Abstract
ApoA-I amyloidosis is an extremely rare form of systemic amyloidosis that commonly involves the heart, kidneys, and liver. ApoA-I amyloidosis is caused by amyloidogenic variants of APOA1 that are inherited in an autosomal dominant manner. Here, we report a 69-year-old man with sporadic cardiac amyloidosis who was born to consanguineous parents and carried a homozygous variant of p.Leu202Arg in APOA1.
Similar content being viewed by others
Amyloidosis is a group of diseases caused by the extracellular deposition of insoluble amyloid fibrils in various tissues and organs, including the heart, nerves, kidneys, and ligaments1. Hereditary amyloidosis is caused by genetic variants in amyloid precursor proteins, such as transthyretin (TTR) and apolipoprotein A-I (ApoA-I)2. ApoA-I amyloidosis is a rare autosomal dominant disorder, with more than 20 reported variants3,4. Here, we report a patient with cardiac ApoA-I amyloidosis who carried a homozygous variant of p.Leu202Arg in APOA1.
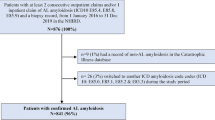
The patient was a 69-year-old man who was born to consanguineous parents and had no family history of heart disease. At 52 years of age, he developed dyspnea and edema in his extremities. A 12-lead electrocardiogram revealed a left bundle block and a first-degree atrioventricular block with low voltage. Echocardiography revealed a normal left ventricular (LV) diameter with a reduced ejection fraction of 46% and severe diffuse hypertrophy. Although diuretic therapy at age 53 temporarily relieved his symptoms, he was admitted to the hospital for the recurrence of heart failure (HF). On the basis of echocardiographic findings, cardiac amyloidosis was suspected; however, biopsy samples from the endocardium and gastrointestinal tract did not demonstrate amyloid deposition. At the age of 57 years, he underwent cavotricuspid isthmus ablation for an atrial flutter that triggered an HF relapse. At 58 years of age, he developed a complete atrioventricular block, and an implantable cardiac resynchronization therapy pacemaker was implanted. Over the subsequent years, the patient experienced multiple hospitalizations for recurrent HF. At 67 years of age, he presented to our hospital for further examination for HF.
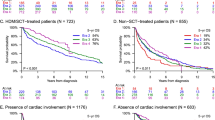
A 12-lead electrocardiogram revealed a biventricular pacing rhythm. Chest radiography revealed cardiomegaly and lung congestion (Fig. 1a). Cardiac scintigraphy with technetium pyrophosphate (99mTc-PYP) showed strong intensity in the myocardial region, with a heart-to-contralateral ratio of 2.0 (Fig. 1b). Echocardiography revealed a slightly enlarged LV diastolic diameter of 55 mm with a reduced ejection fraction of 40% and severe LV diffuse hypertrophy (interventricular septum thickness, 13 mm) accompanied by apical sparing of the longitudinal strain (Fig. 1c, d). Congo red staining of biopsy samples from the right ventricle revealed abundant amyloid deposits (Fig. 1e). Immunohistochemistry revealed no deposition of TTR or immunoglobulin light chain. Blood tests revealed slightly increased B-type natriuretic peptide (BNP, 154 pg/mL) and troponin I (31 pg/ml) levels. Monoclonal gammopathy was not detected. ApoA-I levels were normal (121 mg/dl), but HDL cholesterol (HDL-C) levels were decreased (35 mg/dL). Serum liver enzyme and creatine levels were within the normal range; albuminuria was not detected. A nerve conduction study revealed mild sensory polyneuropathy, which was compatible with amyloid neuropathy.
a Chest radiography image. b Cardiac scintigraphy with technetium pyrophosphate image. c Echocardiography image, long-axis view. d Echocardiography image, longitudinal strain. e Pathological images of Congo red staining of cardiac samples. f Image of immunohistochemistry with ApoA-I antibody. g List of proteins detected using laser microdissection‒liquid chromatography‒tandem mass spectrometry analysis of cardiac samples. The most abundant peptide was derived from ApoA-I.
We then performed laser microdissection‒liquid chromatography‒tandem mass spectrometry (LMD‒LC‒MS/MS) analysis to identify amyloidogenic proteins from formalin-fixed, paraffin-embedded cardiac tissue sections, as previously described4,5. The most abundant peptide was derived from ApoA-I (Fig. 1g); this result was confirmed by immunohistochemistry with an ApoA-I antibody (Fig. 1f).
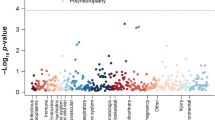
Sanger sequencing of APOA1 revealed that the patient had a homozygous variant of NM_000039.3:c.605 T > G, p.Leu202Arg (corresponding to p.Leu178Arg when excluding the signal peptide and propeptide) (Fig. 2a). p.Leu202 is located in the N-terminal region of ApoA-I and is highly conserved among species. The variant was classified as likely pathogenic (PP3 + PM1 + PM2 + PM5) according to the American College of Medical Genetics and Genomics (ACMG) classification. Multiple protein prediction algorithms indicated that this variant was damaging, with a CADD Phred score of 29.4. Moreover, several single-point variants were identified in N-terminal residues 194–202 of the protein6; previously, a different missense variant at this site, p.Leu202His, was determined to be pathogenic7,8. The patient’s older brother was heterozygous for the variant, whereas his older sister did not harbor it (Fig. 2b). Genetic testing was not performed for the other family members. The older brother showed no abnormal findings on electrocardiogram or echocardiography. Blood test results revealed normal BNP (25 pg/mL), slightly increased ApoA-I (158 mg/dl), and normal HDL-C (44 mg/dL) levels. Similarly, his older sister, who had a history of rheumatic arthritis, had normal electrocardiogram and echocardiography findings. Blood tests revealed normal levels of BNP (18 pg/mL) and increased ApoA-I (209 mg/dl) and HDL-C (93 mg/dL) levels.
The patient continued diuretic treatment (40 mg of furosemide and 8 mg of torsemide) and achieved a stable disease course with a New York Heart Association functional classification II.
Hereditary amyloidosis comprises more than 30 subtypes, including TTR, ApoA-I, ApoA-II, gelsolin, lysozyme amyloidosis, cystatin C amyloidosis (ACys), fibrinogen Aα-chain, β2-microglobulin, ApoC2-II, and ApoC39. Each subtype involves a different precursor protein and exhibits significantly varied clinical presentation. ApoA-I amyloidosis is an extremely rare form of systemic amyloidosis that commonly involves the kidneys, heart, and liver1. Genetically, ApoA-I amyloidosis is caused by amyloidogenic variants of APOA1 inherited in an autosomal dominant fashion. After identification of the p.Gly50Arg variant in 199010, more than 20 causative variants have been identified11. A basic study revealed that the ApoA-I N-terminal fragment is strongly associated with amyloid fibril formation, leading to systemic amyloidosis12. The majority of amyloidogenic mutations are located in two hotspot regions: the N-terminal region containing amino acid residues 50-131 and the C-terminal region containing amino acid residues 178-202 (corresponding to amino acids 26-107 and 154-178, respectively, when excluding the signal peptide and propeptide)1. Amyloid fibrils isolated ex vivo were found to be composed mainly of N-terminal fragments of ApoAI with lengths of 80–100 residues. N-terminal fragments of ApoAI enhance the formation of fibrils containing ApoAI fragments with lengths of 1–83 residues. On the other hand, the amyloid fibrils extracted from patients with C-terminal variants were composed mainly of fragments with lengths of 1–93 residues. Amyloidogenic mutations in the N-terminal region may increase protein flexibility in proximity to the putative cleavage site, releasing the N-terminal amyloidogenic ___domain1.
In addition, a biochemical study of the p.Leu202His variant, which occurs at the same amino acid position as the variant in this patient, demonstrated an increase in α-helical content but not β-strand content, accompanied by the formation of very short fibrils11. These biochemical properties are different from those observed in the classical variant p.Gly50Arg. The exact mechanisms by which the same phenotype develops from different genetic variants have not been fully elucidated. The amyloidogenic phenotype is related to altered structural features, including protein conformation and lipid binding, protein flexibility and stability, susceptibility to proteases, and aggregation propensity1. Variants in the N-terminal region frequently involve the kidney and liver, whereas those in the C-terminal region lead to cardiac, laryngeal, and cutaneous symptoms6. The difference in the structural properties of amyloid fibrils from different genotypic regions may also affect the phenotype.
For the patient in this study, the clinical picture and results of biochemical analysis were compatible with those of ApoA-I amyloidosis; however, the patient unexpectedly harbored a homozygous pathogenic variant, p.Leu202Arg, in the APOA1 gene. Moreover, his older brother, who had a heterozygous p.Leu202Arg variant, did not exhibit amyloidosis-related symptoms at the age of 75 years. Generally, ApoA-I amyloidosis exhibits age-dependent penetrance. A survey of the p.Leu99Pro variant revealed that its penetrance was 38% at 60 years of age and 98.7% at 80 years of age or older13. Moreover, disease penetrance might be associated with the variant and the resulting amino acid substitution6. The incomplete and age-dependent penetrance of the APOA1 variant could account for the presence of unaffected family members, especially the heterozygous older brother. Importantly, the proband inherited the disease in an apparent autosomal recessive manner, although ApoA-I amyloidosis is known to be an autosomal dominant disorder. Furthermore, there have been no reported cases of homozygous amyloidogenic APOA1 variants. We speculate that the heterozygous p.Leu202Arg variant might have only a “weak” effect on amyloidogenesis and that the biallelic variant might be a prerequisite for symptom manifestation.
The p.Leu202Arg variant reported here causes an amino acid substitution in the C-terminal region. The region in which the amyloidogenic variant is located may be responsible for the genotypic differences. However, although we showed that the accumulant was derived from the ApoA1 protein, the biochemical characteristics of the accumulant and the pathophysiology of its accumulation remain unknown. Structural analysis of the protein produced by the mutant and studies using experimental animals are necessary to elucidate this pathophysiology in the future.
ApoA-I is the main apolipoprotein among plasma high-density lipoproteins (HDLs) with well-documented cardioprotective functions3. The reverse transport of cholesterol from peripheral tissues to the liver for excretion by promoting cholesterol efflux from tissues is a pivotal pathway and acts as a cofactor for lecithin cholesterol acyltransferase (LCAT). APOA1 knockout mice presented normal HDL levels but altered HDL composition. Moreover, compared with control mice, knockout mice presented higher levels of triglycerides and free cholesterol and lower levels of cholesteryl ester (CE), suggesting that ApoA-I-deficient HDL is a poor substrate for hepatic lipase and LCAT, which may lead to decreased levels of HDL-C14. Patients with ApoA-I amyloidosis are reported to have decreased serum HDL-C and ApoA-I levels15,16. In our patient, the HDL-C level decreased, whereas his older brother with a heterozygous variant had normal HDL-C levels. This finding further suggests the additive effect of the biallelic p.Leu202Arg variant, which may reduce the function of ApoA-I and eventually decrease the level of HDL-C.
A noninvasive diagnostic criterion for cardiac TTR amyloidosis is applicable to most patients with amyloidosis17. If the results of bone scintigraphy with bisphosphonate are grade 2 or 3 with no monoclonal gammopathy, cardiac TTR amyloidosis can be diagnosed with > 99% sensitivity and 86% specificity. Although our patient met these criteria (grade 3 according to 99mTc-PYP scintigraphy and no monoclonal gammopathy), he was finally diagnosed with ApoA-I amyloidosis using LMD–LC‒MS/MS and genetic testing. The present case reaffirms the reduced specificity of nonbiopsy diagnostic criteria and the importance of biopsies for diagnosing TTR amyloidosis2. Moreover, this case also suggests that when immunohistochemistry results indicate a diagnosis other than TTR, LMD–LC‒MS/MS coupled with targeted gene sequencing can efficiently confirm an etiological diagnosis, even in the absence of a family history.
Currently, amyloid production or deposition in hereditary ApoA-I amyloidosis cannot be suppressed using any established treatment. Therefore, treatment exclusively focuses on relieving the symptoms of organ damage, such as the use of diuretics in patients with HF1. Although disease progression in ApoA-I amyloidosis is usually slow, its management often becomes very difficult once cardiac symptoms fully manifest. ApoA-I amyloidosis is extremely rare; therefore, it is not routinely included in the differential diagnosis of systemic amyloidosis18 and largely remains unexplored. Thus, the genotype‒phenotype correlation in ApoA-I amyloidosis needs to be further delineated to facilitate early diagnosis, effective genetic counseling, and risk stratification of pathogenic variant carriers.
HGV Database
The relevant data from this Data Report are hosted at the Human Genome Variation Database at https://doi.org/10.6084/m9.figshare.hgv.3416.
References
Arciello, A., Piccoli, R. & Monti, D. M. Apolipoprotein A-I: the dual face of a protein. FEBS Lett. 590, 4171–4179 (2016).
Kitaoka, H. et al. JCS 2020 guideline on diagnosis and treatment of cardiac amyloidosis. Circ. J. 84, 1610–1671 (2020).
Joy, T., Wang, J., Hahn, A. & Hegele, R. A. Apoa1 related amyloidosis: a case report and literature review. Clin. Biochem. 36, 641–645 (2003).
Tasaki, M. et al. Apolipoprotein AI amyloid deposits in the ligamentum flavum in patients with lumbar spinal canal stenosis. Amyloid 28, 107–112 (2021).
Tasaki, M. et al. A novel age-related venous amyloidosis derived from EGF-containing fibulin-like extracellular matrix protein 1. J. Pathol. 247, 444–455 (2019).
Tougaard, B. G. et al. A case report of hereditary apolipoprotein A-I amyloidosis associated with a novel APOA1 mutation and variable phenotype. Eur. J. Med Genet 59, 474–477 (2016).
de Sousa, M. M. et al. Apolipoprotein AI and transthyretin as components of amyloid fibrils in a kindred with apoAI Leu178His amyloidosis. Am. J. Pathol. 156, 1911–1917 (2000).
Hazenberg, A. J. C. et al. Laryngeal presentation of systemic apolipoprotein A-I-derived amyloidosis. Laryngoscope 119, 608–615 (2009).
Sipe, J. D. et al. Amyloid fibril proteins and amyloidosis: chemical identification and clinical classification International Society of Amyloidosis 2016 Nomenclature Guidelines. Amyloid 23, 209–213 (2016).
Nichols, W. C., Gregg, R. E., Brewer, H. B. & Benson, M. D. A mutation in apolipoprotein A-I in the Iowa type of familial amyloidotic polyneuropathy. Genomics 8, 318–323 (1990).
Petrlova, J. et al. The fibrillogenic L178H variant of apolipoprotein A-I forms helical fibrils. J. Lipid Res. 53, 390–398 (2012). Mar.
Mizuguchi, C. et al. Mechanisms of aggregation and fibril formation of the amyloidogenic N-terminal fragment of apolipoprotein A-I. J. Biol. Chem. 294, 13515–13524 (2019).
Gregorini, G. et al. Tubulointerstitial nephritis is a dominant feature of hereditary apolipoprotein A-I amyloidosis. Kidney Int. 87, 1223–1229 (2015).
Plump, A. S. et al. ApoA-I knockout mice: characterization of HDL metabolism in homozygotes and identification of a post-RNA mechanism of apoA-I up-regulation in heterozygotes. J. Lipid Res. 38, 1033–1047 (1997).
Gomaraschi, M. et al. Effect of the amyloidogenic L75P apolipoprotein A-I variant on HDL subpopulations. Clin. Chim. Acta 412, 1262–1265 (2011).
Obici, L. et al. Structure, function and amyloidogenic propensity of apolipoprotein A-I. Amyloid 13, 191–205 (2006).
Gillmore, J. D. et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation 133, 2404–2412 (2016).
Lachmann, H. J. et al. Misdiagnosis of hereditary amyloidosis as AL (Primary) amyloidosis. N. Engl. J. Med 346, 1786–1791 (2002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yagi, S., Miyamoto, R., Tasaki, M. et al. The APOA1 p.Leu202Arg variant potentially causes autosomal recessive cardiac amyloidosis. Hum Genome Var 11, 30 (2024). https://doi.org/10.1038/s41439-024-00288-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41439-024-00288-7