Abstract
Background/Objectives
Unfortunately, not all metastatic castration resistant prostate cancer (mCRPC) patients receive available life-prolonging systemic therapies, emphasizing the need to optimize mCRPC treatment selections. Better guidelines are necessary to determine genetic testing in prostate cancer.
Subjects/Methods
In this two-part expert opinion-based guide, we provide an expert consensus opinion on the utilization of germline and somatic testing to detect HRR alterations in patients with mCRPC. This guide was developed by a multidisciplinary expert panel that convened in 2023–2024, including representatives from medical oncology, urology, radiation oncology, pathology, medical genomics, and basic science.
Results/Conclusion
We argue for the widespread adoption of germline testing in all patients with prostate cancer and for somatic mutations testing in patients at the time of recurrent/metastatic disease. In this first part, we review how genomic testing is performed. We also review how to overcome certain barriers to integrate genetic and biomarker testing into clinical practice.
Similar content being viewed by others
Introduction
The incidence of prostate cancer (PCa) has risen, with nearly 300,000 new U.S. cases now projected per year [1], notably in aggressive, higher stage PCa [2,3,4]. Metastatic-castration-resistant-prostate-cancer (mCRPC) has a median overall survival (OS) of only ~2 years [5,6,7,8] and is the second leading cause of cancer death for U.S. males [1]. Unfortunately, not all mCRPC patients receive available life-prolonging systemic therapies, emphasizing the need to optimize mCRPC treatment selections [5,6,7,8,9].
mCRPC is clinically heterogenous, requiring treatments to be tailored to individual patient. Prognosis varies from months to many years based on the pattern of metastatic spread, disease burden, patient health, and tumor molecular features [10, 11]. In recent years, genomic analyses of primary prostate samples and metastatic tissue biopsies have attempted to uncover potentially actionable or targetable alterations [12,13,14,15,16,17]. With the wide availability of comprehensive genomic testing, analysis of a patient’s germline and acquired tumor-only (or “somatic”) genomic alterations can help prognosticate a patient’s course and predict treatment effectiveness. Germline testing also highlights familial cancer risk, prompting early screening of relatives. Unfortunately, the majority of patients still do not undergo the appropriate genetic testing [18].
The DNA damage repair (DDR) pathway with the most therapeutic relevance is homologous recombination repair (HRR). The identification of HRR deficiencies in PCa have led to life-prolonging therapies. Approximately 20-25% of mCRPC patients have germline and/or somatic alterations in HRR, resulting in loss of function [19, 20]. BRCA1 and BRCA2 (1% and 7-13% respectively) are therapeutically targetable, but also associated with a more aggressive PCa phenotype [19,20,21].
The relative ratio of pathogenic germline to somatic mutation events in DDR is highly dependent on the HRR genes interrogated [22]. One study identified that the ratio of germline to somatic alterations in BRCA1/2 genes was roughly 1:1, whereas other HRR genes such as ATM and CDK12 had a much higher ratio of HRR mutations that were somatic in origin relative to germline [23]. 70% of ATM alterations and 89% of CDK12 alterations were somatic, based on a validated computational algorithm [24].
Determining both the origin and precise nature of a mutation may influence treatment decisions by providing a granular assessment of a patient’s DNA damage repair machinery, influencing treatment selections. Many variables must be considered to correctly interpret an HRR genetic testing result. The specific gene and origin and type of mutation has direct therapeutic implications for PARP inhibitors. Whether a mutation is found only in germline DNA, somatic DNA, or in both may affect a patient’s course and expected response from a PARP inhibitor. Similarly, whether it affects one (“monoallelic”) or both alleles (i.e. “biallelic”) provides a clearer picture of a patient’s DDR machinery and likelihood to respond to a PARP inhibitor. Finally, whether a somatic mutation is found in tumor tissue as opposed to plasma (i.e. ctDNA) may influence whether a testing result will have a therapeutic implication.
Recent real-world data from 2014 to 2022 suggests an increase in genetic testing for HRR deficiency from <20% of patients to nearly 50% of patients, with significant disparities noted in the lack of testing particularly in patients with Medicaid, low functional status, earlier time periods, older age, and community/rural sites [25]. A recent report noted that although next generation sequencing testing rates have improved over time, the majority of patients still did not undergo testing [18]. Overcoming structural barriers and improved guidelines are needed to promote more testing.
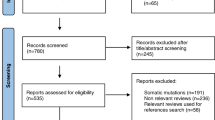
In this two-part expert opinion-based guide, we provide an expert consensus opinion on the utilization of germline and somatic testing to detect HRR alterations in patients with mCRPC (Fig. 1). This guide was developed by a multidisciplinary expert panel that convened in 2023–2024, including representatives from medical oncology, urology, radiation oncology, pathology, medical genomics, and basic science. We argue for the widespread adoption germline testing for all patients at the time of prostate cancer (PCa) diagnosis. Patients with metastatic hormone sensitive PCa (mHSPC) or mCRPC would subsequently qualify for somatic tumor genetic testing to determine eligibility for potential life-prolonging precision therapies. Tumor genetic testing is potentially not necessary for men with only localized PCa.
In this first part, we review how genomic testing is performed. We also review how to overcome certain barriers to integrate genetic and biomarker testing into clinical practice.
Who should be tested and when?
Per National Comprehensive Cancer Network (NCCN) guidelines, germline testing is currently recommended for patients with metastatic, node-positive, or high-risk localized PCa as well as for individuals with a family history of certain cancers (Table 1). To provide clarity for pathologists and medical oncologists, per NCCN guidelines germline testing may also be performed when pathologic review identifies intraductal or cribriform histology, or if a patient has a personal history of another malignancy associated with hereditary cancer syndromes (Table 1). Other societies, such as the American Urological Association, have similar recommendations [26, 27].
Germline multigene testing should include a minimum set of genes (Table 1) [28]. Genes such as HOXB13 may not be therapeutically actionable but can still be relevant depending on the clinical context for discussions including risk or family counseling.
We strongly recommend pre-testing counseling (either in-person or virtually) to address patient concerns over discrimination (e.g. life insurance eligibility), testing methodology and implications. Notable examples exist in the literature [29, 30]. Informed decision-making and consent is critical can be accomplished through video [30] or in-person discussions and documented through well-developed forms (see Fig. 2 for an example) [31]. Post-test counseling is recommended if germline testing reveals any pathogenic/likely pathogenic variants prompting cascade testing in relatives, or if a highly suspicious family history is not reflected in testing results.
Although NCCN guidelines recommend germline testing based on high-risk stratification criteria, such overly stringent testing criteria may miss pathogenic variants. Burgeoning evidence, including the PROCLAIM study [32], has demonstrated that the current paradigm of limiting germline genetic testing to patients with cancer thought to be at the highest risk for hereditary cancer syndromes is overly limiting. PROCLAIM found that even among patients with so-called low- or intermediate-risk disease, approximately 7.7% of patients still had a pathogenic gene variant (pooling together both germline and somatic variants). No significant difference was found in the prevalence of pathogenic gene variants among patients who met NCCN criteria for high-risk, versus those patients who were considered low- or intermediate-risk [2]. An estimated 42% of patients with pathogenic gene variants would be excluded utilizing current testing guidelines. This does not include the intraductal/cribiform histology patients referenced above.
When examining patients from under-represented populations, testing criteria were found to be even less effective at predicting the presence of a pathogenic gene variant. Many identified pathogenic gene variants in this study were actionable, implying a significant potential for impact on a patient’s clinical course when patients are excluded from germline testing [33].
Since current germline testing recommendations may miss patients with pathogenic/likely pathogenic variants, new data need to be collected to identify candidates for germline testing. The PROMISE registry aims to collect long-term to improve guideline recommendations [34]. Furthermore, discovery of index cases in a family will prompt genetic counseling and cascade testing for at-risk family members. As the costs of genetic testing decrease, expanded genetic testing becomes more feasible.
It is our recommendation (Fig. 1, Table 2) that all patients at the time of PCa diagnosis should undergo germline testing. Furthermore, we recommend that patients with recurrent, metastatic hormone sensitive PCa (mHSPC) or mCRPC subsequently undergo somatic tumor genetic testing to determine eligibility for potential prolonging precision therapies. Tumor genetic testing is potentially not necessary for men with only localized PCa. Future data may broaden these recommendations for germline or somatic testing and may have a large impact on clinical management and surveillance. Less than 50% of men are undergoing appropriate genetic testing [25] and we believe that the risks from a patient not undergoing the appropriate germline or somatic tumor testing are higher than any negative consequences from testing. However, we agree that financial barriers (see below) will still need to be addressed to ensure equity in the implementation of guidelines. However, we do not anticipate that insurance coverage for testing would change in the absence of these expert recommendations and guidelines.
The differences between somatic vs. germline testing are illustrated in Table 3. Over time, the mutational profile of a tumor may change, and false negatives will occur, thus repeated testing may be considered at the time of disease progression to evaluate for molecular changes that may influence next steps in treatment or clinical trial options [35]. One recent study identified that 11% of men with mCRPC harbored new actionable somatic alterations on repeat testing, predominantly ctDNA [35]. It is not yet clear whether new oncogenic alterations identified on repeat testing are clonal events that are equally predictive for targeted therapy benefit.
Patients should be informed prior to testing that many types of tumor testing may reveal germline findings, and that confirmatory germline testing may be recommended if such results are identified (Table 2). However, germline testing should not be replaced solely by somatic only testing, as this may lead to missed germline alterations in up to 20% of patients (Table 3) [36, 37]. NCCN recommends that multigene testing should be performed when somatic testing is pursued (Table 1). MSI-H or dMMR testing is additionally recommended for patients with regional or hormone-sensitive or castration-resistant prostate cancer, and TMB testing may be considered as well.
How to test and technical barriers
HRR gene alterations are considered early truncal events in PCa [19, 38]. Indeed, several studies have shown that primary prostate tissues (including needle core biopsies and radical prostatectomy specimens) reflect the mutational status of HRR genes in metastatic tissue [38, 39]. However, a significant fraction (10-40%) of cases yield no results or non-contributory results [40,41,42,43]. Nevertheless, archival formalin-fixed paraffin-embedded (FFPE) primary tumor samples make up most of samples submitted for HRR gene testing. It is therefore critical to consider factors that can increase the likelihood of obtaining informative NGS results.
Sample age, specimen type (resection, core needle biopsy, fine needle aspirate), tumor content, and DNA yield after extraction are the most relevant pre-analytical factors that impact NGS results [40, 41, 43]. Since DNA yield is a key determinant for a successful test, the amount of tumor tissue submitted for analysis is critical. Tumor tissue should be of high enough abundance (minimum 0.2 mm3), and the tumor cell fraction should be at least 25%. Tissue macrodissection can be used to increase the tumor fraction if necessary. Organ site is another determinant for the success of a sequencing test. While soft tissue sites (particularly lymph node biopsies) have the highest success rate, bone biopsies have reportedly lower rates (20–50%) [43]. This is likely due to lower tumor cellularity in bone biopsies as well as the loss of DNA integrity due to decalcification. For bone processing, it is recommended to avoid harsh acid-based decalcification methods and rather use ethylenediaminetetraacetic acid-based calcium extraction [43, 44].
An important consideration is that sample age affects the quality of the study, with younger samples showing higher success rates. This is likely a key limiting factor in cases where archival prostatectomy samples yield false negative results. Older archival specimens (>10 years) can still be used, but in such cases it is particularly important to submit ample tissue material to ensure high DNA yields after extraction [40, 43]. If only old archival material is available for a patient, resection specimens, ideally with high tumor cellularity, are preferred over core biopsies. However if new tissue is procured for NGS testing, ideally multiple core biopsies per lesion should be obtained. The lower DNA yield and DNA integrity present in some older FFPE samples can result in lower quality sequencing studies and challenges in data interpretation.
Finally, a negative initial tumor test, particularly using HSPC tissue, does not rule out a pathogenic germline alteration nor a new mCRPC somatic event [19]. Germline and repeat somatic testing may be recommended in such cases (Table 2). Repeat testing is obvious if the initial sample is insufficient, but even if sufficient, there is evidence that there were clearly identified late mCRPC events that were BRCA2 or MSI-H and missed in the original mHSPC tissue [35]. We acknowledge there is only limited retrospective data that repeat genomic testing can be informative unless there is a question regarding the quality of the initial testing (e.g. tumor purity, inadequate depth of sequencing).
Comparing ctDNA and tissue testing
In cases where archival tissue is unavailable and obtaining a new tissue biopsy is not feasible, NGS-based HRR gene testing of circulating tumor DNA (ctDNA) from peripheral blood draw offers an alternative [45,46,47,48]. There are also inherent advantages in profiling the latest available sample from a patient with advanced disease. However, metastatic PCa presents challenges for collection of a tissue specimen since metastases are often confined to bone, requiring a technically difficult, invasive biopsy [49, 50]. Genomic profiling of ctDNA from plasma provide a minimally invasive alternative method to profile metastatic PCa, with the added capability of detecting variants from multiple metastatic lesions that may have undergone clonal evolution. As discussed above, nearly 11% of mCRPC patients had newly identified actionable alterations in BRCA1/2 or MMR genes by serial ctDNA testing [35].
While ctDNA-based assays are non-invasive, they come with certain limitations compared to tissue-based testing. False negative results can occur due to low levels of ctDNA in the patient’s blood [45]. Low PSA levels and low tumor burden, lymph node only disease, and normal LDH have been linked to a lack of detection of somatic alterations in cfDNA NGS studies [51, 52]. Clonal hematopoiesis of indeterminate potential (CHIP) can also interfere with ctDNA testing, potentially leading to false positive results. In addition, accurate determination of copy-number alterations from ctDNA has been shown to be difficult, especially in low tumor fraction settings [45].
Given these inherent challenges, it is crucial to minimize pre-analytic variability by using standardized protocols for blood collection, storage, and sample preparation for ctDNA-based NGS studies and timing the collection of a ctDNA sample with clear metastatic progression [46, 53].
Despite these limitations, in cases where detectable alterations are found in ctDNA, the concordance with tissue-based studies is high [42, 48, 51]. The largest ever study of ctDNA in prostate analyzed plasma from 3,334 patients with advanced mCRPC (including 1,674 from TRITON 2/3) [54]. The investigators’ goal was to assess concordance between ctDNA and tissue based comprehensive genomic profiling [54]. The TRITON cohorts included patients who had progressed on one prior androgen receptor signaling inhibitor (ARSI) therapy and those who had progressed on 1-2 lines of ARSIs followed by taxane chemotherapy.
Liquid biopsies were found to accurately recapitulate the genomic alterations detected in tissue biopsies with a high level of agreement, especially with regards to BRCA1/2 mutations. 94% of BRCA1/2 mutations and 90% of all BRCA1/2 variants detected by tissue genomic profiling were detected in ctDNA, including 100% of predicted germline variants [54].
ctDNA also identified more acquired resistance alterations than tissue. These included novel AR-activating alterations and subclonal BRCA1/2 secondary mutations and reversions not identified in tissue testing. ctDNA was also enriched for other therapy resistance alterations as well as possible clonal hematopoiesis mutations (e.g. in ATM and CHEK2). In a study by Wyatt and colleagues on the concordance of ctDNA with a time matched tissue-biopsy, 33% of somatic mutations were detected exclusively in liquid biopsy samples [48].
While the above studies do not necessarily correlate their results against clinical outcomes, given the high percentage of patients with detectable ctDNA and agreement found with the tissue-defined genomic landscape of mCRPC observed in the study, genomic profiling through plasma biopsy is a viable option to detect actionable mutations, notably BRCA1/2. Reflex to tissue genetic profiling is suggested if ctDNA is negative or uninformative for actionable variants. Providing the ctDNA fraction or concentration should in the future allow for greater interpretation of negative results given the low sensitivity of ctDNA to detect alterations, particularly copy losses, in low ctDNA concentration patients.
Discordance between tissue and ctDNA (where patients were observed positive for BRCA or ATM in tumor tissue, but negative in ctDNA) have been attributed to limitations in structural variant detection (e.g. homozygous deletions and large rearrangements) in ctDNA, which are more common events in BRCA2 mutant tumors [55]. Low ctDNA shedding can also lead to such discordance. Low predicted tumor fraction has been reported to be particularly striking for patients with homozygous deletions and large rearrangements detected in tissue only, highlighting the need for improved ctDNA assays [55].
Conversely, where discordance was observed between BRCA or ATM alterations identified by ctDNA but not seen in tumor tissue, this was predominantly due to low variant allele frequency if variants fall below the lower limit of detection. In a clinical environment, these patients with false negative ctDNA results could be overlooked for personalized treatment. Reflexive tissue testing should be performed if suspicion is high.
Clinicians should be mindful of factors that impact the concordance between ctDNA and tissue testing. For example, genomic profiling of recent specimens may be more valuable than sequencing archival, pre-systemic treatment of primary tumor tissue. Tissue samples collected a median of 758 days before plasma showed 75% positive agreement whereas samples collected within 30 days of ctDNA had a much higher positive agreement [54]. Additionally, ctDNA fraction is higher in patients with a greater disease burden, such as those who have progressed on more lines of therapy. Therefore, clinicians must view the results of genetic testing through the context of its collection and a patient’s individual disease state before making conclusions about treatment. An online calculator is also available to predict the chances of a positive ctDNA test and the ctDNA fraction (see ctDNA.org) [56]. This can be helpful given the clear prognostic value of ctDNA burden in men with mCRPC.
Additionally, the major advantage of easy repetitive sampling to monitor tumor evolution, coupled with the more comprehensive assessment of tumor mutational burden independent of inter-tumoral heterogeneity and the rapid technological advancements to increase sensitivity and depth of assessment, make ctDNA analysis a useful alternative.
Unfortunately, ctDNA has low sensitivity for deletions which can lead to false negative testing results for HRR alterations and an inability to test for AR splice variants that predict poor outcomes from ARSI therapy. To address these limitations, future work should consider the integration of phenotypic biomarkers, such as CTCs, exosomes, and other blood-based assays or through molecular imaging, which can provide clinically relevant information to guide treatment and improve outcomes. Prior work has suggested CTC specific discordant genetic alterations in men with mCRPC which are associated with outcomes [57, 58]. In addition, CTC transcriptomic signatures can provide additional measures of phenotypic drug resistance in mCRPC, including AR variants and neuroendocrine biology. In addition, cell-free RNA may offer a complementary path to tumor molecular profiling, with utility for identifying RNA aberrations [59].
Clinical trial evidence supporting use of ctDNA
Patients in the phase III trial TALAPRO-2 (first line combination of talazoparib plus enzalutamide in mCRPC) provided solid tumor tissue (either de novo or archival) or blood based samples, or both, which were prospectively assessed for HRR gene alterations. HRR status was informed by tumor tissue in 804/805 patients (99.9%), by both tumor tissue and ctDNA in 114/805 (14.2%) and by ctDNA only in 1 patient (0.1%). Plasma samples that had been collected at screening were then retrospectively tested using a ctDNA assay to perform an exploratory analysis of patients with prospectively unknown HRR status and to examine the concordance between tissue NGS and ctDNA testing results.
A recent post-hoc analysis of these results from TALAPRO-2 reported high concordance between the retrospectively assessed ctDNA samples and the prospectively assessed/collected tumor samples [60]. There was 95% agreement for the determination of HRR deficiency between both tests. Of the 739 patients with retrospective ctDNA test results, 28% were HRR deficient, 60% were non-HRR deficient, and the remainder were either unknown or uncollected.
Secondary analysis of PROpel (phase III trial of first line abiraterone plus olaparib in mCRPC patients) similarly concluded an 85% overall percentage agreement between matched tumor tissue and ctDNA testing and using aggregate retrospective testing results it was possible to maximize the number of patients with known HRR mutated status [61]. These result suggests that, if sufficient tumor DNA is present, both ctDNA testing and tissue testing are reliable methods to detect HRR mutations for guiding clinical decision making.
Clonal hematopoiesis of indeterminate potential (CHIP)
Recent large-scale sequencing studies have revealed that the acquisition of clonally restricted somatic mutations in cancer-associated genes in hematopoietic cells is not limited to individuals with malignancy [62, 63]. These mutations can be detected in people with normal blood counts and without any apparent malignancy. These mutations have been termed “clonal hematopoiesis of indeterminate potential” or “CHIP” to describe individuals with a malignancy associated somatic mutation in blood but without other diagnostic criteria for malignancy.
CHIP is a known confounder of circulating free DNA (cfDNA) testing in prostate cancer [64, 65]. CHIP is detected in approximately 20% of men with advanced prostate cancer and is known to increase with age, in men, and in smokers or in those treated with prior DNA damaging chemotherapy or radiation. Notably, around 10% of men have CHIP variants in DNA repair genes, which complicates analyses but can be excluded by paired whole-blood control sequencing [66]. cfDNA testing only tests plasma where the cfDNA derives from all extant cell sources in the patient, including PCa and CHIP, as a consequence of which plasma-only cfDNA testing cannot reliably distinguish variants derived from prostate cancer versus a CHIP. To determine whether a patient has CHIP requires clonal NGS testing of peripheral blood cells. In this case, circulating tumor cells may be present in peripheral blood and, if so, can be used as a proxy for PCa tissue testing.
Most CHIP related genes are distinct from PCa associated genes, with the notable exception of ATM [67, 68]. ATM has been described as a frequent CHIP clone in clinical cancer predisposition testing, along with CHEK2 and TP53 [66, 69]. A recent, albeit small, study simultaneously analyzed plasma and paired whole-blood control samples in 69 patients with advanced PCa (defined as patients with metastatic disease or rising PSA following localized therapy) [66]. CHIP interference was defined as a pathogenic variant with variant allele fractions of at least 2% in both whole blood and plasma. 13 of 69 patients (19%; 95% CI 10–30%) were found to have CHIP interference clones, and 7 of those 13 had CHIP variants in DNA repair genes that are used in PARP selection. The majority were involving ATM (5) followed by BRCA2 (1) and CHEK1 (1). Only 1 of 12 TP53 variations detected in plasma cell-free DNA from 69 men with advanced PCa was found to be a CHIP interference somatic mutation.
Thus, nearly a quarter of all non-BRCA2 HRR mutations in this study were CHIP, and thus not predicted to be sensitive to PARP inhibitor monotherapy. The remaining patients had CHIP interference in other genes that are known to be frequently impacted by CHIPs. Interestingly, CHIP interference correlated exponentially with increasing age and was highest in those ages 81–90 (71%). The rate of CHIP similarly increased if patients had prior chemotherapy exposure. In this study, 10% of patients would have been misdiagnosed and incorrectly deemed eligible for PARP inhibitor therapy. To mitigate these risks, cfDNA results can be compared to results of whole blood control or tumor tissue.
Clinicians should be careful to not reflexively assume certain mutations identified in cfDNA, notably ATM mutations, are actionable tumor-derived mutations. Where possible, we recommend that a patient found to have an ATM mutation in cfDNA should be referred for CHIP testing via whole blood or validation through genetic testing on tissue. Ideally, cfDNA testing in prostate cancer could include whole blood controls to distinguish between CHIPs and prostate cancer variants. ctDNA results should also be correlated against the clinical trial results above to ensure PARP inhibitors are chosen in patients that will most benefit (notably BRCA2 patients). Furthermore, we encourage physicians to consult with specialized academic groups should questions arise.
Passenger mutations
HRR deficiency and microsatellite instability-H (MSI-H) alterations were historically thought to be mutually exclusive [70]. However, it has been found that 12.8% of BRCA1 and 3.4% of BRCA2 loss of function mutations co-occur in patients that are MSI-H [70]. In these BRCA-associated malignancies, the co-occurring BRCA mutations were generally monoallelic and not associated with genome-wide loss of heterozygosity for DNA damage repair function. This suggested that these BRCA1/2 alterations were “passenger events” and pure bystanders that are not actionable for PARP inhibition. In fact, two patients with PCa and co-occurring BRCA mutations and MSI-H showed resistance to PARP inhibition but were sensitive to subsequent anti-PD-1 therapy.
A recent report [71] of 18 men with high TMBs and concurrent HRR alterations demonstrated that only 33% of these “HRR altered tumors” had a COSMIC signature 3-positive/integrated assessment of HRR deficiency-positive (CSig3(+)/iHRD(+)) signature which verified them as HRR-deficient. In the other 2/3 of patients, the signature was absent, meaning HRR alterations were simply bystander events. Therefore, one must exercise caution in reflexively interpreting HRR mutations as actionable in mCRPC patients who also have high TMBs, as they may simply be “passenger events” not responsive to PARP inhibitor monotherapy. Interestingly, this phenomenon of a “passenger event” increased with TMB. Alternative HRD assays such as RNA signatures are in development to more fully identify additional PARP sensitive or resistant mCRPC patients.
Disparities and insurance implications
PCa mortality rates in black patients are approximately 2-4x higher than all other groups [1]. Despite this dramatic disparity in incidence and mortality, black patients have been the least represented in studies of PCa molecular drivers [72]. Such challenges are compounded by numerous barriers to genetic testing. There is significant potential for worsening health disparities among racial and ethnic minorities, as well as patients who reside in remote/rural areas.
Black or African American, Hispanic, and Asian/Pacific Islander patients with PCa are under-represented in germline testing studies, and thus a gap persists in genomic data in these patient populations, which may contribute to higher rates of VUS observed in these populations as compared to white patients [73]. In one study of patient data sequenced within The Cancer Genome Atlas (TCGA), there was insufficient sample data available to identify mutations with a 5% or 10% frequency in any self-reported race or ethnicity aside from white among PCa samples [74]. However, while pathogenic BRCA mutations do not differ by race, non-BRCA HRR mutations may differ by race/ancestry, such as in CHEK2 mutations in men of Ashkenazi Jewish ancestry, and MSI high disease may be more common in African American patients (9 vs. 4% in one study) [75]. In a second study pathogenic/likely pathogenic variants did not vary by race [76]. Further study is needed to elucidate diverse molecular alterations in PCa and their respective pathogenic potentials.
We note that in many countries, HRD testing takes place as the medical oncologist considers HRD therapeutic targeting. We agree with this approach as we only recommend somatic/tumor testing of patients with metastatic disease who may benefit from PARP inhibition or ARSI combined with PARP inhibition or programmed death-1 (PD-1) blockade. Germline testing is universally recommended given the impact on family members and risk of reducing future procedures as well as implications for screening.
Barriers to genetic testing
Barriers to performing germline testing exist, especially among racial minorities and rural patients. Systemic barriers include limited access to counseling, insurance coverage or educational resources and insufficient clinical capacity [74]. Patient barriers included poor understanding of testing rationale and testing cost [77].
A retrospective analysis of 14,610 PCa patients found that receipt of genetic counseling was the strongest predictor for receipt of genetic testing [78]. Genetic counselors are trained to gather family histories and provide pre and post-test counseling. However there is limited access to genetic counseling resources, especially in remote areas. Providers not formally trained in counseling are then forced to order tests and counsel, leading to disparate testing patterns.
Unfortunately Medicare does not currently recognize genetic counselors as healthcare providers, and Medicaid does not cover genetic counseling in all states. Thus, while the testing is covered by Medicare/Medicaid, providers not trained in such counseling are forced to provide guidance. Since a huge portion of PCa patients have Medicare/Medicaid, it is critical that providers are given genetic testing training/resources such as the PCCTC recommendations [79].
Patient mistrust of genetic testing is fed by concern over being deprived insurance coverage or employment. Providers can anticipate these concerns and assuage patient fears. The 2008 Genetic Information Nondiscrimination Act (GINA) provide legal protections, assurances and safeguards against the misuse of genetic information to patients. Title I of GINA prohibits healthcare coverage discrimination using genetic information; Title II similarly prohibits employment discrimination. Importantly, GINA prohibits health insurers from determining cost, coverage, policy eligibility, or benefits based on genetic information/history.
Many patients need to be educated of GINA’s legal protections [80]. However, presently no requirement exists for providers to educate about these protections. Such counseling may assuage patient fears about testing.
Unfortunately GINA does not protect life insurance eligibility or cost. As a result, this remains a barrier for many patients who may be financially dependent on a family member’s life insurance, leading many patients to still decline genetic testing [80].
The cost of genomic testing varies significantly depending on the testing ordered, the patient’s insurance coverage, and whether a patient is eligible for financial assistance. This underscores the importance of establishing processes to overcome cost barriers and reduce out-of-pocket costs for patients without insurance.
Conclusions
Genetic and biomarker testing have revolutionized mCRPC, bringing precision medicine into PCa. However, there are many dimensions to genetic testing. Furthermore, multiple barriers exist to the utilization and implementation of genetic testing. We recommend germline testing for all patients with PCa after informed decision making by practitioners (Fig. 1). We also recommend somatic tumor and/or ctDNA testing once a diagnosis of distant metastatic disease is made to have such critical, actionable information available for subsequent treatment planning. Such testing could be considered for patients with regional nodal metastatic disease. Testing implications relevant to either the appropriate mCRPC or mHSPC setting will better inform treatment decisions. In addition, repeat ctDNA testing may provide additional informative results in the mCRPC setting to detect novel actionable BRCA or MSI-high disease, especially if initial HSPC tissue testing is not evaluable, available, or uninformative. Improved testing methodology and understanding of therapeutic implications coupled with continued decrease in testing barriers will advance precision medicine in PCa.
References
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA: A Cancer J Clinicians. 2023;73:17–48.
Desai MM, Cacciamani GE, Gill K, Zhang J, Liu L, Abreu A, et al. Trends in Incidence of Metastatic Prostate Cancer in the US. JAMA Netw Open. 2022;5:e222246.
Weiner AB, Matulewicz RS, Eggener SE, Schaeffer EM. Increasing incidence of metastatic prostate cancer in the United States (2004–2013). Prostate Cancer Prostatic Dis. 2016;19:395–7.
Hamid AA, Sayegh N, Tombal B, Hussain M, Sweeney CJ, Graff JN, et al. Metastatic Hormone-Sensitive Prostate Cancer: Toward an Era of Adaptive and Personalized Treatment. Am Soc Clin Oncol Educ Book. 2023;43:e390166.
Ryan CJ, Smith MR, Fizazi K, Saad F, Mulders PF, Sternberg CN, et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2015;16:152–60.
Beer TM, Armstrong AJ, Rathkopf D, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in Men with Chemotherapy-naïve Metastatic Castration-resistant Prostate Cancer: Extended Analysis of the Phase 3 PREVAIL Study. Eur Urol. 2017;71:151–4.
Francini E, Gray KP, Shaw GK, Evan CP, Hamid AA, Perry CE, et al. Impact of new systemic therapies on overall survival of patients with metastatic castration-resistant prostate cancer in a hospital-based registry. Prostate Cancer Prostatic Dis. 2019;22:420–7.
Shore ND, Laliberté F, Ionescu-Ittu R, Yang L, Mahendran M, Lejeune D, et al. Real-World Treatment Patterns and Overall Survival of Patients with Metastatic Castration-Resistant Prostate Cancer in the US Prior to PARP Inhibitors. Adv Ther. 2021;38:4520–40.
Freedland SJ, Davis M, Epstein AJ, Arondekar B, Ivanova JI. Real-world treatment patterns and overall survival among men with Metastatic Castration-Resistant Prostate Cancer (mCRPC) in the US Medicare population. Prostate Cancer Prostatic Dis. 2024;27:327–33.
Halabi S, Yang Q, Roy A, Luo B, Araujo JC, Logothetis C, et al. External Validation of a Prognostic Model of Overall Survival in Men With Chemotherapy-Naïve Metastatic Castration-Resistant Prostate Cancer. J Clin Oncol. 2023;41:2736–46.
Armstrong AJ, Lin P, Tombal B, Saad F, Higano CS, Joshua AM, et al. Five-year Survival Prediction and Safety Outcomes with Enzalutamide in Men with Chemotherapy-naïve Metastatic Castration-resistant Prostate Cancer from the PREVAIL Trial. Eur Urol. 2020;78:347–57.
Hussain M, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. Survival with Olaparib in Metastatic Castration-Resistant Prostate Cancer. N. Engl J Med. 2020;383:2345–57.
de Bono J, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. Olaparib for Metastatic Castration-Resistant Prostate Cancer. N. Engl J Med. 2020;382:2091–102.
Agarwal N, Azad A, Carles J, Fay AP, Matsubara N, Heinrich D, et al. TALAPRO-2: Phase 3 study of talazoparib (TALA) + enzalutamide (ENZA) versus placebo (PBO) + ENZA as first-line (1L) treatment in patients (pts) with metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol. 2023;41:LBA17–LBA.
Clarke N, Wiechno P, Alekseev B, Sala N, Jones R, Kocak I, et al. Olaparib combined with abiraterone in patients with metastatic castration-resistant prostate cancer: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2018;19:975–86.
Chi KN, Sandhu S, Smith MR, Attard G, Saad M, Olmos D, et al. Niraparib plus abiraterone acetate with prednisone in patients with metastatic castration-resistant prostate cancer and homologous recombination repair gene alterations: second interim analysis of the randomized phase III MAGNITUDE trial. Ann Oncol. 2023;34:772–82.
Tsai AK, Kagalwalla S, Langer J, Le-Kumar T, Le-Kumar V, Antonarakis ES. Pembrolizumab for metastatic castration-resistant prostate cancer: trials and tribulations. Expert Opin Biol Ther. 2024;24:51–62.
Hage Chehade C, Jo Y, Gebrael G, Tripathi N, Sayegh N, Chigarira B, et al. Trends and Disparities in Next-Generation Sequencing in Metastatic Prostate and Urothelial Cancers. JAMA Netw Open. 2024;7:e2423186.
Robinson D, Van Allen EM, Wu YM, Schultz N, Lonigro RJ, Mosquera JM, et al. Integrative clinical genomics of advanced prostate cancer. Cell. 2015;161:1215–28.
Mateo J, Boysen G, Barbieri CE, Bryant HE, Castro E, Nelson PS, et al. DNA Repair in Prostate Cancer: Biology and Clinical Implications. Eur Urol. 2017;71:417–25.
Castro E, Goh C, Olmos D, Saunders E, Leongamornlert D, Tymrakiewicz M, et al. Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J Clin Oncol. 2013;31:1748–57.
Lukashchuk N, Barnicle A, Adelman CA, Armenia J, Kang J, Barrett JC, et al. Impact of DNA damage repair alterations on prostate cancer progression and metastasis. Front Oncol. 2023;13:1162644.
Lai Z, Brosnan M, Sokol ES, Xie M, Dry JR, Harrington EA, et al. Landscape of homologous recombination deficiencies in solid tumours: analyses of two independent genomic datasets. BMC Cancer. 2022;22:13.
Sun JX, He Y, Sanford E, Montesion M, Frampton GM, Vignot S, et al. A computational approach to distinguish somatic vs. germline origin of genomic alterations from deep sequencing of cancer specimens without a matched normal. PLoS Comput Biol. 2018;14:e1005965.
Barata PC, Assayag J, Li B, Siu G, Niyazov A. Genetic Testing in Men With Metastatic Castration-Resistant Prostate Cancer. JAMA Oncol. 2024;10:975–7.
Lowrance W, Dreicer R, Jarrard DF, Scarpato KR, Kim SK, Kirkby E, et al. Updates to Advanced Prostate Cancer: AUA/SUO Guideline (2023). J Urol. 2023;209:1082–90.
Lowrance WT, Breau RH, Chou R, Chapin BF, Crispino T, Dreicer R, et al. Advanced Prostate Cancer: AUA/ASTRO/SUO Guideline PART I. J Urol. 2021;205:14–21.
Tung N, Ricker C, Messersmith H, Balmaña J, Domchek S, Stoffel EM, et al. Selection of Germline Genetic Testing Panels in Patients With Cancer: ASCO Guideline. J Clin Oncol. 2024;42:2599–2615.
Cheng HH, Sokolova AO, Gulati R, Bowen D, Knerr SA, Klemfuss N, et al. Internet-Based Germline Genetic Testing for Men With Metastatic Prostate Cancer. JCO Precis Oncol. 2023;7:e2200104.
Russo J, McDougall C, Bowler N, Shimada A, Gross L, Hyatt C, et al. Pretest Genetic Education Video Versus Genetic Counseling for Men Considering Prostate Cancer Germline Testing: A Patient-Choice Study to Address Urgent Practice Needs. JCO Precis Oncol. 2021;5:1377–86.
Loeb S, Keith SW, Cheng HH, Leader AE, Gross L, Sanchez Nolasco T, et al. TARGET: A Randomized, Noninferiority Trial of a Pretest, Patient-Driven Genetic Education Webtool Versus Genetic Counseling for Prostate Cancer Germline Testing. JCO Precis Oncol. 2024;8:e2300552.
Esplin ED, Nielsen SM, Bristow SL, Garber JE, Hampel H, Rana HQ, et al. Universal Germline Genetic Testing for Hereditary Cancer Syndromes in Patients With Solid Tumor Cancer. JCO Precis Oncol. 2022;6:e2100516.
Shore N, Gazi M, Pieczonka C, Heron S, Modh R, Cahn D, et al. Efficacy of National Comprehensive Cancer Network Guidelines in Identifying Pathogenic Germline Variants Among Unselected Patients with Prostate Cancer: The PROCLAIM Trial. Eur Urol Oncol. 2023;6:477–83.
Paller CJ, Barata PC, Lorentz J, Appleman LJ, Armstrong AJ, DeMarco TA, et al. PROMISE Registry: A prostate cancer registry of outcomes and germline mutations for improved survival and treatment effectiveness. Prostate. 2024;84:292–302.
Park JJ, Chu A, Li J, Ali A, McKay RR, Hwang C, et al. Repeat Next-Generation Sequencing Testing on Progression in Men With Metastatic Prostate Cancer Can Identify New Actionable Alterations. JCO Precis Oncol. 2024;8:e2300567.
Green MF, Watson CH, Tait S, He J, Pavlick DC, Frampton G, et al. Concordance Between Genomic Alterations Detected by Tumor and Germline Sequencing: Results from a Tertiary Care Academic Center Molecular Tumor Board. Oncologist. 2023;28:33–9.
Berchuck JE, Boiarsky D, Silver R, Sunkara R, McClure HM, Tsai HK, et al. Addition of Germline Testing to Tumor-Only Sequencing Improves Detection of Pathogenic Germline Variants in Men With Advanced Prostate Cancer. JCO Precis Oncol. 2022;6:e2200329.
Schweizer MT, Sivakumar S, Tukachinsky H, Coleman I, De Sarkar N, Yu EY, et al. Concordance of DNA Repair Gene Mutations in Paired Primary Prostate Cancer Samples and Metastatic Tissue or Cell-Free DNA. JAMA Oncol. 2021;7:1–5.
Mateo J, Seed G, Bertan C, Rescigno P, Dolling D, Figueiredo I, et al. Genomics of lethal prostate cancer at diagnosis and castration resistance. J Clin Invest. 2020;130:1743–51.
Araujo LH, Timmers C, Shilo K, Zhao W, Zhang J, Yu L, et al. Impact of Pre-Analytical Variables on Cancer Targeted Gene Sequencing Efficiency. PLoS One. 2015;10:e0143092.
Ascierto PA, Bifulco C, Palmieri G, Peters S, Sidiropoulos N. Preanalytic Variables and Tissue Stewardship for Reliable Next-Generation Sequencing (NGS) Clinical Analysis. J Mol Diagn. 2019;21:756–67.
Mandel P, Hoeh B, Humke C, Doering C, Wenzel M, Cano Garcia C, et al. Feasibility of Next-generation Sequencing of Liquid Biopsy (Circulating Tumor DNA) Samples and Tumor Tissue from Patients with Metastatic Prostate Cancer in a Real-world Clinical Setting in Germany. Eur Urol Focus. 2024;10:339–45.
Hussain M, Corcoran C, Sibilla C, Fizazi K, Saad F, Shore N, et al. Tumor Genomic Testing for >4000 Men with Metastatic Castration-resistant Prostate Cancer in the Phase III Trial PROfound (Olaparib). Clin Cancer Res. 2022;28:1518–30.
Choi SE, Hong SW, Yoon SO. Proposal of an appropriate decalcification method of bone marrow biopsy specimens in the era of expanding genetic molecular study. J Pathol Transl Med. 2015;49:236–42.
Bayle A, Peyraud F, Belcaid L, Brunet M, Aldea M, Clodion R, et al. Liquid versus tissue biopsy for detecting actionable alterations according to the ESMO Scale for Clinical Actionability of molecular Targets in patients with advanced cancer: a study from the French National Center for Precision Medicine (PRISM). Ann Oncol. 2022;33:1328–31.
Trujillo B, Wu A, Wetterskog D, Attard G. Blood-based liquid biopsies for prostate cancer: clinical opportunities and challenges. Br J Cancer. 2022;127:1394–402.
Taavitsainen S, Annala M, Ledet E, Beja K, Miller PJ, Moses M, et al. Evaluation of Commercial Circulating Tumor DNA Test in Metastatic Prostate Cancer. JCO Precis Oncol. 2019;3:PO.19.00014.
Wyatt AW, Annala M, Aggarwal R, Beja K, Feng F, Youngren J, et al. Concordance of Circulating Tumor DNA and Matched Metastatic Tissue Biopsy in Prostate Cancer. J Natl Cancer Inst. 2017;109:djx118.
Wong SK, Mohamad NV, Giaze TR, Chin KY, Mohamed N, Ima-Nirwana S. Prostate Cancer and Bone Metastases: The Underlying Mechanisms. Int J Mol Sci. 2019;20:2587.
Gandaglia G, Abdollah F, Schiffmann J, Trudeau V, Shariat SF, Kim SP, et al. Distribution of metastatic sites in patients with prostate cancer: A population-based analysis. Prostate. 2014;74:210–6.
Schweizer MT, Gulati R, Beightol M, Konnick EQ, Cheng HH, Klemfuss N, et al. Clinical determinants for successful circulating tumor DNA analysis in prostate cancer. Prostate. 2019;79:701–8.
Herberts C, Wyatt AW. Technical and biological constraints on ctDNA-based genotyping. Trends Cancer. 2021;7:995–1009.
Batool SM, Hsia T, Beecroft A, Lewis B, Ekanayake E, Rosenfeld Y, et al. Extrinsic and intrinsic preanalytical variables affecting liquid biopsy in cancer. Cell Rep. Med. 2023;4:101196.
Tukachinsky H, Madison RW, Chung JH, Gjoerup OV, Severson EA, Dennis L, et al. Genomic Analysis of Circulating Tumor DNA in 3,334 Patients with Advanced Prostate Cancer Identifies Targetable BRCA Alterations and AR Resistance Mechanisms. Clin Cancer Res. 2021;27:3094–105.
Chi KN, Barnicle A, Sibilla C, Lai Z, Corcoran C, Barrett JC, et al. Detection of BRCA1, BRCA2, and ATM Alterations in Matched Tumor Tissue and Circulating Tumor DNA in Patients with Prostate Cancer Screened in PROfound. Clin Cancer Res. 2023;29:81–91.
Fonseca NM, Maurice-Dror C, Herberts C, Tu W, Fan W, Murtha AJ, et al. Prediction of plasma ctDNA fraction and prognostic implications of liquid biopsy in advanced prostate cancer. Nat Commun. 2024;15:1828.
Gupta S, Halabi S, Kemeny G, Anand M, Giannakakou P, Nanus DM, et al. Circulating Tumor Cell Genomic Evolution and Hormone Therapy Outcomes in Men with Metastatic Castration-Resistant Prostate Cancer. Mol Cancer Res. 2021;19:1040–50.
Gupta S, Hovelson DH, Kemeny G, Halabi S, Foo WC, Anand M, et al. Discordant and heterogeneous clinically relevant genomic alterations in circulating tumor cells vs plasma DNA from men with metastatic castration resistant prostate cancer. Genes Chromosomes Cancer. 2020;59:225–39.
Fettke H, Kwan EM, Docanto MM, Bukczynska P, Ng N, Graham LK, et al. Combined Cell-free DNA and RNA Profiling of the Androgen Receptor: Clinical Utility of a Novel Multianalyte Liquid Biopsy Assay for Metastatic Prostate Cancer. Eur Urol. 2020;78:173–80.
Azad A, Fizazi K, Matsubara N, Fong PCC, Carles J, Shore ND, et al. Use of circulating tumor DNA (ctDNA) to complement tumor tissue homologous recombination repair (HRR) gene alteration testing in TALAPRO-2, a phase 3 study of talazoparib (TALA) + enzalutamide (ENZA) versus placebo (PBO) + ENZA as first-line (1L) treatment in patients (pts) with metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol. 2023;41:5056.
Armstrong AJ, Saad F, Thiery-Vuillemin A, Oya M, Shore ND, Mehra N, et al. 1370P Detection of mutations in homologous recombination repair (HRR) genes in tumour tissue (TT) and circulating tumour DNA (ctDNA) from patients (pts) with metastatic castrate-resistant prostate cancer (mCRPC) in the phase III PROpel trial. Ann Oncol. 2022;33:S1168.
Shlush LI, Zandi S, Mitchell A, Chen WC, Brandwein JM, Gupta V, et al. Identification of pre-leukaemic haematopoietic stem cells in acute leukaemia. Nature. 2014;506:328–33.
Busque L, Patel JP, Figueroa ME, Vasanthakumar A, Provost S, Hamilou Z, et al. Recurrent somatic TET2 mutations in normal elderly individuals with clonal hematopoiesis. Nat Genet. 2012;44:1179–81.
Weitzel JN, Chao EC, Nehoray B, Van Tongeren LR, LaDuca H, Blazer KR, et al. Somatic TP53 variants frequently confound germ-line testing results. Genet Med. 2018;20:809–16.
Razavi P, Li BT, Brown DN, Jung B, Hubbell E, Shen R, et al. High-intensity sequencing reveals the sources of plasma circulating cell-free DNA variants. Nat Med. 2019;25:1928–37.
Jensen K, Konnick EQ, Schweizer MT, Sokolova AO, Grivas P, Cheng HH, et al. Association of Clonal Hematopoiesis in DNA Repair Genes With Prostate Cancer Plasma Cell-free DNA Testing Interference. JAMA Oncol. 2021;7:107–10.
Steensma DP. Clinical consequences of clonal hematopoiesis of indeterminate potential. Blood Adv. 2018;2:3404–10.
Steensma DP, Bejar R, Jaiswal S, Lindsley RC, Sekeres MA, Hasserjian RP, et al. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. 2015;126:9–16.
Mateo J, Carreira S, Sandhu S, Miranda S, Mossop H, Perez-Lopez R, et al. DNA-Repair Defects and Olaparib in Metastatic Prostate Cancer. N. Engl J Med. 2015;373:1697–708.
Sokol ES, Jin DX, Fine A, Trabucco SE, Maund S, Frampton G, et al. PARP Inhibitor Insensitivity to BRCA1/2 Monoallelic Mutations in Microsatellite Instability-High Cancers. JCO Precis Oncol. 2022;6:e2100531.
Bhatlapenumarthi V, De Sarkar N, Patwari A, Antonarakis ES, Nelson AA, Kilari D. Homologous recombination repair (HRR) alterations may be passenger events in patients with advanced prostate cancer (PC) with high tumor mutational burden (hTMB). J Clin Oncol. 2024;42:206.
Mahal BA, Gerke T, Awasthi S, Soule HR, Simons JW, Miyahira A, et al. Prostate Cancer Racial Disparities: A Systematic Review by the Prostate Cancer Foundation Panel. Eur Urol Oncol. 2022;5:18–29.
Kwon DH, Borno HT, Cheng HH, Zhou AY, Small EJ. Ethnic disparities among men with prostate cancer undergoing germline testing. Urol Oncol. 2020;38:80.e1–e7.
Paller CJ, Antonarakis ES, Beer TM, Borno HT, Carlo MI, George DJ, et al. Germline Genetic Testing in Advanced Prostate Cancer; Practices and Barriers: Survey Results from the Germline Genetics Working Group of the Prostate Cancer Clinical Trials Consortium. Clin Genitourin Cancer. 2019;17:275–82.e1.
Hwang C, Henderson NC, Chu S-C, Holland B, Cackowski FC, Pilling A, et al. Biomarker-Directed Therapy in Black and White Men With Metastatic Castration-Resistant Prostate Cancer. JAMA Netw Open. 2023;6:e2334208.
Ledet EM, Burgess EF, Sokolova AO, Jaeger EB, Hatton W, Moses M, et al. Comparison of germline mutations in African American and Caucasian men with metastatic prostate cancer. Prostate. 2021;81:433–9.
Weise N, Shaya J, Javier-Desloges J, Cheng HH, Madlensky L, McKay RR. Disparities in germline testing among racial minorities with prostate cancer. Prostate Cancer Prostatic Dis. 2022;25:403–10.
Borno HT, Odisho AY, Gunn CM, Pankowska M, Rider JR. Disparities in precision medicine-Examining germline genetic counseling and testing patterns among men with prostate cancer. Urol Oncol. 2021;39:233.e9–e14.
Szymaniak BM, Facchini LA, Giri VN, Antonarakis ES, Beer TM, Carlo MI, et al. Practical Considerations and Challenges for Germline Genetic Testing in Patients With Prostate Cancer: Recommendations From the Germline Genetics Working Group of the PCCTC. JCO Oncol Pr. 2020;16:811–9.
Lenartz A, Scherer AM, Uhlmann WR, Suter SM, Anderson Hartley C, Prince AER. The persistent lack of knowledge and misunderstanding of the Genetic Information Nondiscrimination Act (GINA) more than a decade after passage. Genet Med. 2021;23:2324–34.
Acknowledgements
The advisory board and meeting that formed the basis for this paper was convened and funded by Pfizer, Inc. The contents were developed and are the opinions solely of the authors listed.
Author information
Authors and Affiliations
Contributions
AA: Conception, manuscript writing, preparation, editing, final production. AT: Manuscript writing, manuscript editing. MCH: Manuscript editing. WA: Manuscript editing. AHB: Manuscript editing. LIK: Manuscript editing. STT: Manuscript editing. PT: Manuscript editing. AVS: Conception, manuscript writing, preparation, editing, final production. JML: Conception, manuscript writing, preparation, editing, final production.
Corresponding author
Ethics declarations
Competing interests
There are no competing financial interests in relation to the work described. Below is a list of the authors total disclosures, none of which compete with this manuscript. AJA: Research support (to Duke) from the NIH/NCI, PCF/Movember, DOD, Astellas, Pfizer, Bayer, Janssen, Dendreon, BMS, AstraZeneca, Merck, Forma, Celgene, Amgen, Novartis. Consulting or advising relationships with Astellas, Pfizer, Bayer, Janssen, BMS, AstraZeneca, Merck, Forma, Celgene, Myovant, Exelixis, GoodRx, Novartis, Medscape, MJH, Z Alpha, Telix. AT: Reports no relevant disclosures. MCH: MCH served as a paid consultant/received honoraria from Pfizer and has received research funding from Merck, Novartis, Genentech, Promicell and Bristol Myers Squibb. WA: WA is partially funded by NIH/NCI Cancer Center Support Grant P30-CA008748 and the Prostate Cancer Foundation. WA received speaking honoraria from Roche, Pfizer, Medscape, Aptitude Health, Clinical Education Alliance, touchIME and Onclive/MJH Life Sciences, consulting fees from Clovis Oncology, Janssen, ORIC Pharmaceuticals, Daiichi Sankyo, MOMA Therapeutics, Laekna Therapeutics and AstraZeneca, and Research Funding (to his institution) from AstraZeneca, Zenith Epigenetics, Clovis Oncology, ORIC Pharmaceuticals, Epizyme/Ipsen, Transthera, Merus, and Nuvation Bio. AHB: Advisory boards or travel support from Merck, Bayer, Pfizer, Astellas, Johnson and Johnson, Lantheus, Astra Zeneca, Novartis, Moma Therapeutics. Past research support (to Mayo Clinic) Johnson and Johnson. LIK: LIK owns stock in Swan Valley Medical, has received honoraria from Astellas, AstraZeneca, Abbvie, Bayer, Dendreon, Janssen, Merck, Myovant, Pfizer, and Sanofi, has received financial compensation as a paid consultant/advisor to Astellas, Astra-Zeneca, Abbvie, Bayer, Bristol Myers Squibb, Bayer, enGene, Ferring, Dendreon, Janssen, Merck, Myovant, Pfizer, and Sanofi, and has received financial compensation to participate in speakers bureaus for Astellas, Astra-Zeneca, Bayer, Dendreon, Janssen, Merck, Myovant, and Pfizer. He has received institutional funding from Janssen Bayer, Bristol Myers Squibb, Dendreon,E pizyme, Astellas, Pfizer, AstraZeneca, Merck, Myovant, BioExcel, Vaxiion, KDx, ImmunisAI/Oncocell,. FKD, Nucleix and Cleveland Diagnostics. STT: Research funding (to institution): Sanofi, Medivation, Astellas, Janssen, Amgen, Progenics, Dendreon, Lilly, Genentech, Newlink, BMS, Inovio, AstraZeneca, Immunomedics, Aveo, Rexahn, Atlab, Boehringer Ingelheim, Millennium, Bayer, Merck, Abbvie, Karyopharm, Endocyte, Clovis, Seattle Genetics, Novartis, Gilead, POINT Biopharma, Ambrx, Clarity. Honoraria for consulting: Sanofi, Medivation, Astellas, Dendreon, Janssen, Genentech, Bayer, Endocyte, Eisai, Immunomedics, Karyopharm, Abbvie, Tolmar, Seattle Genetics, Amgen, Clovis, QED, Pfizer, AAA/Novartis, Clarity, Genomic Health, POINT Biopharma, Blue Earth, AIkido Pharma, Gilead, Telix Pharma, Convergent Therapeutics, EMD Serono, Myovant, Merck, Daiichi Sankyo, TransThera, Regeneron, Ambrx, Boston Scientific. PT: Consulting and Speaker Bureaus: Astellas, Pfizer, Astra Zeneca, Janssen, Bayer, BMS, Merck, Aveo. AVS: 2023 ASCO Young Investigator Award. JML: Consulting for Pfizer, Janssen, Macrogenics, Foundation Medicine, Gilead, Arvinas, Astellas, Cytogen, Seattle Genetics.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Armstrong, A.J., Taylor, A., Haffner, M.C. et al. Germline and somatic testing for homologous repair deficiency in patients with prostate cancer (part 1 of 2). Prostate Cancer Prostatic Dis (2024). https://doi.org/10.1038/s41391-024-00901-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-024-00901-4
This article is cited by
-
A Podcast on Integrating Genetic Testing for Homologous Recombination Repair Gene Alterations in Patients with Prostate Cancer in the USA: a Multidisciplinary Approach to Overcoming the Obstacles
Targeted Oncology (2025)
-
Overcoming barriers to prostate cancer genetic testing: who, when, and how
Prostate Cancer and Prostatic Diseases (2024)



