Abstract
Provision of non-invasive vascular imaging results to individuals has been shown to improve cardiovascular disease risk factor control: its impact on diet remains uncertain. In this two-arm, single-blind, parallel, 12-week randomized controlled trial, 240 participants, 57.5% females aged 60–80 y had abdominal aortic calcification and clinical assessments performed at a hospital clinic. Participants were randomized 1:1 to receive (intervention n = 121) or not (control n = 119) their calcification results. Both groups received educational resources on cardiovascular disease risk control and were unblinded to the intervention. Outcome measures were performed at baseline and 12 weeks. The primary outcomes of the study were changes in fruit and vegetable intake measures over 12 weeks assessed using plasma carotenoid concentrations (biomarkers of FV intake) and a food frequency questionnaire. Secondary outcomes included 12-week changes in other aspects of the diet, physical activity, body weight, blood pressure, heart rate, lipid profile, glucose concentrations, estimated cardiovascular disease risk score, and medication use. Between-group differences were tested using linear mixed-effects regression. There were no between-group differences in the primary outcomes at 12 weeks: plasma carotenoids (mean difference +0.03 µg/mL [95%CI −0.06, 0.13]) and fruit and vegetable intakes (+18 g/d [−37, 72]). However, the provision of calcification results led to between-group differences in serum total (−0.22 mmol/L [−0.41, −0.04]) and non-HDL (−0.19 mmol/L [−0.35, −0.03]) cholesterol, and estimated cardiovascular disease risk score (−0.24% [−0.47, −0.02]). No between-group differences were seen for other secondary outcomes. In this work, providing vascular imaging results did not improve diet but did improve some cardiovascular disease risk factors (Australian and New Zealand Clinical Trials Registry ACTRN12618001087246).
Similar content being viewed by others
Introduction
Suboptimal lifestyle is the major contributor to cardiovascular disease (CVD) globally1, with efforts to improve diet and physical activity a cornerstone to reducing disease burden2. Despite continuing public health messaging and health promotion campaigns, most people fail to meet recommended targets, particularly those for fruit and vegetable (FV) consumption3.
Providing asymptomatic individuals with results of non-invasive vascular imaging may provide a means to elicit behaviour changes to improve diet, physical activity and other CVD risk factors. This may be achieved through affecting motivation, self-efficacy and intentions with behaviour change techniques such as goal settings and providing resources and instructions4, improved CVD risk assessment by health professionals, and improved decision making shared between clients and healthcare professionals5. Provision of coronary artery calcification (CAC) and carotid atherosclerosis results has been shown to lead to better CVD risk control, including blood pressure and circulating lipid levels, by promoting medication initiation and adherence6,7,8. However, to date, only limited evidence from randomized controlled trials (RCTs) exists to suggest that providing individuals (both adults with CVD risk factors and otherwise healthy individuals aged 42–64 years) with their vascular imaging results can positively impact FV consumption, overall diet quality and physical activity behaviours as reported in a scoping review by our team8.
Abdominal aortic calcification (AAC) is a measure of structural vascular disease9. It is characterized by the buildup of calcium in the abdominal aorta, which is one of the first sites where vascular calcification is observed10, often before the coronary arteries. AAC is closely related to subclinical CVD in the coronary, carotid and peripheral arteries11,12, and predicts future fatal and nonfatal CVD events and all-cause mortality13. Consumption of FV14,15 and their constituents16 have been associated with less extensive AAC. To our knowledge, no previous studies have investigated whether provision of visual AAC results can lead to changes in FV intake, improved overall diet and physical activity, as well as other CVD-related risk factors.
The objective of this RCT was to investigate the impact of providing AAC results with educational resources, compared with educational resources alone, on measures of FV intake, physical activity and other CVD risk factors, including circulating lipids and glucose concentrations and blood pressure in 60–80 year-old Australian males and females. Here we show that provision of AAC results with education does not improve measures of fruit and vegetable intake, diet quality or physical activity over 12 weeks, but may contribute to better CVD risk factor control, compared to education alone.
Results
Participants
Baseline demographic characteristics of all participants are reported in Table 1. Mean ( ± SD) age of participants was 67.8 ± 5.0 years, and 57.5% (n = 138) were females. All 240 participants randomized to one of the groups were included in this study (n = 227 completed the 12 weeks). Overall, 57.1% (n = 137) of participants had evidence of AAC which was similar in the those who received the AAC results plus education (AAC+Ed, 57.9%) and those who received education alone (Control+Ed, 56.3%).
Study attrition
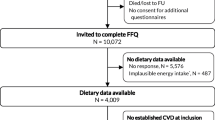
A total of 245 participants were recruited between September 2020 and May 2022. After exclusions, 240 participants were randomized, with 227 (94%) completing the 12-week trial with a similar attrition in the AAC+Ed (n = 6, 5.0%) and Control+Ed (n = 7, 5.9%) groups (Fig. 1).
Primary outcomes
There were no between-group differences for the changes over time in either plasma carotenoid concentrations (pinteraction = 0.494) or FV intake (pinteraction = 0.526), with both groups experiencing similar significant within-group improvements after 12 weeks (Table 2).
Secondary outcomes
There was no between-group difference in changes in dietary quality (Dietary Guideline Index [DGI]) (Table 3), and all other dietary components (i.e., energy intake, macro and micronutrients) after 12 weeks, with the exception of folate which significantly increased in the AAC+Ed group compared to Control+Ed (Supplementary Table 1). Significant within-group increases in consumption of fibre and a significant decrease in the intake of saturated fats was observed in the AAC+Ed (Supplementary Table 1). Both groups improved DGI and intake of vitamin C over 12 weeks.
CVD risk factors including clinical and biochemical measures and their change over 12 weeks are presented in Table 3. The estimated 5-year CVD risk score was significantly reduced in the AAC+Ed group compared to Control+Ed (mean difference for change: −0.24% [−0.47, −0.02], p = 0.048), which was driven by significantly greater improvements in total cholesterol, non- high density lipoprotein cholesterol (non-HDL-c), and low-density lipoprotein cholesterol (LDL-c), in the AAC+Ed group. Changes in non-fasting glucose concentrations were significantly different in the AAC+Ed group compared to the Control+Ed group. This was due to increases in glucose over the 12 weeks in the Control+Ed group, with no changes observed in the AAC+Ed group. There were no significant differences in body weight, physical activity, systolic and diastolic blood pressure, and heart rate changes between groups over 12 weeks.
Medication and health care use
During the 12 week intervention, a similar proportion [all p > 0.05] of participants in both groups visited their general practitioner (GP) (AAC+Ed, n = 94 [82%] vs. Control+Ed, n = 88 [79%]), had a blood test (AAC+Ed, n = 42 [37%] vs. Control+Ed, n = 48 [43%]), and had a medical procedure (AAC+Ed, n = 19 [17%] vs. Control+Ed, n = 20 [18%]). Over the 12 weeks, five participants initiated on lipid-lowering medication (all in the AAC+Ed group) and one participant discontinued lipid-lowering medication (Control+Ed group). Three participants initiated (n = 1 AAC+Ed group, n = 2 Control+Ed group) and one participant discontinued (Control+Ed group) antihypertensive medication over the 12 weeks. One participant in the AAC+Ed group reported initiation on diabetes medication over 12 weeks. Exploratory analyses adjusting for change in lipid- or glucose-lowering medication did not meaningfully alter the observed between-group differences in these outcomes presented in Table 3.
Change in cardiovascular risk factors by AAC score in the AAC+Ed group
In exploratory analyses, we investigated the correlation between baseline AAC24 scores and change in outcomes over 12 weeks as well as comparing AAC24 score changes in participants with evidence (AAC ≥ 1) versus no evidence (AAC = 0) of AAC at baseline, in the AAC+Ed group. There was an inverse association between baseline AAC 24-point scores and change in body weight (Supplementary Table 2). Greater reduction in body weight (p < 0.01), in systolic and diastolic blood pressure (each p < 0.05) and in the Australian CVD risk score (p = 0.05) were found in those with evidence of AAC compared to no evidence of AAC (Supplementary Table 3).
Evidence for an impact of COVID-19 on primary outcomes
There was a significant (p < 0.001) time by study wave interaction for total carotenoid concentrations (Supplementary Fig. 1), which indicates that the response for those outcomes differed between study waves.
Discussion
In this 12-week RCT in community dwelling older adults, we observed that provision of AAC results with lifestyle educational resources did not lead to significant differences in our primary outcomes (plasma carotenoid concentrations and consumption of FV measured by a food frequency questionnaire [FFQ) compared to educational resources alone. Both groups exhibited substantial and significant increases in plasma carotenoid concentrations and self-reported FV consumption over 12 weeks. Provision of AAC results did result in significant beneficial changes in secondary outcomes including blood lipid concentrations, and as a result reduced the 5-year estimated CVD risk relative to controls.
There are several possible reasons for the lack of impact of provision of AAC results on measures of FV intakes relative to control. Conducting this trial during the COVID-19 pandemic may have blunted risk-reducing behaviours. Our results showed differential circulating carotenoid and dietary changes with minimal changes in the first wave most impacted by the pandemic. The differences observed in the 12-week changes in FV intake across study waves may have been due to COVID-19 restrictions that were in place in 202017 when this wave was being recruited. These restrictions may have particularly affected high-risk groups like older individuals17. Limiting movement measures in place18 may have hindered efforts to increase FV consumption in the first wave of the study. As restrictions eased in mid-2021, corresponding with the recruitment of wave 2 and 3, greater FV intake was observed in both groups at 12 weeks. The COVID-19 pandemic or restrictions may also have affected individuals’ perceived threat, efficacy beliefs, and behavioural intentions after receiving AAC results4. This statistically significant difference between waves, may indicate an influence of the pandemic and restrictions on lifestyle behaviours similar to those observed by others19. Another possible reason is that AAC is a less well-established and recognised CVD risk factor than CAC, which has been more used widely and is better understood by healthcare professionals. This is supported by previous studies showing that visualization of CAC may have a positive influence on medication initiation20 and adherence, as well as on lipid profile and other risk behaviours21. This is noteworthy because participants were asked to share and discuss their results with their healthcare teams.
Whilst we did not observe between-group differences in plasma carotenoids and FV intake, relatively large within-group changes from baseline were observed (74 g/day and 92 g/day for Control+Ed and AAC+Ed groups, respectively). The size of the observed change in FV intake may be clinically relevant, considering that one additional serve of FV a day (~80 g) has been reported to lead to a 4% risk reduction in CVD risk22. The significant within-group increases in DGI (Table 3) and vitamin C intake (Supplementary Table 1) in both the AAC+Ed and Control+Ed groups may be explained by the increase in FV consumption within each group. These within-group changes suggest that participation in the study and the education provided to both groups elicited dietary behaviour change, not directly related to the provision of AAC results. This may have blunted the potential for additional increases in the AAC+Ed group. Another possible reason for the changes could have been the “Hawthorne effect” due to being involved in a trial where one is being assessed23. Participants in this trial are likely to have been motivated to change their diet because they volunteered to join a trial on lifestyle change. A meta-analysis of RCTs reported that the Hawthorne effect differs based on the education and roles of the researchers and participants, the study setting, and outcomes, with an overall odds ratio (OR and 95% confidence interval [CI]) of the effect in primary care being 1.41 ([1.13; 1.75])24. The study reports that the trial design is an important factor when attempting to minimize this effect24. Our participants were unblinded and the withholding of AAC information and the expectation of not knowing the AAC results in the Control+Ed group, may have also caused worry, and led to greater levels of behaviour change than if people received the educational resources without the expectation of receiving results. In addition, in the AAC+Ed group ~54% had evidence of AAC (score 1–5) and only ~3% had evidence of extensive AAC (score ≥6) which is much lower than the ~19% seen in other similarly aged populations12. It is possible that visualization of positive imaging results (no evidence of AAC in 42% of the AAC+Ed group) showing a healthy aorta may have reassured some participants in the AAC+Ed group, reducing the stimulus for behaviour modification25. Some evidence for this was seen in the analysis of the AAC+Ed group where higher AAC scores were correlated with greater weight loss over 12 weeks. Future RCTs should recruit only participants with AAC and examine the changes in diet and lifestyle according to AAC severity (presence of lower vs. higher AAC scores).
An important finding from this study was that the provision of AAC led to improved blood lipid concentrations (4.2% in total cholesterol, 5.3% in LDL-c and 5.1% in non-HDL-c). The observed difference in systolic blood pressure of 1.3% was not significant in our study. These results are similar to other trials providing CAC and carotid ultrasound results26,27,28. For example, provision of CAC results in the EISNER study led to improvements in CVD risk factors, including reductions in LDL-c (~4.5%) and blood pressure (~1.5%) over 4 years28. Similarly, in a subgroup of participants receiving lipid-lowering treatment in the VIPVIZA study, the reduction in both total and LDL-c was approximately twofold higher in the intervention group compared to the control group27. The authors also reported a three times greater reduction in systolic blood pressure in the intervention group compared to controls, among those taking antihypertensive medication27. A meta-analysis including six RCTs (n = 7083) reported that provision of vascular imaging led to significant decrease in LDL-c, total cholesterol, and systolic blood pressure29, with potential causal factors being weight loss7, and the initiation and/or adherence to cholesterol or blood pressure-lowering medications6,7,26. Several factors may explain the observed effects on improved blood lipid concentrations in the current study. Exploratory analyses indicated an association of higher baseline AAC scores with greater weight reduction after 12 weeks in the AAC+Ed group (Supplementary Table 2), which may partially explain the observed favourable effects on lipids profile in this group relative to Control+Ed.
In exploratory analyses, the inverse association between baseline AAC 24-point scores and change in body weight in the AAC+Ed group indicates that those with higher AAC scores had greater weight change (Supplementary Table 2) which may partially explain the favourable effects on lipids observed in this group relative to Control+Ed. Additionally, there was a significant increase in fibre intake and a significant reduction in intake of saturated fats from baseline to 12 weeks, which may have contributed to improvements in blood lipids in the AAC+Ed group. Although not significantly different between groups, five participants initiated lipid lowering medication in the AAC+Ed group compared to none in the Control+Ed group which may have had a small impact on the overall difference. Given the size of this study, we cannot identify the underlying cause(s) for these changes. It is possible that the observed changes reflect cumulative benefits of numerous risk-reducing behaviours such as dietary choices (e.g., saturated fat intake), medications and other risk reducing behaviours. However, given our study was only designed to examine if simply providing vascular imaging results with education may impact risk-reducing behaviours compared to education alone, there is a need for larger RCTs combining provision of these results with evidence-based behaviour change programmes, to determine the mechanisms involved.
Our findings also indicate that those with evidence of AAC in the AAC+Ed group had a significantly lower body weight, and systolic and diastolic blood pressure, compared to those with no evidence of AAC (Supplementary Table 3). However, these are hypothesis generating results and should be interpreted with caution.
This study has many strengths. It was the first to provide AAC results to individuals, and to investigate changes in objective (circulating) markers and self-reported measures of dietary changes in FV, biochemical measures, as well as capturing additional testing and changes to medications. Additionally, we used standardized educational resources in both groups allowing comparison to usual practice. The provision of AAC results is a particular strength as this is one of the first sites where calcification occurs30,31. Images to assess AAC can be seamlessly captured at the same time as bone density testing for fracture prediction using ultra-low radiation lateral spine images from Dual energy X-ray Absorptiometry (DXA) machines10,32. AAC can also be assessed on standard radiographs and abdominal computed tomography scans obtained for other clinical indications. This would enable community-based vascular calcification assessment, particularly as the assessment of these images for AAC has recently been automated and shown to strongly predict future CVD events33. Finally, we have also undertaken a detailed process evaluation to further understand what has worked and what needs to be improved in future trials investigating the impact of providing asymptomatic CVD results for CVD risk factor control34.
Limitations
This study has several limitations. The effectiveness of the provision of AAC results may have been limited because results were delivered virtually instead of face-to-face, due to COVID-19 restrictions, so participants may not have fully understood the scans provided. FFQs are designed to be less burdensome than food diaries, as they record the frequency of food consumption. Although they are less burdensome to participants, they also have several limitations such as ability of participants to recall intake over a longer timeframe. Our participants were requested to report their frequency intake in the previous 12 weeks, rather than 12 months, in order to have a better estimate of change within the timeframe of the study. Although the FFQ has been validated for the previous 12 months, 12 weeks is still a relatively long timeframe for food intake recall. Other potential limitations include incomplete food lists, portion size estimation and imprecision. The FFQ was sensitive enough to detect substantial increases in FV in both groups but was not sensitive if there were small between-group differences, as well as a possible seasonal effect due to the varying FV availability throughout the year. The educational videos were concise, around 12 mins in duration, but this was to align with the rationale of the study of offering recommendations similar to those commonly provided by GPs. Also, due to COVID-19 restrictions, we collected non-fasting blood samples, with participants attending the pathology laboratory from early morning to early afternoon and not necessarily at the same time at baseline and 12 weeks. This may have affected the biochemical results. Although we did find differences in blood lipids, non-fasting blood samples will have increased variation in some biochemical measures performed, potentially underestimating the significance of observed differences in blood biochemistry, particularly of the circulating carotenoids. Additionally, we did not reach our target sample size of 300 participants. With the current sample size of 227 (n = 115 AAC+Ed and n = 112 Control+Ed), using observed SDs we had >80% power to detect a difference of 0.16 µg/mL in carotenoids and 101 g/day in total FV at 12 weeks. Finally, the substantial improvements in FV intakes in both groups supports the interpretation that many participants may have altered their behaviours as a result of being observed (the Hawthorne effect). Future trials should consider this in the design, attempting to minimize its impact on participants (e.g., separating enrolment and randomization by 1 month, and repeating assessments at the randomization visit, as participants tend to change their behaviour at the start of the trials24).
In conclusion, the main findings of this 12-week RCT was that provision of AAC results with educational resources did not lead to greater positive dietary changes than the provision of educational resources alone. However, both groups experienced similar significant improvements in FV intake and plasma carotenoid concentrations suggesting that the provision of the educational resources was effective for eliciting some behavioural changes. Provision of AAC results was found to be more effective for improving CVD risk factor control, principally the blood lipids. Further larger studies providing tailored dietary and lifestyle advice, with structured follow-ups, are warranted to explore the impact of the provision of AAC on risk-reducing diet and CVD-risk behaviours, particularly in the subset with higher AAC (≥6). Further research is also needed to assess participants understanding, perceptions and beliefs about AAC, as the potential consequences of the presence of AAC are less well-established and recognised than CAC by healthcare professionals. This has been highlighted by some of the participants in the process evaluation of the study (unpublished data). Improved understanding of the mechanisms driving these changes, and more effective and sustained strategies for CVD prevention and risk management is also needed.
Methods
Trial design
Two consumer representatives (females >65 years) assisted with the design of the Modification Of Diet, Exercise and Lifestyle (MODEL) study, including developing educational resources, and providing feedback on the burden of the intervention, as previously described35. Initial ethics approval for this trial was received in June 2018 (Edith Cowan University Human Research Ethics Committee, project number: 20513 HODGSON). The trial initiated in December 2019 and was terminated in March 2020 due to the COVID-19 pandemic. The study was redesigned, with ethics amendments approved in August 2020 and a new trial started in September 2020. The changes made to the published MODEL study protocol35 (Supplementary Note 1) due to COVID-19 regulations are summarized in Supplementary Table 4. The initial protocol was updated accordingly at the Australian New Zealand Clinical Trial Registry (ACTRN12618001087246). The CONSERVE (joint extension for the CONSORT and SPIRIT reporting guidelines) 2021 Statement36, created to improve reporting of studies that faced substantial modifications due to extenuating circumstances, such as the COVID-19 pandemic, was used to report the results of this trial.
The MODEL study was a 12 week, two-arm RCT, with participants randomly allocated to receive their AAC results with educational resources (AAC+Ed group), or educational resources alone (Control+Ed group) in a 1:1 ratio, assuming 50% would have evidence of AAC10,37. The sequence of allocation and block size was generated using Stata (StataCorp) version 1438 and the user-written module called “ralloc”39 by a statistician (RW). A sequential treatment code was generated for participants joining the study on their own, or to the same block if with partners (e.g., wife and husband or siblings). A blinded research assistant enroled participants in the study and the numeric codes were assigned by an unblinded investigator not involved in data collection. Participants were unblinded and researchers performing the study assessments were blinded to the treatments received until the end of the study.
Participants
A total of 245 ambulant community-dwelling males and female, from the general population in Perth, Western Australia, were screened via newspaper advertisements. Eligibility criteria, assessed via telephone screening, included being aged between 60–80 years, able to attend in person clinic visits and complete electronic questionnaires, and having a mobile phone and email address. The study flow chart is summarized in Fig. 1. Participants who participated in the terminated pre-COVID-19 MODEL trial were not permitted to participate in the subsequent revised trial. Therefore, the same eligibility criteria (exclusion and inclusion criteria) applied for all participants included in this current revised MODEL study.
Participants deemed eligible were sent an information pack via email and invited to attend a baseline clinic visit at the Sir Charles Gairdner Hospital Bone Density Unit, where they signed a written consent form prior to undergoing any assessments. Participants were enroled in one of three study waves, performed during three distinct calendar periods, during a different phase of the COVID-19 pandemic: wave 1, September 2020 to Apr 2021 (early); wave 2, May 2021 to September 2021 (mid); wave 3, October 2021 to May 2022 (late).
Interventions
Approximately 2 weeks after their baseline visit, all participants received a pre-scheduled email informing them of their group allocation. The email included a link to a ~12-min video with information on CVD40 (plus, for the AAC+Ed group only, an explanation of AAC and its link with CVD risk) and dietary and physical activity recommendations41, as well as how to achieve the three goals of the study35 (Supplementary Table 5); Goal 1, increase fresh fruit intake by at least 1 serve/d (150 g/d) and increase vegetable intake by at least 1 serve/d (75 g/d); Goal 2, improve other aspects of the diet (i.e., reduce intake of salt, sugar, processed foods and increase wholegrains and nuts); and Goal 3, increase physical activity and reduce sitting time. In addition to the video, the email included an e-booklet summarizing the educational information provided in the video, as well as frequently asked questions (Supplementary Table 5).
Each individual’s AAC results were provided in the email at baseline for the AAC+Ed group, and for the Control+Ed group, were delayed to the end of the 12-week study. One of three different versions of the AAC results letter was provided to participants based on their AAC scores: (i) evidence of AAC (scores 1-5); (ii) evidence of extensive AAC (scores ≥ 6); or (iii) no evidence of AAC. For any AAC (i.e., ‘i’ and ‘ii’), the results letter included the actual AAC scan showing the spine, and the calcified abdominal aorta indicated by arrows; an illustrative representation of the regions with advanced blood vessel disease marked in red based on AAC scoring; and explanation of the results (Fig. 2). For no evidence of AAC (i.e., ‘iii’), the letter showed a clear image and diagram plus a green circle indicated absence of calcification. Both participants and their GP received a copy of the AAC results letter and the GP information letter. A 30-min scheduled follow-up phone call was conducted by an unblinded investigator (either CPB, JDV or MS) on the same day participants received the email.
Outcomes
All outcome measures were performed at baseline and 12 weeks. The primary outcomes of the RCT were changes in FV intake over 12 weeks using both objective (plasma carotenoid concentrations—biomarkers of FV intake) and subjective (FV intake assessed using a self-reported FFQ) measures—study goal 1. Secondary outcomes included 12-week changes in: (i) Other aspects of the diet, including adherence to the Australian Dietary Guidelines (ADG, assessed by DGI), and intakes of macro and micronutrients—study goal 2; (ii) Physical activity levels—study goal 3; (iii) Other secondary CVD-related risk factor outcomes including clinical [body weight, blood pressure, heart rate] and biochemical [lipid profile and glucose concentrations] measures, as well as the estimated CVD risk score; and (iv) Medication and health-care use. Exploratory analyses were also conducted to determine whether higher baseline AAC scores led to greater changes in CVD-related risk factors in the AAC+Ed group.
Demographic information
Participants’ age (years), sex (male/female)42, relationship status (married, single, divorced, widowed, in a relationship, or other), levels of education (never to some high-school, completed high-school, technical, diploma, certificate, bachelors, higher degree or other), socio-economic status (income brackets), postcode, and smoking habits (never, ever or current smoker) were self-reported using electronic questionnaires.
Dietary assessment
Baseline and 12-week (end of intervention) food intake was assessed using the validated Dietary Questionnaire for Epidemiological Studies Version 3.2 (DQES v3.2) developed by the Cancer Council of Victoria43. This FFQ was originally designed to capture intake over 12 months. Our participants were requested to report their frequency intake in the previous 12 weeks, to have a better estimate of change within the timeframe of the study. The FFQ records the frequency of consumption using 10 frequency options ranging from “never” to “3 or more times per day”43. FV intake (g/d) was estimated by summing all FV from this questionnaire (Supplementary Table 6). Energy intake (kcal/d), consumption of alcoholic beverages (g/d), other food groups and nutrients were estimated based on total intake reported by individuals. Adherence to the ADG41 was estimated using a modified DGI scoring system14,44.
Physical activity
Physical activity levels were estimated using the Community Healthy Activities Model Program for Seniors (CHAMPS) questionnaire. This questionnaire estimates weekly frequency and duration of a variety of physical activities in older adults, including both total and moderate-to-vigorous physical activity (total number of hours per week)45.
Other cardiovascular risk factors
Clinical assessments
DXA scans were performed using a Hologic Horizon A densitometer. AAC was assessed from the lateral spine image by an expert in densitometric imaging (JTS)32 and scored using a semi-quantitative scoring system (ranging from 0 to 24; AAC24)46, which assesses the linear length of the vascular calcification relative to the L1-L4 lumbar vertebra10,12,32. Body weight was measured using digital scales to the nearest 0.1 kg, and height measured using a wall-mounted stadiometer to the nearest 0.1 cm, both with participants wearing lightweight clothes and no shoes. Systolic and diastolic blood pressure (mmHg), and heart rate (bpm) were assessed five times at 1-min intervals using a validated CARESCAPETM, Dinamap v100 Vital Signs blood pressure monitor (GE Healthcare, Buckinghamshire, UK), with participants in a seated position after 5 mins rest. The first reading was discarded, and the average blood pressure of the following four readings recorded.
Biochemical measures and CVD risk
Non-fasting blood samples were collected from early morning to early afternoon at PathWest (Sir Charles Gairdner Hospital, Western Australia) on the same day as the clinic visit with serum/plasma protected from light exposure and stored at −80 °C prior to analysis. Plasma carotenoid (including its subclasses, α-carotene, β-carotene, β-cryptoxanthin, lutein, and lycopene) concentrations, biomarkers of FV consumption47 were assessed using High Performance Liquid Chromatography at the School of Biomedical Science and Pharmacy, University of Newcastle, as previously reported48,49. Total carotenoids are presented as the sum of carotenoid subclasses, except for lycopene, given its presence in high concentrations in processed tomato products, such as tomato paste, ketchup and soups50 high in salt and sugar, which would typically be determined to be unhealthy. The average inter and intra-assay % coefficient of variances for total carotenoids were 7.08 and 7.85, respectively. Serum triglycerides, total cholesterol, HDL-c, non-HDL-c, and LDL-c, and glucose concentrations were analyzed using specific ARCHITECT c-System kits from Abbott Laboratories at PathWest (Sir Charles Gairdner Hospital, Western Australia). Overall CVD risk was calculated using the Australian CVD Risk calculator (https://www.cvdcheck.org.au/calculator) to estimate a 5-year CVD risk (high ≥ 10%, moderate 5–10%, low <5%)51.
Medication and health care use
Use of prescribed and non-prescribed medication was collected using an electronic questionnaire as well as information on health care use, such as number of visits to GPs and other health care professionals, and any clinical testing or procedures requested in the previous 12 weeks. Self-reported medication use at baseline and 12-week were used to determined change in medication over 12 weeks.
Sample size
A sample size of 300 participants (n = 150 in each group) was estimated in order to have 80% power to detect a 20% difference in total carotenoids (0.45 µg/mL)48 and a difference of 40 g/d in FV intake at 12 weeks between AAC+Ed and Control+Ed, with a two-sided Type 1 error rate of alpha = 0.05.
Statistical analysis
All analyses were performed using Stata, version 15.1 (Statacorp, College Station, TX, USA). Baseline demographic data were summarized and reported as either number (%) or mean ± standard deviation (SD). Baseline and 12-week outcome margins were estimated using descriptive analyses. The primary analyses were conducted according to a modified intention to treat protocol, including all participants randomized. Differences between groups over 12 weeks for each of the outcomes were tested using mixed effects regression with fixed effects for group and time (baseline and 12 weeks) and an interaction between group and time. Marginal effects for carotenoid concentrations and FV intake over 12 weeks in each study wave were plotted following model estimation to show the point estimates and 95%CI of the outcomes for each group at each timepoint. Chi-square test was used to compare proportions of participants taking medications, accessing health care and having medical procedures (categorical). In exploratory analyses, changes in lipid and blood pressure concentrations were adjusted for change in lipid- or blood pressure lowering medication (both initiation and cessation), respectively. The association between baseline AAC scores (AAC 0–24 amount of calcification present) and the change in each outcome variable was assessed in the AAC+Ed group using Spearman Rho (ρ) to determine whether higher levels of disease led to greater changes in CVD risk factors. Independent t-test was used for the estimated difference in the change according to evidence vs. no evidence of AAC in the AAC+Ed group. Statistical significance was set at a 2-sided Type 1 error rate of α = 0.05. The required sample size of 300 was not achieved due to COVID-related issues, leaving the study with relatively lower power to detect the original hypothesized difference. We did not adjust for multiple comparisons since many of the secondary outcomes were separate hypothesis that were not closely related to one another. The trial can be considered a phase 2 trial to gather data on effectiveness and was not, therefore, large enough to allow for adjustments for multiple comparisons.
Although self-reported information on sex (male/female) has been collected, our findings have been reported for both males and females together, since stratifying the participants by sex would substantially reduce the statistical power for this study, preventing meaningful conclusions. Analyses by sex were out of the scope for this work.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The minimum dataset that is necessary to interpret, verify and extend the research in the article is provided within the manuscript and its supplementary information, which also includes the original study protocol. The data that support the findings of this study are subject to ethics approval and restrictions related to data being still collected as part of the 4-year follow-up study. Some data may become available upon reasonable request to the corresponding author, subject to ethics approval once the follow-up study has been completed. This includes individual de-identified participant information and data dictionaries such as demographic, dietary, physical activity and cardiometabolic information. Data enquiries can be directed to the corresponding author at [email protected] with response expected within a week.
References
WHO. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation. https://www.who.int/publications/i/item/924120916X (2003).
Lloyd-Jones, D. M. et al. Life’s essential 8: updating and enhancing the American Heart Association’s construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation 146, e18–e43 (2022).
Australian Bureau Of Statistics. National Health Survey. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/apparent-consumption-selected-foodstuffs-australia/2022-23 (2024).
Anokye, R. et al. Impact of vascular screening interventions on perceived threat, efficacy beliefs and behavioural intentions: a systematic narrative review. Health Promot. Int. 38, daad040 (2023).
Bengtsson, A., Lindvall, K., Norberg, M. & Fhärm, E. Increased knowledge makes a difference!–general practitioners’ experiences of pictorial information about subclinical atherosclerosis for primary prevention: an interview study from the VIPVIZA trial. Scand. J. Prim. Health Care 39, 77–84 (2021).
Orakzai, R. H. et al. Effect of patient visualization of coronary calcium by electron beam computed tomography on changes in beneficial lifestyle behaviors. Am. J. Cardiol. 101, 999–1002 (2008).
Wong, N. D. et al. Does coronary artery screening by electron beam computed tomography motivate potentially beneficial lifestyle behaviors? Am. J. Cardiol. 78, 1220–1223 (1996).
Radavelli-Bagatini, S. et al. Provision of non-invasive coronary and carotid vascular imaging results on changes in diet and physical activity in asymptomatic adults: a scoping review. Front Nutr. 9, 946378 (2022).
Schousboe, J. T. et al. Abdominal aortic calcification detected on lateral spine images from a bone densitometer predicts incident myocardial infarction or stroke in older women. J. Bone Min. Res 23, 409–416 (2008).
Schousboe, J. T., Lewis, J. R. & Kiel, D. P. Abdominal aortic calcification on dual-energy X-ray absorptiometry: methods of assessment and clinical significance. Bone 104, 91–100 (2017).
Wong, N. D. et al. Abdominal aortic calcium and multi-site atherosclerosis: the Multiethnic Study of Atherosclerosis. Atherosclerosis 214, 436–441 (2011).
Lewis, J. R. et al. Abdominal aortic calcification identified on lateral spine images from bone densitometers are a marker of generalized atherosclerosis in elderly women. Arterioscler Thromb. Vasc. Biol. 36, 166–173 (2015).
Leow, K. et al. Prognostic value of abdominal aortic calcification: a systematic review and meta‐analysis of observational studies. J. Am. Heart Assoc. 10, e017205 (2021).
Blekkenhorst, L. C. et al. Cruciferous vegetable intake is inversely associated with extensive abdominal aortic calcification in elderly women: a cross-sectional study. Br. J. Nutr. 125, 337–345 (2021).
Bondonno, N. P. et al. Dietary inflammatory index in relation to sub-clinical atherosclerosis and atherosclerotic vascular disease mortality in older women. Br. J. Nutr. 117, 1577–1586 (2017).
Parmenter, B. H. et al. Higher habitual dietary flavonoid intake associates with less extensive abdominal aortic calcification in a cohort of older women. Arterioscler. Thromb. Vasc. Biol. 42, 1482–1494 (2022).
Branch, E. COVID-19 in Western Australia, Bulletin 1: The Impact on Lifestyle. https://www.healthywa.wa.gov.au/ (2020).
Parliament of Western Australia. Review of Western Australia’s COVID-19 Management and Response. https://www.parliament.wa.gov.au/ (2023).
Litton, M. M. & Beavers, A. W. The relationship between food security status and fruit and vegetable intake during the COVID-19 pandemic. Nutrients 13, 712 (2021).
Wu, W. Y. et al. Impact of coronary artery calcium testing on patient management. J. Cardiovasc. Comput. Tomogr. 16, 303–308 (2022).
Mols, R. E. et al. Visualization of coronary artery calcification: influence on risk modification. Am. J. Med. 128, 1023.e1023–1023.e1031 (2015).
Wang, X. et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. Br. J. Nutr. 349, g4490 (2014).
McCambridge, J., Witton, J. & Elbourne, D. R. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J. Clin. Epidemiol. 67, 267–277 (2014).
Berkhout, C. et al. Defining and evaluating the Hawthorne effect in primary care, a systematic review and meta-analysis. Front. Med. 9, 1033486 (2022).
Lederman, J., Ballard, J., Njike, V. Y., Margolies, L. & Katz, D. L. Information given to postmenopausal women on coronary computed tomography may influence cardiac risk reduction efforts. J. Clin. Epidemiol. 60, 389–396 (2007).
Kalia, N. K. et al. Visualizing coronary calcium is associated with improvements in adherence to statin therapy. Atherosclerosis 185, 394–399 (2006).
Näslund, U. et al. Visualization of asymptomatic atherosclerotic disease for optimum cardiovascular prevention (VIPVIZA): a pragmatic, open-label, randomised controlled trial. Lancet 393, 133–142 (2019).
Rozanski, A. et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing: the EISNER (Early identification of subclinical atherosclerosis by noninvasive imaging research) prospective randomized trial. J. Am. Coll. Cardiol. 57, 1622–1632 (2011).
Whitmore, K. et al. Impact of patient visualization of cardiovascular images on modification of cardiovascular risk factors: a meta-analysis. JACC: Cardiovasc. Imag. 16, 1069–1081 (2023).
Jurgens, P. T. et al. Association of abdominal aorta calcium and coronary artery calcium with incident cardiovascular and coronary heart disease events in black and white middle‐aged people: the coronary artery risk development in young adults study. J. Am. Heart Assoc. 10, e023037 (2021).
Strong, J. P. et al. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the pathobiological determinants of Atherosclerosis in youth study. J. Am. Med Assoc. 281, 727–735 (1999).
Schousboe, J. T., Claflin, D. & Barrett-Connor, E. Association of coronary aortic calcium with abdominal aortic calcium detected on lateral dual energy x-ray absorptiometry spine images. Am. J. Cardiol. 104, 299–304 (2009).
Sharif, N. et al. Machine learning for abdominal aortic calcification assessment from bone density machine-derived lateral spine images. EBioMedicine 94, 104676 (2023).
Anokye, R. et al. Implementation, mechanisms of impact and key contextual factors involved in outcomes of the modification of diet, exercise and lifestyle (MODEL) randomised controlled trial in Australian adults: protocol for a mixed-method process evaluation. BMJ Open 10, e036395 (2020).
Radavelli-Bagatini, S. et al. Modification of diet, exercise and lifestyle (MODEL) study: a randomised controlled trial protocol. BMJ Open 10, e036366 (2020).
Orkin, A. M. et al. Guidelines for reporting trial protocols and completed trials modified due to the COVID-19 pandemic and other extenuating circumstances: the CONSERVE 2021 statement. J. Am. Med Assoc. 326, 257–265 (2021).
Lewis, J. R. et al. Long‐term atherosclerotic vascular disease risk and prognosis in elderly women with abdominal aortic calcification on lateral spine images captured during bone density testing: a prospective study. J. Bone Min. Res 33, 1001–1010 (2018).
StataCorp, L. Stata Statistical Software (Version Release 14). https://www.scirp.org/reference/ReferencesPapers?ReferenceID=1858523 (2015).
Ryan, P. Random allocation of treatments balanced in blocks: update. south Australia. Stat. Tech. Bull. STB 54, 49 (2000).
Heart Foundation. Heart Healthy Eating Principles. https://www.heartfoundation.org.au/for-professionals/food-and-nutrition/heart-healthy-eating-principles (2017).
NHMRC. Australian Dietary Guidelines. Australian Government, Canberra. https://www.health.gov.au (2013).
Heidari, S., Babor, T. F., De Castro, P., Tort, S. & Curno, M. Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr. Peer Rev. 1, 1–9 (2016).
Ireland, P. et al. Development of the Melbourne FFQ: a food frequency questionnaire for use in an Australian prospective study involving an ethnically diverse cohort. Asia Pac. J. Clin. Nutr. 3, 19–31 (1994).
Thorpe, M. G., Milte, C. M., Crawford, D. & McNaughton, S. A. A revised Australian dietary guideline index and its association with key sociodemographic factors, health behaviors and body mass index in peri-retirement aged adults. Nutrients 8, 160 (2016).
Stewart, A. L. et al. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med. Sci. Sports Exerc. 33, 1126–1141 (2001).
Kauppila, L. I. et al. New indices to classify ___location, severity and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis 132, 245–250 (1997).
Andersen, L. F. et al. Evaluation of three dietary assessment methods and serum biomarkers as measures of fruit and vegetable intake, using the method of triads. Br. J. Nutr. 93, 519–527 (2005).
Blekkenhorst, L. C. et al. Nitrate-rich vegetables do not lower blood pressure in individuals with mildly elevated blood pressure: a 4-wk randomized controlled crossover trial. Am. J. Clin. Nutr. 107, 894–908 (2018).
Wood, L. G. et al. Manipulating antioxidant intake in asthma: a randomized controlled trial. Am. J. Clin. Nutr. 96, 534–543 (2012).
Agarwal, S. & Rao, A. V. Tomato lycopene and its role in human health and chronic diseases. Cmaj 163, 739–744 (2000).
AusCVDrisk. Australian Guideline and Calculator for Assessing and Managing Cardiovascular Disease Risk. https://www.cvdcheck.org.au/ (2023).
Schousboe, J. T., Wilson, K. E. & Kiel, D. P. Detection of abdominal aortic calcification with lateral spine imaging using DXA. J. Clin. Densitom. 9, 302–308 (2006).
Acknowledgements
The investigators thank the organizations and individuals who helped develop, improve and publicize this study, in particular Mr. Ben Horgan, former Consumer and Community Involvement Coordinator from Edith Cowan University, and the community representatives (Mrs. Barbara Horgan and Mrs. Kathleen Joy Foyle) involved in this research project. We gratefully acknowledge Mrs. Lyn McCahon who worked as a research assistant on the study. This research received funding from an MRFF Preventive and Public Health grant, APP1199751 (2020-2023). CPB was supported by a Royal Perth Hospital Research Foundation Lawrie Beilin Career Advancement Fellowship (ID: CAF 127/2020) and the Western Australian Future Health Research and Innovation Fund (ID: IG2021/5). MS was supported by a Royal Perth Hospital Research Foundation Fellowship (RPHRF CAF 00/21) and an Emerging Leader Fellowship from the Western Australian Future Health Research and Innovation Fund. LCB was supported by a National Health and Medical Research Council (NHMRC) of Australia Emerging Leadership Investigator Grant (ID: 1172987) and a National Heart Foundation of Australia Post-Doctoral Research Fellowship (ID: 102498). ELC was supported by an Australian Government Research Training Program Scholarship at Edith Cowan University. JRL was supported by a National Heart Foundation Future Leader Fellowship (ID: 102817). JMH was supported by an NHMRC of Australia Senior Research Fellowship (ID 1116973). DPK received grants to his institution from Amgen, Radius Health, and Solarea Bio. DPK serves on scientific advisory boards for Solarea Bio, Radius Health and received royalties for publication in UpToDate from Wolters Kluwer. None of the funding agencies had any role in the conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
S.R.B., J.R.L., J.M.H., C.P.B., Ma.S., R.M.D. contributed to the conception and design of the work; S.R.B., C.P.B., J.D.V., Ma.S. and A.K.G. contributed to the acquisition of data. C.P.B., J.D.V. and Ma.S. performed the follow-up calls. K.Z. coordinated and supervised the bone density scans and reporting of the DXA scans. J.T.S. read and scored the AAC images. S.R.B. and R.J.W. performed the data analysis. S.R.B., C.P.B., J.D.V., Ma.S., A.K.G., L.C.B., E.L.C., N.P.B., J.T.S., R.J.W., K.Z., S.M., P.S., B.J., J.D., M.P.S., K.L.C., D.P.K., W.H.L., M.St., A.D., P.L.T., E.J.W., L.G.W., Mo.S., R.M.D., J.M.H., J.R.L. contributed to the interpretation of data, revised and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Robert Makuch, Jayne Woodside and the other, anonymous, reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Radavelli-Bagatini, S., Bondonno, C.P., Dalla Via, J. et al. Impact of provision of abdominal aortic calcification results on fruit and vegetable intake: 12-week randomized phase 2 controlled trial. Nat Commun 15, 8126 (2024). https://doi.org/10.1038/s41467-024-52172-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-52172-1