Abstract
This study evaluated the impact of ventricular rate (VR) in atrial fibrillation (AF) patients with oscillometric BP measurements. This study included 138 patients with AF and 112 patients with sinus rhythm (SR) who underwent coronary angiography. Left arm BP was measured three times with an oscillometric device, and the average was recorded as the final oscillometric value. At the same time, the average of three intra-aortic BP readings was used as invasive values. Delta BP was the difference between intra-aortic and oscillometric BP. Meanwhile, the BP percentage difference (PD-BP) was calculated with the following formula: PD-BP = (delta BP/intra-aortic BP) × 100%. Based on the VR, four subgroups of AF and SR patients, <80, 80–99, 100–120, and >120 bpm, were created, and the mean PD-BP for both systolic blood pressure (SBP) and diastolic blood pressure (DBP) was significantly higher in the AF group than in the SR group. Moreover, the mean PD-SBP values gradually increased as VR increased in both groups. More importantly, the difference in PD-SBP between the AF and SR groups increased as VR increased: when VR was <80 bpm, the levels were similar (−2.0 ± 3.5 vs. −1.4 ± 2.7 mm Hg, NS), but these values in AF patients were significantly higher when VR was 80–99 bpm (−3.7 ± 5.0 vs. −1.8 ± 2.3 mm Hg, p < 0.05), 100–120 bpm (−6.1 ± 4.3 vs. −2.3 ± 1.9 mm Hg, p < 0.05) and >120 bpm (−7.8 ± 4.9 vs. −2.9 ± 1.7 mm Hg, p < 0.05). The accuracy of oscillometric BP measurements are dependent on the ventricular rate in AF patients even after three measurements, and a higher ventricular rate may result in larger underestimations of oscillometric BP.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common supraventricular arrhythmia, which results in serious clinical complications and considerable medical expenses. Meanwhile, hypertension (HT) is the most common risk factor for AF. Epidemiology shows that the incidence of HT complicated with AF is gradually increasing in the older population. Therefore, accurately measuring BP is important for AF patients.
At present, oscillometric BP measuring devices are widely used in offices and at home. However, the accuracy of this method in AF patients remains controversial, because it was developed from subjects with a regular heart rate [1,2,3,4,5,6,7].
Previously, sphygmomanometry has been used in most studies as a reference technique to assess the accuracy of oscillometric BP measurement in AF patients. However, the various stroke volumes in AF may cause beat-to-beat differences in pulse pressure. As a result, the Korotkoff sounds are unstable, and the accuracy of sphygmomanometry measurements decrease. Therefore, to validate the accuracy of the oscillometric BP method, intra-arterial BP is the gold reference.
Using intraradial arterial BP as a reference, Pagonas et al. [2] in 2013 suggested that AF did not significantly decrease the accuracy of oscillometric BP measurement when the average of three consecutive BP readings was used. However, some studies have indicated that ventricular rate (VR) was associated with the accuracy of oscillometric BP measurement in AF patients. For example, Giantin et al. [8] found that in patients with stable AF (with VR of 60–100 beats per minute, bpm), the BP value from ambulatory blood pressure monitoring (ABPM) was similar to that of patients with sinus rhythm (SR), but when VR was >100 bpm, the stability of ABPM was poor. Recently, Wang’s study found that when the mean pulse rate is over 100 bpm, the accuracy of oscillometric systolic blood pressure (SBP) may be impaired [9]. However, these findings were not from an analysis using intra-arterial BP as a reference.
Although intraradial arterial BP was used as a reference in the Pagonas study, unfortunately, the study did not evaluate the association between VR and accuracy of oscillometric BP. In fact, the range of VR among AF patients is wide. Meanwhile, a rapid VR is often associated with VR irregularity; therefore, it is important to evaluate the impact of VR on the accuracy of oscillometric BP measurements in AF patients. This prospective study used the intra-aortic BP as a reference standard to evaluate whether the VR levels have an impact on the accuracy of oscillometric BP measurement in AF patients.
Methods
The proposal and consent procedures for this study were approved by the ethics committee of the Second Affiliated Hospital of Nanchang University. All patients provided written informed consent for participation.
Study population
Our cross-sectional study included 250 patients (male: 152) from our hospital from January 2016 to December 2018. Among them, 112 patients (44.8%) had SR, and 138 patients (55.2%) suffered from persistent AF. All the patients were scheduled to undergo coronary angiography by radial artery.
The exclusion criteria included acute myocardial infarction, acute heart failure, coarctation of the aorta, congenital heart disease, hemodynamic instability and coma, hemiplegia, and pulseless disease.
Oscillometric BP measurements
The oscillometric BP measurement was performed in the cardiac catheterization room with a validated automated oscillometric upper arm device (Omron HEM-7130,Omron Healthcare Co. Ltd, Kyoto, Japan) [10]. First, a standard cuff (12 × 22 cm) was placed on the left upper arm, and then the arm was placed at the same high level as the heart. Therefore, the participants with arm circumferences over 26 cm were excluded. BP was measured when the patients were awake in a supine position.
BP was measured three times at one-minute intervals, and the average was used as the final noninvasive BP value [11].
Invasive BP measurement
In coronary angiography (Philips Allura Xper FD20, Holland), a catheter (6 Fr, Medtronic or Cordis) was located in the ascending aorta root to continuously record the intra-aortic BP. Adjustment to atmospheric zero was performed before initiation of each measurement procedure by opening the transducer to atmospheric pressure. The intra-aortic BP, simultaneously performed with the oscillometric BP measurement, was recorded for 10–15 VR each time. The average of three intra-aortic BP recordings was used as the final intra-aortic BP value, which was the mean value of 30–45 heart beats.
Based on the mean VR on electrocardiography (ECG) at the time of the intra-aortic BP recording, the patients in both the AF and SR groups were divided into four subgroups: <80 bpm; 80–99 bpm; 100–120 bpm, and >120 bpm.
A parameter, delta BP, was calculated based on the difference between the intra-aortic BP and the oscillometric BP. To attenuate the impact of intra-aortic levels on the delta BP, another parameter, the percentage difference in BP (PD-BP) was calculated with the formula: PD-BP = delta BP/intra-aortic BP × 100% [12].
The linear relationship between the oscillometric BP and the intra-aortic BP was evaluated. Meanwhile, their agreement was also evaluated by the Bland–Altman method [13]. For the Bland–Altman analysis, intermeasurement differences were plotted against their means, and the 95% limits of agreement (LoA) were determined (95% LoA = mean intermeasurement difference ± 1.96 standard deviation (SD)).
Statistical analysis
SPSS statistical software version 21.0 (SPSS for Windows, Chicago, SPSS Inc.) was used to collect and analyze data. Data are presented as the means ± SD. All demographic data were analyzed by frequency tests, and the continuous data were analyzed by frequency cross tabulation and chi-square tests. The comparison of numeric BP values was performed by paired two-tailed t-tests. A Bland–Altman scatter plot was used to analyze the agreement between the noninvasive BP and the intra-aortic BP. The limit of significance was determined at p < 0.05.
Results
The baseline characteristics of the two groups are shown in Table 1. In this study, 112 SR patients were selected to match the VR levels of the AF patients (92.8 ± 19.4 vs. 96.7 ± 20.2 bpm). The sex and smoking habits were similar between the two groups, but the age in the AF group was higher than that in the SR group. There was no difference in the incidence of hypertension, hyperlipidemia, previous stroke, diabetes mellitus, and chronic kidney disease. However, coronary heart disease and congestive heart failure were significantly more prevalent in the AF patients (p < 0.05).
Comparison of intra-aortic BP with oscillometric BP
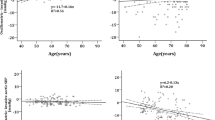
For the 138 AF patients, the oscillometric SBP and diastolic blood pressure (DBP) values were significantly lower than the intra-aortic SBP and DBP values, but in the SR patients, the oscillometric SBP and DBP values were similar to the intra-aortic values (Table 2). Meanwhile, the delta BP and the PD-BP for both SBP and DBP were significantly higher in the AF group than in the SR group (Fig. 1).
Figure 2 shows that a positive linear relationship exists between intra-aortic BP and oscillometric BP in the AF or SR patients, but the relationship was weaker in the AF than in the SR patients.
Meanwhile, the mean difference and the 95% limits were larger in the AF group than in the SR group. For SBP, the mean difference was −6.2 mm Hg vs. −2.9 mm Hg, and the 95% limits were 6.7 to –18.9 mm Hg vs. 3.4 to −15.3 mm Hg, respectively. For DBP, these values were −2.9 mm Hg vs. −2.3 mm Hg and 3.4 to −9.1 mm Hg vs. 5.0 to −9.6 mm Hg, respectively (Fig. 2).
In the AF subgroup of men with VR < 80 bpm, no significant differences were found between the oscillometric BP and intra-aortic BP, either for SBP or DBP. In this situation, the absolute delta BP and PD-BP were similar between the SR and AF subgroups. On the other hand, when the mean VR ≥ 80 bpm, the absolute delta BP and PD-BP for both SBP and DBP increased as the mean VR increased in the AF patients.
In the SR patients, the PD-SBP did not statistically increase as the mean VR increased. Although no significant differences in PD-DBP were observed in the SR <80, 80–99, and 100–120 bpm subgroups, the PD-DBP in the >120 bpm subgroup was significantly higher than in the other subgroups (Table 3).
The agreement between intra-aortic BP and oscillometric BP
When VR < 80 bpm, the SBP difference was −2.9 vs. −2.1 mm Hg with a 95% limit of −6.0 to 11.7 vs. −5.0 to 9.3 mm Hg for the oscillometric and intra-aortic BP measurements, respectively, a similar result was found for the DBP difference: −2.9 vs. −1.5 mm Hg with a 95% limit of 4.2 to −10.0 vs. 5.5 to −8.6 mm Hg. When VR ≥ 80 bpm, the SBP difference and the 95% limits increased as the VR increased in AF patients. The SBP difference in the 80–99, 100–120, and >120 subgroups gradually increased to −5.4, −8.5, and 10.3 mm Hg, respectively, and the corresponding 95% limits increased to 8.2 to −19.0, 3.2 to −20.0, and 2.9 to −23.4 mm Hg. In SR patients, however, these values were −2.7, −3.2, and −4.4 mm Hg, and the 95% limits were 3.7 to −9.1; 2.2 to −8.6 and 0.6 to −9.5 mm Hg, respectively. Similar results were found for DBP values (Table 3 and Fig. 3).
Discussion
Patients with both AF and HT are common, as HT is a common underlying disorder in AF patients [14]. Therefore, an accurate BP measurement is important. Although Pagonas et al. [2] found that AF did not significantly decrease the accuracy in oscillometric BP measurements when the average of three BP readings were used, they also pointed out that AF significantly increased the interindividual variability in oscillometric BP measurements. Recently, Dąbrowski’s research showed that AF did not affect ankle-brachial index (ABI) measurements [15].
However, some clinical studies have indicated that the rapid VR in AF may affect the accuracy of oscillometric BP measurements, but no evidence was related to intra-aortic BP [8]. Therefore, the present study used intra-aortic BP as a reference to evaluate the impact of VR on the accuracy of oscillometric BP monitoring based on AHA recommendations [16].
First, our study found that even using the average of three BP readings, AF could generally impact the accuracy of oscillometric BP because the delta BP, as well as the PD-BP, for both SBP and DBP, were significantly higher in the AF patients than in the SR patients. Meanwhile, the Bland–Altman analysis also showed that the 95% limits for SBP or DBP were larger in the AF group. Our finding is different from that of Pagonas et al. The first reason may be the different population: in the present study, they were coronary angiography patients, while in the Pagonas study, they were intensive or intermediate care patients; furthermore, the sample of AF patients in our study was larger than the Pagonas study (138 cases vs. 50 cases). The second reason may be that the reference was different: intra-aortic BP in our study and intraradial arterial BP in the Pagonas study. It is suggested that intra-aortic BP may be more stable and could better reflect the heart load.
Second, our study demonstrated for the first time that the impact of AF on the accuracy of oscillometric BP measurements is dependent on the VR levels. When the VR is <80 bpm, AF does not significantly impact the accuracy of oscillometric BP measurements; otherwise, the impact becomes more obvious as the mean VR increases. In the SR group, no significant association was found between the HR levels and the delta BP.
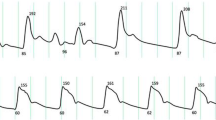
We suggest that the underlying mechanism of this VR-dependent relationship is the more obvious irregularity of ventricular beats when the VR is rapid. Using an oscillometric BP device (CB-1805-B 24 BP monitor, BIOX Devices Co, Ltd, Wuxi, China), which could provide the record of the oscillometric pressure pulses, we found that the shape of the oscillometric pressure pulses was dependent on the VR levels. A characteristic shape in SR is a spindle, which is the basis for oscillometric BP measurement. The shape is close to a spindle in AF patients with VR <80 bpm, but the shape becomes far from a spindle as the VR increases (Supplementary Data). Therefore, the increased VR in AF patients certainly induces a larger bias in the BP readings. This finding also provides evidence for the higher variability in subjects with AF. In this study, only 35 (25.4%) AF patients had VR <80 bpm; thus, we consider that most AF patients may face a problem of inaccurate oscillometric BP measurement in clinical practice.
Third, the baseline characteristics between the AF and SR groups were generally comparable. Although the VR levels were slightly higher in the AF group than in the SR group (96.7 ± 20.2 vs. 92.8 ± 19.4 bpm), this difference was small. Thus, AF itself may be responsible for the lower accuracy of oscillometric BP measurement.
In this study, the mean oscillometric SBP and DBP levels were lower than the intra-aortic SBP and DBP by 2–3 mm Hg in the SR group. This result was similar to that reported by a meta-analysis, which showed a small mean difference (0.3 mm Hg; 95% CI: −1.5 to 2.1 mm Hg; p = 0.77) between cuff SBP and intra-aortic SBP [17]. However, the oscillometric SBP was 6 mm Hg and DBP was 5 mm Hg lower than the intra-aortic BP. More importantly, this underestimation became more obvious as the VR increased in AF. As the same technique and equipment were used in both the AF and SR groups, even if there may be some systematic bias, we could conclude that AF itself may impair the accuracy of oscillometric SBP and DBP measurements, especially in subjects with rapid VR.
Clinical implications
Our study demonstrated for the first time that in AF patients, the accuracy of oscillometric BP measurement is dependent on the VR levels. It is known that exercise or emotional stress may increase VR [12]. In this situation, the oscillometric BP may not be as accurate at rest. As the target VR suggested by the 2016 ESC guidelines for AF management is <110 bpm [18], based on our data, the oscillometric SBP in VR at 110 bpm may be underestimated by approximately a mean of 10 and 8 mm Hg against the intra-aortic SBP and DBP. This information should be taken into the doctor’s consideration when treating AF patients.
Although repeated BP measurements are presently suggested for obtaining a relatively reliable BP reading in AF patients, developing a more accurate BP method for AF patients is necessary in the future.
Limitations
In this study, the mean age of the AF group was higher than that of the SR group but this difference did not influence our conclusion, as the analysis showed a similar result when the two groups had a similar mean age through an age-matching method.
The studied patients were middle-aged to elderly individuals, were there for coronary angiography, and had relatively stable hemodynamics, and the software for automatic BP detection might differ among various oscillometric devices. The values of the BP differences may be somewhat different in other populations or when using other oscillometric devices [19].
Conclusion
The accuracy of oscillometric BP measurement is dependent on the ventricular rate in AF patients even when the average of three BP readings is used, and the higher ventricular rate may result in a larger underestimation of oscillometric BP.
References
Stergiou GS, Kollias A, Destounis A, Tzamouranis D. Automated blood pressure measurement in atrial fibrillation: a systematic review and meta-analysis. J Hypertens. 2012;30:2074–82.
Pagonas N, Schmidt S, Eysel J, Compton F, Hoffmann C, Seibert F, et al. Impact of atrial fibrillation on the accuracy of oscillometric blood pressure monitoring. Hypertension. 2013;62:579–84.
Kollias A, Stergiou GS. Automated measurement of office, home and ambulatory blood pressure in atrial fibrillation. Clin Exp Pharm Physiol. 2014;41:9–15.
Maselli M, Giantin V, Corrado D, Franchin A, Attanasio F, Pengo V, et al. Reliability of oscillometric blood pressure monitoring in atrial fibrillation patients admitted for electric cardioversion. J Clin Hypertens (Greenwich). 2015;17:558–64.
Alpert BS, Quinn D, Gallick D. Oscillometric blood pressure: a review for clinicians. J Am Soc Hypertens. 2014;8:930–8.
Stergiou GS, Kollias A, Karpettas N. Does atrial fibrillation affect the automated oscillometric blood pressure measurement? Hypertension. 2013;62:e37.
Myers MG, Stergiou GS. Should oscillometric blood pressure monitors be used in patients with atrial fibrillation? J Clin Hypertens (Greenwich). 2015;17:565–6.
Giantin V, Perissinotto E, Franchin A, Baccaglini K, Attanasio F, Maselli M, et al. Ambulatory blood pressure monitoring in elderly patients with chronic atrial fibrillation: is it absolutely contraindicated or a useful tool in clinical practice and research? Hypertens Res. 2013;36:889–94.
Wang XX, Shuai W, Hong K, Li P, Cheng XS, Su H, et al. How to evaluate BP measurements using the oscillometric method in atrial fibrillation: the value of pulse rate variation. Hypertens Res. 2016;39:588–92.
Takahashi H, Yoshika M, Yokoi T. Validation of three automatic devices for the self-measurement of blood pressure according to the European Society of Hypertension International Protocol revision 2010: the Omron HEM-7130, HEM-7320F, and HEM-7500F[J]. Blood Press Monit. 2015;20:92–7.
Dart RA, Alpert B, Quinn D. Effect of mechanical behavior of the brachial artery on blood pressure measurement during cuff inflation and cuff deflation[J]. Blood Press Monit. 2014;19:120.
Luo X, Xiong Q, Xu J, Hong K, Li J, Su H, et al. Differences in heart rate response and recovery after 6-minute walking test between patients with atrial fibrillation and in sinus rhythm. Am J Cardiol. 2018;122:592–6.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Badheka AO, Patel NJ, Grover PM, Shah N, Patel N, Mitrani RD, et al. Optimal blood pressure in patients with atrial fibrillation (from the AFFIRM Trial). Am J Cardiol. 2014;114:727–36.
Dąbrowski M, Lewandowski J, Abramczyk P, Łoń I, Gaciong Z, Siński M. Atrial fibrillation does not affect ankle-brachial index measured using the Doppler method. Hypertens Res. 2018;41:60–5.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: a statement for professionals from the subcommittee of professional and public education of the American Heart Association council on high blood pressure research. Hypertension. 2005;45:142–61.
Picone DS, Schultz MG, Otahal P, Aakhus S, Al-Jumaily AM, Black JA, et al. Accuracy of CUff-measured Blood Pressure: Systematic Reviews And Meta-analyses. J Am Coll Cardiol. 2017;70:572–86.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Vardas P, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;2893–962.
Raamat R, Talts J, Jagomägi K, Kivastik J. Accuracy of some algorithms to determine the oscillometric mean arterial pressure: a theoretical study. Blood Press Monit. 2013;18:50–6.
Acknowledgements
We appreciate all the participants and their relatives in the study and the members of the survey teams in the Second Affiliated Hospital of Nanchang University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Xie, F., Xu, J., Xia, Ll. et al. The impact of atrial fibrillation on accuracy of oscillometric blood pressure measurement: effect of ventricular rate. Hypertens Res 43, 518–524 (2020). https://doi.org/10.1038/s41440-019-0386-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0386-4
Keywords
This article is cited by
-
Exploring the link between blood pressure variability and atrial fibrillation: current insights and future directions
Journal of Human Hypertension (2024)
-
Accuracy of oscillometric-based blood pressure monitoring devices: impact of pulse volume, arrhythmia, and respiratory artifact
Journal of Human Hypertension (2023)
-
Home blood pressure monitoring: a position statement from the Korean Society of Hypertension Home Blood Pressure Forum
Clinical Hypertension (2022)
-
Accuracy of non-invasive blood pressure measurement in patients with atrial fibrillation
Journal of Human Hypertension (2022)
-
Validation of an ambulatory blood pressure monitoring device employing a novel method to detect atrial fibrillation
Hypertension Research (2022)