Abstract
People from refugee and migrant backgrounds often face poor experiences and outcomes in healthcare, and genetic healthcare is no exception. Understanding whether and how these health inequities manifest is an important step towards equitable perinatal genetic screening for genetic or chromosomal conditions (offered preconception, prenatally, or during the newborn period). A scoping review was conducted to review international evidence of perceptions and experiences of perinatal genetic screening for people from migrant and refugee backgrounds. Search strategies were applied to Medline, Embase, and CINAHL databases to identify articles meeting eligibility criteria. Evidence was synthesised using descriptive and content analysis, with theoretical frameworks of proportionate universality and relational autonomy used to interpret findings. Of 11,046 unique articles identified, twenty-six met inclusion criteria and underwent full-text review. Most studies were set in Western countries, and participants were primarily born in Asia, South America, or Africa. Studies indicated varying awareness, knowledge, attitudes, and uptake of screening. Several studies highlighted a lack of adequate in-language resources, the use of concepts that were unrecognised in particular communities, and poor interactions with healthcare providers. Strategies to address the above issues included person-centred counselling, increased consultation time, access to interpreters, and training for relevant providers. Other recommendations included addressing structural, financial, and geographical barriers to improve access to screening and associated care. Whilst additional research is required, we propose evidence and theory-informed strategies to improve perinatal genetic screening services for people from migrant and refugee backgrounds.
Similar content being viewed by others
Background
Perinatal genetic screening (‘screening’ herein) refers to screening with the primary purpose of identifying individuals and families with an increased chance of chromosomal and genetic conditions preconception, during pregnancy, or during the first year of life [1,2,3]. This includes reproductive genetic carrier screening offered before or in early pregnancy, aneuploidy screening for chromosome conditions offered during pregnancy, or newborn screening offered in early infancy [1,2,3]. Information from screening may help people to make informed reproductive decisions, and/or access early intervention and support for their children [1,2,3].
A key principle in delivering screening in most contexts is ensuring it is presented as optional and creating the opportunity for informed decision-making [4,5,6]. Informed decision making involves an individual making a deliberate decision that is aligned with their values and based on good knowledge about screening [7]. Informed decision making for screening may be facilitated by healthcare providers (HCPs) such as general practitioners, obstetricians, fertility specialists, and midwives, with the support of genetic HCPs such as genetic counsellors as required. However, HCPs involved in screening have cited a lack of time and complexity of genetic information as key barriers to discussing screening, particularly reproductive genetic carrier screening, and non-invasive prenatal testing [8, 9]. Digital tools such as online decision aids, portals, websites, factsheets, and chatbots have been used to supplement the above conversations, particularly as screening becomes more widely available [10,11,12,13]. It is important to understand whether this wide range of approaches is meeting the needs of the community. The first step in doing so involves understanding experiences and perceptions of screening. Specifically, this should include exploring experiences and perceptions of people who are known to face healthcare inequities, such as people from migrant and refugee backgrounds [14,15,16,17]. While definitions can differ widely across the literature, we use the term migrant to include people born outside the country in which they are residing, who have moved for various reasons including education or to be with family [18]. In contrast, people with a refugee background have been forcibly displaced from their country of nationality or usual residence. The term refugee background includes people who are legally deemed refugees as well as others with refugee-like experiences, including persecution, torture, trauma, loss of human rights, and separation from family members and friends [19]. Although important differences exist between migrant and refugee background experiences, these populations are infrequently and poorly delineated in the genetics literature. We use the term ‘people from migrant and refugee backgrounds’ to acknowledge the overlap and lack of consistency in terminology within the literature. Specific reference to ‘migrant’ or ‘refugee’ is used only when adequately defined by studies cited.
People from migrant and refugee backgrounds often have poorer healthcare experiences compared to those born locally [14,15,16,17]. This is particularly the case for people of refugee backgrounds, or those born in lower-income, conflict-affected, or non-Western countries [14,15,16,17]. Poorer experiences of healthcare may involve delayed or limited access to healthcare services, lack of information about available services, challenges in navigating the healthcare system, inadequate or incorrect health information, and lower empowerment or autonomy in relation to their healthcare [14,15,16,17]. Such experiences vary based on context and may be influenced by individual factors (e.g. English language proficiency), HCP factors (e.g. cultural sensitivity), and systemic factors (e.g. cost and ___location of healthcare services) [16].
While experiences are highly contextual, it is important to understand whether there are any common experiences and opportunities for intervention in the screening setting. An initial literature review revealed heterogeneity in the terminology used to describe both screening and participant demographics or identity. Articles that were identified described experiences of people from migrant and refugee backgrounds across several different screening and healthcare settings. Therefore, we conducted a scoping review, aiming to systematically identify and map global evidence regarding perceptions and experiences of screening for people of migrant and refugee backgrounds.
Methods
Due to the broad exploratory nature of our research enquiry, we undertook a scoping review guided by the Joanna Briggs Institute approach [20] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses scoping review extension [21].
Eligibility criteria
Eligibility criteria were determined through an iterative process as per the Joanna Briggs Institute approach, specifying population, context, concept, and source type (Table 1). In summary, papers were eligible for the scoping review if they were peer-reviewed original research articles reporting on uptake, experience, or perceptions of screening for people born outside the country in which the study was set.
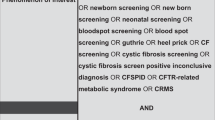
Literature search
The search strategy was developed in collaboration with an experienced medical librarian. The search strategy was built iteratively, based on three constructs: people from migrant and refugee backgrounds; preconception and pregnancy genetic screening; and views and experiences. We included Medical Subject Headings (MeSH) terms, subject headings, and keywords. Once appropriate key search terms were selected, they were adapted to the requirements of three selected databases: Medline, Embase, and CINAHL. The primary search was undertaken on 22nd December 2022 and re-run on 2nd October 2024. The full search strategy is available in Supplementary Material 1.
Study selection
Articles were imported to Zotero reference manager for removal of duplicates, then to Covidence systematic review software for screening [22]. All articles were screened by AK and ET in two stages: screening titles and abstracts; and screening full texts. Inconsistencies were resolved through discussion, involving others in the research team as required.
Quality appraisal
Quality appraisal is not generally performed in a scoping review unless there is a specific reason to do so [20]. In this review, quality appraisal was not conducted. All studies meeting the selection criteria were included, with characteristics and quality of studies discussed where appropriate.
Data charting and analysis
A data extraction form was created in Microsoft Excel, piloted by AK with five papers, and reviewed with the research team prior to use across all studies. Extracted data included details about source type (including year of publication and study type); participants (including country of residence and country of birth); context (including type of screening and study setting); and concept (including study aims and findings). Study characteristics were analysed using descriptive statistics. Total numbers varied due to overlapping categories, and/or missing data.
Results and discussion content were analysed using inductive content analysis [23]. This involved coding any content that related to the scoping review research question. Relevant content was initially coded into broad categories which were then compared and refined into more specific sub-categories and codes. Categories and codes were synthesised, interpreted and presented in a narrative format in the results section below. Data extraction and analysis were led by AK, with analyses refined and interpreted through discussions with the research team.
Results
Study selection
The literature search resulted in 11,046 records. After removing duplicates, 8,784 titles and abstracts were screened. One hundred and ninety-five full texts were screened, resulting in a total of 26 articles eligible for this scoping review (Fig. 1).
Study characteristics
Study characteristics are described in Table 2. In summary, most studies included in the review: were conducted in the continents of Europe (11/26, 42%) and North America (9/26, 35%); included participants born in various regions (10/26, 38%) or focused on participants born in countries in Asia (9/26, 35%); reported on aneuploidy screening (18/26, 69%); explored experiences of screening offered in clinical settings outside the research study (19/26, 73%); and recruited participants from pregnancy care settings (15/26, 58%).
Our synthesis revealed that the articles covered outcomes, experiences, perceptions and suggestions regarding [1]: screening awareness and information, and [2] screening attitudes, decisions, and access. Table 3 illustrates a summary of review findings which are further described below.
Screening awareness and information
Studies included in the review reported on participant awareness, knowledge, recall; experiences of receiving information and being offered screening; and suggestions for how information about screening should be delivered.
Participant awareness and knowledge
Thirteen studies reported on participant awareness and knowledge of screening [24,25,26,27,28,29,30,31,32,33,34,35,36]. Results from these studies are summarised below, with further details provided in columns K, L and M of Supplementary material 2. Most studies relied on participant self-reporting or subjective author assessments about awareness and knowledge of screening [24,25,26,27,28,29,30, 32, 34, 36]. Three studies calculated knowledge scores based on survey questions, which differed from study to study [28, 31, 33].
While outcomes varied within and across studies, over 50% demonstrated limited screening awareness and/or knowledge for participants born overseas (Table 4). There were no apparent trends in awareness and knowledge regarding study characteristics such as participant country of birth, study setting, or test type. However, one study found that higher knowledge scores were associated with English as a first language, a longer time in the country of residence, previous counselling about screening, and having more than one pregnancy [33]. This study reported no associations between knowledge and gestational age, maternal age, employment, marital status, education, income, ethnicity, and health literacy [33]. Overall, the studies provide evidence to suggest limited awareness and knowledge for people born overseas in several contexts. However, there are inconsistencies in awareness and knowledge assessment and variability in participant outcomes.
Experiences of receiving screening information
Those who were aware of screening had obtained information from several different sources, including non-genetics HCPs [25, 27, 32, 34, 36], genetics HCPs [28, 30, 34], family [28, 30, 34], friends [28, 34, 36], other community members [27, 30, 36], mass/ social media [27, 32], and marriage court [27]. However, studies also reported several issues relating to screening information for people born overseas: screening information was sometimes only available in languages they did not understand [29, 37, 32, 35, 36]; included concepts that are unrecognised in their community [25, 38]; lacked information on how to arrange testing [27]; and was generally confusing or inaccessible [25, 26, 32, 35]. In one study, several participants mentioned using a website providing general information for Korean immigrants in the US and identified a lack of screening information on this website [37]. Similarly, participants in another study mistakenly assumed that the information about screening provided via Japanese sources applied in Austria [32]. In some cases, participants also felt that their HCPs were uninformed about screening [26, 31].
Experiences of being offered screening
In addition to screening information sources, nine studies reported on the formal offer of screening when screening was offered in a clinical setting outside the study setting (Table 2). Two studies audited actual offer rates [39, 40], whereas other studies relied on participants self-reporting whether they were offered screening [24, 27, 28, 41, 31, 32, 34]. One study reported that country of birth was not associated with whether participants were offered screening [39]. However, other studies provided several examples of people born overseas not being offered screening or being offered screening too late for it to be relevant [24, 25, 27, 28, 40, 31, 32, 34]. In some cases, a lack of offer was due to late attendance for perinatal care [40, 41], or due to screening not being the most appropriate test for the individual [34]. Authors also speculated that low offer rates and understanding of screening may have been due to HCPs holding implicit biases, not having time, or lacking cultural competence [24, 25, 41, 31, 36].
Suggestions for screening information
Participants across several studies expressed a desire to receive information about screening and/or genetic risk, regardless of decisions they might make [42, 28, 29, 43, 41, 34, 44]. However, most suggestions about how the screening information should be delivered came from authors, often based on other existing literature or evidence generated in their study. Authors emphasized the importance of screening information being high-quality, timely, accurate, detailed, understandable, simple, clear, empathetic, and centralized [25,26,27,28, 30, 40, 32, 38, 44, 35, 36]. Some suggested that general public education may increase awareness for people born overseas [35, 36], whereas some highlighted the importance of targeted information aligning with community beliefs and practices [26, 28, 38, 35, 36].
Only four studies provided evidence of participant preferences for how screening information should be delivered [26, 30, 34, 36]. In these studies, participants emphasized the importance of screening information being high quality, timely, available in accessible locations outside the healthcare setting, delivered in multiple formats, available in multiple languages, and tailored for specific communities as required [26, 30, 34, 36]. For example, participants born in Pakistan and residing in the UK expressed a desire for public education, tailored for the Pakistani community with a belief that this may reduce stigma and enable individuals to discuss genetic risk more openly [26]. They emphasized a need to address disability, ‘options available for limiting disability’, as well as common areas of confusion in the Pakistani community, such as how consanguinity is related to genetic risk [26]. These results indicate limited evidence about participant preferences for screening information and demonstrate that both general and targeted approaches are required.
Screening attitudes, decisions, and access
Studies included in the review described participant attitudes, uptake, beliefs, and values regarding screening. They also explored how social influences, healthcare provider involvement, and structural barriers influenced screening decisions and experiences.
Participants attitudes toward screening
Eight studies reported on participant attitudes toward screening, regardless of actual uptake [45, 46, 26, 30, 31, 38, 47, 44]. Results are summarised below, and further details are provided in N, O, and P of Supplementary material 2. Attitudes toward screening were based on pre-existing knowledge of screening [30, 45], screening information delivered during the study [46, 31, 47, 44], or hypothetical case studies [26, 38]. One study calculated an attitude score based on survey responses [31], and attitudes in the remaining studies were self-reported by participants in surveys or interviews [45, 46, 26, 30, 38, 47, 44]. Participants born overseas generally had a positive attitude towards screening, with variation within and between studies (Table 4). There were no apparent trends in attitudes toward screening regarding study characteristics such as participant country of birth, study setting, or test type. However, one study demonstrated that lower intention to have screening was associated with limited or absent national language proficiency, particular ethnicities, and living in less urban areas [41]. The study reported no association between maternal age or immigrant generation and intention to have screening [41]. Overall, these studies demonstrate variability within and between studies, with a skew toward positive attitudes about screening.
Participant uptake of screening
Fourteen studies reported on screening uptake [24, 25, 27,28,29, 43, 48, 30, 39,40,41, 32, 49, 35]. Results are summarised below, with further details in columns Q, R, and S of Supplementary material 2. Uptake was assessed in relation to screening offered either in a clinical setting external to the study [24, 25, 27,28,29, 43, 48, 30, 39,40,41, 32, 35], or as part of the research study [28, 49]. Screening uptake was either self-reported in surveys and interviews [24, 25, 27,28,29, 43, 30, 32, 35], based on clinical audit data [48, 39, 40, 49], or provided by HCPs [41]. There was variability in screening uptake across studies, with no apparent trends in uptake regarding study characteristics such as participant country of birth, study setting or test type (Table 4). However, one study found that uptake was associated with living in a non-urban area, receiving pregnancy care from a physician or midwife over an obstetrician, being younger, and being in a lower income quintile [48]. The study reported no association between screening uptake and maternal age during first pregnancy, history of pregnancy loss, history of congenital anomalies, or immigration status [48]. Overall, these studies demonstrated that screening uptake was primarily self-reported and varied within and between studies.
Participant beliefs and values about screening
Fourteen studies explored beliefs and values about screening of people born overseas. Those who saw value in screening did so for various reasons, with many believing that it would provide useful information about the health of their pregnancy or children (Table 4). Those who saw less value in screening felt the information would not change anything or believed that genetic conditions had non-genetic causes (Table 4).
Of note in the reviewed articles was a reported complex relationship between religion, spiritual beliefs, screening, and termination of pregnancy (TOP). Some participants felt that they would accept the child that God gave them and/or would not have a TOP because it was not allowed in their religion [42, 26, 30, 34, 38]. Others felt that they would terminate an affected pregnancy regardless of religious rules, or believed that TOP would be accepted by their religion in specific situations [42, 26, 43]. For some, screening felt meaningless if they would not consider further testing or TOP [46, 30, 32], whereas others saw value in screening even if TOP was not an option [42, 30, 34, 35].
Regardless of their decisions, some participants held concerns regarding screening [26, 27, 30, 44, 36]. Some concerns related to the testing process, such as accuracy [30, 44], privacy [30], time taken to test [30], and lack of trust in the result [27]. Other concerns related to implications of the diagnosis such as psychological impact of a diagnosis [30, 44]; whether they would receive adequate information and support [44]; how a diagnosis would be viewed by family, employees, or marriage prospects [26, 36]; and concerns about receiving incidental findings unrelated to the purpose of testing [30].
Involvement of healthcare providers in screening decisions
There were several examples of participants feeling that HCPs had empowered them to make their own decisions about screening [29, 32, 34]. However, some participants had testing because their HCP recommended it [27, 42], they believed it was compulsory [32], felt pressured to have screening [32], or it was mandated by a marriage court [27]. Some participants faced challenges in discussing their decisions with HCPs due to language barriers [37, 32, 36], rushed or ad hoc discussions [32], experiencing passivity when communicating with HCPs [32], concerns that HCPs would not share or understand their views [42], a sense that their culture was being criticised in relation to consanguinity [26], and previous experiences of discrimination perpetuated by HCPs [26, 36].
Involvement of others in screening decisions
Studies explored how participants involved or wished to involve other individuals in their screening decisions. The importance of including family in decisions about screening was highlighted in four studies with participants born in Southeast Asia, East Asia, and Latin America [42, 29, 32, 38]. Involvement of partners varied, with some not involving their partners in screening decisions, some wishing to involve their partner in decisions, and some prioritising their partner’s perspective [42, 29, 43, 32]. In one study, participants expressed frustration about a lack of in-depth communication and support from their partner [32]. Participants in another study tended to seek support from their partner or family as needed and saw HCPs as an information source only [38].
Some studies also commented on the influence of individuals who were not directly involved in decisions. Participants in three studies were influenced by the screening experiences of their family and friends [29, 32, 36]. In a study conducted with people born in Somalia residing in USA, participants were not supportive of screening because TOP was not accepted by their community [46]. Conversely, in a study conducted with people born in Southeast and East Asia residing in USA, participants raised that people may feel social or family pressure to have screening and/or terminate pregnancies due to lack of resources available for people with disabilities in Asian countries, a fear of shame or negative judgement, or lack of exposure to disability [38]. Some participants worried about being judged as irresponsible if they chose not to have screening [42], whereas others commented that they were not concerned about other people’s opinions regarding their screening decisions [30, 42].
Access to screening
Ten studies reported on structural facilitators and barriers that could impact access to information, support, and screening itself [42, 45, 27, 29, 43, 37, 32, 38, 35, 36]. In the context of funded screening, participants appreciated that it was free of charge [42]. Participants in two studies also commented that screening was more available in the country of residence compared to their country of origin [29, 32]. However, some faced barriers such as cost of screening and associated care [45, 27, 29, 43, 37, 32, 38, 35, 36]; inconvenient locations or processes [29, 37, 35, 36]; reluctance to seek healthcare due to fear of deportation [29, 36]; and lack of resources to meet specific needs of people born overseas [36].
Suggestions for decision support and access
Six studies explored participant expectations for HCP involvement in screening decisions. Some participants valued individual autonomy and saw HCPs as a source of information or emotional support [42, 29, 43, 38, 44]. Conversely, some wanted directive advice from HCPs about whether to have screening [42, 38, 44, 36], felt screening should be compulsory [42], or felt it would be challenging to say ‘no’ if an HCP offered it [42]. Reasons for these views included a lack of confidence to make screening decisions on their own or believing that not everyone would be able to decide for themselves. Others felt that their HCP may hold fatalistic beliefs and would therefore recommend against screening [38]. There were no apparent commonalities in these studies in relation to participant country of birth, study setting or test type. Only one study provided participant suggestions of how to address decision support needs, and most participants in this study worked in healthcare themselves [38]. Participants in this study suggested that HCPs disclosing what they would do in a similar situation could facilitate rapport, encourage people from Asian backgrounds to engage in the decision-making process, and remove the individual’s potential burden of making a decision without providing explicit direction [38].
Additionally, two studies explored the approach of discussing screening in a group prenatal care setting, with authors highlighting that this may be more efficient and cost-effective than individual counselling [29, 34]. Some participants saw the group approach as an opportunity for social support and to learn from others in similar situations, particularly when living away from family [29, 34]. Others expressed a preference for individual appointments to ensure privacy and a focus on their individual circumstances [29, 34].
The studies provided limited evidence of participant preferences and needs regarding decision support and no participant suggestions regarding structural access to screening. However, several authors made their own suggestions. Most of these authors highlighted the importance of person-centred counselling through suggestions such as recognising diversity within groups, considering cultural beliefs and practices when discussing screening, incorporating family dynamics into screening decisions, assessing individual expectations of the HCP role in decision making, and using written or visual aids as required [42, 46, 26, 28, 29, 43, 38]. Authors also conveyed that HCPs need to be provided with resources such as time, and access to interpreters for adequate discussions about screening to occur [25, 28,29,30, 40, 36].
Authors in some settings suggested a need for education informing HCPs about relevant cultural beliefs, practices, and implicit biases, as well as screening education for other staff such as social workers and interpreters [24, 46, 25, 43, 36]. Structural access issues were considered from the context of carrier screening in Thailand [35, 36]. Authors suggested approaches such as a government-funded thalassaemia prevention programme for migrants, which already exists for citizens [35, 36]. They also suggested offering screening in more convenient locations to address participant concerns such as missing work and losing income to attend hospital care [35, 36]. However, it was unclear as to where the ideal ___location would be, due to issues such as screening in workplaces requiring employer engagement and raising confidentiality concerns, or screening in schools or premarital settings relying on people migrating in time to be offered [35, 36].
Discussion
This is the first review of international evidence regarding perinatal genetic screening for people from migrant and refugee backgrounds. The review highlighted the variation in experiences, views, and preferences across individuals and communities, as well as potential areas for improvement for screening services. Variability in experiences and views was apparent across different healthcare contexts. Furthermore, it was clear that other factors such as language, religion, and family dynamics influenced experiences. However, our understanding of the intersectionality of these factors was limited by what was reported.
Proportionate universalism can help to explain and contextualise many of the issues related to screening awareness and information raised by this review. Proportionate universalism advocates for the delivery of universal services at a scale and intensity proportionate to level of need [50]. This approach aims to improve health across the whole population while recognizing that needs fall on a continuum [50]. Taking a completely universal or standard approach to delivering healthcare services may disproportionately advantage those who are most able to access the services. Thus, targeted approaches are necessary to achieve health equity [50, 51].
In the context of screening, issues such as receiving inadequate information, not being offered screening in time for it to be useful, or facing structural barriers have also been identified at the broader population level [52,53,54]. Therefore, strategies such as educating HCPs about screening, raising public awareness, and providing access to information about screening in different formats may universally improve screening experiences.
The review also identified considerations about the above issues as well as novel issues that are unique to people of migrant and refugee backgrounds. This included lack of in-language information and support, information that does not consider cultural beliefs and expectations, and HCP implicit biases. Therefore, targeted approaches for people of migrant and refugee backgrounds may include improving language access, providing HCPs with education about cultural safety, considering community specific beliefs or concerns about disability and screening, and addressing structural barriers. Specific interventions may be context-dependent; therefore, health equity and language access frameworks, such as the ‘Cultural responsiveness framework - guidelines for Victorian health services’ [55], recommend that needs assessments should be conducted in any context where this has not previously been explored.
With regard to screening attitudes and decisions, motivations and concerns about screening that were identified in these studies primarily reflected those in broader population studies [56,57,58]. For example, seeking information to inform reproductive decisions or access early diagnosis and treatment are common reasons to pursue screening [56, 57, 59]. These findings emphasize the importance of supporting individuals, including people from migrant and refugee backgrounds, to make screening decisions considering their own beliefs and values.
Notably, several participants experienced, expected, or desired more involvement or direction from their HCP, partner, or other family members. However, informed decision-making is often framed as an autonomous decision being made in relation to the individual’s beliefs with minimal involvement from others [60]. While minimising involvement from others aims to protect individuals from coercion, pressure, or excessive influence, it has also been challenged as being too narrow, placing too much emphasis on the information aspect of informed decision-making, and not always considering the social contexts within which people make health and screening decisions [61,62,63,64,65]. This may particularly be the case for people from more collectivist cultures given close connections between informed decision-making, autonomy, and Western ideologies of individualism [66, 67].
An alternative view of autonomy, relational autonomy, acknowledges that others play a central role in decision-making [60]. Relational autonomy encourages HCPs to respect the individual while also encouraging them to consider their social situation and influences [60]. Suggestions made by the authors of studies included in this review may assist HCP to take a more relational approach to facilitating informed decision-making, including practicing person-centred care, considering family dynamics, and assessing what the individual expects from the HCP. However, these suggestions primarily come from authors rather than participants themselves. Further research from the perspective of community and HCPs is required to further understand how to best meet the needs of people from migrant and refugee backgrounds in healthcare interactions regarding screening.
Using evidence mapped in this review, and connecting to the theoretical concepts discussed, we propose several strategies to improve screening services for people from migrant and refugee backgrounds (Table 5). These strategies may be applied at the healthcare system and/or service level, or by individual healthcare providers and may be aimed at improving screening experiences universally or targeting groups or individuals who experience inequities.
Limitations
Retrieving and mapping evidence in this scoping review was limited by several factors. Heterogeneity of terminology and definitions of terms within the literature may mean that we have not captured all papers relevant to the review. For example, several articles were excluded due to a lack of clarity about whether the study was about screening or diagnostic testing. Articles were also excluded if it was not clear as to whether the study was describing country of birth, ethnicity, or race.
While there are several characteristics and concepts that have a close relation to country of birth, such as language, nationality, ethnicity, and race, we limited the eligibility criteria to be based on the objective construct: country of birth relative to country of residence/study conduct. Concepts such as language, nationality, ethnicity, and race may be included in the eligibility criteria of future reviews to further develop our understanding of how communities experience screening.
Furthermore, while the findings of the included studies are highly contextual, the breadth of evidence highlights key considerations for delivering screening programmes for people of migrant and refugee backgrounds.
Conclusion
This scoping review aimed to map global evidence of perceptions and experiences of perinatal genetic screening for people from migrant and refugee backgrounds. Similar to the studies within the broader population, studies with people from migrant and refugee backgrounds highlighted varying screening awareness, knowledge, attitudes, beliefs, and uptake. Some issues experienced by people from migrant and refugee backgrounds have also been identified in research about the broader population. However, people from migrant and refugee backgrounds experience unique issues such as a lack of screening information in their language, information not tailored to their culture or context, and interactions with healthcare providers that did not meet their expectations or needs. There is a clear need for approaches that are targeted and contextual to the needs of specific communities from migrant and refugee backgrounds. This scoping review provides overarching considerations for health systems, screening services, and HCPs to work toward equitable perinatal genetic screening. Further research could support the development of interventions for specific migrant and refugee communities, and an understanding of what types of support are needed to enable HCPs and systems to deliver more culturally sensitive screening services.
References
Bowman‐Smart H, Savulescu J, Mand C, Gyngell C, Pertile MD, Lewis S, et al. Small cost to pay for peace of mind’: Women’s experiences with non‐invasive prenatal testing. Aust NZ J Obstet Gynaecol 2019;59:649–55.
Delatycki MB, Alkuraya F, Archibald A, Castellani C, Cornel M, Grody WW, et al. International perspectives on the implementation of reproductive carrier screening. Prenat Diagn 2020;40:301–10.
Therrell BL, Padilla CD, Loeber JG, Kneisser I, Saadallah A, Borrajo GJC, et al. Current status of newborn screening worldwide: 2015. Semin Perinatol 2015;39:171–87.
Evans A, LeBlanc K, Bonhomme N, Shone SM, Gaviglio A, Freedenberg D, et al. A newborn screening education best practices framework: development and adoption. Int J Neonatal Screen 2019;5:22.
Sagaser KG, Malinowski J, Westerfield L, Proffitt J, Hicks MA, Toler TL, et al. Expanded carrier screening for reproductive risk assessment: An evidence-based practice guideline from the National Society of Genetic Counselors. J Genet Counsel 2023;32:540–57.
Kater-Kuipers A, de Beaufort ID, Galjaard RJH, Bunnik EM. Rethinking counselling in prenatal screening: An ethical analysis of informed consent in the context of non-invasive prenatal testing (NIPT). Bioethics 2020;34:671–8.
van den berg M, Timmermans D, Kate L, van Vugt J, van der Wal G. Informed decision making in the context of prenatal screening. Patient Educ Counsel 2006;63:110–7.
Best S, Long J, Theodorou T, Hatem S, Lake R, Archibald A, et al. Health practitioners’ perceptions of the barriers and enablers to the implementation of reproductive genetic carrier screening: A systematic review. Prenat Diagn 2021;41:708–19.
Lewis C, Hill M, Chitty LS. Offering non-invasive prenatal testing as part of routine clinical service. Can high levels of informed choice be maintained? Prenat Diagn 2017;37:1130–7.
Archibald AD, McClaren BJ, Caruana J, Tutty E, King EA, Halliday JL, et al. The Australian reproductive genetic carrier screening project (Mackenzie’s Mission): Design and Implementation. J Pers Med 2022;12:1781.
Bombard Y, Ginsburg GS, Sturm AC, Zhou AY, Lemke AA. Digital health-enabled genomics: Opportunities and challenges. Am J Hum Genet 2022;109:1190–8.
Lee W, Shickh S, Assamad D, Luca S, Clausen M, Somerville C, et al. Patient-facing digital tools for delivering genetic services: a systematic review. J Med Genet. 2022;jmedgenet-2022-108653.
Yeşilçinar İ, Seven M, Paşalak Şİ, Güvenç G. Interventions aiming to improve informed decision on prenatal screening and testing: A scoping review of the literature. J Genet Counsel 2021;30:1512–21.
Khatri RB, Assefa Y. Access to health services among culturally and linguistically diverse populations in the Australian universal health care system: issues and challenges. BMC Public Health 2022;22:880.
Mengesha ZB, Perz J, Dune T, Ussher J. Refugee and migrant women’s engagement with sexual and reproductive health care in Australia: A socio-ecological analysis of health care professional perspectives. Smith Fawzi MC, editor. PLoS One 2017;12:e0181421.
Mengesha ZB, Dune T, Perz J. Culturally and linguistically diverse women’s views and experiences of accessing sexual and reproductive health care in Australia: a systematic review. Sex Health 2016;13:299.
Billett H, Vazquez Corona M, Bohren MA. Women from migrant and refugee backgrounds’ perceptions and experiences of the continuum of maternity care in Australia: A qualitative evidence synthesis. Women Birth 2022;35:327–39.
United Nations International Organization for Migration. International Organization for Migration. 2023 [cited 2023 Jun 18]. About Migration. Available from: https://www.iom.int/about-migration.
Yelland J, Riggs E, Szwarc J, Vanpraag D, Dawson W, Brown S. Improving the ascertainment of refugee-background people in health datasets and health services. Aust Health Rev 2018;42:130–3.
Aromataris E, Munn Z JBI Manual for Evidence Synthesis. Joanna Briggs Institute; 2020 [cited 2022 Nov 28]. Available from: https://jbi-global-wiki.refined.site/space/MANUAL.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018;169:467–73.
Veritas Health Innovation. Covidence systematic review software [Internet]. Melbourne, Australia; Available from: www.covidence.org.
Vears DF, Gillam L. Inductive content analysis: A guide for beginning qualitative researchers. Focus Health Prof Educ: A Multi-Prof J 2022;23:111–27.
Anselem O, Saurel-Cubizolles MJ, Khoshnood B, Blondel B, Sauvegrain P, Bertille N, et al. Does women’s place of birth affect their opportunity for an informed choice about Down syndrome screening? A population-based study in France. Anselem O AE Bonnet MP, Cognet M, Deneux Tharaux C, Guedj R, Linard M, Ngo C, Richetin J, Rousseau A, Saurel MJ, Sauvegrain P, editor. BMC Pregnancy Childbirth 2021;21:590.
Chilaka VN, Konje JC, Stewart CR, Narayan H, Taylor DJ. Knowledge of Down syndrome in pregnant women from different ethnic groups. Prenat Diagn 2001;21:159–64.
Darr A, Small N, Ahmad WIU, Atkin K, Corry P, Benson J, et al. Examining the family-centred approach to genetic testing and counselling among UK Pakistanis: A community perspective. J Community Genet 2013;4:49–57.
El Sabeh M, Kassir MF, Ghanem P, Saifi O, El Hadi D, Khalifeh Y, et al. Consanguinity rates among Syrian refugees in Lebanon: a study on genetic awareness. J Biosoc Sci 2021;53:356–66.
Farrell R, Hawkins A, Barragan D, Hudgins L, Taylor J. Knowledge, understanding, and uptake of noninvasive prenatal testing among Latina women. Prenat Diagn 2015;35:748–53.
Garza G, Hodges-Delgado P, Hoskovec J, Palos G, Wagner C, Zacharias N, et al. Exploring experiences and expectations of prenatal health care and genetic counseling/testing in immigrant Latinas. J Genet Counsel 2020;29:530–41.
Josephi-Taylor S, Barlow-Stewart K, Selvanathan A, Roscioli T, Bittles A, Meiser B, et al. User acceptability of whole exome reproductive carrier testing for consanguineous couples in Australia. J Genet Counsel 2019;28:240–50.
Peters IA, Posthumus AG, Reijerink-Verheij JCIY, Van Agt HME, Knapen MFCM, Denktas S. Effect of culturally competent educational films about prenatal screening on informed decision making of pregnant women in the Netherlands. Patient Educ Counsel 2017;100:776–82.
Seidler Y, Mosor E, Stamm T. No one to consult! That is the hardest part’ choice-making experiences for prenatal screening tests among Japanese women and their spouses in Austria - A qualitative interview study. Patient Educ Counsel 2019;102:2286–95.
Sheinis M, Bensimon K, Selk A. Patients’ Knowledge of Prenatal Screening for Trisomy 21. J Genet Counsel 2018;27:95–103.
Thompson S, Noblin SJ, Lemons J, Peterson SK, Carreno C, Harbison A. Perceptions of Latinas on the Traditional Prenatal Genetic Counseling Model. J Genet Couns 2015;24:675–82.
Xu JZ, Tanongsaksakul W, Suksangpleng T, Ekwattanakit S, Riolueang S, Telen MJ, et al. Feasibility of and barriers to thalassemia screening in migrant populations: a cross-sectional study of Myanmar and Cambodian migrants in Thailand. BMC Public Health 2021;21:1177.
Xu JZ, Foe M, Tanongsaksakul W, Suksangpleng T, Ekwattanakit S, Riolueang S, et al. Identification of optimal thalassemia screening strategies for migrant populations in Thailand using a qualitative approach. BMC Public Health 2021;21:1796.
Jun M, Thongpriwan V, Choi J, Sook Choi K, Anderson G Decision-making about prenatal genetic testing among pregnant Korean-American women. Midwifery. 2018;56((Jun) University of Wisconsin-Green Bay, Department of Nursing and Health Studies, 2420 Nicolet Dr., Green Bay, WI 54311, United States):128–34.
Tsai GJ, Cameron CA, Czerwinski JL, Mendez-Figueroa H, Peterson SK, Noblin SJ. Attitudes towards prenatal genetic counseling, prenatal genetic testing, and termination of pregnancy among Southeast and East Asian Women in the United States. J Genet Couns 2017;26:1041–58.
Moses RM, Brown JHW, Wright DC, Diplock H, Melov SJ, McGee TM. Who is and isn’t having babies with Down syndrome in western Sydney: a ten-year hospital cohort study. Aust NZ J Obstet Gynaecol 2017;57:146–51.
Nagle C, McCarthy P, Wallace EM. Uptake of Down syndrome screening in an Australian Vietnamese population. Aust NZ J Obstet Gynaecol 2000;40:157–9.
Peters IA, Heetkamp KM, Ursem NTC, Steegers EAP, Denktas S, Knapen MFCM. Ethnicity and language proficiency differences in the provision of and intention to use prenatal screening for down’s syndrome and congenital anomalies. a prospective, non-selected, register-based study in the Netherlands. Matern child health J 2018;22:343–54.
Ahmed S, Bryant LD, Tizro Z, Shickle D. Interpretations of informed choice in antenatal screening: a cross-cultural, Q-methodology study. Soc Sci Med (1982). 2012;74:997–1004.
Gitsels-van der Wal JT, Martin L, Manniën J, Verhoeven P, Hutton EK, Reinders HS. A qualitative study on how Muslim women of Moroccan descent approach antenatal anomaly screening. Midwifery 2015;31:e43–49.
Wang H, Page R, Lopez D, Arkatkar S, Young C, Martinez D, et al. Pregnant Latinas’ views of adopting exome sequencing into newborn screening: A qualitative study. Gen Med 2022;24:1644–52.
Bet BB, Wielart L, Ravelli ACJ, van Wely M, van Leeuwen E, Pajkrt E. Financial contribution as reason to opt out of non-invasive prenatal testing. Eur J Obstet, Gynecol, Reprod Biol 2023;287:130–6.
Cheung FY, Pratt R, Shire A, Bigalke L, Ahmed Z, Zierhut H. Developing culturally informed genetic services for the Somali immigrants in Minnesota. J Genet Counsel 2019;28:887–96.
Van Elderen T, Mutlu D, Karstanje J, Passchier J, Tibben A, Duivenvoorden HJ. Turkish female immigrants’ intentions to participate in preconception carrier screening for hemoglobinopathies in the Netherlands: An empirical study. Public Health Genomics 2010;13:415–23.
Hayeems RZ, Campitelli M, Ma X, Huang T, Walker M, Guttmann A. Rates of prenatal screening across health care regions in Ontario, Canada: a retrospective cohort study. CMAJ Open 2015;3:E236–43.
Venturelli D, Lodi M, Palazzi G, Bergonzini G, Doretto G, Zini A, et al. Sickle cell disease in areas of immigration of high-risk populations: A low cost and reproducible method of screening in northern Italy. Blood Transfus 2014;12:346–51.
Macdonald W, Beeston C, McCullough S. Proportionate universalism and health inequalities. Edinburgh: NHS Health Scotland. 2014.
Fisher M, Harris P, Freeman T, Mackean T, George E, Friel S, et al. Implementing Universal and Targeted Policies for Health Equity: Lessons From Australia. Int J Health Policy Manag 2021;11:2308–18.
Cernat A, De Freitas C, Majid U, Trivedi F, Higgins C, Vanstone M. Facilitating informed choice about non-invasive prenatal testing (NIPT): a systematic review and qualitative meta-synthesis of women’s experiences. BMC Pregnancy Childbirth 2019;19:27.
Araia MH, Wilson BJ, Chakraborty P, Gall K, Honeywell C, Milburn J, et al. Factors associated with knowledge of and satisfaction with newborn screening education: a survey of mothers. Genet Med 2012;14:963–70.
Henneman L, Borry P, Chokoshvili D, Cornel MC, van El CG, Forzano F, et al. Responsible implementation of expanded carrier screening. Eur J Hum Genet. 2016;24:e1–12.
Department of Health. Victoria A. Cultural responsiveness framework - Guidelines for Victorian health services [Internet]. State Government of Victoria, Australia; 2009 [cited 2024 Oct 16]. Available from: https://www.health.vic.gov.au/publications/cultural-responsiveness-framework-guidelines-for-victorian-health-services.
Timmins GT, Wynn J, Saami AM, Espinal A, Chung WK. Diverse parental perspectives of the social and educational needs for expanding newborn screening through genomic sequencing. Public Health Genomics. 2022;25:185–92.
Vanstone M, Cernat A, Majid U, Trivedi F, De Freitas C. Perspectives of pregnant people and clinicians on noninvasive prenatal testing: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser 2019;19:1–38.
Van Steijvoort E, Chokoshvili D, W Cannon J, Peeters H, Peeraer K, Matthijs G, et al. Interest in expanded carrier screening among individuals and couples in the general population: systematic review of the literature. Hum Reprod Update 2020;26:335–55.
Ramdaney A, Lichten L, Propst L, Mann C, Lazarin GA, Jones M, et al. Expanded carrier screening in the United States: A systematic evidence review exploring client and provider experiences. J Genet Counsel 2022;31:937–48.
Dove ES, Kelly SE, Lucivero F, Machirori M, Dheensa S, Prainsack B. Beyond individualism: Is there a place for relational autonomy in clinical practice and research? Clin Ethics 2017;12:150–65.
Lawson KL, Pierson RA. Maternal decisions regarding prenatal diagnosis: rational choices or sensible decisions? J Obstet Gynaecol Can 2007;29:240–6.
Samuel GN, Dheensa S, Farsides B, Fenwick A, Lucassen A. Healthcare professionals’ and patients’ perspectives on consent to clinical genetic testing: moving towards a more relational approach. BMC Med Ethics 2017;18:47.
Entwistle VA, Carter SM, Cribb A, McCaffery K. Supporting patient autonomy: the importance of clinician-patient relationships. J Gen Intern Med 2010;25:741–5.
Dive L, Newson AJ. Reconceptualizing autonomy for bioethics. Kennedy Inst Ethics J 2018;28:171–203.
Hodgson J, Spriggs M. A practical account of autonomy: why genetic counseling is especially well suited to the facilitation of informed autonomous decision making. J Genet Counseling 2005;14:89–97.
Ahmed S, Yi H, Dong D, Zhu J, Jafri H, Rashid Y, et al. Interpretations of autonomous decision-making in antenatal genetic screening among women in China, Hong Kong and Pakistan. Eur J Hum Genet 2018;26:495–504.
van den Heuvel A, Chitty L, Dormandy E, Newson A, Attwood S, Ma R, et al. Is informed choice in prenatal testing universally valued? A population-based survey in Europe and Asia. BJOG 2009;116:880–5.
Acknowledgements
The authors thank Poh Chua, the medical librarian, for her assistance with the literature search strategy.
Funding
This research was supported by the Victorian Government's Operational Infrastructure Support Program, the Australian Government Research Training Program Scholarship, and the University of Melbourne Master of Genetic Counselling PhD award. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
AK conceptualised the review; led the literature search, screening, extraction, and analysis; and prepared manuscript drafts and revisions. ET contributed to screening and draft revisions. AA, LB, SL, and BM contributed to conceptualisation of the review, project supervision, analysis, and draft revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kanga-Parabia, A., Archibald, A.D., Biggs, L.J. et al. Experiences of perinatal genetic screening for people from migrant and refugee backgrounds: a scoping review. Eur J Hum Genet 33, 701–710 (2025). https://doi.org/10.1038/s41431-024-01748-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-024-01748-y
This article is cited by
-
What’s new in EJHG in May 2025?
European Journal of Human Genetics (2025)