from the US National Nursing Home Survey. J Am Med Dir Assoc. 2011;12:44–9.
Author information
Authors and Affiliations
Contributions
This research project involved multiple contributors, each playing significant roles across various stages of the study. Jay Tewari, Khalid Ahmad Qidwai, Anadika Rana, Prof. Vineeta Tewari, Dr. Ajoy Tewari, Vanshika Singh, Rishabh Tiwari, Prof. Anuj Maheshwari, Prof. Narsingh Verma, Dr. Himali Jha, and Savneet Kaur were involved in conceptualizing and designing the study. In the literature search phase, all contributors except for Dr. Himali Jha and Savneet Kaur participated. The definition of intellectual content was primarily done by Jay Tewari, Prof. Vineeta Tewari, Dr. Ajoy Tewari, Prof. Anuj Maheshwari, and Prof. Narsingh Verma. The analysis and interpretation of results were performed by all the contributors. Manuscript writing was carried out by Jay Tewari, Khalid Ahmad Qidwai, and Anadika Rana, with support from Dr. Himali Jha and Savneet Kaur. Critical appraisal of the manuscript was undertaken by Prof. Vineeta Tewari, Dr. Ajoy Tewari, Vanshika Singh, Prof. Anuj Maheshwari, and Prof. Narsingh Verma. Finally, all contributors held accountability for the manuscript, ensuring the integrity and accuracy of the research findings.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This is a systematic review and meta-analysis which needs no ethical approval. All the included studies had obtained ethical approval individually.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tewari, J., Qidwai, K.A., Tewari, A. et al. Association between antihypertensive drug use and the risk of depression: a systematic review and network meta-analysis. J Hum Hypertens 39, 246–253 (2025). https://doi.org/10.1038/s41371-025-01011-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-025-01011-x