Abstract
The percentage of people aged 80 years or older in Japan has been increasing. The purpose of this study was to investigate the association between vascular functions and aging in the elderly population and to clarify the characteristics of vascular functions in subjects aged 80 years or older. We measured flow-mediated vasodilation (FMD), nitroglycerine-induced vasodilation (NID), and brachial-ankle pulse wave velocity (baPWV) in 737 subjects aged 60 years or older who visited the outpatient clinic at Hiroshima University Hospital. FMD and NID were significantly lower in subjects aged 80 years or older than in subjects aged 60–69 years or in subjects aged 70–79 years (1.9 ± 2.0% vs. 2.9 ± 2.6% and 2.7 ± 2.6%, P = 0.008 and P = 0.03, respectively and 8.6 ± 5.1% vs. 12.1 ± 5.6% and 11.2 ± 5.5%, P < 0.001 and P < 0.001, respectively). baPWV was significantly higher in subjects aged 80 years or older than in subjects aged 60–69 years or in subjects aged 70–79 years (1978 ± 452 cm/s vs. 1724 ± 319 cm/s and 1811 ± 318 cm/s, P < 0.001 and P < 0.001, respectively). Age over 80 years was significantly associated with lower FMD (OR, 2.02; 95% CI, 1.19–3.42; P = 0.01), lower NID (OR, 3.62; 95% CI, 2.13–6.17; P < 0.001), and higher baPWV (OR, 3.48; 95% CI, 1.99–6.08; P < 0.001) after adjustment for other cardiovascular risk factors. Vascular functions, including endothelial function, vascular smooth muscle function, and arterial stiffness, were shown to be further impaired in subjects aged 80 years or older, suggesting that vascular functions continue to be impaired throughout life with aging.
Similar content being viewed by others
Introduction
The Japanese population is aging rapidly. Japan has the highest percentage of elderly adults in the world. The percentage of people aged 65 years or older in Japan increased from 4.9% in 1950 to 28.1% in 2018 (https://www.stat.go.jp/data/topics/topi1131.html). The number of people aged 80 years or older in Japan was ~11 million in 2018, accounting for 8.7% of the total Japanese population, and it is predicted that this percentage will continue to increase. Furthermore, the incidences of stroke and acute myocardial infarction in Japanese individuals increase progressively with the advance of age, with an especially high incidence in people aged 80 years or older [1].
Impairment of vascular functions, such as endothelial dysfunction, vascular smooth muscle dysfunction, and increased arterial stiffness, plays an important role in the development and progression of atherosclerosis, leading to cardiovascular complications. Vascular functions are impaired with aging independent of atherosclerosis [2]. Indeed, endothelial function assessed by flow-mediated vasodilation (FMD) of the brachial artery has been shown to be impaired with aging, and arterial stiffness assessed by brachial-ankle pulse wave velocity (baPWV) has been shown to increase with aging even in subjects without cardiovascular risk factors [3, 4]. However, it is unclear whether vascular functions are further impaired in people aged 80 years or older. There is little information on vascular functions assessed by noninvasive vascular function tests, including FMD of the brachial artery, nitroglycerine-induced vasodilation (NID) of the brachial artery, and baPWV, in subjects aged 80 years or older, and to our knowledge, there has been no clinical study in which FMD of the brachial artery, NID of the brachial artery, and baPWV are simultaneously assessed in subjects aged 80 years or older. Determination of the characteristic features of vascular functions in elderly adults may be important to determine whether vascular functions continue to deteriorate throughout life with aging in a society with an increasing proportion of subjects aged 80 years or older. In this study, we measured FMD of the brachial artery, NID of the brachial artery, and baPWV in subjects aged 60 years or older to investigate the association between vascular functions and aging in the elderly and to clarify the characteristics of vascular functions in subjects aged 80 years or older.
Methods
Participants
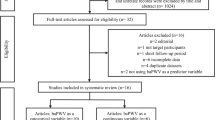
Between April 2007 and October 2018, a total of 1274 participants aged 60 years or older underwent measurements of FMD of the brachial artery, NID of the brachial artery, and baPWV in the cardiology outpatient clinic at Hiroshima University Hospital. Patients receiving nitrate treatment (n = 103); patients with secondary hypertension (n = 90), coronary heart disease (n = 212), cerebrovascular disease (n = 64), peripheral artery disease (n = 59), moderate to severe heart failure (NYHA class III or IV) (n = 3), malignant disease (n = 4), or hepatic cirrhosis (n = 1); and patients receiving dialysis (n = 1) were excluded. Finally, a total of 737 participants aged 60 years or older (368 men and 369 women; mean age, 70.9 ± 6.4 years; age range, 60–87 years) were enrolled in this study. Hypertension was defined as treatment with oral antihypertensive drugs or systolic blood pressure of more than 140 mmHg and/or diastolic blood pressure of more than 90 mmHg measured in a sitting position on at least three different occasions [5]. Diabetes mellitus was defined according to the American Diabetes Association recommendation [6]. Dyslipidemia was defined in accordance with the third report of the National Cholesterol Education Program [7]. Smokers were defined as those who were current smokers. Vascular function tests were performed without withholding medications. The ethics committees of our institutions approved the study protocol. The study was executed in accordance with the Helsinki Declaration of 1975. Written informed consent for participation in the study was obtained from all participants.
Study protocol
Subjects fasted the previous night and abstained from alcohol, smoking, caffeine, and antioxidant vitamins on the day of the vascular function tests. The subjects were kept in the supine position in a quiet, dark, and air-conditioned room (constant temperature of 23–26 °C) throughout the study. A 23-gauge polyethylene catheter was inserted into the left deep antecubital vein to obtain blood samples. Measurements of FMD, NID, and baPWV were performed at least 20 min after maintaining the supine position. Vascular function tests were performed by skilled and trained physicians without detailed knowledge of the baseline clinical characteristics of the subjects.
Measurements of FMD and NID
FMD and NID were measured using UNEXEF18G (UNEX Co., Nagoya, Japan), an ultrasound instrument specialized for FMD and NID measurements equipped with an automated edge detection system for measurement of the brachial artery diameter. Detailed information on the study protocol and on measurements of FMD and NID is provided in the online-only Data Supplement. In brief, FMD measurements were performed using a protocol in which an occlusion cuff was placed around the forearm and inflated to 50 mmHg above systolic blood pressure for 5 min to induce reactive hyperemia with continuous assessment of the diameter change during reactive hyperemia. The brachial artery diameter change in response to a sublingual tablet of 75 μg nitroglycerine was used for the assessment of NID.
Measurement of baPWV
baPWV was measured using a volume-plethysmographic apparatus (Form PWV/ABI, Omron Health Care Co., Kyoto, Japan). Detailed information on the study protocol and measurement of baPWV is provided in the online-only Data Supplement. The higher baPWV value of either side was used for analysis [8].
Statistical analysis
The results are presented as the means ± SD. All reported probability values were two-sided, and a probability value of <0.05 was considered statistically significant. Categorical variables were compared by means of the chi-square test. Continuous variables were compared by using ANOVA with Bonferroni’s test for post hoc comparisons for multiple groups. Multiple logistic regression analyses were performed to identify independent variables associated with endothelial dysfunction, vascular smooth muscle dysfunction, and increased arterial stiffness. The data were processed using JMP version 11 (SAS Institute, Cary, NC).
Results
The baseline clinical characteristics of subjects aged 60 years or older are summarized in Table 1. Of the 737 subjects, 635 (86.3%) had hypertension, 495 (67.5%) had dyslipidemia, 243 (33.1%) had diabetes mellitus, and 88 (12.1%) were current smokers. The mean values were 2.7 ± 2.5% for FMD, 11.3 ± 5.6% for NID, and 1793 ± 346 cm/s for baPWV. We divided the subjects into three groups based on age decades from the 60 s through the 80 s. The baseline clinical characteristics of the three groups are summarized in Table 1. Of the 737 subjects, 87 subjects (11.8%) were aged 80 years or older. There were significant differences in diastolic blood pressure, total cholesterol, triglycerides, low-density lipoprotein cholesterol, glucose, percentage of current smokers, and percentage of subjects taking statins, but there was no significant difference in the prevalence of hypertension, dyslipidemia, or diabetes mellitus among the three groups. FMD was significantly lower in subjects aged 80 years or older than in subjects aged 60–69 years or in subjects aged 70–79 years (1.9 ± 2.0% vs. 2.9 ± 2.6% and 2.7 ± 2.6%, P = 0.008 and P = 0.03, respectively) (Fig. 1a). There was no significant difference in FMD between subjects aged 60–69 years and subjects aged 70–79 years (P = 0.71). NID was significantly lower in patients aged 80 years or older than in subjects aged 60–69 years or in subjects aged 70–79 years (8.6 ± 5.1% vs. 12.1 ± 5.6% and 11.2 ± 5.5%, P < 0.001 and P < 0.001, respectively) (Fig. 1b). There was no significant difference in NID between subjects aged 60–69 years and subjects aged 70–79 years (P = 0.10). baPWV was significantly higher in subjects aged 80 years or older than in subjects aged 60–69 years or in subjects aged 70–79 years (1978 ± 452 cm/s vs. 1724 ± 319 cm/s and 1811 ± 318 cm/s, P < 0.001 and P < 0.001, respectively) (Fig. 1c). baPWV was significantly higher in subjects aged 70–79 years than in subjects aged 60–69 years (P = 0.003). There was no significant difference in baseline brachial artery diameter among the three groups (4.13 ± 0.65 mm vs. 4.11 ± 0.62 mm vs. 4.21 ± 0.66 mm, P = 0.50) (Fig. 1d).
When endothelial dysfunction was defined as FMD of less than the division point for the lowest quartile (<0.9%), there was a significant difference in the prevalence of endothelial dysfunction (21.5% vs. 25.6% vs. 35.6%, P = 0.02) among the three age groups (Table 1). When vascular smooth muscle dysfunction was defined as an NID of less than the division point for the lowest quartile (<7.2%), there was a significant difference in the prevalence of vascular smooth muscle dysfunction (19.3% vs. 24.7% vs. 46.0%, P < 0.001) among the three groups. When increased arterial stiffness was defined as baPWV of more than the division point for the highest quartile (>1971 cm/s), there was a significant difference in the prevalence of increased arterial stiffness (17.8% vs. 27.5% vs. 41.4%, P < 0.001) among the three groups.
Table 2 shows the crude and multivariate-adjusted odds ratios of endothelial dysfunction, vascular smooth muscle dysfunction, and increased arterial stiffness using subjects aged 60–69 years as the reference. Multiple logistic regression analyses revealed that age over 80 years, but not age 70–79 years, was significantly associated with endothelial dysfunction (OR, 2.02; 95% CI, 1.19–3.42; P = 0.01) and vascular smooth muscle dysfunction (OR, 3.62; 95% CI, 2.13–6.17; P < 0.001) and that both age 70–79 years (OR, 2.00; 95% CI, 1.33–3.04; P < 0.001) and age over 80 years (OR, 3.48; 95% CI, 1.99–6.08; P < 0.001) were significantly associated with increased arterial stiffness after adjustment for other cardiovascular risk factors.
The associations between cardiovascular risk factors and vascular functions based on age decades are summarized in Supplementary Table 1. Multiple regression analyses revealed that none of the risk factors included in the model were associated with endothelial dysfunction in any of the age decades and that significant risk factors associated with vascular smooth muscle dysfunction and increased arterial stiffness were different between the age decades (Supplementary Table 1).
We divided the male subjects into three groups by age decades. The clinical characteristics of male subjects are summarized in Supplementary Table 2. In men, although NID was significantly lower in subjects aged 80 years or older than in subjects aged 60–69 years or in subjects aged 70–79 years, there were no significant differences in FMD and baPWV among the three groups (Supplementary Figs. 1a–c). There was a significant difference in the prevalence of vascular smooth muscle dysfunction among the three age groups, but there was no significant difference in the prevalence of endothelial dysfunction or increased arterial stiffness (Supplementary Table 2). Multiple logistic regression analysis revealed that age over 80 years was significantly associated with vascular smooth muscle dysfunction after adjustment for other cardiovascular risk factors in men (Supplementary Table 3).
We divided the female subjects into three groups by age decades. The clinical characteristics of female subjects are summarized in Supplementary Table 4. In women, FMD, NID, and baPWV were significantly more impaired in subjects aged 80 years or older than in subjects aged 60–69 years (Supplementary Figs. 2a–c). There were significant differences in the prevalences of endothelial dysfunction, vascular smooth muscle dysfunction, and increased arterial stiffness among the three groups (Supplementary Table 4). Multiple logistic regression analyses revealed that age over 80 years was significantly associated with endothelial dysfunction, vascular smooth muscle dysfunction, and increased arterial stiffness after adjustment for other cardiovascular risk factors in women (Supplementary Table 5).
Discussion
In the present study, we demonstrated that age over 80 years was significantly associated with impairment of vascular function. There were no significant differences between subjects aged 60–69 years and subjects aged 70–79 years with respect to FMD of the brachial artery and NID of the brachial artery. However, FMD of the brachial artery and NID of the brachial artery were significantly lower in subjects aged 80 years or older than in subjects aged 60–69 years or in patients aged 70–79 years. baPWV increased progressively with aging, and there were significant differences in baPWV among the three groups based on age decades from the 60s through the 80s. The impairment of vascular functions in subjects aged 80 years or older was likely to be more pronounced in women than in men. These findings suggest that endothelial dysfunction, vascular smooth muscle dysfunction, and increased arterial stiffness are further deteriorated in subjects aged 80 years or older and support the population-based observation that incidence rates of cardiovascular disease are especially high in subjects aged 80 years or older in Japan [1]. To our knowledge, this is the first study in which the associations of aging with FMD and NID of the brachial artery and baPWV were simultaneously investigated in the elderly.
Aging alters the function and structure of vascular components, such as the endothelium, subendothelial layer, and tunica media and is involved in the increased risk of cardiovascular events. Endothelial cells of aged individuals tend to be more heterogeneous in shape, size, and axial orientation, resulting in less laminar intraluminal blood flow and an increased number of lipid deposition sites. In the thickened subendothelial layer, the amount of connective tissue and the lipid and calcium content increase with age. In the media, the smooth muscle layers thicken with decreased elastin and increased collagen and calcification [2]. These age-related alterations of vasculature occur independently of atherosclerosis and may contribute to the development of vascular dysfunctions such as endothelial dysfunction, vascular smooth muscle dysfunction, and increased arterial stiffness.
Endothelial dysfunction is the initial step in the process of atherosclerosis and plays an important role in the development and progression of this condition, leading to cardiovascular complications [9, 10]. NO, one of the vasoactive agents released from the endothelium, has a variety of antiatherosclerotic effects, such as vasodilation, inhibition of platelet and leukocyte adhesion, and suppression of vascular smooth muscle cell proliferation [11, 12]. Therefore, reduced NO bioavailability is one of the most important features of endothelial dysfunction. Although several mechanisms underlying age-related endothelial dysfunction have been postulated [13], a disturbed balance between NO and reactive oxygen species (ROS) in favor of oxidative stress may be a crucial regulator of age-related endothelial dysfunction. Oxidant enzyme systems, such as nicotinamide-adenine dinucleotide phosphate, xanthine oxidase, mitochondrial electron transport, and uncoupled endothelial NO synthase, are activated by aging, whereas antioxidant systems, such as superoxide dismutase, glutathione peroxidase, and catalase, are inactivated by aging, resulting in an increase in oxidative stress through increased ROS production and decreased ROS degradation. An increase in oxidative stress causes endothelial dysfunction through reduced NO bioavailability as a result of increased NO inactivation and decreased NO production by ROS. FMD of the brachial artery has been used for the assessment of endothelial function in humans. FMD of the brachial artery has been shown to decrease with age [4, 14,15,16]. However, in previous studies in which the association between FMD and age was investigated, subjects aged 80 years or older were not included or were grouped together with subjects aged 60 years or older or subjects aged 70 years or older. Therefore, it has not been fully determined whether FMD is further decreased in subjects aged 80 years or older. In the present study, FMD was significantly lower in subjects aged 80 years or older than in subjects aged 60–69 years or in subjects aged 70–79 years. In addition, age over 80 years was significantly associated with endothelial dysfunction defined as FMD of less than the division point for the lowest quartile (<0.9%), even after adjustment for other cardiovascular risk factors. These findings suggest that endothelial function is further impaired in subjects aged 80 years or older independently of other cardiovascular risk factors.
Measurement of NID of the brachial artery has been performed as a control test for FMD of the brachial artery to determine whether decreased vasodilatory response to reactive hyperemia is not due to decreased reactivity of vascular smooth muscle cells to NO or vascular structural alterations but is truly due to endothelial dysfunction, as both endogenous NO and exogenous NO act on vascular smooth muscle cells to cause vasodilation. However, recent clinical studies have shown that NID of the brachial artery per se is impaired in patients with cardiovascular risk factors and/or cardiovascular disease, indicating an association between impaired NID of the brachial artery and cardiovascular disorders [17,18,19]. Although the precise mechanisms underlying the impairment of NID in patients with cardiovascular disorders have not been fully elucidated, increased production of ROS in vascular smooth muscle cells under pathological conditions, such as hyperglycemia, hyperlipidemia, and hypertension, has been postulated as a crucial determinant of vascular smooth muscle dysfunction [20,21,22]. Experimental studies have shown that ROS inhibit NO-mediated intravascular signaling pathways by suppressing the activities of soluble guanylyl cyclase and cGMP-dependent kinase in vascular smooth muscle cells, leading to impaired relaxation of vascular smooth muscle cells and consequent impaired NID of the brachial artery. ROS have been shown to increase in vascular smooth muscle cells with aging [23, 24]. Age-related increases in oxidative stress may attenuate NO-induced intracellular signaling pathways in vascular smooth muscle cells, resulting in impaired NID of the brachial artery. Previous studies showed that there is no significant association between NID of the brachial artery and age after adjustment for other cardiovascular risk factors [17, 19]. However, in those studies, subjects aged 80 years or older were not included [17], or the number of subjects aged 80 years or older was too small (n = 22) [19]. In the present study, NID of the brachial artery was significantly lower in subjects aged 80 years or older than in subjects aged 60–69 years or in subjects aged 70–79 years. In addition, age over 80 years was significantly associated with vascular smooth muscle dysfunction defined as NID of less than the division point for the lowest quartile (<7.2%) after adjustment for other cardiovascular risk factors. These findings suggest that vascular smooth muscle function is further impaired in subjects aged 80 years or older independently of other cardiovascular risk factors.
baPWV has been used for the assessment of arterial stiffness in humans. baPWV has been shown to correlate well with carotid-femoral PWV used as the standard noninvasive method for assessment of the central arterial stiffness [25, 26]. The arterial media is composed of vascular smooth muscle cells and extracellular matrix constituents such as elastin and collagen. These components of the media and their interactions are the major determinants of arterial stiffness. With advancing age, arterial stiffness is increased by senescence of vascular smooth muscle cells, by the disturbed balance between elastin and collagens through decreased production of normal elastin and overproduction of abnormal collagens, and by the alterations of interactions between vascular smooth muscle cells and extracellular matrix constituents [27]. Age-related decrease in NO bioavailability leads to an increase in secretion and activity of transglutaminase 2, a multifunctional enzyme catalyzing cross-linking of extracellular matrix proteins and altering the behavior of vascular smooth muscle cells, which may, in part, contribute to increased arterial stiffness with aging [28,29,30,31]. Previous studies in which subjects aged 80 years or older were enrolled have shown that baPWV increases progressively with age [3, 26]. Consistent with these previous observations, baPWV increased with age from the 60s through the 80s in the present study.
Our results demonstrated that vascular functions, including endothelial function, vascular smooth muscle function, and arterial stiffness, are further impaired in subjects aged 80 years or older, suggesting that vascular functions continue to be impaired throughout life with aging. Although impairment of vascular functions with aging is inevitable, it may be possible to decelerate the age-related deterioration of vascular functions through several interventions, including lifestyle modifications such as regular exercise, salt restriction, dietary caloric restriction, and body weight reduction, and pharmacological therapy using specific classes of drugs that exert an additional beneficial effect on vascular functions [10, 32]. Cardiovascular risk management by appropriate interventions should be performed from the early stage of life to decelerate the deterioration of vascular functions. Recently, the concept of vascular aging has been proposed [32]. It has been posited that early vascular aging can be diagnosed in patients with an abnormally high arterial stiffness for their age and sex, whereas supernormal vascular aging can be diagnosed in subjects with an exceptionally low arterial stiffness for their age and sex. This concept is especially focused on arterial stiffness. Our findings showed that not only arterial stiffness but also endothelial function and vascular smooth muscle function are further impaired in subjects aged 80 years or older, indicating that vascular aging should be evaluated not only by arterial stiffness assessed by PWV but also by endothelial function assessed by FMD and vascular smooth muscle function assessed by NID of the brachial artery.
Analyses including only subjects without cardiovascular risk factors would enable more specific conclusions regarding the associations between aging and vascular functions to be drawn. However, the number of subjects aged 80 years or older who did not have cardiovascular risk factors was too small (n = 5) to analyze the effects of aging on subjects without cardiovascular risk factors in the present study.
In conclusion, vascular functions, including endothelial function assessed by FMD, vascular smooth muscle function assessed by NID, and arterial stiffness assessed by baPWV, are further impaired in subjects aged 80 years or older, in agreement with the very high incidence rates of cardiovascular diseases in subjects aged 80 years or older in Japan. Further studies are needed to determine whether aggressive interventions with lifestyle modifications and pharmacological treatment decelerate the age-related deterioration of vascular functions.
References
Hata J, Ninomiya T, Hirakawa Y, Nagata M, Mukai N, Gotoh S, et al. Secular trends in cardiovascular disease and its risk factors in Japanese: half-century data from the Hisayama Study (1961-2009). Circulation. 2013;128:1198–205.
Wei JY. Age and the cardiovascular system. N Engl J Med. 1992;327:1735–9.
Tomiyama H, Yamashina A, Arai T, Hirose K, Koji Y, Chikamori T, et al. Influences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement—a survey of 12 517 subjects. Atherosclerosis. 2003;166:303–9.
Tomiyama H, Kohro T, Higashi Y, Takase B, Suzuki T, Ishizu T, et al. Reliability of measurement of endothelial function across multiple institutions and establishment of reference values in Japanese. Atherosclerosis. 2015;242:433–42.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
American Diabetes Association. Clinical practice recommendations 1999. Diabetes Care 1999;22:S1–114.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Nakamura M, Yamashita T, Yajima J, Oikawa Y, Sagara K, Koike A, et al. Brachial-ankle pulse wave velocity as a risk stratification index for the short-term prognosis of type 2 diabetic patients with coronary artery disease. Hypertens Res. 2010;33:1018–24.
Ross R. Atherosclerosis–an inflammatory disease. N Engl J Med. 1999;340:115–26.
Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial function and oxidative stress in cardiovascular diseases. Circ J. 2009;73:411–8.
Vallance P, Collier J, Moncada S. Effects of endothelium-derived nitric oxide on peripheral arteriolar tone in man. Lancet. 1989;2:997–1000.
Vanhoutte PM. Endothelium and control of vascular function. State of the Art lecture. Hypertension. 1989;13:658–67.
Higashi Y, Kihara Y, Noma K. Endothelial dysfunction and hypertension in aging. Hypertens Res. 2012;35:1039–47.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Relationship between flow-mediated vasodilation and cardiovascular risk factors in a large community-based study. Heart. 2013;99:1837–42.
Celermajer DS, Sorensen KE, Bull C, Robinson J, Deanfield JE. Endothelium-dependent dilation in the systemic arteries of asymptomatic subjects relates to coronary risk factors and their interaction. J Am Coll Cardiol. 1994;24:1468–74.
Benjamin EJ, Larson MG, Keyes MJ, Mitchell GF, Vasan RS, Keaney JF Jr, et al. Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham Heart Study. Circulation. 2004;109:613–9.
Adams MR, Robinson J, McCredie R, Seale JP, Sorensen KE, Deanfield JE, et al. Smooth muscle dysfunction occurs independently of impaired endothelium-dependent dilation in adults at risk of atherosclerosis. J Am Coll Cardiol. 1998;32:123–7.
Raitakari OT, Seale JP, Celermajer DS. Impaired vascular responses to nitroglycerin in subjects with coronary atherosclerosis. Am J Cardiol. 2001;87:217–9.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Nitroglycerine-induced vasodilation for assessment of vascular function: a comparison with flow-mediated vasodilation. Arterioscler Thromb Vasc Biol. 2013;33:1401–8.
Munzel T, Afanas’ev IB, Kleschyov AL, Harrison DG. Detection of superoxide in vascular tissue. Arterioscler Thromb Vasc Biol. 2002;22:1761–8.
Liu S, Ma X, Gong M, Shi L, Lincoln T, Wang S. Glucose down-regulation of cGMP-dependent protein kinase I expression in vascular smooth muscle cells involves NAD(P)H oxidase-derived reactive oxygen species. Free Radic Biol Med. 2007;42:852–63.
Sydow K, Daiber A, Oelze M, Chen Z, August M, Wendt M, et al. Central role of mitochondrial aldehyde dehydrogenase and reactive oxygen species in nitroglycerin tolerance and cross-tolerance. J Clin Investig. 2004;113:482–9.
Moon SK, Thompson LJ, Madamanchi N, Ballinger S, Papaconstantinou J, Horaist C, et al. Aging, oxidative responses, and proliferative capacity in cultured mouse aortic smooth muscle cells. Am J Physiol Heart Circ Physiol. 2001;280:H2779–88.
Fry JL, Al Sayah L, Weisbrod RM, Van Roy I, Weng X, Cohen RA, et al. Vascular smooth muscle sirtuin-1 protects against diet-induced aortic stiffness. Hypertension. 2016;68:775–84.
Sugawara J, Hayashi K, Yokoi T, Cortez-Cooper MY, DeVan AE, Anton MA, et al. Brachial-ankle pulse wave velocity: an index of central arterial stiffness? J Hum Hypertens. 2005;19:401–6.
Tanaka H, Munakata M, Kawano Y, Ohishi M, Shoji T, Sugawara J, et al. Comparison between carotid-femoral and brachial-ankle pulse wave velocity as measures of arterial stiffness. J Hypertens. 2009;27:2022–7.
Najjar SS, Scuteri A, Lakatta EG. Arterial aging—is it an immutable cardiovascular risk factor? Hypertension. 2005;46:454–62.
Nurminskaya MV, Belkin AM. Cellular functions of tissue transglutaminase. Int Rev Cell Mol Biol. 2012;294:1–97.
Santhanam L, Tuday EC, Webb AK, Dowzicky P, Kim JH, Oh YJ, et al. Decreased S-nitrosylation of tissue transglutaminase contributes to age-related increases in vascular stiffness. Circ Res. 2010;107:117–25.
Jung SM, Jandu S, Steppan J, Belkin A, An SS, Pak A, et al. Increased tissue transglutaminase activity contributes to central vascular stiffness in eNOS knockout mice. Am J Physiol Heart Circ Physiol. 2013;305:H803–10.
Steppan J, Bergman Y, Viegas K, Armstrong D, Tan S, Wang H, et al. Tissue transglutaminase modulates vascular stiffness and function through crosslinking-dependent and crosslinking-independent functions. J Am Heart Assoc. 2017;6:e004161.
Laurent S, Boutouyrie P, Cunha PG, Lacolley P, Nilsson PM. Concept of extremes in vascular aging from early vascular aging to supernormal vascular aging. Hypertension. 2019;74:218–28.
Acknowledgements
We thank Megumi Wakisaka, Miki Kumiji, Ki-ichiro Kawano, and Satoko Michiyama for their excellent secretarial assistance.
Funding
Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (18590815 and 21590898 to YH) and a Grant-in-Aid of Japanese Arteriosclerosis Prevention Fund (to YH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Maruhashi, T., Kajikawa, M., Kishimoto, S. et al. Vascular function is further impaired in subjects aged 80 years or older. Hypertens Res 43, 914–921 (2020). https://doi.org/10.1038/s41440-020-0435-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-020-0435-z
Keywords
This article is cited by
-
Vascular function assessed by flow-mediated vasodilation and nitroglycerine-induced vasodilation in subjects with first-degree atrioventricular block
Scientific Reports (2024)
-
Annual reports on hypertension research 2020
Hypertension Research (2022)
-
Vascular Function and Frailty in Community-Dwelling Older Individuals
Artery Research (2022)