Abstract
A disturbed sense of identity is one of the major features of borderline personality disorder (BPD), which manifests early in the course of the disorder, and is potentially examinable using functional imaging during tasks involving self-reflection. Twenty-seven medication-naïve adolescent female patients with BPD, who had no psychiatric comorbidities, and 28 matched healthy female controls underwent fMRI while answering questions either about themselves or acquaintances. Control conditions consisted of answering questions involving factual knowledge and a low-level baseline (cross fixation). When self-reflection was compared to fact processing, BPD patients exhibited reduced activation in the right dorsolateral prefrontal cortex (DLPFC), as well as in the left parietal and calcarine cortex and the right precuneus. In contrast, other-reflection was associated with relatively lower activation in the medial frontal cortex in BPD patients, with further analysis revealing that this change reflected a failure of de-activation during the fact processing condition. There were no differences between the BPD patients and controls when self- and other-processing was examined against low-level baseline. This study provides evidence of reduced DLPFC activation during self-reflection in adolescent females with BPD, which may reflect diminished top-down cognitive control of this process, but not other-reflection in the disorder.
Similar content being viewed by others
Introduction
Borderline personality disorder (BPD), characterized by emotional dysregulation, impulsive behaviors, instability in interpersonal relationships, and a disturbed sense of self, has been estimated to affect up to 5.5% of the population and is often disabling [1]. Although it has traditionally been considered an adult disorder, there is increasing evidence to support that it can be reliably diagnosed in adolescence [2,3,4], something that is of potential importance for theories that propose that it has a basis in development and/or changes that take place in the transition from adolescence to adulthood (e.g. [5, 6]).
The importance of biological factors in BPD is widely recognized and these have been examined in genetic, structural imaging and functional imaging studies [7,8,9,10,11,12,13,14,15]. With respect to the last of these, the focus to date has been on the affective dysregulation that characterizes the disorder, and a range of activation changes have been identified as associated with this. Thus, a meta-analysis of 19 studies examining brain functional responses to negative emotional stimuli in BPD patients found reduced activation in the dorsolateral prefrontal cortex (DLPFC), the left lingual gyrus, and the left superior parietal gyrus bilaterally, and also increased activation in the posterior cingulate gyrus, the left middle temporal gyrus, and left amygdala and hippocampus [15].
Less investigated from the functional imaging point of view has been the disturbed sense of identity that characterizes BPD [1]; see also [16, 17], and which has been argued to be one of the predominant features of the disorder when it presents in adolescence (the other being affective instability) [18]. One potential way to investigate this is by examining brain activity during the processing of self-related information. In the healthy population this process, often referred to as self-reflection, is associated with activation in the medial frontal cortex, particularly rostrally; other regions activated include the posterior cingulate cortex and precuneus and the angular gyrus and the temporoparietal junction (TPJ) (meta-analyses [19,20,21]; see also [22]). Interestingly, processing of information about other people, eg their characteristics and attitudes (‘other-reflection’), activates essentially the same neural network [19,20,21]; see also [22], although with overlapping but discernibly different localizations in the medial frontal cortex according to one meta-analysis [19].
To date, only one functional imaging study has examined self-reflection in BPD. Scherpiet et al. [23] used fMRI to examine 19 adult female BPD patients and 19 healthy controls in two task conditions: cognitive self-reflection where they thought about themselves, specifically to reflect who they were and what were their goals, and a mindfulness-like self-awareness, where they were encouraged to be aware of their current emotions and bodily feelings; there was also a neutral condition where they simply waited for a picture to be shown. In the self-reflection compared to the mindfulness condition the patients showed increased activation compared to the controls in regions including the right dorsomedial prefrontal cortex (superior, medial, and middle frontal areas, as well as the anterior supplementary motor area). It should be noted, however, that the pattern was different when self-reflection was compared to the neutral task: the group comparison here revealed increased activation in the BPD patients in the right pre- and postcentral gyrus, plus in the supramarginal and right superior temporal gyrus (STG).
The aim of the present study was to examine brain functional changes during self– and other-reflection tasks in a sample of adolescent patients with BPD. Focusing on such a group has the potential to establish brain regions involved in the identity disturbance seen in the disorder early in its course, at a time that is relevant to current theoretical proposals about its development. Another advantage of studying adolescent patients is that this can potentially minimize confounding factors, such as drug treatment and later emerging comorbidity with Axis I disorders [24]. We compared activations during these tasks to a low-level baseline (a fixation cross) and also to an active control task commonly used in self-reflection studies, processing of impersonal factual information.
Methods
Participants
The initial clinical sample consisted of 37 treatment-naïve female adolescent patients with a DSM-5 diagnosis of BPD. Patients were recruited from two outpatient mental health services in Barcelona with expertise in BPD in adolescents and young adults, (Vall d’Hebron University Hospital and the Orienta Foundation). Exclusion criteria included left-handedness, age below 12 or above 18 years, alcohol or substance abuse or dependence (excluding nicotine) in the last year, head trauma with loss of consciousness, and general exclusion criteria for MRI such as the presence of metals within the body. We also excluded patients with any comorbid psychiatric disorder according to DSM-5 diagnostic criteria. Drug-naïvety at the time of examination was confirmed by questioning.
The diagnosis of BPD was based on the Spanish version of the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) [25]. The Spanish version of Schedule for Affective Disorders and Schizophrenia for School Age Children-Present and Lifetime version [26] was used to assess psychiatric disorders other than BPD in patients and controls under 16 years old. The Spanish version of the Structured Clinical Interview for DSM-IV Axis I Disorders [27] was used to assess psychiatric disorders other than BPD in those who were between 16 and 18 years old.
Healthy controls (HC) were selected from an initial sample of 40 female adolescents recruited from the community on the basis that they were similar to the patients in age and estimated IQ, as assessed using the Word Accentuation Test (Test de Acentuación de Palabras, TAP [28]). Exclusion criteria were the same as for the patients. HC were also excluded if they reported having a first-degree relative with a psychiatric diagnosis.
All participants gave written informed consent prior to participation in accordance to the Declaration of Helsinki. This was obtained from participants aged 18 years and from parents/legal guardians for participants aged under 18. All the study procedures had been previously approved by the Clinical Research Ethics Committee of Vall d’Hebron University Hospital [PR(AG)353/2015] and the Clinical Research Ethics Committee of Germanes Hospitalàries [PI15/02025].
Self-other fMRI task
Participants performed a self- and other-reflection task previously used by our group [22]. Before scanning, participants were asked to choose an acquaintance to think about inside the scanner. The participant had to be familiar with chosen individual, but not close emotionally, in order to avoid eliciting strong feelings towards them (examples suggested/chosen included a classmate, a neighbour or a distant relative). During the task, participants viewed a series of statements about themselves (‘self” condition), the acquaintance (‘other’ condition), or concerning general knowledge (‘facts’, the control condition). They had to respond with a button press indicating whether they considered the sentence to be true or false. Stimuli were presented on VisualSystem goggles mounted on the head coil, and responses were made and registered with the MRI-compatible response device Response-grip (NordicNeuroLab).
The task consisted of 54 trials (18 per condition) arranged in a block design. Each block started with an instruction screen indicating the condition that corresponded to the block (‘Sentences about me’, ‘Sentences about [Name of the other person]’, ‘Sentences about facts’), which lasted 3 s. After a 1 s delay, three trials were presented, each lasting 9 s, where the sentence appeared in the centre of the screen and the options “Yes” and “No” appeared at the bottom-right and bottom-left corners, respectively, to act as a reminder of the required response (‘Yes’ with the right index finger, and ‘No’ with the left index finger). The trials were separated by a 1 s blank screen. After three trials, the next block started, with a total of 6 blocks per condition. Every 3 blocks there was a baseline period of 16 s in which a fixation cross was presented (‘low-level baseline’). Block order was pseudorandomized, with each of the three conditions occurring once between baseline periods.
Image acquisition
Images were acquired with a 3 T Philips Achieva scanner (Philips Medical Systems, Best, The Netherlands). Functional data were acquired using a T2*-weighted echo-planar imaging (EPI) sequence with the following acquisition parameters: TR = 2000 ms, TE = 30 ms, Flip angle = 78 O, in-plane resolution = 3 × 3 mm, FOV = 240 mm, slice thickness = 3 mm, inter-slice gap = 1 mm. Slices (32 per volume; 364 volumes) were acquired with an interleaved order parallel to the anterior-posterior commissure plane. The first 10 volumes were discarded to avoid T1 saturation effects. Before the functional sequence, a high-resolution anatomical 3D volume was acquired using a TFE (Turbo Field Echo) sequence for anatomical reference and inspection (TR = 8.15 ms; TE = 3.73 ms; flip angle = 8°; voxel-size = 0.9735 × 0.9735 mm; slice thickness = 1 mm; slice number = 160; FOV = 240 mm).
Image pre-processing and analysis
Pre-processing and analyses of the fMRI data were carried out with the FEAT module included in FSL (FMRIB Software Library) [29]. Preprocessing included motion correction (using the MCFLIRT algorithm with 6° of freedom) and co-registration and normalization to a common stereotactic space, for accurate registration, a two-step process was used; first, brain extraction was applied to the structural image, and the functional sequence was registered to it; then the structural image was registered to a standard asymmetric age-appropriate template (for ages 13.0–18.5) [30, 31]); these two transformations were used to finally register the functional sequence to the standard space. Before group analyses, normalized images were spatially filtered with a Gaussian filter (FWHM = 5 mm). Individuals with an estimated maximum absolute movement > 3.0 mm or an average absolute movement > 0.3 mm were excluded from analyses to minimize unwanted movement-related effects.
Statistical analyses were performed by means of General Linear Models (GLMs). At the single-subject level, three regressors of interest were defined in the GLM corresponding to the three task conditions (Self, Other and Facts). Instructions screens were modelled by an additional nuisance regressor. Fixation periods were not modelled and thus acted as an implicit baseline. GLMs were fitted to generate 1) activation and de-activations maps for the self- and another- reflection conditions compared to low level baseline and 2) activations maps comparing the experimental and control conditions (Self vs. Facts and Other vs. Facts).
Temporal derivatives for each regressor of interest, as well as movement parameters (six in total, three rotations and three translations) were included as additional regressors. Images were high-pass filtered with a 130 s cut-off.
At the intra-group level, task-related activations and /or de-activations were assessed with one-sample t-tests on the contrasts defined at the subject level with mixed-effects models [32] within the FEAT module. Comparisons between groups were run to evaluate differences between BPD and healthy controls. All statistical tests were carried out at the cluster level with a corrected p < 0.05 using Gaussian random field methods. A threshold of z > 3.1 (p < 0.001) at the voxel level was used to define the initial set of clusters.
Results
Demographic and clinical data
From the initial samples, 10 patients and 12 controls were excluded due to excessive head movement (see details in Supplementary Table S1) giving a final sample of 27 patients and 28 HC. As shown in Table 1, the finally included subjects were matched for age and estimated IQ.
fMRI results
Self- and other- reflection versus low level baseline
As shown in Fig. 1, clusters of significant activation in the healthy controls were similar for both self- and other-reflection and encompassed bilaterally the cerebellum, the inferior, middle, superior occipital and lingual gyrus, the calcarine, the cuneus, and the fusiform cortex, the anterior insula, the angular gyrus and supramarginal areas, as well as the inferior and dorsolateral frontal cortex, and the medial superior frontal cortex, including the supragenual anterior cingulate. Activations were also seen in the left temporal cortex (middle temporal gyrus and temporal pole) and in the pallidum, the putamen, the amygdala and the hippocampus and parahippocampal region. The TPJ was also activated, with the left side being involved in both tasks, and the right side specifically in the other-reflection task (see Fig. 1; for full details see Supplementary Table S2 and S3).
Areas of de-activation (i.e. BOLD activation < 0 when compared to low-level baseline activation) during both self- and other-reflection were seen in the subgenual anterior medial frontal cortex, the posterior cingulate cortex, the cuneus and precuneus. The right middle/superior temporal and inferior parietal/supramarginal cortex were two other regions showing de-activation (see Supplementary Table S4 and S5).
In the patients, the pattern of activations was similar to that of the healthy controls for both self- and other-reflection. De-activations were also similar, but whereas the anterior medial frontal subgenual cortex was de-activated during performance of both tasks in the controls, this was only the case for other-reflection in patients.
There were no clusters of difference between the patients and the controls in either the self- or other-reflection tasks.
Self-reflection vs facts
Activations in the self-reflection condition compared to fact processing are shown in Fig. 2A, B (for full details see Supplementary Table S6). The healthy controls showed greater activation during self-reflection in the medial frontal cortex, including the pregenual anterior cingulate cortex and the middle/posterior cingulate cortex involving the cuneus and precuneus. Greater activation was also seen in occipital, lingual, fusiform, and temporal polar regions, and in the left angular gyrus and middle temporal cortex and the TPJ, more markedly on the left. Activation was also seen in the left anterior insular and inferior and dorsolateral frontal cortex.
The pattern was broadly similar, though on visual impression, less marked in the BPD patients: greater activation during self-reflection compared to fact processing in a small cluster in the pregenual anterior cingulate cortex and a larger cluster in the middle/posterior cingulate cortex extending to precuneus and cuneus. There was also a small cluster of greater activation in the left TPJ. Greater self-related activation was also seen bilaterally in temporal polar regions.
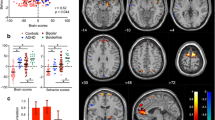
In the comparison between groups (Fig. 2C, for full details see Supplementary Table S7), the BPD patients showed significantly reduced activation in four clusters. One was in the right DLPFC, a second was in the left calcarine cortex, a third was in the left superior parietal cortex and finally there was a cluster in the right precentral gyrus.
Because, as pointed out by Gusnard and Raichle [33], relative changes between two active tasks can be difficult to interpret – specifically both reduced activation and increased de-activation will give the same appearances – we further explored the findings in regions of interest (ROIs) based on these clusters, examining the changes for both self-reflection and fact processing with respect to low level baseline. Boxplots are shown in Fig. 3. It can be seen that the healthy controls showed greater activation during self-reflection than during facts processing (left calcarine and right precentral clusters), or similar activation levels in both conditions (right DLPFC and left superior parietal clusters). In contrast, activation in the BPD patients was lower during self-reflection than fact processing in all clusters apart from the one in the left calcarine cortex. For the right DLPFC, where controls showed moderate activation, the BPD patients showed de-activation.
Other-reflection vs fact processing
In the healthy controls, the contrast other-reflection vs fact processing yielded a similar pattern of activation to the corresponding self-reflection vs fact processing comparison (see Fig. 4 and Supplementary Table S8). Greater activation during other-reflection was seen in the medial frontal cortex including the pregenual anterior cingulate, in this case also including the subgenual region, and in the middle/posterior cingulate cortex and the cuneus/precuneus. Greater activation was also seen in lingual, calcarine and temporal polar regions, and bilaterally in a region including the TPJ; on the left this cluster minimally included the the inferior frontal cortex and insula.
In the patients, activations were visually less marked, particularly in the medial frontal cortex and the lingual/calcarine cortex, but were similar to those of the controls in the cingulate region. Activations were also seen bilaterally in the angular and middle temporal cortex including the TPJ and the temporal poles.
The between-group comparison (Fig. 4C, for full details see Supplementary Table S9) revealed two clusters of decreased activation in the BPD patients, both located in the medial frontal cortex. One affected the subgenual anterior cingulate cortex, with a peak in the left hemisphere and another in a corresponding position on the right.
Figure 5 shows mean activations in a ROI based on these two clusters combined, examining the changes for both other-reflection and fact processing with respect to low level baseline It can be seen that this area was de-activated in both groups during both other-reflection and facts processing, with greater de-activation by the controls during the latter task. Accordingly, the differences between the BPD patients and the HC is attributable to a failure of de-activation in the fact processing task in the patients.
Boxplots for the medial frontal region-of-interest (combined left and right) where differences between the BPD and HC groups were found in the other-reflection vs fact processing contrast, showing mean activations during each condition compared to the low-level baseline It can be seen that this area was de-activated in both groups during both other-reflection and facts processing, with greater de-activation by the controls during the latter task.
Discussion
Our goal in this study was to identify, through a self- and other-reflection task, brain functional abnormalities potentially relevant to the identity disturbance of BPD, in the early stages of the disorder. The main finding was that adolescent patients with BPD showed markedly reduced activation in the right DLPFC, along with the parietal cortex, the occipital cortex and the precentral cortex, during the self-reflection task, but not the other-reflection task: it should also be noted that this alteration was only seen when self-reflection was contrasted with an active control condition, fact processing, and not with a low-level baseline. At a theoretical level, such a finding could be interpreted as reflecting difficulties in top-down cognitive regulation of identity-related processes in BPD.
In some ways our finding of activation changes in the DLPFC in patients with BPD during self-reflection is unexpected, given that in healthy subjects self-related cognition principally activates other regions, in particular the default mode network, i.e., the medial frontal cortex, the posterior cingulate cortex/precuneus and the angular gyrus, and the TPJ [19,20,21]. However, lateral frontal cortex activation has been documented in healthy subjects during performance of self-referential tasks. Thus, in a meta-analysis, Murray et al. [20] found activation in the left inferior frontal cortex compared to control tasks, and activation in the right inferior frontal cortex when self-referencing tasks were contrasted with other-referencing tasks. In another meta-analysis, van der Meer et al. [21] found activations in the left inferior frontal cortex in the contrast between self-reflection and a baseline condition, and in a dorsolateral frontal region similar to the cluster of differences we found when contrasting self- and other- processing. A third meta-analysis by Denny et al. [19] had similar findings.
Our findings in relation to self-reflection in BPD differ from those of the study by Scherpiet et al. [23] described in the introduction. These authors contrasted self-reflection with a task where the participants were asked to be aware of their current emotions and bodily feelings (‘mindful introspection’). Differently to us, their adult BPD patients showed increased activation compared to controls, in regions including in the right motor and somatosensory cortex, the right supramarginal gyrus, and the right superior temporal gyrus during a self-reflection task compared to a low-level baseline task. Contrasting self-reflection with mindful introspection, their BPD patients again showed increased activation compared to the healthy controls, this time in a large cluster encompassing the right anterior portion of the supplementary motor area, the superior, medial and middle frontal gyrus and the dorsomedial prefrontal cortex.
One other study should also be mentioned. Beeney et al. [34] examined self- and other-processing, although they used an unusual comparison task. They scanned 17 adult females with BPD and 21 healthy controls while they answered questions about their own personality characteristics (eg ‘Are you kind?’) and the personality characteristics of a close friend (eg ‘Is Julie kind?); there were also two ‘third-person’ conditions where the participants carried out cognitive operations perhaps best regarded as involving theory of mind (eg ‘According to Julie, are you kind?’ and ‘According to Julie, is she kind?’). Contrasting the self-and other-reflection conditions with the third person conditions revealed no differences between the BPD patients and the healthy controls.
In our study there were differences in activation changes between self- and other-reflection in patients in BPD. When compared to fact processing, self-reflection was associated with reduced DLPFC activation in the patients, whereas during other-reflection relatively reduced activation was seen in a different ___location, the subgenual anterior cingulate cortex. Further analysis then revealed that this reduced activation in fact reflected failure of de-activation in the BPD group during fact processing, something that was not the case for the self-reflection changes. Why differences affecting different frontal brain regions should be seen during self- and other-reflection is on the face of it difficult to explain, given that the two tasks are known to activate largely similar brain regions in healthy controls (something that was also the case in our study). One speculative interpretation might be that self- and other-processing become decoupled from each other in BPD, no longer both activating similar regions of the default mode network and the TPJ as in healthy subjects.
During both self-reflection and other-reflection, both the BPD patients and the healthy controls in our study showed activation in the TPJ. This was seen in the comparisons against both active control (fact processing) and low-level baseline on the left, although there was some variation as to whether this was bilateral or only seen on the left across the different conditions. However, no clusters of differential activation were observed between the BPD patients and the healthy controls in this region. The TPJ is known to be implicated in social cognition, having been argued to play a crucial role in understanding the beliefs of others [35] and possibly other social cognitive processes as well [36, 37]. Given that social interactions are central to BPD, the lack of activation differences between BPD patients and healthy individuals represents a potentially important negative finding, one that could perhaps point to a dissociation between processes underlying social cognition and identity disturbance in the disorder.
With only three functional imaging studies of self- and other-processing in BPD, and inconsistent findings among them, further theoretical speculations are difficult to make. Nevertheless, studies using such paradigms may well prove to be important, given that both ICD-11 and the Criteria A of DSM-5 Alternative Model for Personality Disorders (AMPD) have characterized disturbances in both self and interpersonal functioning as central features not only of BPD but of personality disorders in general [38]. Examination of adolescent patients with the disorder may also be of particular relevance here, as there is currently an emphasis on the ‘lifespan’ perspective in BPD, where proposed pathological mechanisms are viewed through the lens of psychosocial development [2, 6]. In this context, adolescence represents a critical period for the development of social cognition, a ___domain that has been consistently found to be altered in individuals with BPD [3]. Object relations theory posits that these impairments stem from a polarized representation of self and others and a deficient capacity to integrate positive and negative attributes [39]. Studying adolescents who already exhibit these impairments may provide key insights into the disorder’s developmental trajectory. In particular, functional neuroimaging studies of this population—especially those targeting self- and other-processing—could help elucidate the neurobiological mechanisms underlying these core psychopathological features and contribute to a more comprehensive understanding of BPD across the lifespan.
In conclusion, our study finds evidence of reduced activation in the right DLPFC during self-reflection in adolescent females with BPD, which might be indicative of impaired top-down cognitive control of self-processing in the disorder. We also observed a failure in deactivation in the ventromedial prefrontal cortex, a core region of the default mode network, during other-reflection, the significance of which is unclear. Some limitations need to be acknowledged. First, the fMRI task we used was designed to detect the neural correlates of self- and other-reflection, which are only at best only indirectly to the disturbed sense of identity that is central to BPD. However, it is important to bear in mind here that no better task has so far been developed. Related to this point, our study is limited by the fact that we did not employ a behavioral measure of disturbed sense of identity in the patients. Secondly, we only examined female patients with BPD. While BPD is substantially more prevalent in females, it also affects males and so our findings may not be generalizable to the latter. Thirdly, we studied BPD patients who had been screened to exclude comorbidities. While such a strategy makes sense for a functional imaging study, it will have likely resulted in a somewhat artificial group of patients, as comorbidities, including with Axis I disorders are common in the disorder [24], even in this age group [40]. Finally, at 27 patients and 28 controls, our sample sizes were in the accepted range for fMRI studies of clinical disorders, but it is possible that larger groups may have yielded clearer results, particular with respect to resolving the activation differences we found between self- and other-reflection.
Data availability
The data sets generated dunring and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gunderson JG, Herpertz SC, Skodol AE, Torgersen S, Zanarini MC. Borderline personality disorder. Nat Rev Dis Primers. 2018;4:1–21.
Winsper C, Lereya ST, Marwaha S, Thompson A, Eyden J, Singh SP. The aetiological and psychopathological validity of borderline personality disorder in youth: a systematic review and meta-analysis. Clin Psychol Rev. 2016;44:13–24.
Sharp C. Adolescent personality pathology and the alternative model for personality disorders: self development as nexus keywords adolescence · personality disorder · DSM-5 alternative model. Rev Artic Psychopathol. 2020;53:198–204.
Bohus M, Stoffers-Winterling J, Sharp C, Krause-Utz A, Schmahl C, Lieb K. Borderline personality disorder. Lancet. 2021;398:1528–40.
Newton-Howes G, Clark LA, Chanen A. Personality disorder across the life course. Lancet. 2015;385:727–34.
Videler AC, Hutsebaut J, Schulkens JEM, Sobczak S, Van Alphen SPJ. A life span perspective on borderline personality disorder. Curr Psychiatry Rep. 2019;21:51.
Amad A, Ramoz N, Thomas P, Jardri R, Gorwood P. Genetics of borderline personality disorder: systematic review and proposal of an integrative model. Neurosci Biobehav Rev. 2014;40:6–19.
Kimmel CL, Alhassoon OM, Wollman SC, Stern MJ, Perez-Figueroa A, Hall MG, et al. Age-related parieto-occipital and other gray matter changes in borderline personality disorder: a meta-analysis of cortical and subcortical structures. Psychiatry Res Neuroimaging. 2016;251:15–25.
Krause-Utz A, Winter D, Niedtfeld I, Schmahl C The latest neuroimaging findings in borderline personality disorder topical collection on personality disorders. Curr Psychiatry Rep. 2014;16. https://doi.org/10.1007/s11920-014-0438-z.
Lis E, Greenfield B, Henry M, Guilé JM, Dougherty G. Neuroimaging and genetics of borderline personality disorder: a review. J Psychiatry Neurosci. 2007;32:162–73.
Lischke A, Domin M, Freyberger HJ, Grabe HJ, Mentel R, Bernheim D, et al. Structural alterations in the corpus callosum are associated with suicidal behavior in women with borderline personality disorder. Front Hum Neurosci. 2017;11:196. https://doi.org/10.3389/fnhum.2017.00196.
Nunes PM, Wenzel A, Borges KT, Porto CR, Caminha RM, De Oliveira IR. Volumes of the hippocampus and amygdala in patients with borderline personality disorder: a meta-analysis. J Personal Disord. 2009;23:333–45.
Ruocco AC, Amirthavasagam S, Zakzanis KK. Amygdala and hippocampal volume reductions as candidate endophenotypes for borderline personality disorder: a meta-analysis of magnetic resonance imaging studies. Psychiatry Res. 2012;201:245–52. https://doi.org/10.1016/j.pscychresns.2012.02.012.
Ruocco AC, Carcone D. A neurobiological model of borderline personality disorder: systematic and integrative review. Harv Rev Psychiatry. 2016;24:311–29.
Schulze L, Schmahl C, Niedtfeld I. Neural correlates of disturbed emotion processing in borderline personality disorder: a multimodal meta-analysis. Biol Psychiatry. 2016;79:97–106.
Clarkin JF, De Panfilis C. Developing conceptualization of borderline personality disorder. J Nerv Ment Dis. 2013;201:88–93.
Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, et al. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. Am J Psychiatry. 2004;161:1296–8.
Peters JR, Crowe ML, Morgan T, Zimmerman M, Sharp C, Grilo CM, et al. Borderline personality disorder symptom networks across adolescent and adult clinical samples: examining symptom centrality and replicability. Psychol Med. 2023;53:2946–53.
Denny BT, Kober H, Wager TD, Ochsner KN. A meta-analysis of functional neuroimaging studies of self- and other judgments reveals a spatial gradient for mentalizing in medial prefrontal cortex. J Cogn Neurosci. 2012;24:1742–52.
Murray RJ, Schaer M, Debbané M. Degrees of separation: a quantitative neuroimaging meta-analysis investigating self-specificity and shared neural activation between self- and other-reflection. Neurosci Biobehav Rev. 2012;36:1043–59.
Van Der Meer L, Costafreda S, Aleman A, David AS. Self-reflection and the brain: a theoretical review and meta-analysis of neuroimaging studies with implications for schizophrenia. Neurosci Biobehav Rev. 2010;34:935–46.
Fuentes-Claramonte P, Martín-Subero M, Salgado-Pineda P, Alonso-Lana S, Moreno-Alcázar A, Argila-Plaza I, et al. Shared and differential default-mode related patterns of activity in an autobiographical, a self-referential and an attentional task. PLoS ONE. 2019;14:e0209376. https://doi.org/10.1371/journal.pone.0209376.
Scherpiet S, Herwig U, Opialla S, Scheerer H, Habermeyer V, Jäncke L, et al. Reduced neural differentiation between self-referential cognitive and emotional processes in women with borderline personality disorder. Psychiatry Res. 2015;233:314–23.
Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry. 1998;155:1733–9.
First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington, DC: American Psychiatric Press, Inc.; 1997.
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–8. https://doi.org/10.1097/00004583-199707000-00021.
First MB, Spitzer RL, Gibbon M, Williams JBW The structured clinical interview for DSM-III-R personality disorders (SCID-II). Part I: description. J Personal Disord. 1995; 9. https://doi.org/10.1521/pedi.1995.9.2.83.
Gomar JJ, Ortiz-Gil J, McKenna PJ, Salvador R, Sans-Sansa B, Sarró S, et al. Validation of the word accentuation test (TAP) as a means of estimating premorbid IQ in Spanish speakers. Schizophr Res. 2011;128:175–6.
Smith SM, Jenkinson M, Woolrich MW, Beckmann CF, Behrens TEJ, Johansen-Berg H, et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23:208–19.
Fonov V, Evans AC, Botteron K, Almli CR, McKinstry RC, Collins DL. Unbiased average age-appropriate atlases for pediatric studies. Neuroimage. 2011;54:313–27.
Fonov V, Evans A, McKinstry R, Almli C, Collins D. Unbiased nonlinear average age-appropriate brain templates from birth to adulthood. Neuroimage. 2009;47:S102.
Beckmann CF, Jenkinson M, Woolrich MW, Behrens TEJ, Flitney DE, Devlin JT, et al. Applying FSL to the FIAC data: model-based and model-free analysis of voice and sentence repetition priming. Hum Brain Mapp. 2006;27:380–91.
Gusnard DA, Raichle ME. Searching for a baseline: functional imaging and the resting human brain. Nat Rev Neurosci. 2001;2:685–94.
Beeney JE, Hallquist MN, Ellison WD, Levy KN. Self other disturbance in borderline personality disorder: neural, self-report, and performance-based evidence. Personal Disord. 2016;7:28–39.
Samson D, Apperly IA, Chiavarino C, Humphreys GW. Left temporoparietal junction is necessary for representing someone else’s belief. Nat Neurosci. 2004;7:499–500.
Decety J, Grèzes J. The power of simulation: imagining one’s own and other’s behavior. Brain Res. 2006;1079:4–14.
Eddy CM. The junction between self and other? Temporo-parietal dysfunction in neuropsychiatry. Neuropsychologia. 2016;89:465–77.
Swales MA. Personality disorder diagnoses in ICD-11: transforming conceptualisations and practice. Clin Psychol Eur. 2022;4:e9635.
Fertuck EA, Grinband J, Mann JJ, Hirsch J, Ochsner K, Pilkonis P, et al. Trustworthiness appraisal deficits in borderline personality disorder are associated with prefrontal cortex, not amygdala, impairment. Neuroimage Clin. 2019;21:101616.
Kaess M, Von Ceumern-Lindenstjerna I-A, Parzer P, Chanen A, Mundt C, Resch F, et al. Axis I and II comorbidity and psychosocial functioning in female adolescents with borderline personality disorder. Psychopathology. 2013;46:55–62.
Acknowledgements
This work was supported by the Instituto de Salud Carlos III and CIBERSAM-ISCIII, and co-funded by the European Union (ERDF/ESF “A way to make Europe”/“Investing in your future”): project PI15/02025 to MF and grant CD19/00149 to PF-C. Support was also received from the Catalonian Government (2017SGR1271, 2021SGR01475 to EP-C). PF-C is currently funded by a “la Caixa” Junior Leader Fellowship (LCF/BQ/PR22/11920017).
Author information
Authors and Affiliations
Contributions
Conceptualization: MF, XC, PJM, EP-C; Data curation: PS-P, NC, JDD-Y, AR, VP-R, JAR-Q, CV-V, PF-C; Formal analysis: PS-P, PF-C; Investigation: PS-P, MF, NC, JDD-Y, JAR-Q, PF-C, PJM; Methodology: PS-P, PF-C, RS, AR; Visualization: PS-P, MF, PF-C, EP-C; Resources: MF, PJM, EP-C; Funding acquisition: MF, PJM, EP-C; Supervision: RS, PJM, EP-C; Writing – original draft: PS-P, MF; Writing – review & editing: All authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Salgado-Pineda, P., Ferrer, M., Calvo, N. et al. Brain functional abnormality in drug naïve adolescents with borderline personality disorder during self- and other-reflection. Transl Psychiatry 15, 157 (2025). https://doi.org/10.1038/s41398-025-03368-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-025-03368-6