Abstract
Haloperidol is used to manage psychotic symptoms in several neurological disorders through mechanisms that involve antagonism of dopamine D2 receptors that are highly expressed in the striatum. Significant side effects of haloperidol, known as extrapyramidal symptoms, lead to motor deficits similar to those seen in Parkinson’s disease and present a major challenge in clinical settings. The underlying molecular mechanisms responsible for these side effects remain poorly understood. Parkinson’s disease-associated leucine-rich repeat kinase 2 (LRRK2) has an essential role in striatal physiology and a known link to dopamine D2 receptor signaling. Here, we systematically explore convergent signaling of haloperidol and LRRK2 through pharmacological or genetic inhibition of LRRK2 kinase, as well as knock-in mouse models expressing pathogenic mutant LRRK2 with increased kinase activity. Behavioral assays show that LRRK2 kinase inhibition ameliorates haloperidol-induced motor changes in mice. A combination of electrophysiological and anatomical approaches reveals that LRRK2 kinase inhibition interferes with haloperidol-induced changes, specifically in striatal neurons of the indirect pathway. Proteomic studies and targeted intracellular pathway analyses demonstrate that haloperidol induces a similar pattern of intracellular signaling as increased LRRK2 kinase activity. Our study suggests that LRRK2 kinase plays a key role in striatal dopamine D2 receptor signaling underlying the undesirable motor side effects of haloperidol. This work opens up new therapeutic avenues for dopamine-related disorders, such as psychosis, also furthering our understanding of Parkinson’s disease pathophysiology.
Similar content being viewed by others
Introduction
Dopamine D2 receptors (D2Rs) are critical pharmacological targets for neuropsychiatric diseases such as schizophrenia and Parkinson’s disease (PD) [1, 2]. D2Rs are highly expressed in spiny projection neurons (SPNs) of the indirect striatal pathway (iSPNs), one of striatum’s two principal and functionally neuronal subtypes—indirect striatal pathway, together with the direct striatal pathway, controls movement [3,4,5,6]. D2Rs inhibit cAMP production by coupling with Gi/o and, as a result, reduce protein kinase A (PKA) signaling [7]. These intracellular events mediated by D2R signaling pathways significantly impact the physiological functions of iSPNs at both cell-intrinsic and network levels [8,9,10].
D2Rs are known targets of all antipsychotics [11]. Haloperidol, an antagonist of D2Rs, is a first-generation typical antipsychotic that is still widely used to treat various neuropsychiatric diseases [12]. However, it can cause major side effects, including severe motor deficits that mimic PD symptoms, collectively known as extrapyramidal motor symptoms [13, 14]. In rodents, haloperidol administration induces catalepsy, a state of inhibited movement that results from the blockade of D2 receptors in the nigrostriatal pathway [15, 16]. While the side effect profile of this otherwise effective antipsychotic presents a significant challenge in the clinic, details of the signaling cascades and neural circuit adaptations that lead to haloperidol-induced motor deficits remain elusive. Developing efficient and safer therapies for treating D2R-related disorders remains challenging due to the heterogeneous expression of D2R across cell types and diverse cascades downstream of D2R.
PD is a disorder characterized by the loss of the nigrostriatal dopamine neurons, which results in significant motor deficits. Variants of several genes have been linked to familial PD, with the kinase LRRK2 being particularly interesting due to its association with both familial and idiopathic PD [17,18,19]. Previous studies have found that, in the striatum, LRRK2 is highly expressed in SPNs and plays a crucial role in regulating the striatal function [20,21,22,23,24,25,26] including via modulation of D2R signaling [27,28,29]. Pathogenic PD-associated LRRK2 mutations lead to kinase hyperactivity [30, 31], suggesting that LRRK2 activity is important in the pathophysiological mechanisms of PD. Thus, animal models carrying human-disease-linked LRRK2 mutations can be used as a genetic proxy to understand the consequences of enhanced kinase activity on striatal neuronal signaling, structure, and function.
The most etiologically relevant knock-in (KI) mice expressing pathogenic LRRK2 mutations exhibit either normal or moderately altered motor behaviors [32,33,34]. However, perturbation of D2R signaling in these animals unmasks motor phenotypes. Impairment of striatal motor learning as a result of D2R antagonism is enhanced by LRRK2 mutations [23]. Conversely, impairment of locomotor activity by activation of D2R signaling is partially ameliorated in LRRK2 KI mice [34]. Although LRRK2 activity and D2R signaling appear as convergent themes across different studies and genetic models, a coherent synthesis of these results, accounting for variability in model design, D2R manipulation, and technical approaches, is currently lacking.
The current study aims to understand how LRRK2 modulates the effects of haloperidol on the behavioral, physiological, and molecular changes downstream of D2R antagonism in the striatum. To achieve this, we use a combination of behavioral tests, whole-cell electrophysiology, proteomic and phosphoproteomic analyses as well as transcript level measurements in concert with pharmacological and genetic manipulations of LRRK2 activity. Our research demonstrates a critical role for LRRK2 kinase activity in haloperidol-induced motor changes. We find that inhibition of LRRK2 kinase activity can alleviate these motor side effects, paralleled by a reversal of both structural and functional indirect pathway changes induced by haloperidol. Conversely, LRRK2 hyperactivity, the result of PD-linked pathogenic mutations, mimics the molecular and biochemical effects of haloperidol on striatal intracellular signaling. Overall, our work opens new directions for the therapeutic management of psychosis and helps to refine the pathological mechanisms relevant to PD.
Results
LRRK2 kinase activity mediates the effects of haloperidol on movement disruption
To examine the link between LRRK2 activity and motor behaviors sensitive to D2R signaling, we evaluated whether LRRK2 inhibition influences the effects of blocking D2R signaling by haloperidol. Haloperidol, a typical antipsychotic used to treat psychosis, is known to cause Parkinsonian-like side effects, including catalepsy in rodents and dyskinesia in humans [14]. We hypothesized that if LRRK2 kinase activity plays a significant role in D2R signaling in the striatum, its inhibition may interfere with the cataleptic response induced by haloperidol.
Wild-type (WT) mice were injected with a subchronic dose (1 mg/kg) of haloperidol or vehicle control for 7 days, followed by the measurement of their cataleptic response [15]. A potent and selective LRRK2 kinase inhibitor MLi-2 [35,36,37] was administered at 10 mg/kg daily [38] 30 min before haloperidol (Fig. 1A). Consistent with previous studies [16], seven days of haloperidol administration without LRRK2 inhibition induced a significant cataleptic response in WT mice, as measured by the bar test (p < 0.0001, Tukey’s multiple comparisons test after one-way ANOVA; n = 9–15 mice). MLi-2 itself did not affect catalepsy compared to vehicle control (p > 0.999 post-hocs, as noted, n = 8–9 mice). However, when haloperidol and MLi-2 were combined, the haloperidol-induced cataleptic response was significantly attenuated (p = 0.0030, Tukey’s multiple comparisons post-hoc after one-way ANOVA as noted, n = 13–15 mice) (Fig. 1B). To confirm that this MLi-2 administration was sufficient to decrease LRRK2 kinase activity in vivo, we measured phosphorylation of the Ser106 site of Rab12, a well-established measure of LRRK2 kinase activity [38, 39]. Consistent with reduced LRRK2 activity, MLi-2 administration resulted in decreased phosphorylation of Rab12 at Ser106, compared to vehicle controls (p = 0.0043 Tukey’s multiple comparisons test after one-way ANOVA; n = 6 mice (Supplementary Fig. 1A-B). Total Rab12 levels were found unaltered across treatments (p = 0.9994, Tukey’s multiple comparisons test after one-way ANOVA, Supplementary Fig. 1C).
A Schematic of the experiment and treatment schedule. Catalepsy was assessed with the bar test, and distance traveled was recorded in an open-field arena; both were performed 1 hr after the final treatment administration. Treatment conditions: Vehicle for MLi-2, 40% 2-hydroxypropyl-β-cyclodextrin; MLi2, 10 mg/kg; vehicle for PFE-360, 1.25% hydroxypropyl cellulose + 0.5% docusate sodium; PFE- 360, 5 mg/kg; vehicle for haloperidol, saline (0.9% NaCl); haloperidol, 1 mg/kg. Some schematics were created with BioRender.com. X-axis: vehicle = vehicle for MLi-2 + vehicle for haloperidol; haloperidol = vehicle for MLi-2 + haloperidol; MLi-2 or PFE-360 = MLi- 2 or PFE-360 + vehicle for haloperidol; MLi-2 or PFE-360 + haloperidol, as indicated. All drugs were administered intraperitoneally (i.p.) except MLi-2, PFE-360, and their vehicles, which were given orally. B Cataleptic response of WT mice receiving haloperidol, MLi-2, their combination, and vehicle controls for 7 days. N = 9, 15, 8, 13 mice, in order of groups presented. C Same as B, but using PFE-360 and its corresponding vehicle. N = 8, 9, 6, 6 mice, in order of groups presented. D Cataleptic response of LRRK2-WT and LRRK2-KO mice receiving haloperidol or control vehicle for 7 days. N = 11 mice for both genotypes. E Cataleptic response of Drd2fl/fl and Drd2fl/fl; Adora2acre mice receiving haloperidol for 7 days. N = 9 and 15 mice, respectively. F Distance traveled in the open-field test for WT mice receiving haloperidol or haloperidol + MLi-2. N = 8 and 9 mice, respectively. Data are represented as mean ± SEM. Asterisks in B, C show statistical significance for Tukey’s multiple comparison tests after one-way ANOVA; *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Asterisks in D–F show statistical significance for unpaired t-test comparison; **p < 0.01,***p < 0.001, ****p < 0.0001. Error bars as SEM.
To ensure that the observed effects were not limited to the pharmacology of the MLi-2 inhibitor, we treated mice with another potent and specific LRRK2 kinase inhibitor, PFE-360, that also crosses the blood-brain barrier [40, 41] following the same treatment schedule (Fig. 1A). PFE- 360 and MLi-2 have distinct structures and off-target profiles. PFE-360, like MLI-2, also reduced haloperidol-induced catalepsy in WT mice (p = 0.0024, Tukey’s multiple comparisons post-hoc after one-way ANOVA, n = 6–9 mice) (Fig. 1C). To further verify the relevance of LRRK2 kinase activity for haloperidol-induced catalepsy, we examined the effect of genetic ablation of LRRK2 on the motor side effects of haloperidol. Consistent with our pharmacological inhibition data, we found that catalepsy in haloperidol-treated LRRK2-KO mice was significantly lower than that in LRRK2-WT mice (p = 0.0002, unpaired t-test, n = 11 mice) (Fig. 1D).
Haloperidol has a strong affinity for D2Rs, but it lacks selectivity [42]. To determine if haloperidol-associated catalepsy is primarily the result of inhibition of D2R signaling in striatal iSPNs, we generated a mouse line where Drd2, which encodes the D2R, was selectively deleted in iSPNs (Drd2fl/fl). The cataleptic response of Drd2fl/fl mice was significantly reduced compared to littermate controls (p < 0.0001, unpaired t-test, n = 9–15) (Fig. 1E). These data suggest that LRRK2 contributes to the induction of catalepsy as a result of blockade of D2R signaling in iSPNs.
Next, to investigate if LRRK2 inhibition modulates haloperidol effects in a different motor behavior task, we assessed the locomotor behavior of mice in an open field arena after treatment with haloperidol and MLi-2. WT mice were treated for seven days with haloperidol, or haloperidol and MLi-2, with an open field test one hour after the final treatment. Treatment with haloperidol significantly reduced the total distance traveled (p < 0.0001, Tukey’s multiple comparisons test after one-way ANOVA, n = 8 mice), while MLi-2 alone had no effect on locomotion (p = 0.8803, Tukey’s multiple comparisons test after one-way ANOVA, n = 7–8) (Supplementary Fig. 1D). Co-administration of MLi-2 and haloperidol increased the distance traveled, compared to haloperidol alone (p = 0.0039, unpaired t-test, n = 8–9 mice, Fig. 1F). These findings suggest that motor behavior changes induced by subchronic haloperidol administration broadly involve LRRK2.
To better understand the time course of these behavioral effects, we tested the impact of LRRK2 kinase inhibitors on catalepsy after acute (60 min) and chronic (14 days) 1 mg/kg haloperidol administration. In both cases, WT mice were given combined treatments with MLi-2 or vehicle controls 30 min before haloperidol. Catalepsy was measured 1 hr after the last injection (Supplementary Fig. 1E). In line with previous studies, acute administration of haloperidol (1 mg/kg, 1 hr) induced catalepsy [15, 43, 44] as measured with a standard bar test, compared to vehicle controls (p < 0.0001, Tukey’s multiple comparisons post-hoc after one-way ANOVA, n = 5–15 mice) (Supplementary Fig. 1F). Co-administration of haloperidol and MLi-2 decreased the cataleptic response compared to haloperidol-treated mice (p = 0.021, Tukey’s multiple comparisons post-hoc after one-way ANOVA, n = 12–15 mice) (Supplementary Fig. 1F). This timing and dosing of MLi-2 co-administration was also sufficient to decrease the phosphorylation of LRRK2 downstream target p-Rab12 [38] (Supplementary Fig. 1H). In the chronic paradigm, we found that MLi- 2 had no effect on haloperidol-induced catalepsy after 14 days (p = 0.7328, Tukey’s multiple comparisons post-hoc after one-way ANOVA, n = 14–16 mice) (Supplementary Fig. 1G). This is likely due to developing tolerance to the cataleptic effects of the drug [16, 45]. Thus, MLi-2 is no longer effective at modulating the substantially declined cataleptic response (Supplementary Fig. 1I). Taken together; these results are consistent with a critical role of LRRK2 kinase in the events that underlie the motor disruption induced by D2R antagonism. Finally, no sex differences were found in treatment paradigms (Supplementary Fig. 2).
Several studies highlight the importance of dopamine D2R signaling in striatal motor learning [46,47,48], and our previous data report differences with LRRK2 mutations in the presence of D2R antagonists in striatal motor learning [23]. These observations suggest that LRRK2 may interfere with D2R signaling during skill acquisition. Therefore, we determined the impact of LRRK2 kinase activity on modulating the effects of haloperidol using the accelerating rotarod test. We assessed the latency to fall in WT mice treated with either haloperidol, MLi-2, or their controls for 14 days in an accelerated rotarod (Supplementary Fig. 3A). The average latency to fall improved towards the end of the task in the control-treated mice, treatment factor F3344 = 22.35, p < 0.0001, Session Factor F7344 = 7.553, p < 0.0001. Treatment x session interaction F21,344 = 0.8274, p = 0.6857, Tukey’s multiple comparisons test after two-way ANOVA, vehicle, n = 10; haloperidol, n = 10; MLi2, n = 16; MLi2 + haloperidol, n = 11. (Supplementary Fig. 3B) Haloperidol significantly decreased the latency to fall, compared to vehicle controls over the last three sessions of the test (p < 0.001, Tukey’s multiple comparisons post-hoc after one-way ANOVA). This decrease was prevented in mice co-administered with the LRRK2 kinase inhibitor MLi-2 (p = 0.0011, Tukey’s multiple comparisons after one-way ANOVA) (Supplementary Fig. 3C). Our observations suggest that LRRK2 interferes with haloperidol- mediated effects on striatal motor learning.
LRRK2 kinase activity regulates haloperidol-induced adaptations in striatal indirect pathway circuits
Haloperidol is reported to induce a series of homeostatic synaptic and intrinsic adaptations primarily in the indirect pathway circuits [16, 49,50,51,52]. These adaptations include dendritic spine loss in iSPNs, which occurs after 5 days and persists for up to 14 days of daily treatment (Fig. 2A) (synaptic adaptations). Additionally, a decrease in the excitability of iSPNs has been observed after 14 days of haloperidol administration, which is thought to reflect an intrinsic homeostatic change aimed at normalizing the persistent increase in firing rate after D2R antagonism (Fig. 2A) (intrinsic adaptations) [16, 53]. The cataleptic tolerance (e.g., decreased response to haloperidol over time) [45] between sub-chronic (5 days) and chronic (14 days) haloperidol treatment, described above, has been suggested to reflect remodeling of the indirect pathway circuits [16]. However, the exact intrinsic and network changes underlying these processes remain largely unknown.
A Schematic of the proposed timeline for synaptic and cell-intrinsic adaptations with haloperidol treatment based on a synthesis of current and prior findings. Some of the schematics were created with BioRender.com. B Cataleptic response of WT mice receiving haloperidol, or haloperidol + MLi-2, at 7 and 14 days following treatments. Haloperidol-treated mice develop tolerance to catalepsy after 14 but not 7 days of haloperidol administration. N = 15, 14, 13, 16 mice, in order of groups presented. The 7- and 14-day regimen data are from panels 1B and Supplementary Fig. 1G, respectively. C Left, Example of confocal maximum projection image of an Adora2aCre SPN expressing AAV5/DIO-EGFP. Scale bar = 15 μm. Right, Examples of dendritic segments in different treatment conditions. Scale bar = 10 μm. D Summary graph of dendritic spine density in iSPNs across treatments. N = 14–20 cells, 3 mice/group. E Example current clamp recording traces in response to a 150 pA current injection in iSPNs of WT mice after 14 days of treatment, as noted. Recordings were performed 24–48 h after the final injection. Insets: scale 4 mV, 20 ms. F Summary data show decreased cellular excitability with haloperidol, rescued to control levels by LRRK2 inhibition. Scale, as noted. N = 14–29 cells, 3–6 mice/condition. Data are represented as mean ± SEM. Asterisks in B show statistical significance for Tukey’s multiple comparison tests after two-way ANOVA; *p < 0.05. D shows statistical significance for Tukey’s multiple comparison tests after one-way ANOVA **p < 0.01, ****, p < 0.0001. Asterisks in F show statistical significance after two-way ANOVA with multiple comparisons. Large asterisk, interaction between treatment and current steps. Small asterisks, significance at specific current steps, determined by Sidak multiple comparisons. *p < 0.05, **p < 0.01, ***p < 0.001. Error bars as SEM.
The timeline of effects of LRRK2 inhibition on the cataleptic response (7 days of treatment) correlates with a time when synaptic adaptations in the iSPNs have started to occur. Moreover, although the cataleptic tolerance progressively increased from 7–14 days in haloperidol-treated WT mice (p = 0.0226, Tukey’s multiple comparisons test comparisons test after two-way ANOVA), no difference in haloperidol-induced catalepsy was observed in the MLi-2-treated mice between 7 and 14 days (Fig. 2B), suggesting that LRRK2 kinase activity interferes with the well-orchestrated changes in iSPNs pathways after haloperidol treatment. Thus, we examined the haloperidol-induced dendritic spine density patterns in iSPNs after 7 days of treatment. We identified iSPNs by injecting a Cre-dependent adeno-associated virus (AAV) expressing eGFP (AAV5/DIO-EGFP) in the striatum of Adora2aCre mice (Fig. 2C, Supplementary Fig. 4). Consistent with previous reports [16], we found that haloperidol decreased dendritic spines density on iSPNs, compared to the vehicle control (p < 0.0001, Tukey’s multiple comparisons test after one way ANOVA, n = 14–20 iSPNs), (Fig. 2C, D). Co-administration of MLi-2 and haloperidol increased dendritic spine density in iSPNs, compared to iSPNs after haloperidol alone (p = 0.0042, Tukey’s multiple comparisons test after one-way ANOVA, n = 14–20 iSPNs), (Fig. 2C, D). Thus, LRRK2 kinase activity is involved in the synaptic changes in iSPN circuits following haloperidol, consistent with a well-described role for LRRK2 in dendritic spine morphogenesis through actin cytoskeleton regulation.
To better understand LRRK2 effects on intrinsic iSPNs adaptations, Drd2-eGFP BAC reporter mice were injected with haloperidol, haloperidol + MLi-2, or vehicle controls for 14 days. Then, we performed whole-cell current-clamp recordings on identified iSPNs in ex vivo striatal slices (Fig. 2E). Our findings are in line with a previous study [16] that showed a decrease in iSPNs excitability due to haloperidol (treatment group by current interaction, p = 0.0001, 2-way ANOVA with Sidak multiple comparisons, n = 4–6 animals, n = 14–24 iSPNs). Significantly, co-administration of MLi-2 with haloperidol restored the firing of iSPNs to wild-type levels (p = 0.9506, 2-way ANOVA with multiple comparisons, n = 3–6 animals, 14–29 iSPNs) (Fig. 2E, F). However, we did not find notable differences in other membrane properties or the frequency of synaptic activity as assessed by excitatory postsynaptic potentials of iSPNs (Supplementary Fig. 5). Our results indicate that LRRK2 kinase activity is involved in synaptic and intrinsic changes in iSPN circuits after haloperidol treatment.
Haloperidol administration mimics the phosphoproteomic landscape of the LRRK2 G2019S mutation in the striatum
Previous studies have shown that the phosphorylation of ribosomal protein S6 (p-rpS6) at S235/236 residues increases in iSPNs in response to haloperidol activation [54, 55]. This phosphorylation is cAMP/PKA dependent, which is the canonical pathway inhibited by D2R antagonism. We therefore explored whether LRRK2 inhibition interferes with this haloperidol-mediated phosphorylation event.
Mice expressing the eGFP under the Drd2 promoter were treated with haloperidol, MLi-2, haloperidol plus MLi-2, or vehicle controls for 7 days (Supplementary Fig. 6A), and double immunofluorescence experiments in striatal sections using antibodies against the p-rpS6 and GFP (for iSPNs) were performed. As expected, haloperidol increased the percentage of pS6-Ser235/236 positive iSPNs in striatal sections (p < 0.0001, Tukey’s multiple comparisons test after one-way ANOVA, n = 21–22 sections). In mice treated with both MLi-2 and haloperidol, the number of p-rpS6 GFP + neurons was significantly lower than in mice treated only with haloperidol and similar to vehicle controls (p = 0.2311, Tukey’s multiple comparisons test after one-way ANOVA, n = 18–22 sections) and (p = 0.0019, Tukey’s multiple comparisons test after one-way ANOVA, n = 18–21 sections), (Supplementary Fig. 6B). These results indicate that inhibiting LRRK2 kinase activity blunts the intracellular response to haloperidol, which correlates with the observed improvement in haloperidol-induced behavioral responses in the presence of LRRK2 kinase inhibitors.
To confirm that the inhibition of the LRRK2 kinase affects D2R signaling through PKA, WT mice were treated acutely with either haloperidol, MLi-2, a combination of haloperidol and MLi-2, or vehicle controls, as shown in Fig. 1A. Western blot analysis of striatal extracts was performed using an antibody that detects phosphorylated PKA substrates, which recognizes all PKA substrates present in the lysate. Haloperidol increased the p-PKA signal (p = 0.049), whereas MLi-2 reversed the increase in p-PKA signaling (p = 0.0373), similar to the control (p = 0.994); p-value after Tukey’s multiple comparisons after one way ANOVA, n = 9 mice/condition. (Supplementary Fig. 6C-D).
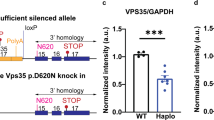
Since LRRK2 kinase inhibition reduces the intracellular response to haloperidol, we predicted that hyperactive mutant LRRK2 should mimic haloperidol-induced molecular alterations in WT mice. To test this hypothesis, we conducted unbiased proteomic characterization in the striatum, using mice expressing the G2019S (GS) mutation of LRRK2, which increases its kinase activity. We acutely (1 h) administered haloperidol or vehicle to WT and GS KI mice, extracting striatal samples for quantitative total and phosphoproteomic analyses (Fig. 3A). Our proteomic analysis detected 3997 proteins, while the phosphoproteomic analysis detected 9399 phosphopeptides mapping to 3010 unique proteins. For phosphoproteomics, the log2 intensity level of each phospho-peptide was normalized over the log2 intensity level of the total corresponding protein. We first compared haloperidol and vehicle-treated WT mice, and we found 252 phosphopeptides that were differentially regulated (p-value < 0.05, & |Log2 fold change (FC)| > 2) (Fig. 3B). Gene set enrichment analysis (GSEA) of the KEGG pathway set was conducted on genes containing at least one significantly altered phosphopeptide. Several KEGG pathways were found to be differentially regulated, including glutamatergic synapses, cAMP signaling, and actin dynamics (Fig. 3C). These processes have been previously linked to the effects of haloperidol on the striatum [54, 56,57,58,59]. Several of the observed differentially altered pathways, such as cAMP/PKA signaling and the regulation of actin cytoskeleton, represent established roles for LRRK2 function [20, 26, 60]. Specifically, LRRK2’s involvement in regulating actin cytoskeleton, which underlies dendritic spine morphogenesis, has been well-established [61,62,63,64,65]. We have previously shown that LRRK2 directs synaptogenesis via a PKA-mediated mechanism [20]. Further ontology analyses of significant phosphopeptides supported the enrichment of cytoskeletal and postsynaptic organization-associated pathways (Supplementary Fig. 7A).
A Schematic of experimental procedures. WT and GS mutant mice were treated with haloperidol or vehicle, and striatal samples were harvested after 1 h. LC-MS/MS analyses for total proteins and phosphopeptides were conducted on the same striatal samples. N = 3 mice/group. Parts of the schematic were created with BioRender.com. B Volcano plot comparing the phosphopeptides between haloperidol and vehicle-treated WT mice. Phosphopeptides that are significantly differentially regulated (|Log2FC| > 2 and unadjusted p-value ≤ 0.05 by multiple unpaired t-tests) are colored red and blue for up- and down-regulated, respectively. C Gene Set Enrichment Analysis (GSEA) results of the KEGG gene set for genes with at least one differentially regulated phosphopeptide in WT haloperidol vs vehicle-treated comparison. Pathways displayed are significantly differently regulated (adjusted p-value ≤ 0.05 by Fisher’s test). The length of bars reflects the number of genes in the pathway whose phosphostate is differentially regulated; bars are shaded by adjusted p-value. Highlighted pathways are related to established LRRK2 functions. D Diagram of genetic and pharmacological conditions for groups analyzed in E. Created with BioRender.com. E Heatmap of effect size (Log2FC) of either haloperidol treatment or LRRK2-GS for all differentially abundant phosphopeptides in the WT haloperidol-treated vs vehicle-treated comparison (|Log2FC| > 2 and unadjusted p-value ≤ 0.05 by multiple unpaired t-tests. Each bar represents a phosphopeptide. Color reflects Log2FC difference from WT saline condition. F Correlation plot for E, comparing GS vehicle/WT vehicle to WT haloperidol-vehicle effect size. All detected phosphopeptides were mapped, and phosphopeptides significantly altered between WT haloperidol vs. vehicle are highlighted. Only highlighted values are used for correlation calculation. Blue line represents the line of best fit. modalities downstream of D2R.
These findings suggest that haloperidol-induced motor changes involve modulation of LRRK2 kinase activity. Further supporting this model, phosphopeptides found to be differentially abundant in haloperidol-treated vs. vehicle-treated WT mice show changes similar in direction and magnitude as phosphopeptides differentially abundant in vehicle-treated LRRK2 GS vs. WT mice (Fig. 3D, E), with a strong correlation of effect size (Fig. 3F). These results indicate that haloperidol treatment results in similar phosphoregulation patterns in the striatum compared to those caused by hyperactive LRRK2. While the phosphoproteomic changes resulting from haloperidol treatment were almost wholly reflected in the changes as a result of hyperactive LRRK2, there was a large population of phosphopeptides that were significantly differentially regulated in the GS mice but unchanged as a result of haloperidol treatment (Supplementary Fig. 7B). This suggests that chronic hyperactivity of LRRK2 in GS mice results in more profound phosphorylation restructuring and reflects broader functions related to the LRRK2 kinase as compared to the changes observed upon transient administration of antipsychotic D2R antagonists. In contrast to the phosphoproteomic data, analysis of changes in total protein levels between wild-type mice treated with haloperidol and vehicle uncovered very few differentially expressed proteins (Supplementary Fig. 7C). These significantly altered proteins did not show similar changes in expression in vehicle-treated LRRK2-GS mice compared to WT (Supplementary Fig. 7D). Finally, a moderate effect of haloperidol on the phosphoproteome was observed when comparing vehicle-treated and haloperidol-treated LRRK2-GS mice (Supplementary Fig. 7E), consistent with the idea that haloperidol mimics LRRK2 hyperactivity. These results demonstrate that haloperidol administration primarily impacts striatal phosphostate due to changes in intracellular signaling, with LRRK2 kinase activity playing a key role in this state transition.
LRRK2 regulates haloperidol mediated upregulation of immediate early genes
Antipsychotics induce the expression of several immediate early genes (IEGs) via D2R antagonism, which then leads to changes in critical signaling pathways in iSPNs [66, 67]. Although the exact intracellular pathways leading to this upregulation are unclear, it is known that D2R blockade by haloperidol increases the activity of PKA (Fig. 4A). This then causes CREB to be phosphorylated, allowing it to bind to various IEG promoters to induce transcription [54, 55, 68, 69].
A Signaling cascades leading to IEGs upregulation in iSPNs. D2R antagonist (haloperidol) releases the inhibition of cAMP and activates PKA, leading to upregulation of IEGs (canonical pathway). D2R blockade prevents the reduction of AKT activity, increasing GSK3β phosphorylation/inactivation. Inhibition of GSK3β elicits IEG expression. Created with BioRender.com. B Example confocal images of Nr4a1 gene expression in the striatum of LRRK2-WT mice treated with haloperidol (1 mg/kg, for 1 h) or vehicle and LRRK2-GS mice treated with vehicle. Scale bar = 500 μm. C Same as B, but high-magnification images depicting Nr4a1 expression. Scale bar = 10 μm. D Comparison of mean puncta/cell of Nra41 in Drd2-positive nuclei of LRRK2-WT mice treated with haloperidol or vehicle and LRRK2-GS mice treated with vehicle. Each dot represents the average number of Nra41 positive cells from one striatal section, n = 6–9 sections/3–4 mice. The number of Nr4a1 + /Drd2 + positive cells across WT and GS mice does not differ (Tukey’s multiple comparison tests after two-way ANOVA). E Comparison of mean puncta/cell of Nra41 in Drd1-positive nuclei of LRRK2-WT mice and LRRK2-GS mice treated with vehicle. Each dot represents the average number of Nra41 positive cells from one striatal section, n = 6–7 sections/3 mice. The number of Nr4a1 + /Drd1 + positive cells across WT and GS mice does not differ (unpaired t-test). F Quantification of Nra41-positive Drd2 nuclei in LRRK2-GS mice administered vehicle, MLi2 (10 mg/kg), PFE-360 (5 mg/kg), D2R agonist quinpirole (1 mg/kg), as well as LRRK2-KO mice treated with vehicle for 2 h. N = 4–8 sections/2–4 mice. Data are represented as mean ± SEM. Asterisks in F reflect statistical significance for Tukey post-hoc comparisons after one-way ANOVA. * p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Error bars as SEM.
Nuclear receptor subfamily 4 group A member 1 (Nr4a1) is a transcription factor and IEG that is strongly upregulated in the iSPNs of the dorsolateral striatum after haloperidol treatment [70, 71]. Since the dorsolateral striatum is crucial for motor control, the upregulation of Nr4a1 after haloperidol administration may be associated with subsequent motor side effects. Indeed, genetic loss of Nr4a1 leads to the complete blockade of haloperidol-induced catalepsy [72].
Therefore, we explored whether LRRK2 kinase is part of the intracellular signaling cascade downstream of D2R that leads to haloperidol-mediated Nr4a1 induction. To define the impact of LRRK2 kinase activity on the expression pattern of Nr4a1 mRNA in the iSPNs, we used multicolored single-molecule fluorescence in situ hybridization. In addition to comparing WT to LRRK2-GS iSPNs, we compared WT mice to those treated with haloperidol (Fig. 4B, C). Consistent with previous work [71], we found an upregulation of Nr4a1 in the iSPNs of WT mice upon haloperidol administration, defined by the number of Nr4a1 puncta per iSPN (p = 0.0002, Tukey’s multiple comparisons test after one-way ANOVA, n = 6–9 sections). Similarly, we observed increased Nr4a1 + puncta in GS iSPNs compared to the WT controls (p = 0.0018, Tukey’s multiple comparisons test after one-way ANOVA, n = 7–9 sections) (Fig. 4D). In contrast, we found no difference in the number of Nr4a1 puncta in the dopamine D1 receptor (D1R)-expressing SPNs in LRRK2-GS mice (p = 0.8193, unpaired t-test, n = 6–7 sections, Fig. 4E), indicating a pathway-specific effect. Two different LRRK2 kinase inhibitors, MLi-2 and PFE-360, were separately delivered orally to GS KI mice (2 h). This restored (decreased) the Nr4a1 expression in LRRK2-GS mice, compared to vehicle controls (p = 0.0237 MLI-2, p = 0.0003 PFE-360, Tukey’s multiple comparisons test after one-way ANOVA n = 4–8 sections, Fig. 4F). Moreover, the number of Nr4a1 + puncta in iSPNs of vehicle-treated LRRK2-KO mice was decreased, compared to LRRK2-GS vehicle-treated mice (p = 0.0019, Tukey’s multiple comparisons test after one-way ANOVA n = 6–7 sections, Fig. 4F). To assess whether decreased D2R signaling mediates the enhanced Nr4a1 mRNA levels in LRRK2-GS iSPNs, we systematically administered the D2R agonist quinpirole. D2R stimulation decreased the levels of Nr4a1 in LRRK2-GS iSPNs (p < 0.0001, Tukey’s multiple comparisons test after one-way ANOVA, n = 6–7 sections) compared to vehicle controls (Fig. 4F). These results demonstrate a LRRK2 kinase-mediated and D2R signaling-dependent upregulation of Nr4a1 in the LRRK2-GS iSPNs.
If LRRK2 regulates IEG expression through modulation of the D2R signaling, the effects of increased LRRK2 kinase activity should be generalizable for any IEG that responds to D2R signaling, even across IEGs that encode proteins with diverse functions. In addition to the expression levels of Nr4a1, which encodes a transcription factor, we examined the number of Arc (encoding a dendritic spine protein) positive puncta in iSPNs of LRRK2-GS mice and WT mice treated with haloperidol (Supplementary Fig. 8A). Using in situ hybridization, we found an increase in Arc-positive puncta in the iSPNs of haloperidol- treated compared to vehicle-treated WT mice (p = 0.0056, Tukey’s multiple comparisons test after one-way ANOVA n = 4–7 sections) (Supplementary Fig. 8B). We also observed higher Arc + puncta in iSPNs from LRRK2-GS, compared to WT (p = 0.0002, Tukey’s multiple comparisons test after one-way ANOVA as noted in Supplementary Fig. 8B, n = 4–7 sections). To determine whether this increase is LRRK2 kinase-dependent, we treated LRRK2-GS mice with the kinase inhibitor MLi-2, which decreased the Arc RNA levels, compared to vehicle-treated LRRK2-GS iSPNs (p = 0.0101, Tukey’s multiple comparisons test after one-way ANOVA, n = 6–7 sections), (Supplementary Fig. 8C). Moreover, we found that LRRK2- KO iSPNs had less Arc + puncta/cell than LRRK2-GS iSPNs (p = 0.0251, Tukey’s multiple comparisons test after one-way ANOVA, n = 6–7 sections), (Supplementary Fig. 8C). Together, our data show that–similar to haloperidol treatment–genetically increased LRRK2 kinase activity results in a D2R-dependent upregulation of several IEGs, which reflects a broad effect of LRRK2 on signaling modalities downstream of D2R.
Discussion
This study shows that LRRK2 kinase activity is involved in D2R-mediated motor behaviors and their modulation by antipsychotic D2R antagonism. We employed both pharmacological (potent and specific LRRK2 kinase inhibitors) and genetic (LRRK2-KO and LRRK2-GS KI mice) models to modulate levels of LRRK2 kinase activity. We demonstrated that pharmacological or genetic inhibition of LRRK2 kinase activity attenuates the behavioral, electrophysiological, and synaptic effects of haloperidol administration. Furthermore, we characterized the proteomic and phosphoproteomic changes induced by haloperidol treatment in the striatum and found the impact of increased LRRK2 kinase activity mirrored them. In addition, increased LRRK2 kinase activity contributed to intracellular pathway responses of iSPNs to haloperidol treatment. Our study suggests that LRRK2 kinase activity is involved in critical D2R-mediated signaling events, broadly relevant to PD pathophysiology. Furthermore, our results highlight the potential of LRRK2 inhibitors to ameliorate extrapyramidal motor side effects of D2-antagonistic antipsychotics.
Converging effects of haloperidol and LRRK2 kinase activity on changes in striatal indirect pathway behavioral and anatomical insights
We observed that catalepsy and reduced locomotion induced by haloperidol treatment were attenuated in the presence of pharmacological or genetic LRRK2 inhibition (Fig. 1). Although we cannot rule out the potential effects of LRRK2 on other D2R-[55] or D1R-expressing [73] striatal subpopulations, our findings show that knockout of the long isoform of D2R [15], which is predominantly expressed in iSPNs, decreases substantially the cataleptic response to haloperidol. This demonstrates a critical contribution of D2R signaling in iSPNs to the cataleptic response.
Haloperidol has been shown to induce synaptic changes in the indirect striatal pathway, including a decrease in the density of dendritic spines [16]. Our data replicate these findings and demonstrate that this decrease is partially restored by inhibiting LRRK2 (Fig. 2). LRRK2 plays a crucial role in dendritic spine morphogenesis, through PKA-dependent regulation of the actin cytoskeleton [20]. Actin-dependent remodeling of dendritic spines as a result of haloperidol administration is supported by our phosphoproteomic data, which showed significant alterations in the phosphostate of actin cytoskeletal-related proteins with important roles in dendritic spine formation, such as drebrin, cofilin, and neurabin after haloperidol treatment. Altogether, our results suggest that LRRK2 and haloperidol converge on regulating actin remodeling as a functional downstream effect of D2R antagonism.
Despite a decrease in the density of dendritic spines after haloperidol treatment (Fig. 2), we noted a small but significant increase in the frequency of spontaneous EPSPs. These findings are consistent with previous reports [16, 56] and indicate that the effects of haloperidol on striatal neurons are complex. Future work is warranted to determine the mechanisms underlying the structure-function relationships of these findings.
Molecular mechanisms
Unbiased phosphoproteomics in striatal extracts from haloperidol-treated mice revealed changes in phosphoregulation of cAMP/PKA signaling-linked pathways, which are the canonical pathways downstream of D2R activation. Although the study was conducted on the whole striatum without selectivity for iSPNs, we observed changes in proteins linked to actin cytoskeleton dynamics and glutamatergic synapses (Fig. 3). These findings align with structural and functional changes previously reported to result from haloperidol treatment in corticostriatal glutamatergic synapses [16, 52]. Our findings showed a larger magnitude of phosphoproteomic changes compared to a largely stable proteome. This stands in contrast to prior findings reporting substantial proteomic changes as a result of haloperidol treatment [56]. These differences are likely due to the temporal dynamics of haloperidol administration in each study. We chose acute treatment to capture the initial signaling dynamics following D2R antagonism, as this is where phosphoregulation by LRRK2 kinase is expected to be involved. In contrast, Santa and colleagues employed a 30-day chronic haloperidol treatment paradigm. Our combined findings suggest that phosphoproteomic alterations precede the subsequent reshaping of the proteomic landscape that occurs with continued haloperidol treatment.
Although we cannot currently understand how LRRK2 kinase activity phenocopies the effects of haloperidol treatment, our data point to convergent alterations in signaling downstream of D2Rs. Haloperidol-induced D2R inhibition increases cAMP production and enhances PKA activity. Our prior work indicates that pathogenic LRRK2 can also increase PKA activity. We provide evidence that LRRK2 kinase activity is involved in increased PKA signaling following haloperidol treatment (Supplementary Fig. 6). Therefore, both haloperidol and increased LRRK2 kinase activity converge to elevate PKA activity. Alternatively, LRRK2 activity has been shown to impact the intracellular trafficking of D2Rs [74], which in this manner may mimic the downstream intracellular cascades that are affected by the direct action/blockade of antipsychotics on D2Rs. In addition, we find that expression of the hyperactive LRRK2-GS mutation mimics the increase in IEG mRNAs such as Nr4a1 and Arc in iSPNs (Fig. 4). This may directly contribute to the cataleptic tolerance upon LRRK2 kinase inhibition since Nr41a1 knockout mice have been shown to have a blunted cataleptic response [72].
Immediate early gene expression responds to PKA activity [75]. LRRK2 increases PKA activity, leading to IEGs increased expression. A selective increase in PKA activity in LRRK2 iSPNs does not correlate with differences in LRRK2 levels [76], which are similar across dSPNs and iSPNs; this likely indicates altered cAMP/PKA-mediated signaling events downstream of the D2R specific to iSPNs and altered with LRRK2 mutations.
The selective induction of IEGs in the GS mice is a striking example of a pathway-specific signaling effect, in line with our previous anatomical, physiological, and behavioral studies that support pathway-specific effects of LRRK2 [23, 26].
Clinical implications
Our study shows that inhibiting LRRK2 kinase activity decreases locomotor deficits as a result of D2R antagonism via haloperidol treatment. This finding has two significant clinical implications. First, under conditions of increased kinase activity, such as in individuals with GS mutations, stimulation of D2R signaling may act to reverse the negative pathological effects of hyperactive LRRK2. Our data show that quinpirole, a D2R agonist, attenuates the increased expression of IEGs in GS iSPNs (Fig. 4). This is consistent with other studies showing that stimulation of D2R signaling is beneficial in the context of enhanced LRRK2 kinase activity [27, 28] with significant implications on the clinical use of DA agonists in PD [77]. Second, LRRK2 kinase inhibition may ameliorate the serious Parkinsonian-like motor phenotypes induced by haloperidol. Our data suggest a framework by which LRRK2 kinase inhibition [78] or anti-sense oligonucleotides to LRRK2 [79], both of which are currently in clinical development, could be used as adjuncts to antipsychotics. This is a viable therapeutic opportunity as LRRK2 loss of function variants in humans are not associated with disease state or dysfunction [80]. It remains to be determined whether LRRK2 kinase activity is relevant to the therapeutic benefits of haloperidol. The delayed clinical effect of haloperidol (weeks or months) suggests that it ameliorates psychotic symptoms through mechanisms beyond the acute blockade of D2R, potentially involving network-level adaptations [81, 82]. Investigating the effects of LRRK2 inhibition on the complex and less well-understood effect of haloperidol on the positive symptoms of schizophrenia would be valuable in future studies. Our work is an important step in understanding the neurobiology of dopamine-related disorders and their connection with motor symptoms, paving the way for more effective therapeutics for these neurological conditions.
Materials and methods
Animals
All experiments were in compliance with National Institutes of Health guidelines and were reviewed by the Northwestern Animal Care and Use Committee. P28–P35 male and female mice were used in all experiments. The effect of sex for key behavioral experiments is summarized in Supplementary Fig. 2. Mice were group-housed on a standard 12/12 h light/dark cycle with standard feeding. Littermates were randomly assigned to the experimental procedures. C57BL/6 and heterozygous KI mice expressing the LRRK2-GS pathogenic mutation [33] referred to as LRRK2-GS, as well as homozygous LRRK2-KO mice [64] were from Jackson Laboratory. BAC transgenic mice in which dopamine receptor D2 Drd2 drives EGFP expression regulatory elements (GENSAT) [81], referred to as Drd2-eGFP, allow the visual identification of these SPNs for electrophysiological (Fig. 2) and immunofluorescence studies (Supplementary Fig. 6). These mice crossed with LRRK2-GS KI mice were used in heterozygosity in all experiments. GENSAT generated [83] Adora2a (KG139) BAC mice which express Cre recombinase under the control of the Adenosine A2a receptor promoter (Adora2aCre) were crossed to a mouse line with loxP sites flanking exon dopamine receptor D2 (Drd2) gene, referred to as Drd2fl/fl mice [84] and used in behavioral tests (Fig. 1) Conditional expression of fluorescent proteins in Adora2aCre (iSPNs)-containing neurons for dendritic spines analysis (Fig. 2) was achieved using adeno-associated viruses encoding a double-floxed inverted open reading frame (DIO) of eGFP referred to as AAV-DIO-EGFP. The Cre + mice used were heterozygous. All mice were backcrossed several generations and maintained on a C57BL/6J background. Standard genotyping primers are available on the Jackson Lab or MMRC website. All animals were genotyped according to the Jackson Laboratory or MMRRC strain-specific primers and protocols. Details about the mouse strains are in the resources table (Supplementary Table 1). Age matched mice were randomly selected for all experimental procedures. Researcher blinding was conducted across experiments.
Drugs and treatment dosing
Haloperidol (1 mg/Kg) was dissolved in 0.05% acetic acid in saline (pH adjusted to 6.0 with NaOH), and quinpirole (1 mg/kg) was dissolved in saline. Both drugs and corresponding vehicle controls were administered intraperitoneally (i.p). Mli-2 (10 mg/Kg) was dissolved in 40% (w/v) Hydroxypropyl-β-Cyclodextran, and PFE-360 (5 mg/Kg) in 1.25% hydroxypropyl cellulose + 0.5% docusate sodium. Mli-2, PFE360, and their vehicle controls were administered via oral gavage. Drugs and all reagents used are detailed in the Resources Table, along with identification numbers when applicable. Males or females from the same litter were randomly assigned to different control and treatment groups.
Acute treatments
Mice were given a dose of MLi-2 or PFE-360 or vehicles via oral gavage 30 min before i.p. haloperidol injections or its vehicle for an hour. At this time point, the mice were euthanized for subsequent behavioral (Fig. 1), immunoblotting (Supplementary Fig. 1), mass spectrometry (haloperidol for 1 h) (Fig. 3) or in situ hybridization (Fig. 4) studies. Quinpirole was administered for 1 h (Fig. 4).
7- and 14-day treatments
Mice were administered haloperidol following MLi-2 or PFE-360 as in the acute paradigm once a day for 7 or 14 days. They were euthanized for behavioral (Supplementary Fig. 1), immunoblotting (Supplementary Fig. 1), and immunofluorescence (Supplementary Fig. 5) studies 1 h after the last injection. The indicated experimental procedures for the haloperidol-mediated synaptic and intrinsic adaptations (Fig. 2) and the rotarod test in Supplementary Fig. 3 was performed 24 h after the last haloperidol injection.
Behavioral analyses
Bar test
Mice were gently removed from their home cage, and their forepaws were placed over a horizontal bar, 0.2 cm in diameter, fixed at a height of 4 cm above the working surface. The time a mouse remained immobile was measured in 3 trials, with the cut-off at 120 s [15]. The average of 3 trials was used for further statistical testing.
Open field
Mice were placed in 56 × 56 cm open-field arenas in noise-canceling boxes illuminated by dim red lights. The 20-min session started when mice were placed in the center of the arena. The LimeLight 5 (Actimetrics) software analyzed locomotor activity and reported it as distance traveled.
Rotarod
Motor learning was assessed with an accelerating rotarod. The task was done using a rotarod apparatus (Panlab) equipped with a mouse rod (3 cm diameter) and set to 4–40 rpm acceleration over 300 s. The task consisted of daily sessions (five trials per session; intertrial-interval = 15 s, max trial duration = 300 s). Following a 24-h break, mice were tested for 8 sessions.
Stereotaxic surgeries
Neonatal
For dendritic spine analysis in Fig. 2, C57BL/6 mice were crossed with Adora2aCre mice. Intracranial injections were performed as previously described [26, 85,86,87]. P4-5-day-old pups were cryoanesthetized and received ketoprofen for analgesia. They were placed on a cooling pad on a stereotaxic frame. 200 nl of the AAV-DIO-EGFP virus (7 × 10¹² vg/mL) were delivered into the dorsal striatum at a rate of 100 nl min−1 using Micro-4 controller (WPI). In order to ensure the dorsal striatum was targeted, the needle was placed 1 mm anterior to the midpoint between the ear and eye, 1.5 mm from the midline, and 1.8 mm ventral to the brain surface. The pups’ age and size determined slight adjustments in the coordinates. After the injection, the pups were warmed on a heating pad before returning to their home cages.
Confocal microscopy and dendritic spine analysis
Confocal images of fixed 80-um-thick brain sections of P30 pups injected with the AAV-DIO-EGFP (Fig. 2) were obtained with the Nikon A1R microscope. Fluorescence projection images of dendrites and the corresponding dendritic spines were acquired with a 60x oil immersion objective (NA = 1.4) at 0.1 um intervals with 1024 × 1024 pixel resolution. Based on our prior experience, 3 or more segments per neuron 5 or more neurons from 2 or more mice is suitable for an experimental condition. For each group, 2–4 segments per neuron 5–9 neurons from 2–3 animals were used to generate z-stacks. Segments from secondary and tertiary dendrites without overlap with other neurons or discontinuities were chosen for analysis. Dendritic spine density was assessed using Imaris 10.1 software (Bitplane, Concord, USA). Images of dendritic segments were traced using autopath mode of the filament tracer at default settings. The following settings were used for spine detection: thinnest diameter of seed points at 0.45 μm; maximum length at 2.5 μm; no branched spines allowed; and seed point threshold at auto.
Acute slice preparation
Drd2-eGFP mice were treated with either haloperidol or haloperidol plus LRRK2 inhibitor (MLi-2) as described above for 14 days. On day 15 or 16, mice were deeply anesthetized on isoflurane (3%) before perfusion with ice-cold aCSF containing in (mM): 127 NaCl, 2.5 KCl, 1.25 NaH2PO4, 25 NaHCO3, 20 glucose, 2 CaCl2, and 1 MgCl2. Brains were dissected and sectioned on a Leica vibratome (VT1000S) to 300 um thickness. Slices were transferred to a holding chamber and incubated at 34 °C for 20 min before recordings.
Current clamp recordings
Slices were placed in the recording chamber at RT and continually perfused with oxygenated aCSF with 1 mM scopolamine to block cholinergic interneuron firing. The dorsal striatum was located under a 10x air objective. A 60x water immersion objective was used to target neurons for recording (Olympus, Tokyo, Japan). Slices were visualized using DIC and a QIClick microscope camera (QImaging, Surrey, Canada). GFP-positive cells were selected using a CoolLED pe4000 system (CoolLED Ltd., Andover, UK). Patch electrodes were pulled from borosilicate capillary glass to a resistance of 2.5–6 MΩ. Electrodes were filled with an intracellular solution comprised of (in mM) 135 K-gluconate, 4 KCl, 10 HEPES, 10 Na-phosphocreatine, 4 MgATP, 0.4 Na2GTP, 1 EGTA, 20 µM Alexa 594 (pH 7.28, 298–305 mOsm/L). After break-in, cells were held for ~5–10 min prior to current clamp recordings.
Recordings were acquired using a Multiclamp 700B amplifier (Axon Instruments, Union City, CA), digitized at a rate of 20 kHz, and filtered at a rate of 3–4 kHz. Five second-long sweeps were acquired using a version of the MATLAB-based (MathWorks, Natick, MA) acquisition suite, ScanImage [88]. A series of 500 ms-long current steps from −50–300 pA were pseudorandomized. Current steps occurred one second after the start of the sweep, followed by 2.5 s of no current injection, and ended with a 20 ms-long, −20 pA current step to test input resistance throughout the recording. Cells were held at −70 mV for the duration of these recordings. The firing rate was determined over the course of the current injection, and EPSP frequency and amplitude were calculated during the period after the current injection. Cells with input resistance that changed > 10% over the recording was higher than 500 m Ohms, or had action potential height less than 10 mV or changed greater than 10 mV over the course of the recording were discarded. Sweeps occurred with an inter-sweep interval of 10–20 s. A minimum of five sweeps for each current step magnitude was obtained. For RheoBase and resting membrane potential, cells were allowed to freely rest for 500 ms prior to a 1 s, 400 pA ramp protocol. This was repeated 5 times, with an interstimulus interval of 10 s.
Current clamp recording analysis
All acquisition, exclusion determination, and firing rate data analysis was done blinded to treatment condition. The average firing rate at each current step was determined using custom-built MatLab code. All values are reported as Hz. Firing rate values were then exported to GraphPad Prism (GraphPad, LaJolla, CA) for data visualization and statistics. Two-way ANOVA with Geisser-Greenhouse correction for symmetry was used to determine significance of treatment by current injection interaction, with post hoc multiple comparisons with Šídák correction across current injection levels.
Input resistance was determined by the change in membrane potential prior to and during the 200 ms −20 pA current step at the end of each recording. EPSP amplitude and frequency were calculated from 4 of the first 5 current sweeps that displayed the least amount of baseline variability. If a cell had more than 1 mV of baseline variability across the recording, it was discarded. A two second bin after current injection was isolated, and number of peaks and prominence of each peak was calculated using custom built MATLAB protocol. Peak amplitude (prominence) was determined as a change in mV from the top of the peak to the baseline most proximal to peak. All peaks that had a prominence above 0.4 mV were included in the analysis. Frequency was determined by summing the total number of peaks divided by the bin time per trace. Trace frequencies were then averaged to determine frequency per cell. All frequency data represents average frequency per cell. Action potential threshold was determined as the first inflection point (by a change in slope) that exceeded 10 mV/ms during the ramp protocol. Resting membrane potential was taken as an average of membrane potential between 200 and 300 ms prior to rheobase protocol. Rheobase was determined as the first inflection point (by change in slope of more than 10 mV/ms) along the ramp protocol. All were exported to GraphPad Prism, and all statistics are ordinary one-way ANOVA.
Western blot analysis
After receiving the drug treatments as described in the relevant sectionh striatal tissues were extracted and homogenized in 1x cell lysis buffer (Cell Signaling Technologies) supplemented with Halt protease and phosphatase inhibitor cocktail (Thermo Fisher Scientific) using pellet pestles (30 s). Protein concentration was determined by BCA Protein Assays (Thermo Scientific) 30 μg of total lysate were separated by 4–12% NuPage Bis-Tris PAGE (Invitrogen) and transferred to membranes using the iBlot nitrocellulose membrane Blotting system (Invitrogen) by following manufacture protocol. The membranes were incubated with primary antibodies specific for phospho-Rab12 (1:1000, Abcam), total Rab12 (1:1000 Proteintech and β-actin (1:3000, Sigma) at 4C overnight. The membranes following probing with secondary anti-mouse or and anti-rabbit antibodies (1:2000, Thermo Scientific) for 1 h at room temperature were incubated with Immobilon ECL Ultra Western HRP Substrate (Millipore) for 3 min prior to image acquisition. Chemiluminescent blots were imaged with iBright CL1000 imaging system (Thermo Fisher Scientific). Chemicals and antibodies are detailed in the resource table.
Striatal sections immunofluorescence and analysis
Drd2-eGFP mice crossed with LRRK2-GS KI and control littermates were treated as indicated and perfused with 50 ml of PBS and followed with 50 ml 4% paraformaldehyde in PBS 1 h after the last vehicle/haloperidol administration. Brains were dehydrated with 30% sucrose in PBS for 48 h and cut coronally (30 μm) by cryostat (Leica Biosystems, CM305). Slices were collected in PBS + 0.1% sodium azide and stored at 4 °C for immunohistochemistry. Striatal sections were incubated with 5% goat serum in 0.2% Triton X-100 for 2 h. After, the sections were incubated in the same solution overnight at 4 °C with the primary antibodies anti-GFP (1:1000, Invitrogen) and anti-phospho-S6 Ribosomal protein (Ser236/236) (1:300, Cell Signaling Technology). Then, sections were washed with PBS and incubated with the secondary antibodies Alexa Fluor™ 488 and Alexa Fluor™ 647 (both 1:600, Invitrogen) for 3 h. All the slices were washed with PBS and mounted on ProLong™ Diamond Antifade Mountant. Detailed catalog and identification numbers are shown in the resource table.
Confocal images were obtained with a Nikon A1R microscope. Fluorescence images were acquired with a 20x objective at 1024 × 1024 pixel resolution. Stitched images of the whole striatum were automatically acquired with Nikon Element. GFP and phospho-S6 Ribosomal protein signal were measured using Imaris 10.1 software (Bitplane, Concord, USA). Surface rendering function was used to segment Drd2-eGFP cells. Background subtraction was enabled, the diameter of the largest sphere was set at 15 μm and automatically thresholded, and smooth surface was set to 1.23 μm. Segments were filtered with an area ranging between 100 and 6000 μm2. Mean intensity of phospho-S6 Ribosomal protein within Drd2-eGFP surface above 2 times of average phospho-S6 Ribosomal protein channel mean intensity was considered positive. Based on our prior experience, 4–6 sections per mouse from 3–4 mice is suitable for an experimental condition.
LC-MS/MS analysis
The tissue samples were processed by Tymora Analytical Operations (West Lafayette, IN). For lysis, 200 µL of phase- transfer surfactant lysis buffer (PTS, containing 12 mM sodium deoxycholate, 12 mM sodium lauroyl sarcosinate, 10 mM TCEP, 40 mM CAA), supplemented with phosphatase inhibitor cocktail 3 (Millipore-Sigma) was added to each of the tissue samples, pulse-sonicated several times with a sonicator probe to lyse the tissues. Based on our experience, 3 mice per treatment group is suitable for this experimental condition. The samples were incubated for 10 min at 95 °C, pulse-sonicated several times again with a sonicator probe, and incubated again for 5 min at 95 °C. The lysed samples were then centrifuged at 16,000 × g for 10 min to remove debris and the supernatant portions collected. The samples were diluted fivefold with 50 mM triethylammonium bicarbonate and BCA assay was carried out to calculate the protein concentration and all samples were normalized by protein amount. Then 250 ug of each sample was digested with Lys-C (Wako) at 1:100 (wt/wt) enzyme-to-protein ratio for 3 h at 37 °C. Trypsin was added to a final 1:50 (wt/wt) enzyme-to- protein ratio for overnight digestion at 37 °C. To remove the PTS surfactants from the samples, the samples were acidified with trifluoroacetic acid (TFA) to a final concentration of 1% TFA, and ethyl acetate solution was added at 1:1 ratio. The mixture was vortexed for 2 min and then centrifuged at 16,000 × g for 2 min to obtain aqueous and organic phases. The organic phase (top layer) was removed, and the aqueous phase was collected. This step was repeated once more. The samples were dried in a vacuum centrifuge and desalted using Top-Tip C18 tips (Glygen) according to manufacturer’s instructions. The samples were dried completely in a vacuum centrifuge and used for phosphopeptide enrichment using PolyMAC Phosphopeptide Enrichment Kit (Tymora Analytical) according to the manufacturer’s instructions.
The sample was dissolved in 10.5 μL of 0.05% trifluoroacetic acid with 3% (vol/vol) acetonitrile, and 10 μL of each sample was injected into an Ultimate 3000 nano UHPLC system (Thermo Fisher Scientific). Peptides were captured on a 2-cm Acclaim PepMap trap column and separated on a 50-cm column packed with ReproSil Saphir 1.8 μm C18 beads (Dr. Maisch GmbH). The mobile phase buffer consisted of 0.1% formic acid in ultrapure water (buffer A) with an eluting buffer of 0.1% formic acid in 80% (vol/vol) acetonitrile (buffer B) run with a linear 90-min gradient of 6–30% buffer B at flow rate of 300 nL/min. The UHPLC was coupled online with a Q-Exactive HF-X mass spectrometer (Thermo Fisher Scientific). The mass spectrometer was operated in the data-dependent mode, in which a full-scan MS (from m/z 375–1500 with the resolution of 60,000) was followed by MS/MS of the 15 most intense ions (30,000 resolution; normalized collision energy - 28%; automatic gain control target (AGC)-2E4, maximum injection time-200 ms; 60 s exclusion). Minimum precursor mass was set at 350 Da, with the lowest charge state of 2 and the highest of 6. The S/N threshold was set at 1.5 and the minimum peak count of 1. In this dataset, less than 9% of all phosphopeptides had 2 missed cleavages.
LC-MS data processing
The raw files were searched directly against the mouse database with no redundant entries, using Byonic (Protein Metrics) and Sequest search engines loaded into Proteome Discoverer 2.3 software (Thermo Fisher Scientific). The data from the two search engines was combined together. In most cases, the same peptides were identified both. The final data reported is the combination of both search engines, including the identifications reported by only one search engine. MS1 precursor mass tolerance was set at 10 ppm, and MS2 tolerance was set at 20 ppm. Search criteria included a static carbamidomethylation of cysteines (+57.0214 Da), and variable modifications of phosphorylation of S, T and Y residues (+79.996 Da), oxidation (+15.9949 Da) on methionine residues and acetylation (+42.011 Da) at N terminus of proteins. Search was performed with full trypsin/P digestion and allowed a maximum of two missed cleavages on the peptides analyzed from the sequence database. The false-discovery rates of proteins and peptides were set at 0.01. All protein and peptide identifications were grouped and any redundant entries were removed. Only unique peptides and unique master proteins were reported. Total proteomics and phospho-proteomics triplicated data for WT and GS mice treated with haloperidol or saline contained the [log2 intensity value per gene or phospho-peptide normalized to the mean of the run]. Total proteomics data were QCed to i) remove the entries with no gene-name and ii) remove duplicated genes (keeping the replica with the smallest standard error on the fold change haloperidol vs saline). Phospho-proteomics data were only QCed to remove the entries with no gene-name. The number of proteins captured by total proteomics was 3997 proteins, while the total number of phospho- peptides was 9399 mapping to a total of 3010 unique proteins. The fold-change (FC) for the total protein level was calculated for both WT and GS as protein intensity after haloperidol treatment / protein intensity after saline treatment (t- test, two-tailed and homoscedastic). FC = mean(log2(treated)) - mean(log2(saline)). For phospho-proteomics the log2 intensity level of each phospho-peptide was normalized to the log2 intensity level of the total corresponding protein (for each run of saline and haloperidol treatments): Log2 normalized peptide intensity = log2(phospho-peptide) - log2(total protein) before calculating the FC as: peptide intensity after haloperidol treatment / peptide intensity after saline treatment (t-test, two-tailed and homoscedastic). FC = mean(log2(treated)) - mean(log2(saline)). Of note, not for all phospho-peptides a corresponding protein was available in the total proteomics analysis, this reduced the total amount of phospho-peptides that could be analyzed down to 6787 peptides mapping to a total of 1641 unique proteins. Threshold for significance was set to p < 0.05 (unadjusted p-value) & FC (difference on the log2 intensity values) ≥ |2 | . To capture a greater number of phosphorylations for GO-term and kinase-substrate analysis, the statistical cut-off for inclusion was set at uncorrected p > 0.05.
Pipelines for proteome analysis
GSEA analysis of significantly enriched phosphopeptides for each comparison were analyzed in the listed ontology groups using the enrichR R package to query the Enrichr database [89].
Volcano plots
All quantified phosphopeptides (for proteomic sets) were graphed according to their log2fc and the statistical significance of the change using the ggplot2 R package.
Heatmaps were generated using the ComplexHeatmap R package [90].
Multicolor fluorescence in situ hybridization and analysis
The smFISH protocol was implemented according to manufacturer guidelines (ACD RNAscope Multiplex Fluorescent Assay v2). Mice were euthanized with carbon dioxide, decapitated, their brains rapidly removed, and placed immediately on foil on dry ice. Brains were then placed in molds containing OCT embedding medium and snap-frozen on dry ice. Embedded brains were sectioned on a cryostat into 20 µm sections, mounted onto Superfrost™ slides (and stored at −80 °C. Two sections (at ~−0.1 and –0.34 mm from Bregma) were processed for probe hybridization. All probes and kits were purchased from Advanced Cell Diagnostics, and the chemicals used are described in detail in the resource table. Slides were counterstained with DAPI for 30 s, cover slipped with mounting medium. Sections were imaged with the Nikon A1 laser microscope system using a 60X 0.75NA objective, to capture 3 z-stack images across 4 channels: 458 (DAPI), 488 (FITC), 561 (TRITC), 638 (Cy5). Projections were obtained using Maximum Intensity Z-projection in ImageJ. Images were analyzed using the CellProfiler4 speckle counting pipeline. Each field was processed in Cell Profiler [91, 92] to identify nuclei and measure Drd2/Nr4a1 using the nuclei as seed objects. DAPI channel was enhanced with Enhance Or Suppress Features module, with feature size set at pixel size 30. Identify Primary Objects module was implemented on identified nuclei, object pixel unit was set for Min 5, Max 50, with threshold strategy set as Global and thresholding method set as Otsu. Drd1 or Drd2 channel was enhanced with Enhance Or Suppress Features module, with feature size set at pixel size 10. Nr4a1 or Arc channel was enhanced with Enhance Or Suppress Features module, with feature size set at pixel size 5. Identify Primary Objects module was implemented on identified Drd1 or Drd2 signal puncta, object pixel unit was set for Min 3, Max30, threshold strategy for Global and thresholding method set as Manual. Nr4a1 object pixel unit was set for Min 1, Max10, threshold strategy for Global and thresholding method set as Manual. Masked D1 positive nuclei and Masked D2 positive nuclei were generated with RelateObjects. The number of objects were measured with the Measure Object Intensity module.
Statistics
Group statistical analyses were done using GraphPad Prism 10.1 software (GraphPad, LaJolla, CA). Sample size (n value) is defined by the number of observations (i.e., neurons, sections, or mice) and is indicated in the legends. All data are expressed as mean + SEM, or individual plots. Unless otherwise indicated, statistical significance was determined by two-tailed Student’s t-tests for two-group comparisons. For multiple group comparisons, one-way or two-way analysis of variance (ANOVA) tests were used for normally distributed data, followed by post-hoc analyses. In some behavioral studies, most vehicle-treated mice spend no time at the bar, making a normal distribution unsuitable. Normal distributions of data were not assumed for electrophysiological data. Comparisons for unrelated samples were performed using Mann–Whitney U test at a significance level (α) of 0.05.
Key resource table (Supplementary Table 1)
Detailed information about all the resources used and material associated with this article can be found in Supplementary Table 1.
Data availability
The mass spectrometry proteomics data have been deposited to the ProteomeXchange Consortium via the PRIDE partner repository with the dataset identifier PXD053892; raw tabular data of all experiments, all images and codes used in this study are available through the open access option on the Zenodo repository (https://doi.org/10.5281/zenodo.15092155) or Github. The protocols used in this study were uploaded to protocols.io, and their DOI can be found in the key resource table (Supplementary Table 1).
References
Beaulieu JM, Gainetdinov RR. The physiology, signaling, and pharmacology of dopamine receptors. Pharmacol Rev. 2011;63:182–217. https://doi.org/10.1124/pr.110.002642.
Neve KA, Seamans JK, Trantham-Davidson H. Dopamine receptor signaling. J Recept Signal Transduct Res. 2004;24:165–205. https://doi.org/10.1081/rrs-00029981.
Gerfen CR, Surmeier DJ. Modulation of striatal projection systems by dopamine. Annu Rev Neurosci. 2011;34:441–66. https://doi.org/10.1146/annrev-neuro-061010-113641.
Kreitzer AC, Malenka RC. Striatal plasticity and basal ganglia circuit function. Neuron. 2008;60:543–54. https://doi.org/10.1016/j.neuron.2008.11.005.
Delong MR. Primate models of movement disorders of basal ganglia origin. Trends Neurosci. 1990;13:281–5. https://doi.org/10.1016/0166-2236(90)90110-v.
Alexander GE, Crutcher MD. Functional architecture of basal ganglia circuits: neural substrates of parallel processing. Trends Neurosci. 1990;13:266–71. https://doi.org/10.1016/0166-2236(90)90107-I.
Zhai S, Shen W, Graves SM, Surmeier JD. Dopaminergic modulation of striatal function and Parkinson’s disease. J Neural Transm. 2019;126:411–22. https://doi.org/10.1007/s00702-019-01997-y.
Lee SJ, Lodder B, Chen Y, Patriarchi T, Tian L, Sabatini B. Cell-type-specific asynchronous modulation of PKA by dopamine in learning. Nature. 2020;590:451–6. https://doi.org/10.1038/s41586-020-03050-5.
Ma L, Day-Cooney J, Benavides O, Muniak MA, Qin M, Ding J, et al. Locomotion activates PKA through dopamine and adenosine in striatal neurons. Nature. 2022;611:762–8. https://doi.org/10.1038/s41586-022-05407-4.
Cui G, Jun SB, Jin X, Pham MD, Vogel SS, Lovinger D, et al. Concurrent activation of striatal direct and indirect pathways during action initiation. Nature. 2013;494:238–42. https://doi.org/10.1038/nature11846.
Creese I, Burt DR, Snyder SH. Dopamine receptor binding predicts clinical and pharmacological potencies of antischizophrenic drugs. Science. 1976;192:481–3. https://doi.org/10.1126/science3854.
Seeman P, Lee T, Chau-Wong M, Wong K. Antipsychotic drug doses and neuroleptic/dopamine receptors. Nature. 1976;261:717–9. https://doi.org/10.1038/261717a0.
Novick D, Haro JM, Bertsch J, Haddad PM. Incidence of extrapyramidal symptoms and tardive dyskinesia in schizophrenia: thirty-six-month results from the European schizophrenia outpatient health outcomes study. J Clin Psychopharmacol. 2010;30:531–40. https://doi.org/10.1097/JCP.0b013e3181f14098.
Siafis S, Wu H, Wang D, Burschinski A, Nomura N, Takeuchi H, et al. Antipsychotic dose, dopamine D2 receptor occupancy and extrapyramidal side-effects: a systematic review and dose-response meta-analysis. Mol Psychiatry. 2023;28:3267–77. https://doi.org/10.1038/s41380-023-02203-y.
Usiello A, Baik JH, Rouge-Pont F, Picetti R, Dierich A, LeMeur M, et al. Distinct functions of the two isoforms of dopamine D2 receptors. Nature. 2000;9:199–203. https://doi.org/10.1038/35041572.
Sebel LE, Graves SM, Chan CS, Surmeier JD. Haloperidol selectively remodels striatal indirect pathway circuits. Neuropsychopharmacology. 2017;42:963–73. https://doi.org/10.1038/npp.2016.173.
Taymans JM, Fell M, Greenmamyre T, Hirst WD, Mamais A, Padmanabhan S, et al. Perspective on the current state of the LRRK2 field. NPJ Parkinsons Dis. 2023;9:104. https://doi.org/10.1038/s41531-023-00544-7.
Alessi DR, Sammler E. LRRK2 kinase in Parkinson’s disease. Science. 2018;360:36–7. https://doi.org/10.1126/science.aar5683.
Tokars V, Chen C, Parisiadou L. Closing the structure-to-function gap for LRRK2. Trends Biochem Sci. 2022;47:187–8. https://doi.org/10.1016/j.tibs.221.10.003.
Parisiadou L, Yu J, Sgobio C, Xie C, Liu G, Sun L, et al. LRRK2 regulates synaptogenesis and dopamine receptor activation through modulation of PKA activity. Nat Neurosci. 2014;17:367–76. https://doi.org/10.1038/nn3636.
Matikainen-Ankney BA, Kezunovic N, Mesias RE, Tian Y, Williams FM, Huntley GW, et al. Altered development of synapse structure and function in striatum caused by Parkinson’s disease-linked LRRK2-G2019S mutation. J Neurosci. 2016;36:7128–41. https://doi.org/10.1523/JNEROSCI.3314-15.2016.
Matikainen-Ankney BA, Kezunovic N, Menard C, Flanigan M, Zhong Y, Russo SJ, et al. Parkinson’s disease-linked LRRK2-G2019S mutation alters synaptic plasticity and promotes resilience to chronic social stress in young adulthood. J Neurosci. 2018;38:9700–11. https://doi.org/10.1523/JNEUROSCI.1457-18.2018.
Xenias HS, Chen C, Kang S, Cherian S, Situ X, Shanmugasundaram B, et al. R1441C and G2019S LRRK2 knockin mice have distinct striatal molecular, physiological, and behavioral alterations. Commun Biol. 2022;5:1211. https://doi.org/10.1038/s42003-022-04136-8.
Skelton PD, Tokars V, Parisiadou L. LRRK2 at striatal synapses: cell-type specificity and mechanistic insights. Cells. 2022;11:169. https://doi.org/10.3390/cells11010169.
Volta M, Beccano-Kelly DA, Paschall SA, Cataldi S, MacIsaac SE, Kuhlmann N, et al. Initial elevations in glutamate and dopamine neurotransmission decline with age, as does exploratory behavior, in LRRK2 G2019S knock-in mice. eLife. 2017;6:e28377. https://doi.org/10.7554/eLife28377.
Chen C, Soto G, Dumrongprechachan V, Bannon N, Kang S, Kozorovitskiy Y, et al. Pathway-specific dysregulation of striatal excitatory synapses by LRRK2 mutations. eLife. 2020;9:e58997. https://doi.org/10.7554/eLife.58997.
Tozzi A, Tantucci M, Marchi S, Mozzocchetti P, Morari M, Pinton P, et al. Dopamine D2 receptor-mediated neuroprotection in a G2019S Lrrk2 genetic model of Parkinson’s disease. Cell Death Dis. 2018;9:204. https://doi.org/10.1038/s41419-017-0221-2.
Tozzi A, Durante V, Bastioli G, Mazzocchetti M, Novello S, Mechelli A, et al. Dopamine D2 receptor activation potently inhibits striatal glutamatergic transmission in a G2019S LRRK2 genetic model of Parkinson’s disease. Neurobiol Dis. 2018;118:1–8. https://doi.org/10.1016/j.nbd.2018.06.008.
Beccano-Kelly DA, Volta M, Munsie LN, Paschall SA, Tatamikov I, Co K, et al. LRRK2 overexpression alters glutamatergic presynaptic plasticity, striatal dopamine tone, postsynaptic signal transduction, motor activity and memory. Hum Mol Genet. 2015;24:1336–49. https://doi.org/10.1093/hmg/ddu543.
Steger M, Tonelli F, Ito G, Davies P, Trost M, Vetter M, et al. Phosphoproteomics reveals that Parkinson’s disease kinase LRRK2 regulates a subset of Rab GTPases. eLife. 2016;5:e12813. https://doi.org/10.7554/eLife.12813.
Greggio E, Jain S, Kingsbury A, Bandopadhyay R, Lewis P, Kaganovich A, et al. Kinase activity is required for the toxic effects of mutant LRRK2/dardarin. Neurobiol Dis. 2006;23:329–41. https://doi.org/10.1016/j.nbd.2006.04.001.
Volta M, Melrose H. LRRK2 mouse models: dissecting the behavior, striatal neurochemistry and neurophysiology of PD pathogenesis. Biochem Soc Trans. 2017;45:113–22. https://doi.org/10.1042/BST20160238.
Yue M, Hinkle K, Davies P, Trushina E, Fiesel F, Christenson T, et al. Progressive dopaminergic alterations and mitochondrial abnormalities in LRRK2 G2019S knock-in mice. Neurobiol Dis. 2015;78:172–95. https://doi.org/10.1016/j.nbd.2015.02.031.
Tong Y, Pisani A, Martella G, Shen J. R1441C mutation in LRRK2 impairs dopaminergic neurotransmission in mice. Proc Natl Acad Sci USA. 2009;106:14622–7. https://doi.org/10.1073/pnas.0906334106.
Fell MJ, Mirescu C, Basu K, Cheewatrakoolpong B, DeMong DE, Ellis JM, et al. MLi-2, a potent, selective, and centrally active compound for exploring the therapeutic potential and safety of LRRK2 kinase inhibition. J Pharmacol Exp Ther. 2015;355:397–409. https://doi.org/10.1124/jpet.115.227587.
Murillo MS, Suarez A, Dederer V, Chatterjee D, Louro JA, Knapp S, et al. Inhibition of Parkinson’s disease-related LRRK2 by type I and type II kinase inhibitors: activity and structures. Sci Adv. 2023;9:eadk6191. https://doi.org/10.1126/sciadv.adk6191.
Scott JD, DeMong DE, Greshock TJ, Basu K, Dai X, Harris J, et al. Discovery of a 3-(4-Pyrimidinyl) indazole (MLi-2), an orally available and selective leucine- rich repeat kinase 2 (LRRK2) inhibitor that reduces brain kinase activity. J Med Chem. 2017;60:2983–92. https://doi.org/10.1021/acs.jmedchem.7b00045.
Kluss JH, Mazza MC, Li Y, Manzoni C, Lewis P, Cookson MR, et al. Preclinical modeling of chronic inhibition of the Parkinson’s disease associated kinase LRRK2 reveals altered function of the endolysosomal system in vivo. Mol Neurodegener. 2021;16:17. https://doi.org/10.1186/s13024-021-00441-8.
Dhekne HS, Tonelli F, Yeshaw WM, Chiang CY, Linouse C, Jaimon E, et al. Genome-wide screen reveals Rab12 GTPase as a critical activator of Parkinson’s disease-linked LRRK2 kinase. eLife. 2023;12:e87098. https://doi.org/10.7554/eLife.87098.
Baptista MAS, Merchant K, Barrett T, Bhargava S, Bryce DK, Ellis JM, et al. LRRK2 inhibitors induce reversible changes in nonhuman primate lungs without measurable pulmonary deficits. Sci Transl Med. 2020;12:eaav0820. https://doi.org/10.1126/scitranslmed.aav0820.
Yuan Y, Li H, Sreeram K, Malankhanova T, Boddu R, Strader S, et al. Single molecule array measures of LRRK2 kinase activity in serum link Parkinson’s disease severity to peripheral inflammation. bioRxiv. 2024. https://doi.org/10.1101/2024.04.15.589570.
Bymaster FP, Calligaro DO, Falcone JF, Marsh RD, Moore NA, Tye NC, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology. 1996;14:87–96. https://doi.org/10.1016/0893-133X(94)00129-N.
Radl D, Chiacchiaretta M, Lewis RG, Brami-Cherrier K, Arcuri L, Borelli E. Differential regulation of striatal motor behavior and related cellular responses by dopamine d2l and d2s isoforms. Proc Natl Acad Sci USA. 2018;115:198–203. https://doi.org/10.1073/pnas.1717194115.
Gilbert F, Morissette M, Hilaire MST, Paquet B, Rouillard C, DiPaolo T, et al. Nur77 gene knockout alters dopamine neuron biochemical activity and dopamine turnover. Biol Psychiatry. 2006;60:538–47. https://doi.org/10.1016/j.biopsych.2006.04.023.
Ezrin-Waters C, Seeman P. Tolerance to haloperidol catalepsy. Eur J Pharmacol. 1977;41:321–7. https://doi.org/10.1016/0014-2999(77)90325-9.
Augustin SM, Loewinger GC, O’Neal TJ, Kravitz AV, Lovinger DM. Dopamine D2 receptor signaling on iMSNs is required for initiation and vigor of learned actions. Neuropsychopharmacology. 2020;45:2087–97. https://doi.org/10.1038/s41386-020-00799-1.
Lemos JC, Friend DM, Kaplan AR, Shin JH, Rubinstein M, Kravitz AV, et al. Enhanced GABA transmission drives bradykinesia following loss of dopamine D2 receptor signaling. Neuron. 2016;90:824–38. https://doi.org/10.1016/j.neuron.2016.04.040.
Yin HH, Mulcare SP, Hilario MRF, Clouse E, Holloway T, Davis MI, et al. Dynamic reorganization of striatal circuits during the acquisition and consolidation of a skill. Nat Neurosci. 2009;12:333–41. https://doi.org/10.1038/nn.2261.
Lobo MK, Zaman S, Damez-Werno DM, Wook Koo J, Bagot RC, DiNieri JA, et al. ΔFosB induction in striatal medium spiny neuron subtypes in response to chronic pharmacological, emotional, and optogenetic stimuli. J Neurosci. 2013;33:18381–95. https://doi.org/10.1523/JNEUROSCI.1875-13.2013.
Yael D, Zeef DH, Sand D, Moran A, Katz DB, Cohen D, et al. Haloperidol-induced changes in neuronal activity in the striatum of the freely moving rat. Front Syst Neurosci. 2013;7:110. https://doi.org/10.3389/fnsys.2013.00110.
Kruyer A, Parrilla-Carrero J, Powell C, Brandt L, Gutwinski S, Angelis A, et al. Accumbens D2-MSN hyperactivity drives antipsychotic-induced behavioral supersensitivity. Mol Psychiatry. 2021;26:6159–69. https://doi.org/10.1038/s41380-021-01235-6.
Centonze D, Usiello A, Costa C, Picconi B, Erbs E, Bernardi G, et al. Chronic haloperidol promotes corticostriatal long-term potentiation by targeting dopamine D2L receptors. J Neurosci. 2004;24:8214–22. https://doi.org/10.1523/JNEUROSCI.1274-04.2004.
Nicola SM, Surmeier J, Malenka RC. Dopaminergic modulation of neuronal excitability in the striatum and nucleus accumbens. Annu Rev Neurosci. 2000;23:185–215. https://doi.org/10.1146/annurev.neuro.23.1.185.
Valjent E, Bertran-Gonzalez J, Bowling H, Lopez S, Santini E, Matamales M, et al. Haloperidol regulates the state of phosphorylation of ribosomal protein S6 via activation of PKA and phosphorylation of DARPP-32. Neuropsychopharmacology. 2011;36:2561–70. https://doi.org/10.1038/npp.2011.
Kharkwal G, Brami-Cherrier K, Lizardi-Ortic JE, Nelson A, Ramos M, Del Barrio D, et al. Parkinsonism driven by antipsychotics originates from dopaminergic control of striatal cholinergic interneurons. Neuron. 2016;91:67–78. https://doi.org/10.1016/j.neuron.2016.06.014.
Santa C, Rodrigues D, Coelho JF, Anjo S, Mendes VM, Bessa-Neto B, et al. Chronic treatment with D2-antagonist haloperidol leads to inhibitory/excitatory imbalance in striatal D1-neurons. Transl Psychiatry. 2023;13:312. https://doi.org/10.1038/s41398-023-02609-w.
Eastwood SL, Porter RH, Harrison PJ. The effect of chronic haloperidol treatment on glutamate receptor subunit (GluR1, GluR2, KA1, KA2, NR1) mRNAs and glutamate binding protein mRNA in rat forebrain. Neurosci Lett. 1996;212:163–6. https://doi.org/10.1016/0304-3940(96)12801-9.
Meshul CK, Casey DE. Regional, reversible ultrastructural changes in rat brain with chronic neuroleptic treatment. Brain Res. 1989;489:338–46. https://doi.org/10.1016/0006-8993(89)90867-6.
Critchlow HM, Maycox PR, Skepper JN, Krylova O. Clozapine and haloperidol differentially regulate dendritic spine formation and synaptogenesis in rat hippocampal neurons. Mol Cell Neurosci. 2006;32:356–65. https://doi.org/10.1016/j.mcn.2006.05.007.
Russo I, Berti G, Plotegher N, Bernardo G, Filograna R, Bubacco L, et al. Leucine-rich repeat kinase 2 positively regulates inflammation and down-regulates NF-κB p50 signaling in cultured microglia cells. J Neuroinflammation. 2015;12:230. https://doi.org/10.1186/s12974-015-0449-7.
Parisiadou L, Cai H. LRRK2 function on actin and microtubule dynamics in Parkinson disease. Commun Integr Biol. 2010;3:396–400. https://doi.org/10.4161/cib.3.5.12286.
MacLeod D, Dowman J, Hammond R, Leete T, Inoue K, Abeliovich A. The familial Parkinsonism gene LRRK2 regulates neurite process morphology. Neuron. 2006;52:587–93. https://doi.org/10.1016/j.neuron.2006.10.008.
Tombesi G, Kompella S, Favetta G, Chen C, Zhao Y, Sevegnani M, et al. LRRK2 regulates synaptic function through BDNF signaling and actin cytoskeleton. biorxiv. 2024. https://doi.org/10.7554/eLife.95987.1.
Parisiadou L, Xie C, Cho HJ, Lin X, Gu XL, Long CX, et al. Phosphorylation of ezrin/radixin/moesin proteins by LRRK2 promotes the rearrangement of actin cytoskeleton in neuronal morphogenesis. J Neurosci. 2009;29:13971–80. https://doi.org/10.1523/JNEUROSCI.3799-09.2009.
Civiero L, Cogo S, Biosa A, Greggio E. The role of LRRK2 in cytoskeletal dynamics. Biochem Soc Trans. 2018;46:1653–63. https://doi.org/10.1042/BST20180469.
De Bartolomeis A, Buonaguro EF, Latte G, Rossi R, Marmo F, Iasevoli F, et al. Immediate-early genes modulation by antipsychotics: translational implications for a putative gateway to drug-induced long-term brain changes. Front Behav Neurosci. 2017;11:240. https://doi.org/10.3389/fnbeh.2017.00240.
Sakuma K, Komatsu H, Maruyama M, Imaichi S, Habata Y, Mori M. Temporal and spatial transcriptional fingerprints by antipsychotic or propsychotic drugs in mouse brain. PLoS ONE. 2015;10:e0118510. https://doi.org/10.1371/journal.pone.0118510.
Onimus O, Valjent E, Fisone G, Gangarossa G. Haloperidol-induced immediate early genes in striatopallidal neurons requires the converging action of cAMP/PKA/DARPP-32 and mTOR pathways. Int J Mol Sci. 2022;23:11637. https://doi.org/10.3390/ijms231911637.
Benito E, Barco A. The neuronal activity-driven transcriptome. Mol Neurobiol. 2015;51:1071–88. https://doi.org/10.1007/s12035-014-8772-z.
Beaudry G, Langlois MC, Weppe I, Rouillard C, Levesque D. Contrasting patterns and cellular specificity of transcriptional regulation of the nuclear receptor nerve growth factor-inducible B by haloperidol and clozapine in the rat forebrain. J Neurochem. 2000;75:1694–702. https://doi.org/10.1371/journal.pone.0118510.
Maheux J, Ethier I, Rouillard C, Levesque D. Induction patterns of transcription factors of the nur family (nurr1, nur77, and nor-1) by typical and atypical antipsychotics in the mouse brain: implication for their mechanism of action. J Pharmacol Exp Ther. 2005;313:460–73. https://doi.org/10.1124/jpet.104.080184.
Éthier I, Beaudry G, Hilaire MST, Milrandt J, Rouillard C, Levesque D. The transcription factor NGFI-B (Nur77) and retinoids play a critical role in acute neuroleptic- induced extrapyramidal effect and striatal neuropeptide gene expression. Neuropsychopharmacology. 2004;29:335–46. https://doi.org/10.1038/sj.npp.1300318.
Yun S, Yang B, Anair JD, Martin MM, Fleps SW, Pamucku A, et al. Antipsychotic drug efficacy correlates with the modulation of D1 rather than D2 receptor-expressing striatal projection neurons. Nat Neurosci. 2023;26:1417–28. https://doi.org/10.1038/s41593-023-01390-9.
Rassu M, Del Giudice MG, Sanna S, Taymans JM, Morari M, Brugnoli A, et al. Role of LRRK2 in the regulation of dopamine receptor trafficking. PLoS ONE. 2017;12:e0179082. https://doi.org/10.1371/journal.pone.0179082.
Kandel E. The molecular biology of memory: cAMP, PKA, CREB-1, CREB-2, and CPEB. Mol Brain. 2012;5:14. https://doi.org/10.1186/1756-6606-5-14.
Saunders A, Macosko EZ, Wysoker A, Goldman M, Krienen FM, de Rivera H, et al. Molecular diversity and specializations among the cells of the adult mouse brain. Cell. 2018;174:1015–30. https://doi.org/10.1016/j.cell.2018.07.028.
Connolly BS, Lang AE. Pharmacological treatment of Parkinson disease: a review. JAMA. 2014;311:1670–83. https://doi.org/10.1001/jama.2014.3654.
Jennings D, Huntwork-Rodriguez S, Henry AG, Sasaki J, Meisner R, Diaz D, et al. Preclinical and clinical evaluation of the LRRK2 inhibitor DNL201 for Parkinson’s disease. Sci Transl Med. 2022;14:eabj2658. https://doi.org/10.1126/scitranslmed.abj2658.
Zhao HT, John N, Delic V, Ikeda-Lee K, Kim A, Weihofen A, et al. LRRK2 antisense oligonucleotides ameliorate α-synuclein inclusion formation in a Parkinson’s disease mouse model. Mol Ther Nucleic Acids. 2017;8:508–19. https://doi.org/10.1016/j.omtn.2017.08.002.
Whiffin N, Armean IM, Kleinman A, Marshall JL, Minikel EV, Goodrich JK, et al. The effect of LRRK2 loss-of-function variants in humans. Nat Med. 2020;26:869–77. https://doi.org/10.1038/s41591-020-0893-5.
Agid O, Kapur S, Arenovich T, Zipursky RB. Delayed-onset hypothesis of antipsychotic action a hypothesis tested and rejected. Arch Gen Psychiatry. 2023;60:1228–35. https://doi.org/10.1001/archpsyc.60.12.122881.
Leucht S, Busch R, Hamann J, Kissling W, Kane JM. Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol Psychiatry. 2005;57:1543–9. https://doi.org/10.1016/j.biopsych.2005.02.023.
Gong S, Zheng C, Doughty ML, Losos K, Didkovsky N, Schambra UB, et al. A gene expression atlas of the central nervous system based on bacterial artificial chromosomes. Nature. 2003;425:917–25. https://doi.org/10.1038/nature02033.
Bello EP, Mateo Y, Gelman DM, Noain D, Shin JH, Low MJ, et al. Cocaine supersensitivity and enhanced motivation for reward in mice lacking dopamine D2 autoreceptors. Nat Neurosci. 2011;14:1033–8. https://doi.org/10.1038/nn.2862.
Wu M, Minkowicz S, Dumrongprechachan V, Hamilton P, Kozorovitskiy Y. Ketamine rapidly enhances glutamate-evoked dendritic spinogenesis in medial prefrontal cortex through dopaminergic mechanisms. Biol Psychiatry. 2021;89:1096–105. https://doi.org/10.1016/j.biopsych.2020.12.022.
Wu M, Zhang X, Feng S, Freda SN, Kumari P, Dumrongprechachan V, et al. Dopamine pathways mediating affective state transitions after sleep loss. Neuron. 2024;112:141–54. https://doi.org/10.1016/j.neuron.2023.10.002. e8
Dumrongprechachan V, Salisbury RB, Soto G, Kumar M, MacDonald ML, Kozorovitskiy Y. Cell type and subcellular compartment specific APEX2 proximity labeling proteomics in the mouse brain. Nat Commun. 2021;12:4855. https://doi.org/10.1101/2021.04.08.439091.
Pologruto T, Sabatini BL, Svodoba K. ScanImage: flexible software for operating laser scanning microscopes. Biomed Eng Online. 2023;17:2. https://doi.org/10.1186/1475-925X-2-13.
Kuleshov MV, Jones MR, Rouillard A, Fernandez NF, Duan Q, Wang Z, et al. Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 2016;44:W90–W97. https://doi.org/10.1093/nar/gkw377.
Gu Z, Hubschmann D. Make interactive complex heatmaps in R. Bioinformatics. 2022;38:1460–2. https://doi.org/10.1093/bioinformatics/btab806.
Erben L, Buonanno A. Detection and quantification of multiple RNA sequences using emerging ultrasensitive fluorescent in situ hybridization techniques. Curr Protoc Neurosci. 2019;87:e63. https://doi.org/10.1002/cpns.63.
Stirling DR, Swain-Bowden MJ, Lucas AM, Carpenter A, Goodman A, Cimini BA. CellProfiler 4: improvements in speed, utility, and usability. BMC Bioinformatics. 2021;22:433. https://doi.org/10.1186/s12859-021-04344-9.
Acknowledgements
This work was supported by NIH R01 NS097901 (L.P.), R01NS107539 (Y.K.) and 2021 OneMind Nick LeDeit Rising Star Research Award (Y.K.). This research was funded in whole or in part by Aligning Science Across Parkinson’s [ASAP- 020600] through the Michael J. Fox Foundation for Parkinson’s Research (MJFF) (L.P.). For the purpose of open access, the author has applied a CC BY public copyright license to all Author Accepted Manuscripts arising from this submission. Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number T32GM105538 (M.M.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Imaging work was performed at the Northwestern University Center for Advanced Microscopy (RRID:SRC_020996), generously supported by NCICCSGP30 CA060553, awarded to the Robert H Lurie Comprehensive Cancer Center.
Author information
Authors and Affiliations
Contributions
Conceptualization, CC, LP; scientific input, DA, EG, SH, and YG; methodology, CC, MM, NS, VP, GT, CM; molecular and anatomical methods CC; electrophysiological measurements, MM and YK; behavioral tests, CC, VP, GT, data curation, formal analysis, CM; formal analysis, NS, writing first draft, CC, and LP; writing, review and editing, all authors; funding acquisition, LP YK; supervision, LP.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. All mouse experiments were approved by Northwestern University Animal Care and Use Committee (approved protocol numbers IS00019801, and IS00030531).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, C., Masotti, M., Shepard, N. et al. LRRK2 mediates haloperidol-induced changes in indirect pathway striatal projection neurons. Mol Psychiatry (2025). https://doi.org/10.1038/s41380-025-03030-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-025-03030-z