Abstract
Objective
This study aims to systematically review all adverse events (AEs) associated with orotracheal intubation in pediatric patients, with the ultimate goal of aiding healthcare center administration in establishing evidence-based guidelines and devising preventive strategies to mitigate AEs in pediatric intubation procedures.
Methods
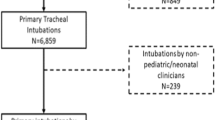
Systematic automated searches across pivotal databases were conducted up to 2023. The screening process was facilitated by EndNote X9 following the importation of citations. Data extraction was guided by predefined eligibility criteria after the elimination of duplicates and ineligible publications. The National Institutes of Health (NIH) quality evaluation instrument was employed to assess biases.
Results
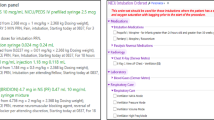
A total of twenty-four studies spanning from 2002 to 2023, encompassing 7135 patients were included in the analysis. Among the identified adverse events, moderate desaturation(≤90%) emerged as the most prevalent, affecting 508/2398 (23.9%, 95% CI: 17.6% to 30.3%) of cases across 13 studies. Mainstem intubation was observed in 342 out of 4,481 cases (9.1%, 95% CI: 6.3% to 11.9%) and in 173 out of 3903 cases (3.9%, 95% CI: 2.5% to 5.3%), making these significant AEs. Cardiac complications, including arrhythmias 55/3858 (1.2%, 95% CI: 0.6% to 1.8%), hypotension 121/4536 (2.6%, 95% CI: 1.5% to 3.7%), and cardiac arrest 105/4836 (1.4%, 95% CI: 0.7% to 2.2%), were observed in 10, 11, and 11 trials, respectively. Severe complications, with an incidence rate of 274/3298 (8.8%, 95% CI: 4.2% to 13.3%), were reported in five studies.
Conclusion
This comprehensive investigation and subsequent meta-analysis of adverse events associated with pediatric intubation provide valuable insights that can inform the development of enhanced safety protocols and evidence-based guidelines for pediatric emergency care.
Impact
-
High Success Rate with Complications: An 84.7% intubation success rate is reported, with a 30.1% complication rate, including desaturation, mainstem and esophageal intubation, and cardiac issues.
-
Need for Enhanced Safety Measures: Findings stress the importance of better training and standardized protocols to reduce complications in pediatric emergency intubation.
-
Focus on Adverse Events: This study uniquely highlights adverse events, offering crucial data for developing guidelines to improve safety in pediatric intubation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
269,00 € per year
only 19,21 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
The dataset supporting the conclusions of this article is included within the article and its Supplementary file 1.
References
Nishisaki, A. et al. Characterization of tracheal intubation process of care and safety outcomes in a tertiary pediatric intensive care unit. Pediatr. Crit. Care Med. 13, e5–e10 (2012).
Nishisaki, A. et al. A National Emergency Airway Registry for children: landscape of tracheal intubation in 15 PICUs. Crit. Care Med. 41, 874–885 (2013).
Griesdale, D. E. et al. Complications of endotracheal intubation in the critically ill. Intensive Care Med. 34, 1835–1842 (2008).
Sagarin, M. J. et al. Rapid sequence intubation for pediatric emergency airway management. Pediatr. Emerg. Care 18, 417–423 (2002).
Walls, R. M. et al. Emergency airway management: a multi-center report of 8937 emergency department intubations. J. Emerg. Med. 41, 347–354 (2011).
Kojima, T. et al. Epidemiology of adverse events attributed to airway management in paediatric anaesthesia: protocol for the prospective, multicentre, registry-based, cross-sectional Japan Pediatric Difficult Airway in Anesthesia study (J-PEDIA). BMJ Open 13, e067554 (2023).
Heinrich, S. et al. Incidence and predictors of difficult laryngoscopy in 11,219 pediatric anesthesia procedures. Paediatr. Anaesth. 22, 729–736 (2012).
Russotto, V. et al. Intubation practices and adverse peri-intubation events in critically ill patients from 29 countries. Jama 325, 1164–1172 (2021).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71 (2021).
Higgins J. P. T. et al. (editors). Cochrane handbook for systematic reviews of interventions. Version 6.2 [updated February 2021]. Cochrane Handbook Syst. Rev. Interven. (2021).
Miller, S. A. & Forrest, J. L. Enhancing your practice through evidence-based decision making: PICO, learning how to ask good questions. J. Evid. Based Dent. Pract. 1, 136–141 (2001).
Institution N. H. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
Capone, C. A. et al. Intubation practice and outcomes among pediatric emergency departments: A report from National Emergency Airway Registry for Children (NEAR4KIDS). Acad. Emerg. Med. 29, 406–414 (2022).
Eisenberg, M. A., Green-Hopkins, I., Werner, H. & Nagler, J. Comparison between direct and video-assisted laryngoscopy for intubations in a pediatric emergency department. Acad. Emerg. Med. 23, 870–877 (2016).
Funakoshi, H. et al. Association between repeated tracheal intubation attempts and adverse events in children in the emergency department. Pediatr. Emerg. Care 38, e563–e568 (2022).
Ghedina, N. et al. Paediatric intubation in Australasian emergency departments: a report from the ANZEDAR. Emerg. Med. Australas. 32, 401–408 (2020).
Hagiwara, Y. et al. Airway management in the pediatric emergency department in Japan: A multicenter prospective observational study. Acute Med. Surg. 9, e798 (2022).
Kerrey, B. T. et al. Rapid sequence intubation for pediatric emergency patients: higher frequency of failed attempts and adverse effects found by video review. Ann. Emerg. Med. 60, 251–259 (2012).
Kim, J.-H. et al. Impact of intubator’s training level on first-pass success of endotracheal intubation in acute care settings: a four-center retrospective study. Children 9, 960 (2022).
Long, E., Sabato, S. & Babl, F. E. Endotracheal intubation in the pediatric emergency department. Pediatr. Anesthesia 24, 1204–1211 (2014).
Miller, K. A. et al. See one, see one, teach one–Decisions on allocating intubation opportunities in pediatric emergency medicine. AEM Educ. Train. 6, e10830 (2022).
O’Connell, K. J. et al. Process conformance is associated with successful first intubation attempt and lower odds of adverse events in a paediatric emergency setting. Emerg. Med. J. 36, 520–528 (2019).
Pacheco, G. S. et al. Intubation during pediatric cardiac arrest in the emergency department is associated with reduced first-pass success. Pediatr. Emerg. Care 38, e1271–e1276 (2022).
Pallin, D. J., Dwyer, R. C., Walls, R. M. & Brown, I. iiC. A. Investigators NI. Techniques and trends, success rates, and adverse events in emergency department pediatric intubations: a report from the National Emergency Airway Registry. Ann. Emerg. Med. 67, 610–615 (2016).
Pek, J. H. & Ong, G. Y.-K. Emergency intubations in a high-volume pediatric emergency department. Pediatr. Emerg. Care 34, 852–856 (2018).
Schmidt, S. K. et al. Frequency and characterization of tracheal intubation adverse events in pediatric sepsis. Pediatr. Crit. Care Med. 19, e80–e87 (2018).
Shah, A. et al. Don’t hold your breath—a video-based study of procedural intervals during pediatric rapid sequence intubation. Pediatr. Emerg. Care 38, e784–e790 (2022).
Shiima, Y., Hsieh, T.-C., Long, A. & Donoghue, A. Videographic assessment of pediatric tracheal intubation technique during emergency airway management. Pediatr. Crit. Care Med. 19, e136–e144 (2018).
Sukys, G. A., Schvartsman, C. & Reis, A. G. Evaluation of rapid sequence intubation in the pediatric emergency department. J. de. Pediatr. 87, 343–349 (2011).
To, Y. H. et al. Differences in intubation outcomes for pediatric patients between pediatric and general Emergency Departments. Pediatr. Anesth. 31, 713–719 (2021).
Yurtseven, A., Turan, C., Kılınç, M. A. & Saz, E. U. Frequency and outcomes of endotracheal intubation in the pediatric emergency department. Turk. J. Pediatr. 59, 524–530 (2017).
Cicek A. et al. Endotracheal intubation practice from a pediatric emergency clinic of a tertiary hospital in Turkey. Ann. Clin. Anal. Med. (2022).
Couto T. B. et al Changing the view: Video versus direct laryngoscopy for intubation in the pediatric emergency department. Medicine (Baltimore). 99, e22289 (2020).
Edmunds, K., Sabato, S., Babl, F. E. & Long, E. Fraction of expired oxygen as a measure of preoxygenation prior to rapid sequence intubation in the pediatric emergency department. J. Emerg. Med. 63, 62–71 (2022).
Matettore, A. et al. Adverse tracheal intubation-associated events in pediatric patients at nonspecialist centers: a multicenter prospective observational study*. Pediatr. Crit. Care Med. 20, 518–526 (2019).
Abid, E. S., Miller, K. A., Monuteaux, M. C. & Nagler, J. Association between the number of endotracheal intubation attempts and rates of adverse events in a paediatric emergency department. Emerg. Med J. 39, 601–607 (2022).
Lee, J. et al. Pediatric Acute Lung Injury and Sepsis Investigators (PALISI); National Emergency Airway Registry for Children (NEAR4KIDS): The number of tracheal intubation attempts matters! A prospective multi-institutional pediatric observational study. BMC Pediatr. 16, 58 (2016).
Pallin, D. J., Dwyer, R. C., Walls, R. M., Brown, I. I. I. C. A. & Investigators, N. I. Techniques and trends, success rates, and adverse events in emergency department pediatric intubations: a report from the National Emergency Airway Registry. Ann. Emerg. Med. 67, 610–615.e1 (2016).
Chen D. Y. et al. Factors that determine first intubation attempt success in high-risk neonates. Pediatr. Res. (2023).
Gupta, B. & Ahluwalia, P. Prediction of endotracheal tube size in the pediatric age group by ultrasound: A systematic review and meta-analysis. J. Anaesthesiol. Clin. Pharm. 38, 371–383 (2022).
Weihing, V. K., Crowe, E. H., Wang, H. E. & Ugalde, I. T. Prehospital airway management in the pediatric patient: A systematic review. Acad. Emerg. Med. 29, 765–771 (2022). Jun.
Schmölzer G. M., Roehr C. C. Techniques to ascertain correct endotracheal tube placement in neonates. Cochrane Database Syst Rev. 9, Cd010221. (2014).
Lin, M. J., Gurley, K. & Hoffmann, B. Bedside ultrasound for tracheal tube verification in pediatric emergency department and icu patients: a systematic review. Pediatr. Crit. Care Med. 17, e469–e476 (2016).
George, S. et al. Intubation practices for children in emergency departments and intensive care units across Australia and New Zealand: A survey of medical staff. EMA 32, 1052–1058 (2020).
Eich, C. et al. Reply to Letter: paediatric tracheal prehospital intubation—what makes different our practice across the ocean?. Resuscitation 81, 634–635 (2010).
Acknowledgements
The authors would like to thank Mahmoud M. Elhady; Faculty of Medicine, Benha university, Qalubiya, Egypt, email: [email protected] for his help.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
Mohammed Alsabri (M.A.) and Mohammed Sayed Aazoue (M.S.Z.) are considered co-first authors. M.A. proposed the project, wrote the protocol, participated in the screening and selection of studies, contributed to the conception and formulation of the article, and drafted, reviewed, and revised the manuscript. M.S.Z. contributed significantly to the protocol, conducted the search strategy, assisted with data analysis, and participated in the screening and selection of studies alongside Ala Ahmed (A.A.). Mohammed Al-Tawil (M.A.T.) and Ibrahim Kamal (I.K.) were involved in data extraction, quality assessment, and critical revision of the manuscript. I.K. also conducted the data analysis and contributed to the writing and revision of the final manuscript. In cases of discrepancies during data extraction or assessment, M.A. resolved the conflicts. E.B., A.Z., A.B., J.C., and M.S. provided substantial input in writing and revising the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alsabri, M., Kamal, I., Al-Tawil, M. et al. Adverse events in pediatric orotracheal intubation in the pediatric emergency department: systematic review and meta-analysis. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04142-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-025-04142-6