Abstract
Background
This study aimed to identify contextual factors associated with life satisfaction during the COVID-19 pandemic for adolescents with mental, emotional, behavioral, and developmental (MEBD) disabilities.
Methods
Data were collected from a sample of 1084 adolescents aged 11–21 years from April 2020 to August 2021. This cross-sectional study used a sequential machine learning workflow, consisting of random forest regression and evolutionary tree regression, to identify subgroups of adolescents in the Environmental influences on Child Health Outcomes (ECHO) consortium who demonstrated enhanced vulnerability to lower life satisfaction as described by intersecting risk factors, protective factors, and MEBD disabilities.
Results
Adolescents with a history of depression, anxiety, autism, and attention-deficit/hyperactivity disorder were particularly susceptible to decreased life satisfaction in response to unique combinations of stressors experienced during the COVID-19 pandemic. These stressors included decreased social connectedness, decreased family engagement, stress related to medical care access, pandemic-related traumatic stress, and single-caregiver households.
Conclusion
Findings from this study highlight the importance of interventions aimed specifically at increasing adolescent social connectedness, family engagement, and access to medical support for adolescents with MEBD disabilities, particularly in the face of stressors, such as a global pandemic.
Impact
-
Through a machine learning process, we identified contextualized risks associated with life satisfaction among adolescents with neurodevelopmental disabilities during the COVID-19 pandemic.
-
The COVID-19 pandemic resulted in large-scale social disruptions for children and families. Such disruptions were associated with worse mental health outcomes in the general pediatric population, but few studies have examined specific subgroups who may be at heightened risk. We endeavored to close that gap in knowledge.
-
This study highlights the importance of social connectedness, family engagement, and access to medical support as contributing factors to life satisfaction during the COVID-19 pandemic for adolescents with neurodevelopmental disabilities.
Similar content being viewed by others
Introduction
Health policies to curb the spread of the SARS-CoV-2 virus caused major disruptions for children and families. Schools were closed to in-person learning; extracurricular activities were canceled; and universal stay-at-home orders meant children spent more time quarantined with family members than engaging in social interactions with friends. Parents in the United States (US) reported that school closures were accompanied by a twofold increase in their children’s anxiety and depression compared with pre-closure levels,1 and 78% of parents in the US reported decreases in their children’s emotional well-being.2 Adolescents may be particularly vulnerable to social disruptions, as studies show the transition to adolescence is the beginning of a critical period of social development, where peer relationships are particularly salient.3 Lacking such social interactions may therefore put adolescents at increased risk for negative mental health outcomes.4 Emerging research suggests that older children and adolescents were at a greater risk than younger children for adverse mental health impacts during the COVID-19 pandemic, with approximately a quarter of youth worldwide meeting the criteria for depression and anxiety.5 Moreover, the pandemic increased financial hardships, especially among families already in poverty, which amplified the negative effects of the pandemic on youth mental health.6
To date, most research has focused on understanding the extent to which the COVID-19 pandemic impacted mental health across the general pediatric population. Fewer studies have examined the pandemic’s impact on youth with pre-existing developmental and behavioral disabilities. Limited research, primarily from the early months of the pandemic, suggests amplified psychosocial impacts of the pandemic for children with depression, anxiety, attention-deficit/hyperactivity disorder (ADHD), and autism.7,8 Further, with few exceptions, prior work focused exclusively on negative mental health outcomes resulting from the COVID-19 pandemic.9,10 Alternatively, focusing on positive psychological well-being (e.g., life satisfaction) can provide additional insight into youth’s pandemic experiences given that the two constructs (negative and positive psychological health) are related but not direct opposites, such that evaluating one does not provide a proxy for the other. Further, identifying risk and protective factors across development and the broader social ecology that alter responses to adversity are critical to understanding the differential impact of the pandemic on youth and may be targeted to improve outcomes or identify those requiring more intensive recovery efforts.
To address these limitations, the current study draws on a large, diverse sample of adolescents from the National Institutes of Health (NIH) Environmental influences on Child Health Outcomes (ECHO) research program11,12 to investigate differences in life satisfaction for children with and without pre-existing mental, emotional, behavioral, and developmental (MEBD) conditions across person-level experiences of potential COVID-19 pandemic–related risk factors (financial hardship, stress) and protective factors (social connectedness, family engagement). The primary aim of this paper was to identify the contextualized characteristics and experiences of individuals that can inform mental health practitioners, as well as general pediatricians and family physicians, who are often charged with supporting children’s mental health, in order inform potential intervention targets among adolescents with disabilities. We used a sequential machine learning workflow to identify subgroups of adolescents who demonstrated enhanced vulnerability to lower life satisfaction as described by intersecting risk and protective factors and MEBD conditions.
Methods
Sample
Data came from the ECHO consortium, consisting of over 61,000 children drawn from 69 longitudinal cohort studies across the US11,12 Aligned with previous work indicating that adolescence represents a developmental period beginning with the onset of puberty and ending in the mid-20s, the study sample for this analysis included 1084 adolescents (11–21 years of age) and their caregivers across seven ECHO cohorts in the US13 This cross-sectional study included 1084 ECHO dyads, which represented all adolescent and caregiver pairs for whom COVID-19 survey data were collected between April 2020 and August 2021. ECHO COVID-19 self-report assessments were completed separately by caregivers and adolescents. All data collection, informed consent procedures, and analysis activities were approved by local and/or central ECHO Institutional Review Boards. Written informed consent or parent’s/guardian’s permission was obtained along with child assent as appropriate, for ECHO-wide Cohort Data Collection Protocol participation and for participation in specific cohorts.
Measures
Apart from pre-existing MEBD conditions and sociodemographic variables, all measures were obtained from the ECHO COVID-19 questionnaires, which were developed in March 2020 to capture the physical, mental, and social impact of the COVID-19 pandemic on youth and families.9 Although it is clear that some racial and ethnic groups have been more adversely affected by the pandemic than others,14 there is no prior literature to suggest that race or ethnicity would intersect with pandemic-related stress, family hardships, or connectedness and engagement to differentially predict adolescent life satisfaction. Furthermore, with respect to the COVID-19 pandemic, Massion and colleagues have cautioned against unwarranted statistical adjustments and the perpetuation of stereotypes, instead recommending that researchers focus on identifying underlying and modifiable risks.15 Race and ethnicity, “frequently included in analytic models either as poor proxies for other constructs or without any justification at all,”16 were not included as predictors in the current study.
Adolescent life satisfaction, the outcome variable, was measured using a single item adapted from the Patient-Reported Outcome Measurement Information System (PROMIS®) Life Satisfaction instrument.17 Adolescents were asked, “Since becoming aware of the COVID-19 outbreak, how often have you felt happy and satisfied with your life?” The item was scored on a 5-point Likert scale from not at all (1) to very often (5).
COVID-19 pandemic–related traumatic stress was measured via adolescent and caregiver self-report using the 9-item Pandemic-related Traumatic Stress Scale (PTSS),18 which is aligned to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria for acute stress disorder (i.e., intrusive thoughts, negative mood, disassociation, avoidance, arousal).19 Each item was scored on a 5-point Likert scale from not at all (1) to very often (5), and a total average score was computed (range: 1-5). The adult and adolescent PTSS scales had alpha values of 0.84 and 0.86, respectively, in the validation samples.20
COVID-19 pandemic–related family hardships were reported by caregivers across nine domains: concerns about health, impact on the child, impact on the community, financial stress, food insecurity, social distancing/quarantine, access to medical care, difficulty finding childcare, and rearranging work schedules to accommodate childcare. Items were modified from the COVID-19 Perinatal Experiences Impact Survey (COPE-IS).21
Social connectedness reflected adolescents’ self-reported current level of social connectedness (i.e., feelings of interpersonal closeness and a sense of belonging to a social group22) compared with before the COVID-19 pandemic using a 6-point Likert scale from much less socially connected (1) to much more socially connected (6). This item was modified from the Adolescent Social Connection and Coping during COVID-19 Questionnaire.23
Family and social engagement items were adapted from the COVID-19 Perinatal Experiences Impact Survey (COPE-IS).21 Adolescents were asked one item regarding engaging in more family activities (0=no, 1=yes). Caregivers were asked two items indicating whether they (1) talked to friends and family and (2) engaged in more family activities (both scored 0=no, 1=yes), which we averaged (possible values = 0, 0.5, 1).
Pre-existing MEBD diagnoses were captured through caregiver report on whether the adolescent was ever diagnosed with anxiety, depression, ADHD, autism, or an intellectual disability. Each diagnosis was treated as a separate binary indicator (1=yes).
Other predictors of interest included cohort membership, adolescent age in years, sex assigned at birth (male, female), primary caregiver highest educational attainment (high school degree or less; some college; college degree; master’s, professional, or doctorate degree), and whether the adolescent ever received a COVID-19 diagnosis.
Analytic approach
In this study, we used a sequential, supervised, tree-based machine learning workflow, starting with random forest regression24 to select predictors. Evolutionary tree regression (i.e., evtree algorithm)25 was then used to identify which subsamples were most vulnerable to, or protected from, COVID-19–related reductions in life satisfaction, focusing specifically on contextual risks that involved the presence/absence of MEBD conditions. The Supplemental Material offers more background and details on our analytic approach.
First, we used the mice package26 in R to generate 10 completed data sets, with missing values substituted by multiple imputed values. We then used each imputed data set to optimize the random forest complexity parameters using the caret package27 in R. We then estimated a final random forest model with the stacked data set (i.e., treated as a single data set) using the average complexity parameter from the imputation-specific random forests. From this stacked random forest, we obtained estimates of variable importance for all predictors of life satisfaction. In the subsequent evolutionary tree analysis, we removed any variable with an importance less than 10% of the maximum observed importance value, with the exception that, regardless of estimated importance, all indicators of MEBD conditions were included in evolutionary trees. We then estimated our final evolutionary trees using the stacked data set. Although each individual run of the evtree algorithm always yields a single tree, multiple random starts do not always yield the same exact solution. Therefore, to balance the computational intensiveness of the evtree algorithm with interpretation difficulty due to model complexity, we estimated five trees using the default tuning parameters in the evtree package, interpreting all five as plausible representations of the data.
Results
Table 1 includes descriptive statistics for all predictors as well as child race and ethnicity. 65.9% of participants were White, 22.8% were Black, and the remaining 11.3% were missing or another race. 91.9% of the sample was non-Hispanic. With respect to parent reports of MEBD diagnoses, 18.5% of our sample was diagnosed with anxiety, 11.4% with depression, 5.4% with autism, 19% with ADHD, and 3% with intellectual disability. 67% of our sample had no MEBD diagnoses, 16.9% had one, and the remaining 16.1% had more than one condition.
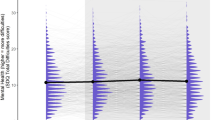
Random forest regression
Of the 25 candidate predictors, the following six variables had importance values <10% of the maximum observed importance value: cohort membership, difficulty finding childcare, work schedule changes to accommodate childcare, an adolescent’s COVID-19 diagnosis, and the indicators for intellectual disability and autism. We retained indicators for intellectual disability and autism as they were of primary interest in this study but removed the other three variables from further analyses. Therefore, the final evolutionary tree model was estimated with the following predictors: (1) hardships: concerns about health, impact on the child, impact on the community, financial stress, food insecurity, social distancing/quarantine, and access to medical care; (2) adolescent pre-existing MEBD conditions: anxiety, depression, autism, ADHD, and intellectual disability; (3) caregiver and adolescent pandemic-related traumatic stress; (4) adolescent social connectedness; (5) adolescent family/social engagement; (6) caregiver family/social engagement; and (7) sociodemographics: adolescent age and sex, and caregiver educational attainment and marital status.
Evolutionary tree regression
In total, five evolutionary trees were estimated. The two tree solutions discussed in this article (Trees 1 and 2) were comparable with respect to root-mean-square error (RMSE) but differed with respect to some of the variables used, splits, and ultimately the branches. Trees 3, 4, and 5 can be found in the Supplementary Material (Supplementary Fig. 1, Supplementary Fig. 2, Supplementary Fig. 3). Despite having similar, and in some cases equivalent, branches, Trees 3, 4, and 5 are not discussed here because all branches related to MEBD conditions were redundant, approximately or exactly, with the branches discussed in Trees 1 and 2. That is, Trees 3, 4, and 5 did not include unique information beyond what was captured in Trees 1 and 2.
As the primary focus of this study was understanding the COVID-19 experience of adolescents with MEBD disabilities, we focused on branches involving MEBD indicators. Depression, anxiety, autism, and ADHD emerged as predictors of differential vulnerability with respect to adolescent life satisfaction, while intellectual disability did not. The standard deviation of life satisfaction in this study’s sample was 0.96, which will be referenced throughout to frame group comparisons.
Depression
Findings related to depression appeared only in Tree 1. Differences between adolescents with and without a history of depression manifested within the subset of the sample defined by a social connectedness score \(\ge\)2 (which spans the range from less to more socially connected during the pandemic) and a traumatic stress score <2.67, which was essentially at the mean value (2.56; SD = 0.77). Adolescents with previous depression diagnoses whose parents were married/cohabitating had an average life satisfaction of 3.56. Among the group of adolescents with depression, those whose caregivers were divorced/not-cohabiting had an average life satisfaction of 1.86, which was 1.63 standard deviations lower than their peers with married/cohabiting caregivers, when their separated caregivers expressed stress related to medical care access. When stress related to medical care access was not endorsed, adolescents with caregivers whose family/social engagement was equal to one (i.e., talked to friends and family and engaged in more family activities) had an average life satisfaction of 3.84, which was nearly one standard deviation higher than the average life satisfaction of adolescents whose caregivers had family/social engagement scores <1 (mean life satisfaction = 2.91). In contrast to the five terminal nodes (subgroups) that included adolescents with depression, eight terminal nodes among adolescents without depression had mean life satisfaction scores ranging from 3.20 to 4.35.
Anxiety
Findings related to anxiety appear in Tree 1 and Tree 2. In both trees, differences between adolescents with and without a history of anxiety manifested within the subset of adolescents whose social connectedness was negatively impacted during the pandemic and who had above-average traumatic stress, but other branching patterns differed between the trees (Figs. 1, 2). In Tree 2, adolescents with pre-existing anxiety diagnoses and higher COVID-19–related traumatic stress (\(\ge\)2.56) had a lower life satisfaction than individuals with lower COVID-19-related traumatic stress (<2.56), with mean life satisfaction scores of 1.85 and 2.56, respectively. In Tree 1, this same split manifested at the same threshold, but only among adolescents with pre-existing anxiety diagnoses whose caregivers did not report being stressed over access to medical care (means of 2.01 and 2.74, respectively), whereas such adolescents whose caregivers reported medical care–related stress had the lowest life satisfaction (1.79).
AcuteStress Caregiver-reported COVID-19 pandemic-related traumatic stress, ADHD Adolescent ADHD diagnosis, AdultEngage Caregiver-reported social engagement as coping mechanism, Age adolescent age, Anxiety Adolescent anxiety diagnosis, Depression Adolescent depression diagnosis, Marital Caregiver marital status, Medical Caregiver-reported stress related to medical care, Sex Adolescent biological sex, Social Adolescent Social Connectedness, StressCommunity Caregiver-reported community stress during COVID-19 pandemic, StressFood Caregiver-reported stress related to the availability of food, TeenEngage Adolescent-reported family engagement as coping mechanism, Trauma Adolescent COVID-19 pandemic-related traumatic stress, Quarantine caregiver-reported stress related to quarantine.
AcuteStress Caregiver-reported COVID-19 pandemic-related traumatic stress, ADHD Adolescent ADHD diagnosis, Age adolescent age, Anxiety Adolescent anxiety diagnosis, ASD Adolescent autism, Social Adolescent Social Connectedness, TeenEngage Adolescent-reported family engagement as coping mechanism, Trauma Adolescent COVID-19 pandemic-related traumatic stress.
Autism
Tree 2 indicated that autism emerged as a meaningful factor in adolescents with below-average traumatic stress whose social connectedness was reduced during the pandemic and who indicated that family engagement was used as a coping strategy. Autistic individuals had an average life satisfaction of 2.98, which was one standard deviation lower compared with their typically developing peers (mean = 4.01; Tree 2).
Attention-deficit/hyperactivity disorder
Differences between adolescents with and without a history of ADHD manifested within three branches (from separate trees). In Tree 2, ADHD emerged as a meaningful predictor when adolescents did not endorse family engagement as a coping strategy; they were further differentiated based on age. Adolescents with ADHD who were \(\ge\)16.6 years of age had an average life satisfaction of 2.58, which was about one standard deviation lower compared with their younger counterparts with ADHD (mean = 3.65; Tree 2). In contrast, individuals without ADHD in this subset had a weighted average life satisfaction of 3.74. Transitioning to the first Tree 1 branch with ADHD, age and adolescent family engagement were not included, but this group contained no individuals with previous depression diagnoses. In this branch, individuals with ADHD had an average life satisfaction of 3.46, which was a one-half standard deviation decrease in life satisfaction compared with adolescents without ADHD (mean = 3.87; Tree 1). In contrast, the second Tree 1 branch containing ADHD included adolescents who were older than 15.99 years, who experienced decreased social connectedness, below-average trauma, no community stress, and no food stress. These adolescents with ADHD had a mean life satisfaction of 2.25 compared to their counterparts without ADHD who had a mean life satisfaction equal to 3.3, a decrease of slightly more than a standard deviation.
Discussion
The purpose of this study was to elucidate how life satisfaction varied among groups of adolescents with and without pre-existing MEBD disabilities during the COVID-19 pandemic based on family-level hardships, pandemic-related traumatic stress, family engagement, and social connectedness. The results from the sequential, tree-based machine learning approach used in this study uncovered differential vulnerabilities with respect to life satisfaction for adolescents with pre-existing diagnoses of depression, anxiety, autism, and ADHD in addition to potential protective factors that may be important intervention targets.
Particularly for adolescents with a history of depression, this study highlighted the protective nature of having caregivers who live together, possibly due to increased stability of the family unit. Compared to the weighted average of adolescents with pre-existing depression who lived in single-caregiver households, those in dual-caregiver households had an average life satisfaction level about 0.69 standard deviations higher on average. The evolutionary tree indicated that among adolescents with depression who felt less socially connected than they did before the pandemic, those in dual-caregiver households reported a higher life satisfaction. These results provide further evidence of the differential vulnerability of adolescents in single-caregiver households who demonstrated higher rates of emotional instability during the pandemic.28 Decreased social connectedness among adolescents with previous depression diagnoses may have been compounded by a lack of access to caregiver support and a host of other challenges faced by single-caregiver households, such as the stress associated with financial insecurity.29
Adolescents with previous anxiety diagnoses who experienced above-average traumatic stress and whose caregivers were concerned about access to medical care emerged as the subgroup with the lowest life satisfaction. This finding supports previous work in adults with pre-existing anxiety conditions during the pandemic that showed higher levels of COVID-19–related stress, voluntary self-isolation, and self-isolation stressors.30 Alternatively, adolescents whose caregivers did not report being stressed over medical care access had an average life satisfaction that was nearly one-half standard deviation higher than adolescents whose caregivers reported this source of stress. This finding suggests that access to medical care may be an important protective factor for adolescents with anxiety who experienced traumatic stress.
The finding that autism only appeared as a split in the evolutionary tree for adolescents with below-average traumatic stress and decreased social connectedness who indicated they were engaged with their families during the pandemic suggests that decreased social engagement was especially deleterious for autistic individuals. It follows, however, that life satisfaction ratings among autistic individuals were not distinguishable from their typically developing peers when social connectedness was not impacted during the pandemic or when individuals’ pandemic-related traumatic stress was high. Such findings highlight the protective factor of social connectedness and reflect the importance of evaluating positive psychological well-being rather than only assessing negative mental health outcomes. These findings reflect and add additional context to recent work suggesting that children with chronic conditions (both neurodevelopmental and physical) can have similar levels of life satisfaction as their peers without chronic conditions,31,32 which in this study was contingent on social connectedness. These findings highlight the importance of continued access to social support services for autistic adolescents, particularly during periods of mandated or encouraged social isolation.
Adolescents with a history of ADHD emerged as a vulnerable group when they had below-average traumatic stress, did not endorse family engagement as a coping strategy (Tree 2), had reduced social connectedness during the pandemic and no previous depression diagnosis (Tree 1, upper ADHD split), or were older but did not experience stress related to community or food during the COVID-19 pandemic (Tree 1, lower ADHD split). These adolescents with ADHD had average life satisfaction about one-half and one standard deviation lower than their peers who did not have ADHD, respectively. These findings support earlier work that showed adolescents with ADHD experienced greater increases in mental health symptoms compared with their peers without ADHD and work suggesting that positive coping strategies, such as family engagement, can protect against such increases.33
More broadly, this study found that 80% of adolescents, regardless of pre-existing conditions, reported decreases in social connectedness during the COVID-19 pandemic. Although the deleterious effect of decreased social connectedness was amplified among individuals with certain MEBD conditions, this risk factor, which was included in several complex, multi-way interactions, was widespread even among adolescents without additional vulnerabilities during a developmental period when social connection is paramount. Future research should include investigations of the long-term impacts of decreased social connection and other contextual risks resulting from responses to the COVID-19 pandemic during developmentally critical time periods. Furthermore, findings from this study provide insight into potential differences between adolescents with disabilities and their typically developing peers in terms of life satisfaction in the context of individual- and family-level factors—the results also identify salient subgroups of adolescents with disabilities that warrant further investigation. Therefore, we encourage future researchers to design inquires that target vulnerable subgroups identified in this study.
Limitations
First, due to the lack of pre-pandemic life satisfaction data for this sample, we were unable to identify changes in well-being resulting from the pandemic. However, the emphasis here was on identifying clinically informative contextualized characteristics and experiences of adolescents with disabilities as potential intervention targets vs. assessing changes in well-being over time. Related to the measure of life satisfaction, we acknowledge that using a single item to measure this construct is limited with respect to reliability and the breadth of the dimension. Although caregiver stress over access to medical care was a meaningful predictor in the final evolutionary tree, this variable did not differentiate between mental vs. physical healthcare. The MEBD conditions for adolescents referred to any previous diagnoses; therefore, diagnoses may not have been current and MEBD treatments (e.g., medication) were not included in these analyses. Further research should investigate whether current vs. past diagnosis and/or MEBD treatments influence the identified risks associated with MEBD conditions and decreased life satisfaction. Although we believe the evolutionary tree analysis used in this study constitutes a sophisticated, powerful technique for uncovering complex vulnerabilities and compound risk, comorbidities among diagnoses complicate interpretation because of potential effect masking. Therefore, we recommend that these findings be used to guide further clinical inquiry but not be considered sufficient to guide policy or intervention in the absence of further research. Furthermore, we were primarily interested in modifiable risk factors; given known disparities with respect to non-modifiable risk factors like race and ethnicity,14 as well as cautionary notes encouraging researchers to focus on underlying factors,15 we opted to exclude such risk factors from the model to avoid excessive collinearity leading to spurious and difficult-to-interpret splits. Future work applying similar methods to the question of equity would be a valuable contribution to the literature. Finally, we excluded participants without available data on the COVID-19 self-report survey, including adolescents with cognitive impairment which precluded them from self-reporting to the questionnaire. Adolescents with cognitive impairments represent a population of interest whose differential life satisfaction should be explored in future work, with special attention to measurement issues inherent in assessing this population.
Conclusion
This study provided evidence that adolescents with a history of depression, anxiety, autism, and ADHD are particularly susceptible to decreased life satisfaction in response to unique combinations of stressors experienced during the COVID-19 pandemic. These stressors include decreased social connectedness, decreased family engagement, stress related to medical care access, traumatic stress, and single-caregiver households. Taken together, these findings highlight the importance of interventions aimed specifically at increasing adolescent social connectedness, family engagement, and access to medical support for adolescents with MEBD disabilities, particularly in the face of stressors, such as a global pandemic.
Data availability
De-identified data from the ECHO Program are available through NICHD’s Data and Specimen Hub (DASH) (https://dash.nichd.nih.gov). DASH is a centralized resource that allows researchers to access data from various studies via a controlled-access mechanism. Researchers can now request access to these data by creating a DASH account and submitting a Data Request Form. The NICHD DASH Data Access Committee will review the request and provide a response in approximately two to three weeks. Once granted access, researchers will be able to use the data for three years. See the DASH Tutorial for more detailed information on the process (https://dash.nichd.nih.gov/resource/tutorial).
References
Raviv, T. et al. Caregiver perceptions of children’s psychological well-being during the COVID-19 pandemic. JAMA Netw. Open 4, e2111103 (2021).
Martinelli K., Cohen Y., Kimball H., Sheldon-Dean H. 2020 children’s mental health report: Telehealth in an increasingly virtual world. Child Mind Institute. https://childmind.org/awareness-campaigns/childrens-mental-health-report/2020-childrens-mental-health-report/. Published 2020. Accessed February 27, 2023.
Blakemore, S. J. & Mills, K. L. Is adolescence a sensitive period for sociocultural processing? Annu Rev. Psychol. 65, 187–207 (2014).
Orben, A., Tomova, L. & Blakemore, S.-J. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc. Health 4, 634–640 (2020).
Racine, N. et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatr. 175, 1142–1150 (2021).
Whitehead M., Taylor-robinson D., Barr B. Poverty, health, and covid-19 yet again, poor families will be hardest hit bytthe pandemic’s long economic fallout. BMJ. 372, (2021).
Nonweiler, J. et al. Prevalence and associated factors of emotional and behavioural difficulties during COVID-19 pandemic in children with neurodevelopmental disorders. Children 7, 128 (2020).
Shorey, S. et al. Families with children with neurodevelopmental disorders during COVID-19: A scoping review. J. Pediatr. Psychol. 46, 514–525 (2021).
Blackwell C. K. et al. Youth well-being during the COVID-19 pandemic. Pediatrics. 149, (2022).
Paizan, M. A., Benbow, A. E., Aumann, L. & Titzmann, P. F. Home-learning during COVID-19: The psychological adjustment of minority and majority adolescents. Sch. Psychol. 37, 75–84 (2021).
Blaisdell, C. J. et al. The NIH ECHO program: Investigating how early environmental influences affect child health. Pediatr. Res. 92, 1215–1216 (2022).
Gillman, M. W. & Blaisdell, C. J. Environmental influences on Child Health Outcomes, a research program of the National Institutes of Health. Curr. Opin. Pediatr. 30, 260–262 (2018).
National Academies of Sciences E, Medicine. The promise of adolescence: Realizing opportunity for all youth. Washington, DC, The National Academies Press 2019.
Mackey, K. et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths : A systematic review. Ann. Intern Med 174, 362–373 (2021).
Massion, S. P., Murry, V. M. & Grijalva, C. G. Racial disparities in COVID-19 outcomes: Unwarranted statistical adjustments and the perpetuation of stereotypes. Lancet Reg. Health Am. 14, 100352 (2022).
Chandran, A., Knapp, E., Liu, T. & Dean, L. T. A new era: Improving use of sociodemographic constructs in the analysis of pediatric cohort study data. Pediatr. Res. 90, 1132–1138 (2021).
Forrest, C. B. et al. Development and psychometric evaluation of the promis pediatric life satisfaction item banks, child-report, and parent-proxy editions. Qual. Life Res. 27, 217–234 (2018).
Margolis A. et al. Acute stress questions for ECHO COVID-19 survey. PsychArchives. (2021).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). 2013.
Blackwell, C. K. et al. Development and Psychometric Validation of the Pandemic-related Traumatic Stress Scale for Children and Adults. Psychol. Assess. (2023).
Thomason M. E., Graham A., VanTieghem M. R. The cope-is: Coronavirus perinatal experiences – impact survey. https://www.nlm.nih.gov/dr2/COPE-Impact_Survey_Perinatal_Pandemic_Survey.pdf Published 2020.
Lee, R. M. & Robbins, S. B. Measuring belongingness: The social connectedness and the social assurance scales. J. Counseling Psychol. 42, 232–241 (1995).
Pfeifer J. H. Adolescent social connection and coping during COVID questionnaire. https://osf.io/jakg5/. Published 2020.
Breiman, L. Random forests. Mach. Learn. 45, 5–32 (2001).
Grubinger, T., Zeileis, A. & Pfeiffer, K.-P. Evtree: Evolutionary learning of globally optimal classification and regression trees in r. J. Stat. Softw. 61, 1–29 (2014).
van Buuren, S. & Groothuis-Oudshoorn, K. Mice: Multivariate imputation by chained equations in r. J. Stat. Softw. 45, 1–67 (2011).
M. K. _caret: Classification and regression training_. R package version 6.0-92. https://CRAN.R-project.org/package=caret. Published 2022. Accessed February 27, 2023.
Naito T. et al. Did children in single-parent households have a higher probability of emotional instability during the COVID-19 pandemic? A nationwide cross-sectional study in japan. Int. J. Environ. Res. Public Health. 19, (2022).
Taylor, Z. E. et al. Strengths of the heart: Stressors, gratitude, and mental health in single mothers during the COVID-19 pandemic. J. Fam. Psychol. 36, 346–357 (2022).
Asmundson, G. J. G. et al. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J. Anxiety Disord. 74, 102271 (2020).
Blackwell, C. K. et al. General health and life satisfaction in children with chronic illness. Pediatrics 143, e20182988 (2019).
Schuchard, J. et al. Influences of chronic physical and mental health conditions on child and adolescent positive health. Acad. Pediatr. 22, 1024–1032 (2022).
Dvorsky, M. R. et al. Coping with COVID-19: Longitudinal impact of the pandemic on adjustment and links with coping for adolescents with and without adhd. Res. child Adolesc. Psychopathol. 50, 605–619 (2022).
Acknowledgements
We wish to thank our ECHO colleagues; the medical, nursing, and program staff; and the children and families participating in the ECHO cohorts.
Funding
Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) program, Office of the Director, National Institutes of Health, under Award Numbers U2COD023375 (Coordinating Center), U24OD023382 (Data Analysis Center), U24OD023319 with co-funding from the Office of Behavioral and Social Sciences Research (PRO Core), UH3OD023332 (Trasande), UH3OD023313 (Deoni), UH3OD023282 (Gern), UH3OD023389 (Leve, Neiderhiser, Ganiban), UH3OD023286 (Oken), UH3OD023348 (O’Shea), UH3OD023290 (Herbstman, Perera), UH3OD023249 (Stanford). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Consortia
Contributions
P.S. and M.M.: substantial contributions to conception and design, analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, final approval of the version to be published. C.K.B.: substantial contributions to conception and design, drafting the article or revising it critically for important intellectual content, final approval of the version to be published. C.B., Deoni, Fry, Ganiban, Herbstman, Leve, LeWinn, Margolis, Miller, Neiderhiser, Oken, O’Shea, and Stanford: acquisition of data and drafting the article or revising it critically for important intellectual content, final approval of the version to be published. D.C., R.G., J.-S.L. and P.D.Z.: drafting the article or revising it critically for important intellectual content, final approval of the version to be published. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Written informed consent or parent’s/guardian’s permission was obtained along with child assent as appropriate, for ECHO-wide Cohort Data Collection Protocol participation and for participation in specific cohorts.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sherlock, P., Mansolf, M., Blackwell, C.K. et al. Life satisfaction for adolescents with developmental and behavioral disabilities during the COVID-19 pandemic. Pediatr Res 95, 827–834 (2024). https://doi.org/10.1038/s41390-023-02852-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02852-3