Abstract
The emergence of Rocahepevirus ratti genotype 1 (rat hepatitis E virus; rat HEV) in humans presents an unprecedented threat; however, the risk of rat HEV transmission to humans is not well understood. Here, we report the “Distinguishing Antibody Response Elicitation (DARE)” method, which distinguishes exposure to rat HEV. We use four study sets from China for large-scale population analysis: set 1 (hospital visit) and set 3 (ALT abnormality) from Yunnan province, a biodiversity hotspot, and set 2 (received physical examination) and set 4 (ALT abnormality) from Jiangsu province, a non-hotspot control region. rat HEV exposure risk is significantly higher in Yunnan, with 21.97% (190 of 865) in set 1 and 13.97% (70 of 501) in set 3, compared to 0.75% (9 of 1196) in Jiangsu’s set 2. Six spillover infections for rat HEV are identified in set 1, with one case of abnormal ALT. The rat-1d strains carried by rats are closely related to those human infections. Our study reveals the substantial spillover burden posed by rat HEV in biodiversity hotspots and highlights the utility of DARE method for proactive surveillance of public health emergencies.
Similar content being viewed by others
Introduction
Rats, a species of rodent, serve as natural reservoirs for medically important pathogens, including hantavirus and arenavirus, which cause severe hemorrhagic fever in humans, and Yersinia pestis, which causes plague across Asia, Europe, and the Americas1,2,3. The viral diversity and abundance in rats can create favorable conditions for the emergence of new or known highly virulent viruses4,5. Commensal rats are distributed worldwide, with human exposure to rats documented in Asia6,7,8,9, Europe10,11, the Americas12,13,14 and Africa15. In rat hotspots, 90% of respondents reported observing rats in or around their households and frequently coming into contact with them6. Hantaviral disease outbreaks have been linked to fluctuations in rodent population densities16. Epidemiological studies have linked the extent of hantaviral exposure to closer contact between rats and humans. Outdoor hantaviral exposure has been associated with activities such as intense farm labor, threshing, sleeping on the ground, and military exercises, while indoor exposure is linked to rats invading homes during colder months or nesting near dwellings17,18. The aerosol route is the primary mode of hantaviral transmission between rats and humans, while virus transmission through bites may occur among some rats and occasionally lead to human infection19,20. Hantaviral exposure are more common among individuals of lower socioeconomic status due to poorer housing and agricultural activities that increase rat-human contact. However, suburbanization and outdoor recreational activities have also exposed middle- and upper-income individuals to the pathogen. Additionally, landscape disturbance in biodiversity regions increases human-rat contact, enhancing the spillover of infectious diseases21. Zoonotic viral transmission from rats to humans poses significant public health threats.
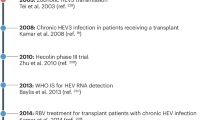
Rats serve as a natural host of Rocahepevirus ratti genotype 1 (rat hepatitis E virus; rat HEV). Rat HEV has been identified in rats across multiple countries/regions, including Asia (12 countries/regions, such as China, Japan, Indonesia, Vietnam, and Mongolia), Europe (19 countries/regions, such as Spain, Germany, France, the United Kingdom, and Italy), the Americas (four countries/regions, including the United States, Canada, Mexico, and Brazil), and Africa (five countries/regions, including Nigeria, Kenya, Sierra Leone, Guinea, and Ethiopia)14,22,23,24,25,26,27. Rat HEV was previously thought to be limited to rodents, with rodent hosts projected to be the nonrecent evolutionary origins of human-pathogenic HEV28. However, thirty-seven cases of rat HEV infection (19 in Hong Kong and Hainan, China29,30,31,32,33,34, 1 in Central Africa35, 1 in France36, and 16 in Spain37,38,39,40,41) have been reported worldwide since 2018, challenging this assumption. The zoonotic nature of rat HEV is demonstrated via strain analysis of rats and humans from the same district31. The spillover of rat HEV represents an unusual and unprecedented threat to humans42. Most people living with rat HEV are unaware that they have it. Previous studies reported that rat HEV infection accounted for 0.27% (6 of 2201) in a set of hepatitis patients in Hong Kong, China31 and 1.12% (3 of 267) in a Spanish cohort of hepatitis patients37. Acute rat hepatitis E was found in people living with HIV, children and drug user in Spain38,39,40. These findings highlight the viral hepatitis burden caused by rat HEV infection. In China, rat HEV RNA was detectable in 19.1% (13/68) and 20.19% (124/614) of rat liver tissue samples9,43. If rat HEV becomes more transmissible, it could pose a risk for larger outbreaks or a pandemic. The spillover burden of rat HEV in humans remains undetermined, suggesting the need for conventional rat HEV exposure testing in human-rat hotspots.
Rat HEV is partly antigenically similar to Paslahepevirus balayani (balayani hepatitis E virus; b HEV). Cross-genus antibody response may exist in persons exposed to either rat HEV or b HEV due to ~50% amino acid (aa.) identity, complicating the assessment of rat HEV spillover burden in humans44. Given these issues, it is crucial to distinguish the antibody response elicited by either rat HEV or b HEV exposure. Studies have shown that persons exposed to HEV maintain anti-HEV IgG positivity for at least five years, whereas they might significantly lose detectable anti-HEV IgG after ten years45,46. Therefore, the “distinguishing antibody response elicitation (DARE)” method was developed to address the blind spot in assessing human global spillover burden to rat HEV.
Yunnan, a Province on China’s southwestern land border, shares cultural and geographical connections to Myanmar, Laos, and Vietnam in mainland Southeast Asia, a region known as a biodiversity hotspot21. This geographical area is an epidemic center for the emergence of viruses posing significant public health threats47. In this region, a high prevalence of b HEV has been reported in humans, cows, and goats due to traditional mixed farming practices48,49. Additionally, ~20% prevalence of rat HEV was observed in wild rats43. Jiangsu, a Province on China’s eastern coast, is endemic for b HEV infection, with ~50% of persons tested being seropositive50,51. In this region. The coastal region is more urbanized and can serve as a valuable control for biodiversity hotspots. By analyzing biodiversity hotspots in Yunnan Province and in Jiangsu Province, our study aimed to understand the spillover of rat HEV from rats to humans and shed light on the spillover burden of rat HEV in humans to better prevent outbreaks and pandemics.
Results
Antibody response analysis
HEV 239 protein (p239) is a truncated form of the capsid protein that self-assembles into virus-like particles (VLPs) and mimics the conformation of natural HEV particles52. We first detected HEV IgG levels in rat and b HEV RNA-positive serum samples using recombinantly expressed ratti HEV genotype 1 (r-1; rat) p239 and b HEV genotype 4 (b-4) p239 coated in microplates. The clinical properties of rat and b HEV-infected patients are listed in Table S1. Based on the OD values of anti-HEV IgG for rat p239 and b-4 p239, we created a two-dimensional (2D) scatter plot. We observed that the OD values of most samples reached the upper plateau range, making it difficult to distinguish the true HEV IgG levels (Fig. 1A). We next used serially diluted samples to detect. Among rat HEV RNA-positive samples, 22.22% (2 of 9) of the samples showed significantly higher anti-rat HEV IgG levels than anti-b-4 HEV IgG, while 44.44% (four of nine) of the samples showed comparable anti-HEV IgG titer levels between rat p239 and b-4 p239. Anti-b-4 HEV IgG was undetectable in 33.33% (three of nine) of the samples (Fig. 1A). In b HEV RNA-positive samples, 78.6% (11 of 14) showed significantly higher anti-b-4 HEV IgG levels than anti-rat HEV IgG, and 21.4% (3 of 14) of the samples showed comparable anti-HEV IgG titer levels between rat p239 and b-4 p239 (Fig. 1A). A previous study reported an immunoassay system to differentiate rat HEV- and b HEV-infected patient samples based on the anti-HEV IgG ratio of 2.947 (ODb-4/ODrat)53. The immunoassay system was developed using individuals with active rat HEV infection and b HEV infection, which limits the utility of the anti-HEV IgG ratio of ODb-4/ODrat when applied to convalescent sera. Another limitation of this system is that it can be confusing when serum samples show comparable anti-HEV IgG levels between rat p239 and b-4 p239. Due to the high prevalence of b HEV in humans54, individuals are likely to have been exposed to both b HEV and rat HEV (dual exposure), exhibiting comparable anti-HEV IgG titer levels in serum samples. An overlapping range of b-4/rat values of 100 was found in samples from b and rat HEV RNA-positive patients (Fig. 1A), suggesting possible dual immunogen exposure. These results highlight that it is crucial to distinguish the antibody response elicited by either rat HEV, b HEV, or both HEV.
Two-dimensional scatter plot of HEV IgG levels in HEV RNA-positive samples (A), immunized BALB/c samples at week 4 (B), and infected gerbil samples at week 6 (C). HEV IgG levels were evaluated using serial dilutions of serum samples. Samples were simultaneously tested with rat p239 (blue dots) and b−4 p239 (red dots). The X-axis represents anti-rat HEV IgG titer levels; the Y-axis represents anti-b−4 HEV IgG titer levels. Healthy controls were individuals unexposed to either HEV. Each serum sample was tested in duplicate. The dashed line indicates the HEV IgG assay cutoff, defined as 2.5 times the mean reading of healthy control samples. Binding trends for anti-rat and anti-b−4 HEV IgG were evaluated in HEV RNA-positive samples (A), immunized BALB/c samples at week 4 (B), and infected gerbil samples at week 6 (C). The ratio values of anti-rat HEV IgG titer levels divided by anti-b−4 HEV IgG titer levels were calculated to assess HEV exposure characteristics in various situations. Initial exposure to b HEV (red) or rat HEV (blue) immunogens for BALB/c samples and gerbil samples are shown, with a single and dual exposures designated as circles and squares, respectively. Source data are provided as a Source Data file. b HEV species HEV balayani, b-1 species HEV balayani-1, b-3 species HEV balayani-3, b−4 species HEV balayani−4, HEV hepatitis E virus, rat HEV species HEV ratti-1.
To exclude unknown background interference, BALB/c mice were vaccinated with HEV p239 immunogen using multiple schemes (Fig. S1A). Vaccination of mice with either a single (b-1, b-4, rat) or dual (b-41st/rat2nd, rat1st/b-42nd) immunogen was designed to simulate naturally occurring HEV exposure. Anti-rat and anti-b-4 IgG titer levels in serum samples were detected weekly, with increased IgG titer levels (Fig. S1B). Overlapping clusters were observed in samples vaccinated with single and dual immunogens based on OD values (Fig. 1B). We next used serially diluted samples to detect. Samples formed separated clusters on the 2D scatter plot when classified according to the immunogen to which they were first exposed, with clear demarcation. However, samples from single and dual immunogen groups with the same initial exposure showed overlapping clusters, with no demarcation (Fig. 1B). We assessed the ratio (b-4/rat value) of anti-HEV IgG titer levels to further quantitatively visualize the characteristics of HEV exposure. A b-4/rat value of 100 was able to distinguish samples with different initial exposures (Fig. 1B). In the case of the same initial immunogen exposure, samples from a secondary heterologous immunogen exposure did not significantly increase in IgG titers to heterologous immunogens due to immune imprint. This resulted in overlapping clusters on the 2D scatter plot with similar ratio values (Fig. 1B). A b-4/rat value of higher than 102 or lower than 10−2 was able to distinguish samples from groups with a single (b-1, b-4) and dual (b-41st/rat2nd) immunogen exposure, as well as samples from groups with a single (rat) and dual (rat1st/b-42nd) immunogen exposure. However, samples with ratio values between 102 and 10−2 could not be distinguished (Fig. 1B).
Mongolian gerbils are highly susceptible to both b HEV and rat HEV infections55,56,57. The gerbil model can be used to mimic typical antibody response features in humans and exclude potential background interference in patients. Gerbils were challenged with HEV using multiple schemes (Fig. S2A). Infection of gerbils with either a single (b-3, rat) or dual (b-3/ratco-infection) HEV was designed to simulate naturally occurring HEV exposure. Anti-rat and anti-b-4 IgG titer levels in serum samples were detected weekly, with increased IgG titer levels (Fig. S2B). Separated clusters on the 2D scatter plot were observed in gerbil samples infected with single HEV and co-infected with dual HEV based on OD values and titer levels (Fig. 1C). We assessed the ratio (b-4/rat value) of anti-HEV IgG titer levels to further quantitatively visualize the characteristics of HEV exposure. A b-4/rat value of higher than 101 or lower than 10−1 was able to distinguish gerbil samples from groups with a single (b-3, rat) and dual (b-3/ratco-infection) HEV exposure (Fig. 1C). Considering the b-4/rat values generated in vaccinated BALB/c and infected gerbil samples, a robust b-4/rat value of higher than 102 or lower than 10−2 potentially identify single HEV exposure (b HEV or rat HEV). However, we sought to address this issue by developing a reliable and effective method to distinguish the antibody response elicited by rat HEV exposure.
DARE method establishment
We developed a method called DARE (Fig. 2A). Samples from a single immunogen exposure were categorized as either b HEV-elicited IgG response (HEVb IgG response) or rat HEV-elicited IgG response (HEVrat IgG response). Samples from dual immunogen exposure were classified as both rat and b HEV-elicited IgG response (HEVrat and b IgG response). Three samples from the same individual were separately incubated with two p239-linked magnetic beads and unlinked magnetic beads. After the adsorption process was completed, the three samples from the same individual were independently added to two p239-coated microplates. If the individual had an HEVrat IgG response, their sera might contain IgG that specifically recognized rat p239 while showing undetectable or cross-reactive IgG against b-4 p239. It was expected that rat p239-linked magnetic beads would completely absorb the IgG from the HEVrat response, resulting in almost complete blocking of binding to the two p239-coated microplates. On the other hand, b-4 p239-linked magnetic beads would only adsorb a small portion of cross-reactive IgG from the HEVrat response, leading to partial blocking of binding to rat p239-coated microplates and almost complete blocking of binding to b-4 p239-coated microplates. If the individual had a HEVb IgG response, the situation would be reversed. If the individual had a HEVrat and b IgG response, their sera might contain IgG that specifically recognized rat p239 and b-4 p239, while also showing undetectable or cross-reactive IgG. In this case, rat p239-linked magnetic beads would adsorb cross-reactive IgG and IgG that specifically recognized rat p239, resulting in almost complete blocking of binding to rat p239-coated microplates and partial blocking of binding to b-4 p239-coated microplates. On the other hand, b-4 p239-linked magnetic beads would adsorb cross-reactive IgG and IgG that specifically recognizes b-4 p239, leading to partial blocking of binding to rat p239-coated microplates and almost complete blocking of binding to b-4 p239-coated microplates.
A Establishment of the DARE method. The overall scheme is shown. Before detecting anti-rat and anti-b−4 HEV IgG simultaneously, three samples from the same individual were separately incubated with two p239-linked magnetic beads and unlinked magnetic beads. After the adsorption process, the three samples from the same individual were independently added to two p239-coated microplates. B Adsorption of serum samples from immunized BALB/c at week 4. Samples were separately incubated with rat p239- and b−4 p239-linked magnetic beads, then simultaneously tested in rat p239 and b-4 p239. Samples adsorbed to unlinked magnetic beads served as controls. C Algorithm setup. The ODadsorbed/ODnon ratio values, representing the OD values after adsorption with two p239-linked magnetic beads (ODadsorbed) divided by the OD values after adsorption with one unlinked magnetic beads (ODnon), were calculated to analyze the exposure situation. An ODadsorbed/ODnon ratio value of 0.35 was used to identify the IgG response, effectively distinguishing between single and dual immunogen/HEV recent exposures. Blue boxes represent samples incubated with p239-linked magnetic beads, where an ODadsorbed/ODnon ratio value is greater than 0.35 (insufficient adsorption). Red boxes represent samples incubated with p239-linked magnetic beads, where an ODadsorbed/ODnon ratio value is less than or equal to 0.35 (sufficient adsorption). Source data are provided as a Source Data file. b HEV species HEV balayani, b−1 species HEV balayani-1, b−4 species HEV balayani−4, DARE distinguishing antibody response elicitation, GA gray area, HEAg hepatitis E virus antigen, HEV hepatitis E virus, Neg. negative, rat HEV species HEV ratti-1.
Based on the above principles, we used mouse samples for identifying IgG response using DARE. As expected, our DARE method preliminarily distinguished mouse samples with a single or dual immunogen exposure based on the changes in IgG (Fig. 2B). Mouse samples with a single and dual immunogen exposure, were further analyzed to assess the characteristics of HEV exposure by evaluating the b-4/rat ratio values. The ODadsorbed/ODnon ratio values, representing the OD values after adsorption with two p239-linked magnetic beads (ODadsorbed) divided by the OD values after adsorption with one unlinked magnetic beads (ODnon), were calculated to analyze the exposure situation. An ODadsorbed/ODnon ratio value of 0.35 was used to identify the IgG response, effectively distinguishing between a single and dual immunogen/HEV recent exposures in samples (Fig. 2C). These results demonstrated that our DARE method can effectively distinguish individuals with a single or dual HEV exposure.
DARE method validation
Given the unknown accuracy of the established DARE method, the previously reported immunoblot method was applied to validate in immunized BALB/c samples44,53. None (0 of 6) of the samples from PBS immunized BALB/c exhibited a visible band at parallel b-4 p239 and rat p239 immunoblots (Fig. 3A), demonstrating the specificity of the DARE method. Among samples from b-1 and b-4 immunized BALB/c, 50% (three of six) and 83.33% (five of six), respectively, reacted exclusively with b-4 p239 immunoblot and did not cross-react with rat p239 immunoblot (Fig. 3A). Additionally, 66.67% (four of six) of samples from rat immunized BALB/c reacted exclusively with rat p239 immunoblot and did not cross-react with b-4 p239 immunoblot (Fig. 3A). Since the immunoblot method was developed without considering the possibility of dual exposure, we hypothesize that positive visible bands on both the parallel b-4 p239 and rat p239 immunoblots indicate HEVrat and b IgG response. It is important to note that this hypothesis may incorrectly classify BALB/c samples immunized with a single antigen as dual immunized. Among samples from b-41st/rat2nd and rat1st/b-42nd immunized BALB/c, 66.67% (four of six) and 50% (three of six) of sera cross-reacted with b-4 p239 and rat p239 immunoblots (Fig. 3A).
A Immunoblot using immunized BALB/c samples at week 4. Immunoblot was used to validate the accuracy of the DARE method established with immunized BALB/c samlpes at week 4. Parallel b−4 p239 and rat p239 immunoblots were conducted using immunized BALB/c samples at week 4 to identify HEV antibody response. M represents the lane labeled with the marker. P indicates the positive control, representing the lane labeled with an antibody that cross-reacts with both b HEV and rat HEV. Two times each experiment was repeated independently with similar results. B Algorithm validation using infected gerbil samples at week 6. An ODadsorbed/ODnon ratio value of 0.35 was used in the algorithm setup to identify the IgG response, effectively distinguishing immunized BALB/c samples at week 4 between single and dual immunogen/HEV recent exposures. Infected gerbil samples at week 6 were used to validate the algorithm setup with an ODadsorbed/ODnon ratio value of 0.35. Blue boxes represent samples incubated with p239-linked magnetic beads, where an ODadsorbed/ODnon ratio value is greater than 0.35 (insufficient adsorption). Red boxes represent samples incubated with p239-linked magnetic beads, where an ODadsorbed/ODnon ratio value is less than or equal to 0.35 (sufficient adsorption). C Immunoblot using infected gerbil samples at week 6. An immunoblot was used to validate the accuracy of the DARE method established with immunized BALB/c at week 4. Parallel b−4 p239 and rat p239 immunoblots were conducted using infected gerbil samples at week 6 to identify HEV antibody response. M represents the lane labeled with the marker. P indicates the positive control, representing the lane labeled with an antibody that cross-reacts with both b HEV and rat HEV. Two times each experiment was repeated independently with similar results. Source data are provided as a Source Data file. b HEV species HEV balayani, b-1 species HEV balayani-1; b-3 species HEV balayani-3, b−4 species HEV balayani−4, DARE distinguishing antibody response elicitation, HEV hepatitis E virus, rat HEV species HEV ratti-1.
Since BALB/c samples from week 4 post-immunization were still in the phase of a steady increase in antibody response, which could limit the credibility of the DARE method established by the immunization model. Serum samples from immunized BALB/c at week 6, with steady antibody response levels, were validated in parallel using the DARE method and the immunoblot method. An ODadsorbed/ODnon ratio value of 0.35 established using immunized BALB/c samples at week 4 was used in the algorithm to identify the IgG response, effectively distinguishing between single and dual immunogen/HEV recent exposures in immunized BALB/c samples at week 6 (Fig. S3A). None (0 of 6) of the BALB/c samples at week 6 exhibited a visible band at parallel b-4 p239 and rat p239 immunoblots (Fig. S3B). Among samples from week 6 of b-1 and b-4 immunized BALB/c, 16.67% (1 of 6) and 100% (6 of 6), respectively, reacted exclusively with b-4 p239 immunoblot and did not cross-react with rat p239 immunoblot (Fig. S3B). Additionally, 33.33% (2 of 6) of samples from week 6 of rat immunized BALB/c reacted exclusively with rat p239 immunoblot and did not cross-react with b-4 p239 immunoblot (Fig. S3B). Among samples from week 6 of b-41st/rat2nd and rat1st/b-42nd immunized BALB/c, 100% (6 of 6) and 100% (6 of 6) of sera cross-reacted with b-4 p239 and rat p239 immunoblots (Fig. S3B).
The gerbil infection model can be used to mimic typical antibody response features in humans and was also validated in parallel using the DARE method and the immunoblot method. An ODadsorbed/ODnon ratio value of 0.35 established using immunized BALB/c samples at week 4 was used in the algorithm to identify the IgG response, effectively distinguishing between single and dual immunogen/HEV recent exposures in infected gerbil samples (Fig. 3B). Among samples from b-3 infected gerbil, 40% (2 of 5) of sera reacted exclusively with b-4 p239 immunoblot and did not cross-react with rat p239 immunoblot (Fig. 3C). Additionally, 33.33% (1 of 3) of samples from rat infected gerbil reacted exclusively with rat p239 immunoblot and did not cross-react with b-4 p239 immunoblot (Fig. 3C). Among samples from b-3/ratco-infection infected gerbil, 100% (3 of 3) of sera cross-reacted with b-4 p239 and rat p239 immunoblots (Fig. 3C). These results demonstrate that the DARE method has higher sensitivity and comparable specificity to the immunoblot method.
The algorithm of the DARE method
To further facilitate the reliability and convenience of the DARE method for large populations, a set of optimized workflows and algorithms is proposed based on rigorous experimental data (Fig. 4). Samples from large populations were preliminarily tested for anti-rat and anti-b-4 HEV IgG. Samples negative for both anti-rat and anti-b-4 HEV IgG were considered as having either no exposure or having had a short time or a long time since the last exposure. If a sample is only anti-rat IgG positive or only anti-b-4 IgG positive, it is designated as HEVrat IgG response (indicating rat HEV exposure within the recent 5 years) or HEVb IgG response (indicating b HEV exposure within the recent 5 years), respectively. Further specificity test (*, #) is required to determine the specificity of binding. An ODadsorbed value (using the same p239-linked magnetic beads as the p239-coated microplate) less than or equal to the cutoff, or an ODadsorbed/ODnon ratio value less than or equal to 0.7 (twice the value of distinguishing algorithm) is used for identification. For samples positive for both anti-rat and anti-b-4 HEV IgG, weakly positive samples can interfere with the identification of the IgG response. This is a limitation of our DARE method, so we defined samples with both anti-rat and anti-b-4 HEV IgG OD values less than 1.5 (cutoff/0.35) as unrecognizable exposure. Samples with both anti-rat and anti-b-4 HEV IgG OD values higher than 1.5 could be identified as HEVrat IgG response, HEVrat and b IgG response (indicating both rat and b HEV exposure within the recent 5 year) or HEVb IgG response based on the specificity test and the algorithm (label 1, 2, and 3). The remaining samples (ODanti-rat IgG ≥ 1.5 and ODanti-b-4 IgG < 1.5, ODanti-rat IgG < 1.5 and ODanti-b-4 IgG ≥ 1.5) that were positive for both anti-rat and anti-b-4 HEV IgG could be identified as HEVrat IgG response or HEVb IgG response based on the specificity test and the algorithm for IgG OD values higher than 1.5. In addition, for these remaining samples, a b-4/rat value of anti-HEV IgG titer levels higher than 102 or less than 10−2 can be directly designated as HEVb IgG response or HEVrat IgG response. For samples with high HEV IgG levels, the ODadsorbed value (using the same p239-linked magnetic beads as the p239-coated microplate) must meet the specificity test. If it does not, the DARE method needs to be repeated with diluted serum samples for accurate HEV IgG response identification.
The algorithm was based on rigorous experimental data. To further facilitate the reliability and the convenience of the DARE method in large populations, an optimized workflow and algorithm are proposed. In the figure, the labels 1, 2, and 3 indicate the algorithms applied when ODanti-rat and b−4 IgG ≥ 1.5. Label 1 corresponds to the condition where ODb-4-adsrobed/ODnon-adsorbed > 0.35 (anti-rat IgG) and ODrat-adsrobed/ODnon-adsorbed ≤ 0.35 (anti-b-4 IgG), which is designated as HEVrat IgG response. Label 2 corresponds to the condition where ODb-4-adsrobed/ODnon-adsorbed ≤ 0.35 (anti-rat IgG) and ODrat-adsrobed/ODnon-adsorbed > 0.35 (anti-b-4 IgG), which is designated as HEVb IgG response. Label 3 represents all cases except those of labels 1 and 2, which is designated as HEVrat and b IgG response. For the cases where ODanti-rat IgG ≥ 1.5 and ODanti-b-4 IgG < 1.5, different algorithms are applied. Label 1 corresponds to the condition where ODb-4-adsrobed/ODnon-adsorbed > 0.35 (anti-rat IgG) or anti-rat/anti-b-4 IgG titers > 102, which is designated as HEVrat IgG response. All other conditions are designated as unrecognizable exposure. For the cases where ODanti-rat IgG < 1.5 and ODanti-b-4 IgG ≥ 1.5, different algorithms are applied. Label 1 corresponds to the condition where ODrat-adsrobed/ODnon-adsorbed > 0.35 (anti-b-4 IgG) or anti-b-4/anti-rat IgG titers >102, which is designated as HEVb IgG response. All other conditions are designated as unrecognizable exposure. b HEV species HEV balayani, b-4 species HEV balayani-4, DARE distinguishing antibody response elicitation, HEV hepatitis E virus, OD optical density, QC quality control, rat HEV species HEV ratti−1.
Burden of rat HEV spillover
To gauge the exposure risk of rat HEV, population samples were collected from two sets: set 1 from Menghai, a city on China’s southwestern border in Yunnan province, and set 2 from Dongtai, a city on China’s eastern coast in Jiangsu province.
In set 1, preliminary anti-HEV IgG testing showed that 55.49% (480 of 865) of individuals were positive for anti-rat or anti-b-4 HEV IgG (Fig. 5). We identified samples with both anti-rat and anti-b-4 HEV IgG OD values less than 1.5 as unrecognizable exposure, accounting for 4.28% (37 of 865) of set 1. Using the DARE method, we analyzed individuals who were positive for only anti-rat IgG, only anti-b-4 IgG, and those who were positive for both anti-rat and anti-b-4 IgG based on the specificity test and the algorithm (Fig. S4A–J). In set 1, HEV exposures were comprehensively documented, with 21.97% (190 of 865) showing rat HEV exposure, 5.43% (47 of 865) showing both rat and b HEV exposure and 23.82% (206 of 865) showing b HEV exposure (Fig. 5). To confirm the accuracy of the DARE method in human population samples, we applied the previously developed immunoblot method to five types of samples distinguished by the DARE method44,53. These serum samples were randomly selected. None (0 of 41) of sera from individuals with anti-HEV IgG negative exhibited visible band at parallel b-4 p239 and rat p239 immunoblots (Fig. S5), demonstrating specificity of the DARE method. Additionally, none (0 of 36) of the sera from individuals with unrecognizable exposure showed a visible band (Fig. S6), further highlighting the higher sensitivity of the DARE method. Among sera from individuals with HEVrat IgG response, 24.44% (11 of 45) of sera only reacted with rat p239 immunoblot and did not cross-react with b-4 p239 immunoblot (Fig. S7). Among sera from individuals with HEVb IgG response, 4.44% (2 of 45) of sera only reacted with b-4 p239 immunoblot and did not cross-react with rat p239 immunoblot (Fig. S8). Among sera from individuals with HEVrat and b IgG response, 5.56% (2 of 36) of sera cross-reacted with b-4 p239 and rat p239 immunoblots (Fig. S9). These results support that the DARE method has higher sensitivity and comparable specificity to the immunoblot method.
The summary of HEV spillover risk and infection in the two sets is displayed on the left and right, respectively. Purple boxes represent the results of a preliminary test using anti-HEV IgG assays. Gray boxes represent identification of anti-HEV IgG negative individuals and unrecognizable exposure. Blue boxes represent identification of HEVrat, HEVrat and b, and HEVb IgG responses using the DARE method. Additionally, red boxes represent results of HEV nucleic acid testing. Source data are provided as a Source Data file. b HEV species HEV balayani, b−4 species HEV balayani−4, HEV hepatitis E virus, NAT nucleic acid testing, rat HEV species HEV ratti−1.
In set 2, preliminary anti-HEV IgG testing showed that 39.72% (475 of 1196) of individuals were positive for anti-rat or anti-b-4 HEV IgG (Fig. 5). No unrecognizable exposure was identified. The specificity test and algorithm revealed that 0.75% (9 of 1196) had rat HEV exposure, 0.33% (4 of 1196) had both rat and b HEV exposure, and 38.63% (462 of 1196) had b HEV exposure (Fig. 5 and Fig. S10A–G). The profiles of HEV exposure differed significantly between set 1 and set 2, indicating that rat HEV is endemic in humans and spreads regionally. The spillover burden posed by rat HEV is notably higher in the hotspot.
We further analyzed the demographic characteristics of the HEV IgG response in the two sets. Compared to anti-HEV IgG negative individuals, we found that individuals with HEVrat IgG response, HEVb IgG response, or both HEVrat and b IgG response generally had an older median age, except for those with HEVrat IgG response in set 2 (Table 1). Cochran-Armitage trend test revealed significant differences in age distribution. In the two sets, the proportion of individuals with HEVrat and b IgG response and HEVb IgG response increased with age, demonstrating higher HEV and b HEV exposure with age. In set 1, the subgroup aged 20–29 with HEVrat IgG response had a higher composition ratio compared to those with HEVb IgG response or HEVrat and b IgG response. Conversely, the subgroup aged 60 and above showed a lower composition ratio than the other two subgroups. This suggests that, unlike b HEV whose prevalence increases with age, the prevalence of rat HEV may be due to specific exposure patterns among younger individuals. We also conducted a retrospective analysis of laboratory test indicators over the past five years for set 1 (Table 2). Individuals with indicators at two or more time points (more than two months apart) were included, accounting for 13.3% (115 of 865) of set 1. The proportion of individuals with an IgG response or anti-HEV IgG negative roughly matches that of set 1. During the retrospective period, abnormal ALT levels were observed in 39.5% (15 of 38) of individuals with rat HEV exposure, 60.0% (6 of 10) of those with both rat and b HEV exposure, 63.0% (17 of 27) of those with b HEV exposure and 22.5% (9/40) of those with anti-HEV IgG negative. The relative risks (RRs) were 1.76, 2.67, and 2.80, respectively. This indicates that rat HEV infection in humans increases the hepatitis burden.
Spillover infection of rat HEV to humans
In set 1, 0.69% (6 of 865) of individuals had detectable rat HEV RNA (Fig. 5). Among these six individuals, 33.33% (2 of 6) had HEVrat IgG response, 50% (2 of 6) had HEVrat and b IgG response, 16.67% (1 of 6) had unrecognizable exposure, and 16.67% (1 of 6) were anti-HEV IgG negative. In set 2, 0.25% (3 of 1196) of individuals had detectable b HEV RNA. Among these three individuals, 33.33% (1 of 3) had an HEVb IgG response, and 66.67% (2 of 3) were anti-HEV IgG negative. These findings indicate the infection risk posed by rat HEV is significantly higher in the hotspot.
We amplified a portion of the ORF1 genome using broad-spectrum nested RT-PCR assays targeting the rat HEV RdRp gene. Phylogenetic analysis showed that the rat HEV strains formed four distinct subclades, labeled rat-1a to rat-1d. Human-derived rat HEV strains are isolated into subclades rat-1a (the Democratic Republic of Congo, France, and Spain) and rat-1b (Hong Kong, China). In our study, the human-derived strains were classified into subclade rat-1d (GenBank nos. PQ001569-PQ001574) (Fig. 6). By BLAST analysis, these strains showed 99.35–100% nucleotide identity with rat HEV strains (GenBank nos. OP921755 and OP921756) isolated from rats in Yunnan province collected in 201958. These results suggest zoonotic potential in subclade rat-1d, with rat HEV infections closely related to local rats. Three rat HEV subclades with zoonotic crossover to humans have been discovered worldwide.
Phylogenetic tree was reconstructed by the neighbor-joining method based on a partial RdRp gene of the rat HEV ORF1. Viral species and genotype, GenBank accession number, virus host, country (province or state) of origin, and year of collection are indicated. Sequences obtained in rat HEV-infected individuals from set 1 are highlighted with a red circle (GenBank nos. PQ001569-PQ001574). HEV strains derived from human-infected are marked in bold. Bootstrap values >70 are shown. Source data are provided as a Source Data file. HEV hepatitis E virus, ORF1 the open reading frame 1, rat HEV species HEV ratti−1, RdRp RNA-dependent RNA polymerase.
The median age of six rat HEV RNA-positive individuals was 47.0 years (IQR 27.0–59.0) and 66.67% (four of six) were female (Table 3). None had HBV and immunosuppression, and none presented with hepatitis. Three out of four women were pregnant, and two men were admitted for pulmonary infection and acute tonsillitis. Of the six individuals, one (individual 2) had a chronic medical condition (type 2 diabetes mellitus) and abnormal ALT levels (Table 3). According to retrospective analysis of laboratory test indicators, individual 2 showed abnormal ALT levels in the past 203 days (day 0, rat HEV RNA positive) (Fig. 7). This suggests that potential liver damage appears not to be caused by rat HEV infection. Individual 2 cleared rat HEV RNA and did not progress to chronic infection. None of the individuals had abnormal renal markers (Table 3 and Fig. S11). These results indicate that these rat HEV RNA-positive individuals are considered asymptomatic carriers with concomitant disease.
Liver markers in individual 2 with positive rat HEV RNA were traced. Liver markers include ALT, AST, ALP, GGT, BChE, and total bilirubin. Data points are marked as blue circles. Source data are provided as a Source Data file. ALP alkaline phosphatase, ALT alanine aminotransferase, AST aspartate aminotransferase, BChE butyrylcholinesterase, GGT gamma-glutamyl transferase, rat HEV species HEV ratti−1.
Public health burden of rat HEV
Population samples with ALT abnormality were collected from two sets: set 3 from Dali, a city on China’s southwestern border in Yunnan province, and set 4 from Dongtai, a city on China’s eastern coast in Jiangsu province. Demographic characteristics for the populations in these two sets are summarized in Table S2.
In set 3, 13.97% (70 of 501) showed rat HEV exposure, 4.99% (25 of 501) showed both rat and b HEV exposure, 41.92% (210 of 501) showed b HEV exposure and 1.60 (8 of 501) showed unrecognizable exposure (Table S3 and Fig. S12A–J). This exposure spectrum was similar to that of set 1. Testing for rat and b HEV RNA revealed that 0.4% (2 of 501) of patients had detectable b HEV RNA. In set 4, 1.91% (15 of 786) of individuals had detectable b HEV RNA, demonstrating the high prevalence of b HEV in this region (Table S4). We amplified a portion of the ORF1 genome from b HEV RNA-positive patients in set 4 and phylogenetic analysis showed that these b HEV strains belonged to subtype 4d (Fig. S13).
Discussion
Rodents, the largest group of mammals, include rat species that are natural reservoirs for virulent pathogens posing severe threats to humans59. Currently, hotspots of rat reservoir diversity are found in North America, the Atlantic coast of South America, Europe, Russia, and parts of Central and East Asia, with many hyper-reservoir rat species located in higher latitudes (above 40° N)60,61,62. These hotspots showed human-rat closely contacting. So far, investigations of disease outbreaks have primarily been reactive, highlighting the need for a more proactive approach63. The rising frequency of rat HEV incidents highlights the necessity of developing monitoring tools to adopt more preemptive diagnostic or predictive approaches for investigating public health risk to mitigate impacts on both human and animal health.
HEV was first discovered in 1983 and confirmed to be enterically transmitted64. In 1990, the viral genome was identified and named b HEV65. Retrospective studies from the 1950s and 1970s in India demonstrated outbreaks caused by b HEV66,67. Rat HEV was reported to infect humans via zoonotic transmission in 201829, but potential transmission may have occurred earlier68,69. In Yunnan Province, a biodiversity hotspot, rats coexist with humans due to highly disturbed habitats. Additionally, frequent human-rat contact driven by wildlife trade and consumption increases the spillover burden47. The zoonotic potential of rat HEV strains, which have been evolving for a long time, should be taken seriously. In this study, we found that exposure to rat HEV was 21.97% (190 of 865) in set 1 (Menghai, Yunnan Province), 13.97% (70 of 501) in set 3 (Dali, Yunnan Province), and 0.75% (9 of 1196) in set 2 (Dongtai, Jiangsu Province). Furthermore, we observed the disparity between the high seroprevalence of rat HEV and b HEV in Yunnan Province, suggesting that most individuals with HEV IgG might have been exposed to rat HEV. It raised a public health concern, indicating a need for public health surveillance by implementing an effective examination method like DARE, particularly in the areas highly endemic for rat HEV. Additionally, exposure to both rat and b HEV was 4.62% (40 of 865) in set 1, 4.99% (25 of 501) in set 3, and 0.33% (4 of 1196) in set 2 (Fig. 5 and Figs. S4, S10, S12). A recent study in Hong Kong, China, found rat HEV exposure in 1.2% (7 of 599) of solid organ transplant recipients and 0.7% (4 of 599) of immunocompetent individuals, similar to the rates observed in set 253. In set 1, exposure to rat HEV was higher than in set 2 and Hong Kong, China, reflecting diverse spatial distribution. Retrospective analysis of set 1 showed that the RRs of ALT abnormality with rat HEV exposure were 1.76 (Table 2). Analysis of local rat strains found them to be highly phylogenetically similar to six human-infecting strains in Yunnan Province. Three subclades (rat-1a, rat-1b, and rat-1d) of the four reported rat HEV strains have proven enhanced zoonotic capability. Lessons from severe acute respiratory syndrome (SARS) and coronavirus disease 2019 (COVID-19) remind us to remain vigilant about zoonotic diseases70,71. Most reported rat HEV infection cases disclosed no rat exposure or travel29,31,32,35,36,37, leaving the exact transmission route undetermined. Notably, in the study, we determined the HEVrat IgG seroprevalence was 18.7% in men and 24.1% in women in set 1. It might be explained as a certain transmission route for rat HEV, such as house cleaning, contact with domestic animals, and subsequent exposure to potentially contaminated objects, which might be more common for women in daily housework; or potential sampling bias. Prospective cohort studies should focus on daily contact objects and foods potentially contaminated by rats, as well as frequent contact with domestic animal such as swine and dogs72,73,74. Interestingly, none of the patients in sets 3 and 4 with ALT abnormality tested positive for rat HEV RNA, despite the widespread circulation of rat HEV suggested by the seroprevalence results. Our vaccinated and infected animal samples using b HEV show cross-reactive IgG against rat HEV (Fig. 1 and Figs. S1, S2). This supports the notion that prior vaccination with b HEV p239 antigen can provide partial protection against rat HEV infection in rats44. Additionally, both b HEV patient sera and vaccine immunized human sera demonstrated partial cross-inhibition of rat HEV p239 binding to human target cells75. These results suggest potential cross-protection between rat HEV and b HEV, particularly in areas with high b HEV endemicity in humans.
The DARE method offers advantages over the previously developed immunoblot method, including a higher throughput (approximately eight times greater) and shorter experimental time (about five times faster). According to our validation results, the DARE method highlights higher sensitivity and comparable specificity to the immunoblot method. Furthermore, the immunoblot method was developed considering the possibility of dual exposure, whereas the DARE method can simultaneously distinguish dual exposure and single exposure. There were several study limitations. First, we included a total of four sets of individuals in the study, covering local residents visited the hospitals whose serum samples were collected for public health surveillance, adults received routine physical examination, and patients with ALT abnormality examined in hospitals. Thus, it might lead to a sampling bias, which limited the generalizability of our findings. Second, in set 1, set 3, and set 4, individuals had diverse medical conditions and diseases. However, we did not retrospectively collect the reasons for hospital visits. Furthermore, we could not determine possible risk factors, such as demographics or medical conditions, which might have association with rat HEV infection. Third, many HEV infections have been described in immunosuppressive individuals. Due to the loss or weakness of antibody responses in immunosuppressive individuals, analyzing antibody responses in such individuals is complex and challenging. A limitation of the DARE method is its complexity in analyzing antibody responses within this population. In addition, ratti HEV exhibits genetic variability, with four genotypes (r-1 to r-4) showing 54.0–64.9% of nucleotide identity76. Although our DARE method (based on rat HEV of HEV-r-1) exhibits similar detection efficacy for HEV-r-2 antibody response, lower sensitivity was observed in detecting antibody response to HEV-r-3 and HEV-r-4 exposures due to lower sequence homology (Fig. S14). HEV-r-2 has been identified in ferret, while HEV-r-3 and HEV-r-4 are putative genotypes found in field mice and kestrels76. Current evidence primarily links rat HEV infections to r-129,30,31,32,35,36,37,38,39,40,75. There is limited supporting evidence for human infection with the other three genotypes. The hosts for these three genotypes do not have the same frequency of contact with humans or the extensive geographical distribution as rats. The zoonotic transmission potential of these three genotypes warrants further investigation. Given enzyme immunoassay used in our preliminary screening, the development of a supportive system suitable for large-scale preliminary screening is worth considering for the future.
China, with diverse landscapes, encompasses a wide variety of geographical features that provide suitable habitats for rats. Climate change, land use change, land fragmentation, and human expansion into natural habitats accelerate landscape disturbances. In contrast to the biodiversity of Yunnan Province on China’s southwestern land border, rats thrive in the expansive prairies of the northern grasslands. The rugged terrain of the western plateau also supports substantial rat populations. In the densely populated southern and eastern coastal regions, rats are frequently observed in residential areas. The remarkable adaptability of rats to various environments emphasizes the potential spillover risk from rats to humans. The evolution, mutation, and diversity of pathogens complicate the assessment of spillover in humans and animals due to cross-reactive antibody responses. The DARE method’s plug-and-display approach allows for the straightforward production of protein-linked magnetic beads. This method can be used to investigate emerging spillovers. Further research is necessary to monitor hotspots using the DARE method, identify areas where new outbreaks are most likely to occur, and implement a more proactive approach to preventing zoonotic disease outbreaks to minimize risks. Applying our DARE approach to rat HEV could serve as a paradigm for other infectious pathogens transmitted from animals to humans. In summary, a substantial spillover burden of rat HEV in humans was found in the biodiversity hotspot of Yunnan Province. The DARE approach provides a model for zoonotic disease surveillance, enabling proactive prevention of public health emergencies.
Methods
Samples and settings
The study complies with all relevant ethical regulations. The study population included four cross-sectional sets (set 1 to set 4). Serum samples from four sets were collected between May 1, 2023 and November 1, 2023.
Set 1 comprises 865 persons who visited the hospital and was from Menghai, Xishuangbanna Dai Autonomous Prefecture, Yunnan Province, a city located on the southwestern land border of China. The sample collection in set 1 was conducted at Menghai People’s Hospital. All the individuals were local residents who visited the hospital for diagnosis, medication dispensing, or treatment for various medical conditions and diseases. Set 3 comprises 501 persons with ALT abnormality from Dali, Dali Bai Autonomous Prefecture, located in the northwestern part of Yunnan Province, the same province as Menghai, where the set 1 population was collected (Dali is ~600 km away from Menghai). The sample collection in set 1 was conducted at Dali People’s Hospital. Sample collection in set 1 and set 3 was approved by the Institutional Review Board of the School of Public Health, Fudan University (IRB #2021-04-0892), which approved the data and sample collection in Menghai and Dali of Yunnan province. In this IRB approval, we were allowed to retrospectively collect the remaining serum samples for public health surveillance of HEV infection, from the laboratory departments of local hospitals in Menghai and Dali.
The set 2 comprises 1196 persons who received a physical examination was from Dongtai, Jiangsu Province, a city located on the eastern coast of China. The sample collection in set 2 was conducted at the Dongtai Center for Disease Control and Prevention. All the individuals were local adults receiving physical examination; of them, 50.4% were the elderly aged 60 years and above. Set 4 comprises 786 individuals with ALT abnormality from Dongtai, Jiangsu Province. The sample collection in set 4 was conducted at virtually all healthcare centers in Dongtai based on a previously established hepatitis surveillance system50,77,78,79. Sample collection in set 2 and set 4 was approved by the Institutional Review Board of Yancheng City Center for Disease Control and Prevention (IRB #YJK-SC-BD-202308), which approved the data and sample collection in Dongtai of Jiangsu province. In this IRB approval, we were allowed to retrospectively collect the remaining serum samples for public health surveillance of HEV infection, from the laboratory departments of local healthcare centers in Dongtai. In our study, the two IRB approvals waived the written informed consent on the following reasons: (1) serum samples were originally collected for routine examinations and clinical diagnosis, involving minimal risk to the participants; (2) serum samples were kept confidential without any personal identifier; (3) no additional interview or sample collection were conducted, and no data were independently collected in our study; (4) the waiver of written informed consent did not adversely affect the rights and welfare of the participants; and (5) the waiver of written informed consent facilitated the feasibility of the study, as we were not allowed to access the participants in the study.
In set 1 and set 3, we collected and utilized the remaining serum samples from the laboratory departments of local hospitals in Menghai and Dali for public health surveillance of HEV cross-species infection. Therefore, in set 1, we did not implement specific inclusion criteria, and simply collected all the remaining serum samples, regardless of reasons for medical visit. In set 3, we collected the serum samples with ALT examination available and ALT ≥2.5 ULT in the remaining serum samples, regardless of the reasons for a medical visit. Similarly, we did not implement any inclusion criteria in set 2 and implemented an inclusion criterion of ALT ≥2.5 ULT in set 4.
In our study, serum samples from 14 b HEV-infected individuals were collected at local healthcare centers in Dongtai of Jiangsu province. Sample collection was also approved by the Institutional Review Board of Yancheng City Center for Disease Control and Prevention (IRB #YJK-SC-BD-202308). Written informed consent was obtained from each b HEV-infected individual. Serum samples from nine rat HEV-infected individuals were collected previously at the Department of Microbiology of Queen Mary Hospital (QMH) and the Department of Health Public Health Laboratory Services Branch (DH PHLSB) in Hong Kong of China, with approval from the University of Hong Kong/Hospital Authority West Cluster has been obtained (IRB #UW 18-074)29,31,32. Written informed consent was obtained from each rat HEV-infected individual for permitting the use of the samples for our research related to rat HEV antibody. Following this approval, the samples were transferred to Xiamen University under a Material Transfer Agreement (MTA #HT/HKU/1085-22). The protocol of the study and other related materials were approved by the ethics committee of Xiamen University, Xiamen, China.
HEV 239 construction, expression, and purification
The open reading frame 2 (ORF2) gene sequences of rat HEV and b HEV variants were downloaded from GenBank. HEV 239 protein (p239) is a truncated form of the capsid protein that self-assembles into virus-like particles (VLPs) and mimics the conformation of natural HEV particles52. Genes encoding b-1 and b-4 HEV p239 (aa. 368–606), were derived from GenBank nos. D11092 (Xinjiang strain) and JF915746 (SAAS-FX17 strain). Gene encoding rat HEV p239 (aa. 357–597), corresponding to b HEV p239, was derived from GenBank no. MG813927 (LCK-3110 strain). All genes encoding recombinant HEV protein were cloned into the pTO-T7 plasmid80. Recombinant HEV proteins were overexpressed in E. coli ER2566. Proteins were harvested from inclusion bodies and treated by dissolution in 4-M urea. Renatured proteins were obtained in 20-mM phosphate-buffered saline (PBS, pH = 7.4) by gradient dialysis. Renatured p239 was characterized by SDS-PAGE using Coomassie blue staining according to standard laboratory protocols.
BALB/c vaccination
Special pathogen-free (SPF) female BALB/c mice of 6 weeks old were purchased from SLAC Laboratory (strain 003) and randomly assigned into six groups (n = 6 mice per group). SPF BALB/c mice were vaccinated subcutaneously with twice single dose of HEV p239 immunogen with multiple schemes according to immunization program of 2 weeks interval, which had been mixed with Freund’s Complete Adjuvant (Sigma‒Aldrich). The vaccine was manufactured in a 20 μg formulation mixed with Freund’s complete adjuvant, and mice immunized with PBS suspended in Freund’s complete adjuvant were used as controls. Mouse serum samples were collected weekly and tested for HEV IgG assays. The animal study protocol was approved by the Institutional Animal Care and Use Committee and Laboratory Animal Management Ethics Committee of Xiamen University (ethics approval number: XMULAC20200198). Sex was not considered in the study design because the objective was to investigate general antibody responses irrespective of sex. Animals were housed in groups of up to 5/cage at 18–24 °C ambient temperatures and 40–60% humidity. Animals were fed a 20% protein diet and maintained on a 12 h light/dark cycle (8 am to 8 pm). Food and water were available ad libitum.
Gerbil infection
SPF male Mongolian gerbils (Meriones unguiculatus) of 13 weeks old were purchased from SPF Biotechnology Co, Ltd and randomly assigned into three groups (n = 5 or 3 gerbils per group). SPF gerbils were inoculated intraperitoneally with a fecal suspension containing 2 × 107 genome copies of HEV RNA, either with a single infection or co-infection of HEV virions according to various schemes. The HEV strains used were the b-3 Kernow-C1 strain (GenBank no. HQ389544) isolated from an infected patient and the rat Vietnam-105 strain (GenBank no. JX120573) isolated from an infected rat. Gerbil serum samples were collected weekly and tested for HEV IgG assays. Animals were housed in separate cages with adequate supplies of water and food. The animal study protocol was approved by the Institutional Animal Care and Use Committee of Peking University Health Science Center (ethics approval number: DLASBE0020). Sex was not considered in the study design because the objective was to investigate general antibody responses irrespective of sex. Animals were housed in groups of up to 5/cage at 18–24 °C ambient temperatures and 40–60% humidity. Animals were fed a 20% protein diet and maintained on a 12 h light/dark cycle (8 am to 8 pm). Food and water were available ad libitum.
Production of HEV 239-linked magnetic beads
The target protein HEV p239 was dialyzed in PBS. Magnosphere™ MS300/Carboxyl magnetic beads were activated according to the manufacturer’s instructions. The beads were activated using 0.1-M 2-(N-morpholino) ethanesulfonic acid (MES, pH = 5.0) binding buffer and 10 μg/μL 1-ethyl-3-(3-dimethylaminopropyl] carbodiimide hydrochloride (EDC) coupling reagent. After removing the supernatant, the HEV p239 protein solution was incubated with the activated beads to facilitate protein coupling. The beads were then thoroughly washed three times with Tris-buffered saline with Tween (TBST, pH = 7.2) to remove unbound p239 and residual reaction reagents. The coupled beads were suspended in PBS for further use.
HEV IgG adsorption assays (DARE)
HEV IgG levels were evaluated in serum samples using rat and b-4 p239-coated microplates individually. Briefly, purified rat and b-4 p239 were coated onto the wells of 96-well microplates at 100 ng/well. After blocking, 10 μL of serum was added into the wells containing 100 μL of sample diluent and incubated at 37 °C for 30 min. After five washes with phosphate-buffered saline with Tween (PBST, pH = 7.4), wells were incubated with HRP-conjugated goat anti-human IgG secondary antibodies (Thermo Scientific, 1:5000) at 37 °C for 30 min. For mouse serum samples, HRP-conjugated goat anti-mouse IgG secondary antibodies (Thermo Scientific, 1:5000) were used. For gerbil serum samples, HRP-conjugated rabbit anti-gerbil IgG secondary antibodies (Bioss, 1:5000) were used. The microplates were washed 5 times and incubated with 100 μL of TMB substrate. The reaction was stopped by the addition of 50 μL of 2 M H2SO4 after incubation for 15 min at 37 °C. The OD450 nm was measured at a reference wavelength of OD630 nm.
For either rat or b-4, or both, HEV IgG positive samples, the extra step is to be implemented. Magnetic beads linked 1 μg rat and b-4 p239 were mixed individually with each serum sample before being added to the wells. After incubation for 30 min at 37 °C and removing magnetic beads, each HEV IgG positive serum sample was added into the corresponding microplates coated either rat or b-4, or both p239. HEV recent exposure was distinguished according to the algorithm calculating the level changes between original and adsorbed HEV IgG, evaluated individually in rat and b-4 p239.
Immunoblot assays
Immunoblot assays were performed as previously reported44,53. Separated b-4 p239 (22 µg) and rat p239 (22 µg) were transferred to a nitrocellulose membrane (Bio-Rad), using the Trans-Blot Turbo Transfer System (Bio-Rad). Blocking was done at 4 °C overnight using 10% skim milk in PBST. The membranes were exposed to an antibody that cross-reacts with both b HEV and rat HEV (1:10,000)81, diluted human sera (1:400), or animal sera (1:5000) in blocking buffer at room temperature for 45 min for the immunoblot experiments. The blots were then washed in PBST. After exposure for 1 h to HRP-conjugated secondary antibodies and subsequent washes were performed as described for the primary antibodies. Membranes were visualized using the Fusion FX Spectra image analyzer (Vilber).
HEV real-time RT-PCR assays
Real-time RT-PCR assays detecting rat and b HEV RNA were performed separately. HEV RNA was extracted from the serum samples with each volume of 50 μL using QIAamp Viral RNA Mini Kit (Qiagen). In-house nucleic acid amplification assays were performed to detect rat HEV RNA using the following primer and probe sequences: forward primer 5′-CTTGTTGAGCTYTTCTCCCCT-3′, reverse primer 5′-CTGTACCGGATGCGACCAA-3′, and probe 5′-HEX-TGCAGCTTGTCTTTGARCCC-IABkFQ-3′29. Real-time RT-PCR testing b HEV RNA was performed using OneStep RT-PCR Kit (Qiagen) with the following primer and probe sequences: forward primer 5′-GGTGGTTTCTGGGGTGAC-3′, reverse primer 5′-AGGGGTTGGTTGGATGAA-3′, and probe 5′-FAM-TGATTCTCAGCCCTTCGC-TAMRA-3′82. Quantitation was obtained separately using 2 plasmid standards ranging from 101 to 106 copies/reaction to generate standard curves for rat and b HEV. All real-time RT-PCR assays were performed using the C1000 TouchTM Thermal Cycler from the CFX96TM Real-Time System (Bio-Rad).
HEV strain gene sequencing
Nested RT-PCR assays were further performed in serum samples testing for detectable rat and b HEV RNA. Partial the ORF1 genome was amplified using broad-spectrum nested RT-PCR assays targeting the rat HEV RNA-dependent RNA polymerase (RdRp) gene, with nt 4064 - 4395 based on GenBank no. MG813927 (LCK-3110 strain)11. In the first round of PCR, the forward primer was 5′-TCGCGCATCACMTTYTTCCARAA-3′ and the reverse primer was 5′-GCCATGTTCAGACDGTRTTCCA-3′. The second round used forward primer 5′-TGTGCTCTGTTTGGCCCNTGGTTYMG-3′ and reverse primer 5′-CCAGGCTCACCRGARTGYTTCTTCCA-3′. Multiple Primers targeted to the partial ORF1 genome were used to amplify b HEV RdRp gene, with nt 3961 - 4497 and 4339 - 4868 based on GenBank no. AJ272108 (T1 strain)83. In the first round of PCR, forward primer was 5′-CAGGGRATATCYGCRTGGAG-3′ and reverse primer was 5′-GCAAACCTRACRACATCAGG-3′. The second round used forward primer 5′-TGGTTCCGYGCYATTGARAA-3′ and two reverse primers: R1, 5′-GCYACAACMACACCAGCATA-3′; and R2, 5′-GCWACAACSACACCAGCATA-3′. All nested RT-PCR assays were performed using the T100TM Thermal Cycler (Bio-Rad). The products were subjected to 1.5% agarose gels stained with SYBR Green reagent (Solarbio). The products with the correct target size were purified using the QIAquick Gel Extraction Kit (Qiagen). Sense and antisense strands were sequenced using the Sanger method with the corresponding nested RT-PCR primers using the 3130xl Genetic Analyzer from Applied Biosystems (HITACHI).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The partial ORF1 genome sequences of human-derived rat hepatitis E virus (HEV) strains have been deposited in GenBank (accession numbers: PQ001569, PQ001570, PQ001571, PQ001572, PQ001573, and PQ001574). All other data that support the findings of this study are present in the paper and/or the Supplementary Information. Source data are provided with this paper.
References
Armien, B. et al. High seroprevalence of hantavirus infection on the Azuero peninsula of Panama. Am. J. Trop. Med. Hyg. 70, 682–687 (2004).
Brisse, M. E. & Ly, H. Hemorrhagic fever-causing arenaviruses: lethal pathogens and potent immune suppressors. Front. Immunol. 10, 372 (2019).
Demeure, C. et al. Yersinia pestis and plague: an updated view on evolution, virulence determinants, immune subversion, vaccination and diagnostics. Microbes Infect. 21, 202–212 (2019).
Wu, Z. et al. Comparative analysis of rodent and small mammal viromes to better understand the wildlife origin of emerging infectious diseases. Microbiome 6, 178 (2018).
Wu, Z. et al. Decoding the RNA viromes in rodent lungs provides new insight into the origin and evolutionary patterns of rodent-borne pathogens in Mainland Southeast Asia. Microbiome 9, 18 (2021).
Shanta, I. S. et al. Human exposure to bats, rodents and monkeys in Bangladesh. Ecohealth 20, 53–64 (2023).
Suwannarong, K. et al. Hunting, food preparation, and consumption of rodents in Lao PDR. PLoS ONE 10, e0133150 (2015).
Wang, B. et al. Detection and characterization of three zoonotic viruses in wild rodents and shrews from Shenzhen city, China. Virol. Sin. 32, 290–297 (2017).
He, W. et al. The prevalence and genomic characteristics of hepatitis E virus in murine rodents and house shrews from several regions in China. BMC Vet. Res. 14, 414 (2018).
Johne, R. et al. Rat hepatitis E virus: geographical clustering within Germany and serological detection in wild Norway rats (Rattus norvegicus). Infect. Genet. Evol. 12, 947–956 (2012).
Johne, R. et al. Detection of a novel hepatitis E-like virus in faeces of wild rats using a nested broad-spectrum RT-PCR. J. Gen. Virol. 91, 750–758 (2010).
Fitzpatrick, J. L. et al. Rabies in rodents and lagomorphs in the United States, 1995-2010. J. Am. Vet. Med. Assoc. 245, 333–337 (2014).
Fulhorst, C. F. et al. Hantavirus and arenavirus antibodies in persons with occupational rodent exposure. Emerg. Infect. Dis. 13, 532–538 (2007).
Purcell, R. H. et al. Hepatitis E virus in rats, Los Angeles, California, USA. Emerg. Infect. Dis. 17, 2216–2222 (2011).
Douno, M. et al. Hunting and consumption of rodents by children in the Lassa fever endemic area of Faranah, Guinea. PLoS Negl. Trop. Dis. 15, e0009212 (2021).
Schmaljohn, C. & Hjelle, B. Hantaviruses: a global disease problem. Emerg. Infect. Dis. 3, 95–104 (1997).
Vial, P. A. et al. Hantavirus in humans: a review of clinical aspects and management. Lancet Infect. Dis. 23, e371–e382 (2023).
Armstrong, L. R. et al. Hantavirus pulmonary syndrome associated with entering or cleaning rarely used, rodent-infested structures. J. Infect. Dis. 172, 1166 (1995).
Glass, G. E. et al. Association of intraspecific wounding with hantaviral infection in wild rats (Rattus norvegicus). Epidemiol. Infect. 101, 459–472 (1988).
Douron, E. et al. HFRS after a wild rodent bite in the Haute-Savoie–and risk of exposure to Hantaan-like virus in a Paris laboratory. Lancet 1, 676–677 (1984).
Kane, Y. et al. Viral diversity in wild and urban rodents of Yunnan Province, China. Emerg. Microbes Infect. 13, 2290842 (2024).
Ding, Q. et al. Prevalence and molecular characterization of hepatitis E virus (HEV) from wild rodents in Hubei Province, China. Infect. Genet. Evol. 121, 105602 (2024).
Takahashi, M. et al. First detection and characterization of rat hepatitis E Virus (HEV-C1) in Japan. Virus Res. 314, 198766 (2022).
Ryll, R. et al. Detection of rat hepatitis E virus in wild Norway rats (Rattus norvegicus) and Black rats (Rattus rattus) from 11 European countries. Vet. Microbiol. 208, 58–68 (2017).
Johne, R. et al. Novel hepatitis E virus genotype in Norway rats, Germany. Emerg. Infect. Dis. 16, 1452–1455 (2010).
Murphy, E. G. et al. First detection of Hepatitis E virus (Orthohepevirus C) in wild brown rats (Rattus norvegicus) from Great Britain. Zoonoses Public Health 66, 686–694 (2019).
Wu, H. et al. Molecular epidemiology and phylogeny of the emerging zoonotic virus Rocahepevirus: a global genetic analysis. Infect. Genet. Evol. 118, 105557 (2024).
Jo, W. K. et al. Ancient evolutionary origins of hepatitis E virus in rodents. Proc. Natl Acad. Sci. USA 121, e2413665121 (2024).
Sridhar, S. et al. Rat hepatitis E virus as cause of persistent hepatitis after liver transplant. Emerg. Infect. Dis. 24, 2241–2250 (2018).
Hon, K. L. & Sridhar, S. Rat hepatitis E in an immunocompromised patient. Indian Pediatr. 57, 1085–1086 (2020).
Sridhar, S. et al. Transmission of rat hepatitis E virus infection to humans in Hong Kong: a clinical and epidemiological analysis. Hepatology 73, 10–22 (2021).
Sridhar, S. et al. Hepatitis E virus species C infection in humans, Hong Kong. Clin. Infect. Dis. 75, 288–296 (2021).
Cheung, C. Y., Chan, K. M. & Sridhar, S. Rat hepatitis E in kidney transplant recipients: case studies and review of literature. Transpl. Infect. Dis. 26, e14266 (2024).
Cui, X. et al. Prevalence of Rocahepevirus ratti (rat hepatitis E virus) in humans and rats in China. JHEP Rep. 341, 101370 (2025).
Andonov, A. et al. Rat hepatitis E virus linked to severe acute hepatitis in an immunocompetent patient. J. Infect. Dis. 220, 951–955 (2019).
Rodriguez, C. et al. Orthohepevirus C hepatitis, an underdiagnosed disease? J. Hepatol. 79, e39–e41 (2023).
Rivero-Juarez, A. et al. Orthohepevirus C infection as an emerging cause of acute hepatitis in Spain: first report in Europe. J. Hepatol. 77, 326–331 (2022).
Caballero-Gomez J. et al. Acute hepatitis in children due to rat hepatitis E virus. J. Pediatr. 73, 114125 (2024).
Casares-Jimenez, M. et al. Rat hepatitis E virus (Rocahepevirus ratti) in people living with HIV. Emerg. Microbes Infect. 13, 2295389 (2024).
Casares-Jimenez, M. et al. Serological and molecular survey of rat hepatitis E virus (Rocahepevirus ratti) in drug users. Emerg. Microbes Infect. 13, 2396865 (2024).
Caballero-Gomez J., et al. Rat hepatitis E virus as an aetiological agent of acute hepatitis of unknown origin. J. Hepatol. (2025).
Debing, Y. et al. Update on hepatitis E virology: implications for clinical practice. J. Hepatol. 65, 200–212 (2016).
Qian, Z. et al. Rat hepatitis E virus is a potential zoonotic pathogen to humans. J. Hepatol. 77, 868–870 (2022).
Sridhar, S. et al. Multimodal investigation of rat hepatitis E virus antigenicity: implications for infection, diagnostics, and vaccine efficacy. J. Hepatol. 74, 1315–1324 (2021).
Kyuregyan, K. K. et al. [The duration of preservation of anamnestic antibodies to hepatitis E virus.]. Klin. Lab Diagn. 63, 310–314 (2018).
Rapicetta, M. et al. Seroprevalence and anti-HEV persistence in the general population of the Republic of San Marino. J. Med. Virol. 58, 49–53 (1999).
Morcatty, T. Q. et al. Risk of viral infectious diseases from live bats, primates, rodents and carnivores for sale in Indonesian wildlife markets. Viruses 14, 2756 (2022).
Huang, F. et al. Excretion of infectious hepatitis E virus into milk in cows imposes high risks of zoonosis. Hepatology 64, 350–359 (2016).
Long, F. et al. High prevalence of hepatitis E virus infection in goats. J. Med. Virol. 89, 1981–1987 (2017).
Zhu, F. C. et al. Efficacy and safety of a recombinant hepatitis E vaccine in healthy adults: a large-scale, randomised, double-blind placebo-controlled, phase 3 trial. Lancet 376, 895–902 (2010).
Huang, X. et al. Active surveillance of hepatitis E: a 10-year epidemiological analysis in a city in eastern China. Emerg. Microbes Infect. 13, 2373315 (2024).
Zhang, J. et al. Hepatitis E virus: neutralizing sites, diagnosis, and protective immunity. Rev. Med. Virol. 22, 339–349 (2012).
Situ, J. et al. An immunoassay system to investigate epidemiology of Rocahepevirus ratti (rat hepatitis E virus) infection in humans. JHEP Rep. 5, 100793 (2023).
Nimgaonkar, I. et al. Hepatitis E virus: advances and challenges. Nat. Rev. Gastroenterol. Hepatol. 15, 96–110 (2018).
Liu, T. et al. An immunocompetent Mongolian gerbil model for hepatitis E virus genotype 1 infection. Gastroenterology 167, 750–763 e710 (2024).
Subramaniam, S. et al. Distinct disease features of acute and persistent genotype 3 hepatitis E virus infection in immunocompetent and immunosuppressed Mongolian gerbils. PLoS Pathog. 19, e1011664 (2023).
Liu, T. et al. Establishment of enterically transmitted hepatitis virus animal models using lipid nanoparticle-based full-length viral genome RNA delivery system. Gut 74, 467–476 (2025).
Wu, H. et al. Genomic characterization of Rocahepevirus ratti hepatitis E virus genotype C1 in Yunnan province of China. Virus Res 341, 199321 (2024).
Han, B. A. et al. Rodent reservoirs of future zoonotic diseases. Proc. Natl Acad. Sci. USA 112, 7039–7044 (2015).
Jenkins, C. N., Pimm, S. L. & Joppa, L. N. Global patterns of terrestrial vertebrate diversity and conservation. Proc. Natl Acad. Sci. USA 110, E2602–E2610 (2013).
Wolfe, N. D., Dunavan, C. P. & Diamond, J. Origins of major human infectious diseases. Nature 447, 279–283 (2007).
McFarlane, R., Sleigh, A. & McMichael, T. Synanthropy of wild mammals as a determinant of emerging infectious diseases in the Asian-Australasian region. Ecohealth 9, 24–35 (2012).
Morse, S. S. et al. Prediction and prevention of the next pandemic zoonosis. Lancet 380, 1956–1965 (2012).
Balayan, M. S. et al. Evidence for a virus in non-A, non-B hepatitis transmitted via the fecal-oral route. Intervirology 20, 23–31 (1983).
Reyes, G. R. et al. Isolation of a cDNA from the virus responsible for enterically transmitted non-A, non-B hepatitis. Science 247, 1335–1339 (1990).
Naidu, S. S. & Viswanathan, R. Infectious hepatitis in pregnancy during Delhi epidemic. Indian J. Med. Res. 45, 71–76 (1957).
Khuroo, M. S. Study of an epidemic of non-A, non-B hepatitis. Possibility of another human hepatitis virus distinct from post-transfusion non-A, non-B type. Am. J. Med. 68, 818–824 (1980).
Shimizu, K. et al. Serological evidence of infection with rodent-borne hepatitis E virus HEV-C1 or antigenically related virus in humans. J. Vet. Med. Sci. 78, 1677–1681 (2016).
Dremsek, P. et al. Seroprevalence study in forestry workers from eastern Germany using novel genotype 3- and rat hepatitis E virus-specific immunoglobulin G ELISAs. Med. Microbiol. Immunol. 201, 189–200 (2012).
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395, 507–513 (2020).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506 (2020).
Rios-Munoz, L. et al. Detection of rat hepatitis E virus in pigs, Spain, 2023. Emerg. Infect. Dis. 30, 823–826 (2024).
Shun, E. H. et al. Rat hepatitis E virus (Rocahepevirus ratti) exposure in cats and dogs, Hong Kong. Emerg. Microbes Infect. 13, 2337671 (2024).
Li, B. et al. Using codon usage analysis to speculate potential animal hosts of hepatitis E virus: an exploratory study. Infect. Genet. Evol. 101, 105284 (2022).
Guo, H. et al. Cell binding tropism of rat hepatitis E virus is a pivotal determinant of its zoonotic transmission to humans. Proc. Natl Acad. Sci. USA 121, e2416255121 (2024).
Bai, H. et al. Characterization of a novel rat hepatitis E virus isolated from an Asian musk shrew (Suncus murinus). Viruses 12, 715 (2020).
Zhang, J. et al. Long-term efficacy of a hepatitis E vaccine. N. Engl. J. Med. 372, 914–922 (2015).
Huang, S. et al. Long-term efficacy of a recombinant hepatitis E vaccine in adults: 10-year results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 403, 813–823 (2024).
Zhuang, C. et al. Effectiveness of a hepatitis E vaccine against medically-attended symptomatic infection in HBsAg-positive adults from a test-negative design study. Nat. Commun. 16, 1699 (2025).
Im, S. W. et al. A bacterially expressed peptide prevents experimental infection of primates by the hepatitis E virus. Vaccine 19, 3726–3732 (2001).
Chen, Z. et al. Redeveloping antigen detection kits for the diagnosis of rat hepatitis E virus. J. Clin. Microbiol. 61, e0071023 (2023).
Jothikumar, N. et al. A broadly reactive one-step real-time RT-PCR assay for rapid and sensitive detection of hepatitis E virus. J. Virol. Methods 131, 65–71 (2006).
Mizuo, H. et al. Polyphyletic strains of hepatitis E virus are responsible for sporadic cases of acute hepatitis in Japan. J. Clin. Microbiol. 40, 3209–3218 (2002).
Acknowledgements
This research was funded by the National Natural Science Foundation of China, grant numbers 82071783 (Z.Z.), 32370160 (Z.Z.), 81973101 (Y.L.), and 82402603 (D.Y.), the Natural Science Foundation of Fujian Province, grant number 2022J02005 (Z.Z.), the Shanghai Municipal Science and Technology Major Project, grant number ZD2021CY001 (Y.L.), the National Key Research and Development Program of China (NKPs), grant numbers 2023YFC2306900 (L.W.) and 2024YFC2310602 (Z.Z.), the Beijing Natural Science Foundation, grant number L244032 (Z.Z.), the China Postdoctoral Science Foundation, grant numbers 2023M732935 (Y.H.), 2024M751776 (D.Y.), and GZC20231425 (D.Y.), the Major Science and Technology Project for Significant New Drugs Creation, grant number 2018ZX09303005-002 (N.X.), the CAMS Innovation Fund for Medical Sciences, grant number 2019RU022 (N.X.), and was supported by the Fundamental Research Funds for the Central Universities, grant number 20720220006 (N.X.).
Author information
Authors and Affiliations
Contributions
Conceptualization, Z.C., N.X., L.W., Y.L. and Z.Z.; methodology, Z.C., G.L., and Z.Z.; experiment, Z.C., L.W., Y.Z., G.L., J.Y., J.F., T.L., H.W., Y.H., W.H., D.L., X.Z., X.Z., X.H., L.S., S.W., and J.L.; resources, L.W., Y.Z., J.Y., L.S., M.F., Y.W., T.W., S.S., J.Z., N.X., L.W., Y.L., and Z.Z.; writing—original draft preparation, Z.C.; writing—review and editing, Z.C., S.S., L.W., Y.L and Z.Z.; funding acquisition, Y.H., D.Y., N.X., L.W., Y.L. and Z.Z. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Antonio Rivero-Juárez and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, Z., Wang, L., Zhang, Y. et al. Substantial spillover burden of rat hepatitis E virus in humans. Nat Commun 16, 4038 (2025). https://doi.org/10.1038/s41467-025-59345-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-59345-6