Abstract
Healthy blood vessels supply neurons to preserve metabolic function. In blinding proliferative retinopathies (PRs), pathological neovascular tufts often emerge in lieu of needed physiological revascularization. Here we show that metabolic shifts in the neovascular niche define angiogenic fate. Fatty acid oxidation (FAO) metabolites accumulated in human and murine retinopathy samples. Neovascular tufts with a distinct single-cell transcriptional signature highly expressed FAO enzymes. The deletion of Sirt3, an FAO regulator, shifted the neovascular niche metabolism from FAO to glycolysis and suppressed tuft formation. This metabolic transition increased Vegf expression in astrocytes and reprogrammed pathological neovessels to a physiological phenotype, hastening vascular regeneration of the ischemic retina and improving vision. Hence, strategies to change the metabolic environment of vessels could promote a regenerative phenotype in vascular diseases.
Similar content being viewed by others
Introduction
Proliferative retinopathy (PR) is a leading cause of blindness in children with retinopathy of prematurity and working-age adults with diabetic retinopathy1. The initial blood vessel loss in PR and the neuroretinal ischemia that follows trigger the excessive and misplaced production of vascular endothelial growth factor (VEGF), driving pathological angiogenesis in an attempt to reinstate metabolic homeostasis1,2. While inhibiting VEGF to block pathological neovascular tuft formation has been the focus of therapeutic interventions to date3, the regenerative forces driving physiological revascularization of the ischemic neuroretina have been less explored. Discerning unique molecular fingerprints differentiating pathological and physiological neovessels, along with their associated vascular niche, could help reveal the drivers of healthy revascularization and neuronal survival.
Neuroglial cells of the vascular unit secrete growth factors and guidance cues that shape vascular architecture to meet their metabolic requirements4,5. During vascular development, astrocytes6,7 and retinal ganglion cells8 (RGCs) secrete VEGF that guides the advancing migratory tip endothelial cells (EC) of the vascular front. During PR, when the retina has fewer blood vessels and is hypoxic and nutrient-starved, excessive VEGF and repulsive guidance cues are secreted by ischemic neuroglial cells8,9,10,11. However, dosed amounts of VEGF are critical for the survival of astrocytes and the physiological revascularization of the ischemic retina12. While many secreted factors regulating pathological angiogenesis have been identified, it is unclear whether metabolic shifts could influence angiogenic fate, be it healthy or diseased.
During developmental angiogenesis, endothelial metabolism relies primarily on glycolysis to produce energy13. Glycolysis contributes to EC proliferation and migration required for vessel growth. Glycolytic enzymes are localized in lamellipodia and leading membrane ruffles of EC, powering the migration of endothelial tip cells14 that guide physiological vascular growth. Since glucose diffuses further from vessels than oxygen14,15,16, EC can rely on anaerobic glycolysis when sprouting in avascular tissues. Pharmacological inhibition of glycolysis prevents sprouting angiogenesis14,17. Hence, glycolysis may be a metabolic trait of EC that would be advantageous to revascularizing the ischemic retina.
Fatty acid oxidation (FAO) also promotes EC proliferation13. In addition to energy production, fatty acids are an essential carbon source to produce de novo nucleotides for DNA replication in EC18. This biosynthetic function contributes to EC proliferation, but unlike glycolysis, it is not associated with increased EC migration, a characteristic of tip cells driving vascular regeneration14. Inhibition of carnitine palmitoyl-transferase 1 (CPT1), shuttling long-chain fatty acids inside mitochondria for oxidation, decreases pathological tufts in murine PR18, but its impact on physiological revascularisation is unknown.
Sirtuins (SIRT) are NAD + -dependent deacetylases pivotal for mitochondrial function19. SIRT3 is a master regulator of FAO and oxidative energy metabolism within mitochondria20,21,22. Since both FAO and glycolysis fuel many critical biological functions, including angiogenesis, we reasoned that SIRT3 could be a metabolic switch able to modulate the relative balance of energy utilization within the vascular niche without the deleterious effects of completely abrogating one of these essential energy sources. We combined unbiased large-scale metabolomics and single-cell transcriptomics data to define distinct metabolic and transcriptional signatures for physiological and pathological EC. While glycolysis is essential to the migratory and regenerative tip EC, we show that FAO is a hallmark of misguided yet actively proliferating pathological neovascular EC. Metabolic reprogramming of the retinal microenvironment caused by Sirt3 deletion, primarily expressed in astrocytes, shifts neovascular metabolism from FAO to glycolysis and enhances physiological vascular regeneration of the retina, improving neuroretinal function.
Results
Fatty-acid oxidation is a metabolic hallmark of pathological angiogenesis
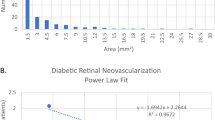
We first examined the metabolite profile of vitreous humor from subjects with proliferative diabetic retinopathy (Supplementary Table 1, Supplementary Fig. 1a–c). Vitreous samples were collected adjacent to leaky pathological neovascular tufts that characterize PR (Fig. 1a). Amongst the top 25 most significantly dysregulated metabolites, we observed an accumulation of acylcarnitines in human neovascular PR samples compared to control subjects with epiretinal membranes (Fig. 1a, red font). Fatty acylcarnitines are by-products of fatty-acid β-oxidation (FAO), the process of oxidizing fatty acids in mitochondria to produce acetyl-CoA (Fig. 1b). Using Metaboanalyst23, a metabolomics analysis tool, 5 of the 6 most enriched metabolic pathways in human PR pertained to FA metabolism, including long and short-chain saturated FAO pathways (Fig. 1b). Hence, the accumulation of FAO metabolites is a prominent characteristic of human proliferative retinopathy.
a Heatmap of the top 25 most significantly dysregulated metabolites (two-tailed Student’s t-test) from vitreous biopsies of subjects with epiretinal membranes (Control, n = 4) and proliferative diabetic retinopathy (n = 7) by LC/MS/MS. b Metabolite set enrichment analysis of dysregulated metabolites for metabolic pathways and intracellular localisations in proliferative diabetic retinopathy. See also Supplementary Fig. 1 and Supplementary Table 1.
Vitreous metabolites are often used as surrogate markers of adjacent retinal metabolism24,25. However, decerning the precise cellular origin of these metabolites in human retinas could impair residual vision. Fibrovascular membranes (FVM) resected from diabetic retinopathy patients have been analyzed through single-cell RNAseq26, revealing some tip-like endothelial cells (FVM EC 2, ESM1), yet these lesions typically lack active neovascular tufts (Supplementary Fig. 1d–f). We, therefore, used the oxygen-induced retinopathy (OIR) mouse model to study the formation of pathological neovascular tufts characteristic of PR (Fig. 2a)27. In this model, mice pups are exposed to high oxygen concentration for 5 days (post-natal day (P) 7 to 12), causing vaso-obliteration (VO) and subsequent retinal ischemia. After returning to room air (P12), the ischemic neuroretina triggers both its physiological revascularization and the formation of pathological neovascular tufts that invade the vitreous27. At the start of neovascularization in OIR (P14), we observed comparable enrichments of FAO metabolites to human PR (Fig. 2b and Supplementary Fig. 2a–c). Interestingly, acyl-carnitine fatty acid levels across all chain lengths (C2–C18) were elevated in both PR models despite their distinct etiologies, indicating a global disruption in FAO rather than a specific enzymatic blockage. Thus, the metabolomic profile in mice with PR closely resembled the human condition, establishing a relevant model to investigate the influence of FAO on neovascular disease.
a Schematic representation of the oxygen-induced retinopathy (OIR) mouse model of proliferative retinopathy. b Heatmap of fatty acylcarnitine metabolites measured in human vitreous and mouse retinas of control (human n = 4, mouse n = 4) and proliferative retinopathy samples (human n = 7, mouse n = 4). c UMAP of single-cell RNAseq from normoxic (n = 6, 21305 cells) and OIR (n = 8, 17814 cells) retinas taken during the neovascularisation period (P14-P17) representing the 11 retinal cell types identified by graph-based clustering of normalized RNA count (GEO accession number GSE150703). d Ridge plot of GSVA score for REACTOME mitochondrial beta-oxidation of saturated fatty acids pathway for OIR cell types at P14 and P17. e Dot plot illustrating the expression levels of genes from the REACTOME pathway related to mitochondrial beta-oxidation of saturated fatty acids across OIR cell types at P14 and P17. f Graphical representation of the vascular unit during the neovascular phase of OIR.
To determine the retinal source of FAO intermediates in PR, we compared the transcriptome of individual retinal cells using single-cell RNA sequencing data from mice exposed to OIR and their normoxic littermate controls at the instigation of retinal revascularization (at P14) and the peak of pathological angiogenesis (at P17)28. Retinal cells were annotated, as previously described28 (Fig. 2c). Gene set variation analysis (GSVA) for FAO pathways showed that cell types forming the vascular unit (EC, pericytes, astrocytes, and Müller glia) were the most enriched in transcripts coding for saturated FAO enzymes at both time points in the OIR hypoxic retina (Fig. 2d). EC (P14) and astrocytes (P17) showed strong transcriptional expression of mitochondrial FAO genes (Acadl, Acadvl, Hadh, Hadha, and Hadhb) compared to other cell types (Fig. 2e and Supplementary Fig. 2d). These results indicated that cell types comprising the neovascular unit (Fig. 2f), particularly EC and astrocytes, may contribute to the accumulation of FAO intermediates in ischemic PR.
Single-cell RNAseq identifies a unique transcriptional signature for neovascular tufts
Uncovering the specific molecular fingerprints of pathological neovessels has been a critical objective in vascular biology. To examine EC heterogeneity in PR, we enriched retinal single-cell suspensions for EC (using magnetic beads coated with PECAM1/CD31, Supplementary Fig. 3a-b) and performed a single-cell transcriptomic analysis of OIR and normoxic retinas. The unbiased assessment of uniform manifold approximation and projection (UMAP) results uncovered six retinal EC subclusters (Fig. 3a) comprising five known EC subtypes according to vascular zonation (arterial, vein, capillary, proliferative, tip cells29) and one previously unidentified EC subtype (Aqp1 + EC, Fig. 3b). Normoxic control retinas were composed primarily of capillary, vein, and arterial EC, with relatively few tip cells (1-3%) and proliferating EC (0–5%). In contrast, OIR retinas at P14, following the initial vaso-obliterative phase, contained more proliferative (24%) and endothelial tip cells (25%) to revascularize the ischemic retina and less mature arteries (2%) and veins (32%) (Fig. 3c). Later, at P17, once further retinal revascularization was achieved, arterial (11%) and vein EC (57%) were more abundant, and fewer tip (10%) and proliferative EC (5%) were recovered.
a UMAP of endothelial-enriched retinal single-cell RNAseq from normoxic (n = 4, 2094 cells) and OIR (n = 5, 1875 cells) retinas during the neovascular phase (P14-P17). b Dot plot of the top 10 marker genes for each of 6 endothelial subtypes identified on UMAP. c Representation of the percentage of cells within each endothelial subtype, calculated from the total number of endothelial cells for each condition and at each time point. d Hierarchical dendrogram of endothelial subtypes using k-mean Euclidean distances constructed on high variable genes (HVGs). e Immunofluorescence of retinal flat-mounts for AQP1 (green) counterstained with Lectin (red) from normoxia and OIR P17 mice (n = 3 retina each). Scale: 150 μm. f Immunofluorescence of P17 OIR retinal flat-mounts (n = 5 retina) for ESM1 (green) and Lectin (red). Scale: 10 μm. Graphical representation of physiological (tip cells) and pathological (Tuft) angiogenesis during neovascularisation in OIR. g Volcano plot of differentially expressed genes between tuft and tip endothelial cells from P17 OIR retinas (P-value < 0.05, absolute log2 Fold Change (FC) > 0.5, non-parametric two-sided Wilcoxon rank-sum test, percent of expression > 10%, see Source data). h KEGG pathway analysis of up-regulated genes in tip or tuft ECs from panel g (combined Fisher exact test P-value and Benjamini-Hochberg corrected z-score from EnrichR). i Ridge plot of normalized GSVA score for glycolysis (Hallmark) and mitochondrial beta-oxidation of saturated fatty acids (Reactome) pathways in OIR endothelial subtypes at P17. j Dot plot of the most expressed glycolytic and FAO genes from the metabolic pathways in previous panel. k In situ hybridization by RNAscope of P17 OIR retinal cryosection (n = 3 retina) for Aqp1 (red) and Hadha (blue) counterstained with Lectin (green). Scales: 25 μm (top and left middle panels), 10 μm (bottom and right middle panels). l Heat map of GSVA scores for metabolic pathways between EC subtypes (top) and among cell types of the vascular niche in OIR versus normoxic condition (bottom). m Graphical model of the metabolic reliance on FAO and glycolysis of cells of the neovascular niche.
Exclusively in OIR retinas, we detected a small EC cluster (1 to 2 % of total EC) defined by the specific expression of Aquaporin 1 (Aqp1), a water channel that controls cellular osmotic homeostasis. These unique Aqp1+ cells co-expressed bona fide EC genes (Cdh5, Cldn5, Pecam1) as well as vein (Rpl18a, Tmsb10, Rps28) and tip cell (Esm1, Mcam, Prss23) markers. Still, they were unique in their expression of genes involved in cell permeability (Aqp1) and matrix remodeling (Col18a1, Col15a1), amongst other pathways (Fig. 3b and Supplementary Fig. 3c, d). We also confirmed the presence of Aqp1+ endothelial subclusters in publicly available scRNAseq datasets from mouse OIR retinas (P14) (Supplementary Fig. 3e,f)30. Hierarchical clustering based on highly variable genes showed that the Aqp1 + EC were the most divergent compared to other endothelial subtypes and closest to the tip cell subcluster (Fig. 3d). Based on these transcriptional characteristics and the absence of Aqp1 + EC in normoxic retinas (devoid of tufts), we postulated that Aqp1 + EC might correspond anatomically to pathological neovascular tuft EC. Indeed, we localized AQP1-expressing EC to pathological tufts in OIR retinas using immunofluorescence but not in healthy normoxic vessels (Fig. 3e) nor other retinal cell types, contrarily to previous reports31 (Supplementary Fig. 3g, h). We also confirmed the expression of tip cell marker ESM1 in both tip and tuft EC (Fig. 3f), in line with previous evidence that tuft EC might be misguided tip cells9. Hence, we identified a unique transcriptional signature for pathological neovascular tuft EC in the murine OIR model, characterized by AQP1 expression.
FAO and glycolysis dichotomize neovascular tufts and physiological tip cells
We then compared the newly obtained transcriptional signature of pathological tuft EC to the physiological tip EC required for regenerative angiogenesis. We identified 449 differentially expressed genes (DEGs) between tuft and tip EC (P value < 0.05, log2(FC) > 0.5, Fig. 3g). Up-regulated genes in tip EC were enriched for extracellular matrix-receptor interaction, focal adhesion, and glycolysis pathways. In contrast, tuft EC genes were significantly enriched for ferroptosis, fatty-acid degradation, tyrosine, and nicotinamide metabolism pathways (Fig. 3h). To better visualize the metabolic dichotomy between tuft and tip EC, we performed a gene set variation analysis (GSVA) to rank EC subtypes based on their relative expression of genes implicated in glycolysis and FAO pathways (Fig. 3i). In OIR, tip EC were highly glycolytic and relied less on FAO (P17). Inversely, tuft EC relied preferentially on FAO and least on glycolysis (P17).
Focusing on the most abundant FAO and glycolysis transcripts, tip cells showed greater expression of essential glycolic genes (Pkm, Aldoa, Tpi1, Gpi1), particularly at P17, while tuft EC expressed higher levels of FAO genes (Hadha, Acadvl) (Fig. 3j). Notably, tuft EC strongly expressed Hadha (Hydroxyacyl-CoA Dehydrogenase Trifunctional Multienzyme Complex Subunit Alpha), which encodes a subunit of the mitochondrial trifunctional protein essential for FAO. Importantly, Hadha expression colocalized with pathological Aqp1+ tufts by RNAscope in situ hybridization on retinal cryosections (Fig. 3k). Thus, we discerned distinct transcriptional metabolic identities for healthy and diseased EC in murine PR, favoring glycolysis in the case of tip EC and FAO in the case of pathological tuft EC (Fig. 3l, top). This metabolic dichotomy was also evident in the vascular niche, with astrocytes over-expressing FAO pathways, while Müller cells were more glycolytic in OIR (Fig. 3l, bottom). Importantly, our findings provide an endothelial atlas from the ischemic phase of proliferative retinopathy (P14/P17), enabling deeper insights into the divergent transcriptomic programs separating pathological and physiological angiogenesis (Fig. 3m).
Targeting FAO curbs pathological neovascular tufts
We then explored the role of FAO in neovascular tuft formation. We utilized etomoxir to inhibit FAO, blocking CPT1a, which is essential for transporting lipids into mitochondria18 (Fig. 4a). Etomoxir reduced pathological neovascularization (NV) and vaso-obliteration (VO) in WT retinas exposed to OIR (Fig. 4b), in line with a contribution of FAO to neovascular tuft formation. However, etomoxir caused substantial toxicity and fatalities during the hypoxic phase of OIR (P12 to P17), highlighting the vital role of FAO metabolism systemically. We, therefore, sought to identify a more targeted metabolic regulator capable of yielding therapeutic gains without harmful systemic side effects.
a Graphical representation of Sirtuin-3 regulation of mitochondrial FAO. b Lectin-stained retinal flat-mount of P17 OIR treated with vehicle (n = 14 retinas) or etomoxir (n = 13 retinas). Littermate pups were injected intraperitoneally twice daily with etomoxir (27 mg/kg per day) or vehicle (0.9% saline) from P12 to P17. Scale: 500 μm. c Dot plot of retinal Sirt3 expression in OIR (P14 and P17) and EC subtypes (P17), showing only significant increase in astrocytes (12.5%, p = 0.008). d Lectin-stained retinal flat-mount of WT and Sirt3−/− mice (n = 28 retinas each) exposed to the OIR model (P17). Scale: 500 μm. e Metabolic cages were used to measure the O2 consumption (vO2) and CO2 production (vCO2) from 6-month-old WT and Sirt3−/− mice (n = 3 each). Respiratory Exchange Ratio (RER) ≥ 1 indicates carbohydrates as the predominant fuel source. f in vivo glucose uptake in WT and Sirt3−/− retinas (n = 8 each) following OIR. Bar graph shows the mean ( ± SEM) retinal radioactivity counts of 2-[3H] deoxyglucose (DG) tracer relative to WT. DPM: Disintegration per minute. g Graphical representation of fatty acyl-CoA degradation enzymes and their deacetylation by SIRT3. h Heatmap of fatty acylcarnitine metabolites in OIR P14 WT (n = 4 mice) and Sirt3−/− (n = 3 mice) retina from acylcarnitine-targeted metabolomics analysis. i UMAP and j lollipop plot of cell type prioritization score (AUGUR) from single-cell RNAseq of WT (n = 5; 4047 cells) and Sirt3−/− (n = 5; 3639 cells) retinas during the neovascularisation phase of OIR (P14-P17 combined). AUC = area under the curve. k UMAP of endothelial subclusters from WT (n = 5; 1875 cells) and Sirt3−/− (n = 5; 1949 cells) retinas (P14-P17 combined). l Percent of tip (WT = 321 cells, Sirt3−/−=327 cells) and tuft ECs (WT = 16 cells, Sirt3−/−=15 cells) out of the total number of ECs per genotype and time point. m Heatmap representing the log2 fold change of normalized GSVA score for metabolic and angiogenic pathways between WT and Sirt3−/− tip and tuft ECs, and neovascular-related cell types (P14-P17 combined). Bar graph of mean (±SEM) VO (blue) and NV (yellow) areas relative to the total retinal area (b,d). Statistical significance was established using two-tailed Student’s t-tests (b, d, f).
Mitochondrial SIRT3 is an interesting metabolic target due to its central role in regulating cellular energy homeostasis without entirely inhibiting FAO. SIRT3 enhances the activity of essential enzymes of FAO22, the Krebs cycle32,33, and the respiratory chain34 (Fig. 4a). SIRT3 directly deacetylates HADHA and ACADVL35 (Supplementary Fig. 4a), two FAO enzymes predominantly enriched in the neovascular unit (Fig. 2e). During OIR, Sirt3 expression increased significantly in astrocytes (12.5% of cells, P = 0.008), whereas its expression was limited in EC (2%) and absent in tuft EC by scRNAseq (Fig. 4c). Accordingly, conditional EC deletion of Sirt3 (Cdh5-CreERT2, Sirt3lox/lox) did not impact the vascular phenotype of transgenic mice exposed to OIR (Supplementary Fig. 4b–d). Interestingly, global Sirt3 deletion (Sirt3−/−) markedly reduced pathological neovascular tuft (NV) and vaso-obliteration (VO) compared to wild-type (WT) retinas (Fig. 4d), akin to the effects of etomoxir but without increased mortality or apparent deleterious consequences. Hence, Sirt3 depletion of the neurovascular niche, but not EC alone, reduced pathological angiogenesis.
Next, we examined the metabolic effects of Sirt3 depletion. Using metabolic cages, Sirt3−/− mice displayed a higher exchange ratio (vCO2/vO2) during their active nocturnal phase, indicating a preference for carbohydrate metabolism over lipid reliance (Fig. 4e). We also observed increased glucose uptakes in Sirt3−/− retinas compared to WT, using trace amounts of radioactively labeled 2-deoxyglucose (DG) in mice exposed to OIR (Fig. 4f); 2-DG is a glucose analog that is not metabolized by the retina. Their acyl-carnitine profiles revealed that Sirt3 deletion prevented the increase in total acylcarnitines noted in WT retinas during OIR (Supplementary Fig. 2c). Indeed, reduced levels of fatty acylcarnitine metabolites were measured in mutant retinas compared to WT during OIR (Fig. 4g, h), underscoring the importance of SIRT3 in mitochondrial FAO.
To define the transcriptional effects of Sirt3 deletion during pathological angiogenesis, we repeated a single-cell RNAseq of EC-enriched retinal cell suspensions. The enrichment strategy improved EC yields, but other retinal cell types were also detected, except for retinal ganglion cells (Fig. 4i). To identify which retinal cell types were most impacted by the global deletion of Sirt3 at a transcriptional level, we employed a machine-learning approach using a Random Forest Classifier termed Augur36. Based on Augur results, EC and macroglial cells, comprising Müller cells and astrocytes, were the most impacted cell types in our model (Fig. 4j). In Sirt3 depleted retinas, the EC composition transitioned rapidly from a more proliferative neovascular profile at P14 compared to WT (tuft, tip, and proliferative EC: 43.7% vs. 38.2%) to a more quiescent EC composition at P17 (16.1% vs 23.7%), resembling the normoxic retina (Fig. 4k and Supplementary fig. 4e). At P17, tuft EC were barely detected (0.1 % vs 0.7%) in Sirt3−/− retinas (Fig. 4l). This reduction in pathological angiogenesis in Sirt3-depleted retinas (Fig. 4d, l) was associated with a metabolic shift from FAO to glycolysis within the vascular niche, particularly in tuft EC and astrocytes (Fig. 4m).
Sirt3 depletion alters the metabolic and angiogenic landscape of the neovascular niche
Since Sirt3 was mainly expressed in astrocytes (Fig. 4c), we characterized the metabolic impact of Sirt3 depletion in human retinal astrocytes exposed to hypoxia to mimic the ischemic retinal environment of PR. Using a Seahorse analyzer, Sirt3-depleted astrocytes (siSIRT3) exhibited higher glycolysis and glycolytic capacity than controls (scrRNA, Fig. 5a, b). In contrast, their basal oxygen consumption rates (OCR) and ATP-linked respiration were not significantly impacted (Fig. 5c), suggesting a Warburg-like effect (Fig. 5d). In turn, Sirt3 deletion altered the interactome of the vascular niche with tip and tuft EC (Fig. 5e), dampening inflammatory and proliferative signals observed in WT retinas during OIR (Supplementary Fig. 5a–d). Notably, astrocytes of Sirt3-depleted retinas expressed more Vegfa (5-fold increase) and other important angiogenic factors (Fig. 5f, g) to levels comparable during retinal development (P6-P10) (Supplementary Fig. 5e–g). This was also observed in vitro, where silencing Sirt3 further increased hypoxia-induced Vegfa expression in human cultured astrocytes (Supplementary Fig. 5h).
a–d Human retinal astrocytes (35000 cells/well) under hypoxia were treated with scrambled siRNA (scrRNA) or siRNA against Sirt3 (siSIRT3) and characterized using a Seahorse metabolic analyzer. a Glycolysis stress tests measured changes in extracellular acidification rates (ECAR, mean ± SEM) to calculate b glycolysis and glycolytic capacity between control (scrRNA, n = 5 wells) and Sirt3-depleted astrocytes (siSIRT3, n = 5 wells). c Mitochondrial stress tests measured changes in oxygen consumption rates (OCR, mean ± SEM) between control (scrRNA, n = 13 wells) and Sirt3-depleted astrocytes (siSIRT3, n = 9 wells). d Energy map of ATP-linked respiration and the glycolytic capacity of scrRNA and siSIRT3 astrocytes (mean ± SEM) from a–c. e Circos Plot from NicheNet analysis showing the differential communication between WT and Sirt3-/- neovascular ligands and tip and tuft EC receptors in OIR retinas based on scRNAseq data (P14-P17 combined). Selected ligands were differentially expressed between WT and Sirt3-/- neovascular cells (log2FC > 0.25, % expression > 40%). Selected receptors were differentially expressed between WT and Sirt3-/- tip (left) or tuft (right) ECs (log2FC > 0.25, % expression > 10%). f Dot plot representing the differential expression of selected ligands from WT and Sirt3-/- retinal neovascular cells based on NicheNet analysis. g Bar graph depicting log2 FC of Vegfa expression between Sirt3-/- versus WT cell types of the neovascular unit based on scRNAseq data (P14/P17 combined). h Lectin-stained retinal flat-mount of P17 Sirt3lox/lox mice treated with intravitreal injection of PBS (n = 7 retinas), pAAV.GFAP.GFP (n = 6 retinas) or pAAV.GFAP.Cre (n = 13 retinas) and exposed to the OIR model. Littermate Sirt3lox/lox pups were injected intravitreously at P7, one eye with pAAV.GFAP.cre and the other eye with either PBS or pAAV.GFAP.GFP. Bar graph of VO (blue) and NV (yellow) areas relative to the total retinal area (mean ± SEM). Scale: 500 μm. i Graphical representation of the neovascular niche in proliferative retinopathy. Statistical significance was established using two-tailed Student’s t-test (b) and one-way ANOVA (h) with Tukey post hoc analysis. ns: not significant.
To confirm the critical role of Sirt3 in retinal astrocytes, we infected Sirt3lox/lox retinas with AAV2 viruses carrying a GFAP-driven Cre recombinase, which explicitly targets neuroglial cells37 (Supplementary Fig. 5i). The virus was delivered by intravitreal injection at P7, before OIR. Similar to Sirt3−/− OIR retinas, selective depletion of Sirt3 in astrocytes and activated Müller cells (AAV2-GFAP-Cre) reduced vaso-obliteration (VO) compared to control contralateral retinas injected with AAV2-GFAP-GFP or PBS (Fig. 5h), indicating accelerated retinal revascularization. However, tuft formation (NV) remained unchanged, suggesting the involvement of additional neovascular niche cells. Astrocytes classically form a physical path and secrete VEGF, guiding and enabling physiological vascular growth4,7. In OIR, the shift in the vascular niche metabolism and the higher VEGF secretion from astrocytes were associated with more tip and tuft EC in Sirt3−/− retinas at P14 (Fig. 4l). At this early stage in retinal revascularization (P14), neovascular cells are not yet fully committed, and tufts are barely visible histologically. Surprisingly, fewer tuft EC were observed at P17 in Sirt3−/− retinas, raising the possibility that early tuft EC fate was altered due to their microenvironment (Fig. 5i).
Sirt3 depletion reprograms early neovascular tufts for regenerative angiogenesis
Given that EC behavior adapts to their environment, we explored whether the angiogenic shift noted in the Sirt3−/− neovascular niche could prompt tuft EC to adopt a tip-like endothelial fate. Indeed, despite an early increase in tuft EC at P14, the ratio of tip to tuft EC significantly increased at P17 in Sirt3−/− retinas (Fig. 6a), suggesting a transition from pathological to physiological angiogenesis in the mutant retinas. Moreover, analysis of transcriptional trajectory (using Monocle 3 and RNA velocity) showed that in contrast to WT, tuft EC were still connected to tip cells in Sirt3−/− retinas (Fig. 6b and Supplementary Fig. 6a), raising the possibility that they could be reprogrammed to take on a physiological fate.
a Bar plot representing the ratio of tip to tuft ECs (left) and inversely (right) during the neovascularisation period (P14-P17) in WT and Sirt3−/− OIR retinas. b UMAP of single-cell RNAseq from WT and Sirt3−/− neovascular cells (tip cells and tuft ECs) during the neovascularisation phase (P14-P17), showing the connectivity between cells through a trajectory analysis performed with Monocle 3. c Ridge plot of Tip and Tuft ECs from OIR WT and Sirt3−/− retinas at P14 and P17 representing the normalized GSVA score for the Physiological angiogenesis gene set as previously defined from the Tip cell vs Tuft ECs signature (Fig. 3h). d Dot plot of gene expression in tip and tuft ECs from P14 OIR WT and Sirt3−/− retinas for Tip and Tuft ECs-related pathways as previously defined from the tip cell vs tuft ECs signature (Fig. 3g). e Representative images of tip cells forming motile filopodia in WT OIR and Sirt3−/− OIR retinas at P14; staining with lectin. Quantification of the average number (±SEM) of filopodia per tip cells in WT (n = 25 tip cells) and Sirt3−/− (n = 10 tip cells) retinas exposed to OIR. Scale: 10 μm. f Lectin-stained retinal flat-mount of WT and Sirt3−/− mice exposed to the OIR model. The VO areas (blue) are calculated relative to the total retinal area. Scale: 500 μm. Bar graphs show the average percentage (±SEM) of retinal revascularization of max VO relative to P12 WT. We compared Sirt3−/− (P12 n = 26 retinas, P14 n = 18 retinas, P17 n = 30 retinas) to WT (P12 n = 26 retinas, P14 n = 24 retinas, P17 n = 28 retinas) retinas at each timepoints. g Graph of PhNR at 10 cd.s/m2 from P21 OIR WT (n = 8) and Sirt3−/− (n = 14) retinas. Bar graphs show the average amplitudes (±SEM) in WT and Sirt3−/− for global b-wave, PhNR to baseline and global PhNR. Statistical significance was determined using two-tailed Student’s t-tests (e–g).
Considering that FAO distinctly characterizes tuft from tip EC (Fig. 3), we examined the expression of FAO genes in tuft EC of Sirt3−/− retinas. Using GSVA and differential quantitative set analysis for gene expression (QuSAGE38), we identified a marked reduction in FAO pathways in Sirt3−/− tuft EC, primarily due to reduced gene expression of Acadl, Acadm, and Hadha (Supplementary Fig. 6b,c). Given the predisposition of tuft EC to proliferate, possibly aided by FAO18, we compared the expression of cell cycle genes coding for proliferation (G2/M) or cell cycle arrest (G1) in both tuft and tip EC. We observed that, at P14, tuft EC in Sirt3−/− retinas were less proliferative than WT (30% vs. 80%), akin to the reduced proliferation index of migratory tip cells (~30%, Supplementary Fig. 6d). Hence, Sirt3 deletion prevented tuft EC from acquiring defining traits of tuft identity.
Finally, we investigated if the initial reduction in FAO and proliferation of tuft EC in Sirt3−/− retinas might correlate with a comprehensive transcriptional shift towards a tip-cell-like identity. Using GSVA and a pre-established tip cell gene signature (Fig. 3g), we found that early tuft EC (P14) exhibited a transcriptional profile resembling physiological tip cells, more so than their WT counterparts (Fig. 6c). We then analyzed pathways that define tip cell identity at P14 (Fig. 3h), a critical time point for EC fate specification in OIR. Tip cells in WT and Sirt3−/− retinas shared analogous expression profiles (Fig. 6d). However, tuft EC of Sirt3−/− retina began expressing tip cell markers, focal adhesion, hypoxia-regulated, and glycolytic genes (Fig. 6d) to levels comparable to tip cells. The findings corroborated with the elevation of hypoxia, glycolysis, and sprouting angiogenesis pathways in Sirt3−/− retinas, in contrast to WT (Fig. 4m). These pathways are characteristic transcriptional traits of tip cells39. Correspondingly, Sirt3 deletion markedly increased the number of early tip cell filopodia (P14; Fig. 6e) and accelerated revascularization of the ischemic neuroretina in OIR at P14 and P17 without significantly affecting maximal vaso-obliteration at P12 (Fig. 6f). More importantly, prompt revascularization of Sirt3−/− retinas improved later inner neuroretinal and RGC function (at P21) assessed by the photopic negative response40 (PhNR) of full-field electroretinogram (ERG, Fig. 6g). Hence, Sirt3 deletion within the neovascular niche shifted the transcriptional identity of tuft EC to resemble tip cells, thereby accelerating the physiological vascular regeneration of the ischemic neuroretina in PR and improving vision.
Discussion
Recognizing the unique attributes of healthy and diseased blood vessels and their microenvironment could pave the way for more targeted and efficacious therapies against vascular diseases. The lack of a suitable murine model that accurately replicates human proliferative retinopathies (PR) is a challenge in the field. Poor glucose control in diabetics and extreme prematurity in neonates correlate with neovascular retinal disease in humans but not in mice. The most commonly used murine model of PR is the oxygen-induced retinopathy (OIR) model27, giving rise to the predictable formation of pathognomonic tufts that resemble human retinal proliferative neovessels. Interestingly, we observed comparable FAO metabolite signatures in both human diabetic PR and murine OIR samples, suggesting a shared metabolic dysregulation in neovascular disease despite their distinct etiologies. This study uncovered a distinct transcriptional signature for pathological tuft EC, a defining feature of PR and a leading cause of blindness. Unlike healthy tip cells, these pathological EC exhibited a preferential metabolic dependency on FAO. Notably, shifting the metabolic program of the vascular niche from FAO to glycolysis in Sirt3−/− retinas reduced pathological neovascular tufts and promoted healthy retinal revascularization.
Pathological neovascular tufts are portrayed as misdirected tip cells invading the vitreous9 that are more proliferative and leaky, resulting in retinal edema41. Through single-cell transcriptomics, we found a novel subset of EC that, while displaying multiple tip cell markers such as ESM1, were less prone to migrate and more inclined to proliferate. The new EC sub-cluster expressed high levels of aquaporin 1 (AQP1) which we localized to pathological neovascular tufts. In tumor models, Aqp1 directly contributes to EC migration, sprouting, and tubulogenesis42, implying a direct role in pathological angiogenesis43. Hence, AQP1 uniquely labels pathological tuft EC in PR and could be a potential therapeutic target to curb pathological neovascularization in proliferative vascular diseases.
Using their distinct transcriptional signature, we showed that unique metabolic profiles defined tip and tuft EC. In both human neonates and mice, aberrant vascular growth is ushered by an increase in the neuroretina’s metabolic demands, pointing to the pivotal role that retinal metabolism plays in determining EC fate5. Unbiasedly comparing tip and tuft EC’s most enriched transcriptional pathways revealed divergent metabolic preferences: tip cells favored glycolysis, whereas tuft cells leaned towards FAO. Notably, glycolysis is less dependent on oxygen for energy production and cellular growth, a phenomenon known as the Warburg effect, while FAO necessitates mitochondrial respiration44. This metabolic specialization aligns anatomically with the ___location of tip EC at the leading edge of the oxygen-poor, avascular neuroretina. In contrast, neovascular tufts are found at the confluence of venous capillaries45, an area richer in oxygen. FAO is a fuel source for the neuroretina46 and serves as a biosynthetic pathway promoting EC proliferation18. Unlike glycolysis, FAO is not associated with the increased migration typical of tip cells14. Hence, distinct metabolic pathways define the behavior of glycolytic tip cells, essential to the regenerative process, in contrast to misguided yet actively proliferating tuft EC that rely on FAO. We speculate that using FA as an alternative fuel substrate in better-perfused regions could limit glucose uptake in tufts and surrounding cells, thereby preserving glucose for critical revascularization and diffusion into the avascular retina to nourish hypoxic neurons. Hence, metabolic heterogeneity could help sustain the regenerating retina and is not necessarily in contradiction with an overall reduction in mitochondrial function in PR avascular regions. Crucially, these distinct metabolic profiles for healthy and pathological angiogenesis become apparent at specific stages of disease development, presenting a potential therapeutic window for targeted interventions.
Localization of the metabolic and angiogenic signals shapes regenerative angiogenesis. Sirt3 expression was only significantly increased in astrocytes in mouse PR and was not detected in tuft EC. In the absence of Sirt3, astrocytes exhibited a pronounced metabolic shift towards glycolysis and elevated angiogenic signaling, with a 5-fold increase in Vegfa expression, comparable to levels seen in the developing retina (P6). Given that astrocytes act as a scaffold to guide migrating EC during retinal development, they could provide localized signals to guide beneficial revascularization in PR. PR treatments aim to lower VEGF concentrations after neovascular tuft formation has taken place, irrespective of its source. Our findings highlight the importance of the cellular source of growth factors, including VEGF, to guide healthy retinal revascularization, not merely its concentration. VEGF has multiple neuroprotective roles that could be leveraged to enhance neuronal function47. Timely revascularization and the redistribution of VEGF expression in supporting neuroglial cells may contribute to restoring inner retinal function, as indicated by ERG. Therefore, modifying the metabolic topography of the vascular niche, especially in astrocytes, could help steer EC toward a more regenerative path, thereby improving vision.
Maintaining lower oxygen saturation levels is the mainstay of retinopathy of prematurity (ROP) prevention48, which might contribute to EC reprogramming. Within limits, however, since more severe hypoxia, although beneficial to ROP, is associated with increased mortality49. Hypoxia blocks mitochondrial respiration, forcing tissues to rely on glycolysis instead50,51, as we observed in SIRT3-depleted mice. In mouse models of mitochondrial diseases, exposure to chronic hypoxia is protective by diverting energy metabolism away from mitochondrial oxidative phosphorylation and reducing oxidative stress50. In the OIR model, pharmacological stabilization of hypoxia-inducible factor (HIF) also shifts the retina towards aerobic glycolysis, improving retinopathy52. Similarly, Sirt3 null mice shifted their metabolism from FAO towards glycolysis53, recreating a pseudo-hypoxic state that could pre-condition mice for ischemic stress in proliferative retinopathy. Thus, if administered locally in the eye, targeting SIRT3 could favor a regenerative phenotype while avoiding some of the harmful consequences of severe hypoxia. Then again, SIRT3 was reported to have protective antioxidant roles in photoreceptors54. Fortunately, SIRT3 was not significantly expressed in photoreceptors during PR, and Sirt3 depletion alone did not negatively impact vision in other models, suggesting protective effects of other mitochondrial sirtuins, such as SIRT555,56.
Our current therapies target pathological neovessels that emerge in the later phases of PR. In contrast, our research aims to enable early physiological vascular regeneration to minimize neuroretinal ischemia and improve vision. Targeting SIRT3 shifted the metabolic environment of the vascular niche, steering EC fate towards a regenerative vascular phenotype. This work expands our understanding of the distinct metabolic and transcriptomic landscapes of healthy and diseased vessels and their microenvironment, offering insights for developing targeted therapies against vascular diseases57,58. Additionally, our findings have implications for other neuro-ischemic conditions like stroke, where enhancing regenerative angiogenesis could preserve neuronal function59.
Methods
Human subjects
The study conforms to the tenets of the Declaration of Helsinki, and approval of the human clinical protocol and informed consent were obtained from the Maisonneuve-Rosemont Hospital Ethics Committee (CER: 10059). All patients previously diagnosed with proliferative diabetic retinopathy or epiretinal membrane were followed clinically, and surgery was performed by a single vitreoretinal surgeon when indicated by ‘standard-of-care’ guidelines (Supplementary Table 1). The collection was performed prior to 2017, and informed written consent was obtained. Patients with epiretinal membranes represent appropriate controls because they don’t exhibit proliferative retinopathy but still need surgery, allowing the collection of vitreous fluid under informed consent. Undiluted vitreous samples were aspirated in the region adjacent to neovascular tufts or epiretinal membrane (control) and were frozen on dry ice immediately after biopsy and stored at –80 °C. All patients received their first anti-VEGF injection after vitreous sampling; they did not have prior anti-VEGF or photocoagulation treatment. Medication details are provided in Supplementary Table 1, except for four deceased diabetic patients whose records were no longer available (NA). Sex and gender factors were not analyzed due to insufficient statistical power when disaggregated.
Animal care
Animal procedures complied with the Animal Care Committee of CHU Sainte-Justine (CIBPAR Nagano 2024-5421#712), following the principles of the Guide for the Care and Use of Experimental Animals developed by the Canadian Council on Animal Care. All in vivo work adhered to the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research. S129 (#002448), mutant mice with Sirt3 deletion (129-Sirt3tm1.1Fwa/J, #012755), CAG-tdTomato reporter mice (#007914), and Sirt3lox/lox mice (#031201) were obtained from The Jackson Laboratory. Cdh5-CreERT2 mice were kindly provided by Dr. Ralf Adams (Max Planck Institute, Germany). Mutant mice did not carry Pde6b (rd1) or Crb1 (rd8) mutations, and a single-nucleotide polymorphism panel analysis confirmed that S129 (#002448) and Sirt3−/− (#012755) had comparable genetic backgrounds. Mice were housed under a standard 12-hour light-dark cycle and had ad libitum access to water and chow. Animals were monitored daily for general health status, body weight, hydration, and signs of distress or discomfort. Humane endpoints, including sustained weight loss exceeding 15%, lethargy, respiratory distress, or severe morbidity, were established. Animals meeting these endpoints were promptly euthanized using CO₂ asphyxiation followed by cervical dislocation, per institutional guidelines. Pups weighing less than 6 grams or more than 9 grams on post-natal (P) day 14 or 17 (P14, P17) were excluded. Both female and male littermates were used, but sex information was not collected. All animals were sacrificed by lethal intraperitoneal (i.p.) injections of pentobarbital at P12, P14, or P17 for analyses.
Oxygen-induced retinopathy model
Mice pups and their adoptive lactating S129 mother were exposed to 75% oxygen from P7 to P12, as first described27. Mice were returned to room air at P12 until used for experimentation. All animals were euthanized before ocular enucleation. Littermate controls, as well as age and weight-matched mice, were injected intraperitoneally twice daily with etomoxir (27 mg/kg per day) or vehicle (0.9% saline) from P12 to P17 and euthanized at P17. 4-OH tamoxifen (5 μg) was injected intraperitoneally daily for 3 days (P12-P14) and euthanized at P17.
Human vitreous metabolomics
Human vitreous metabolite extracts were analyzed using two liquid chromatography-tandem mass spectrometry (LC-MS) methods to measure polar metabolites, as described previously60. From vitreous samples, negative ion mode profiling samples were prepared from 30 µl extracted with 120 µl of 80% methanol containing inosine-15N4, thymine-d4, and glycocholate-d4 internal standards (Cambridge Isotope Laboratories, MA). In comparison, samples for positive ion mode profiling were prepared by extracting 10 µL with 90 µl of acetonitrile/methanol/formic acid (74.9:24.9:0.2 v:v:v) containing valine-d8 and phenylalanine-d8 internal standards (Cambridge Isotope Laboratories, MA). Negative ion mode data were acquired by injecting extracts (10 µL) onto a 150 × 2.0 mm Luna NH2 column (Phenomenex, CA). The column was eluted at a flow rate of 400 µl/min with initial conditions of 10% mobile phase A (20 mM ammonium acetate and 20 mM ammonium hydroxide in water) and 90% mobile phase B (10 mM ammonium hydroxide in 75:25 v/v acetonitrile/methanol) followed by a 10 min linear gradient to 100% mobile phase A. MS analyses were carried out using electrospray ionization in the negative ion mode using full scan analysis over m/z 70–750 at 70,000 resolution and 3 Hz data acquisition rate. Additional MS settings were ion spray voltage, −3.0 kV; capillary temperature, 350 °C; probe heater temperature, 325 °C; sheath gas, 55; auxiliary gas, 10; and S-lens RF level 50. Positive ion mode data were acquired by injecting extracts (10 µl) onto a 150 × 2 mm, 3 µm Atlantis HILIC column (Waters, MA). The column was eluted isocratically at a flow rate of 250 µl/min with 5% mobile phase A (10 mM ammonium formate and 0.1% formic acid in water) for 0.5 minutes, followed by a linear gradient to 40% mobile phase B (acetonitrile with 0.1% formic acid) over 10 minutes. MS analyses were carried out using electrospray ionization in the positive ion mode using full scan analysis over 70–800 m/z at 70,000 resolution and 3 Hz data acquisition rate. Other MS settings were: sheath gas 40, sweep gas 2, spray voltage 3.5 kV, capillary temperature 350 °C, S-lens RF 40, heater temperature 300 °C, microscans 1, automatic gain control target 1e6, and maximum ion time 250 ms. Raw data were processed using TraceFinder 3.3 and 4.1 software (Thermo Scientific, MA) and Progenesis QI (Nonlinear Dynamics, UK). For each method, metabolite identities were confirmed using authentic reference standards.
Mouse retinal lipidomics
Metabolic profiling was performed by LC-MS on samples pooled from both retinas of P14 mice; samples were analyzed for fatty acylcarnitine species and beta-oxidation intermediate metabolites. Retinas were harvested after sacrificing P14 mice and immediately snap-frozen in liquid nitrogen. The acylcarnitines were extracted by protein precipitation (PP) and derivatized with butanol-HCl for analysis by LC/MS/MS. The samples were diluted with 400 µl solution of methanol with eight ISTD. After 1.5 minutes of homogenization in a bead Ruptor12 from Omni International Inc., samples were centrifuged for 5 minutes at 12,000 rpm. The supernatant was transferred in a 2 ml polypropylene tube for evaporation under nitrogen. When dry, 100 µl of butanol-HCl (3 N) is used for butanolysis performed by heating at 55 °C for 20 min. After evaporation under nitrogen, the residue was reconstituted in 100 µl of mobile phase (ACN:H2O 80:20 with 0.05% of formic acid). Twenty microliters were injected in flow injection onto an Alliance 2795 LC coupled to a Quattro micro MS/MS (Waters). Data were recorded in positive electrospray ionization and analyzed with Neolynx from Waters Corp. The average of two technical replicates (2 LC/MS/MS reads/sample) was recorded.
Metabolomics data analysis
Human metabolomics profiles were analyzed using MetaboAnalyst23. Data were filtered based on the interquartile range for further statistical comparisons. We used a Random Forest (RF) classifier to identify outliers based on proximities during tree construction, utilizing the randomForest R package and PlotRF. Glucuronate and urate levels contributed the most to classifier accuracy. Outliers exhibited elevated levels of cotinine, hydroxycotinine (PDR 153), ceramide (PDR 126), caffeine (PDR 144), and bilirubin (ERM 136). Outliers detected by the Random Forest algorithm were removed, and PCA, t-test, AUC test, and Metabolite Set Enrichment Analysis were performed on auto-scaled data previously normalized on internal standard (Phe-d8). Mouse acylcarnitine profiling was performed on unfiltered, auto-scaled values from MetaboAnalyst23 followed by PCA and hierarchical clustering (dendrogram and heatmap).
Calorimetry/Metabolic chambers
Mice (5-6 months old) were acclimatized to the metabolic cages for the first 24 hours and evaluated for the next 5 days. Mice had free access to food and water. The consumption of oxygen (vO2), the production of carbon dioxide (vCO2), the ratio of gaseous exchange (RER), the heat production, and the physical activity were repeatedly collected with the Oxymax/clams calorimetry system (Colombus Instruments). The weight of every animal was measured before and after the stay in metabolic cages.
Droplet Sequencing (Drop-seq)
Drop-seq procedure was done on endothelial enriched cell suspension isolated from mouse retinas. Briefly, single-cell suspensions were prepared from P14 and P17 retina, as reported61, through successive steps of digestion (using papain solution; Worthington, LK003150), trituration, and filtration to obtain a final concentration of 120 cells/μl. According to the manufacturer’s protocol, endothelial cells were enriched using CD31 microbeads (Miltenyi Biotech, 130-097-418). Droplet generation and cDNA libraries were performed as described in the Drop-seq procedure61, and sequencing was done on Illumina NextSeq 500.
Unique molecular identifier (UMI) counts for WT and/or Sirt3–/– scRNAseq replicates were merged into one single Digital Gene Expression (DGE) matrix and processed using the Seurat package62. Cells expressing less than 100 genes and more than 10% of mitochondrial genes were filtered out. Single-cell transcriptomes were normalized by dividing by the total number of UMIs per cell and then multiplying by 10,000. All calculations and data were then performed in log space. PCA analysis on the most variable genes in the DGE matrix identified 20 significant PCs, which served as input for Uniform Manifold Approximation and Projection (UMAP). We used a density clustering approach to identify putative cell types on the embedded map and computed average gene expression for each identified cluster based on Euclidean distances. We then compared each cluster to identify marker genes differentially expressed across clusters.
Cell type-specific transcriptomic differences between conditions, time points, and genotypes were statistically compared using a negative binomial model. Seurat visualization tools included Ridge Plot, Dot Plot, and UMAP Plot. Single-cell gene expression profiles from each separate cell type identified by scRNAseq were further analyzed using ggplot263, Gene Set Variation Analysis64, EnrichR65, AUGUR36, Psupertime66, NicheNet67, SCENIC68, Monocle369 and Qusage38. For RNA velocity analysis, Drop-seq fastq files were processed with kb-python70 to obtain spliced and unspliced matrices that were further analyzed with Seurat RunVelocity function based on Velocyto71.
RNAscope in situ hybridization and Immunohistochemistry
For RNAscope analysis, experiments were performed per manufacturer instructions on fixed retinal cryosections (12 μm) using the RNAscope 2.5 chromogenic duplex assay (ACD bio-techne). WT and Sirt3–/– eyes at P17 were fixed in paraformaldehyde (PFA) 4% (24 h) at 4 °C. Eyes were then immersed in a sucrose gradient (10 to 30%), frozen in optimal cutting temperature compound (Surgipath FSC22 Clear, Leica), and stored at −80 °C until use. Aqp1 and Hadha mRNA expression were targeted using probes designed by ACD Bio-techne. For cryosection, fixed and cryoprotected samples were embedded in OCT compound (Fisher Scientific; Cat # 23-730-571). Retinal cryosections (10 μm) were blocked with 1% bovine serum albumin (Multicell; Cat #800-095-EG), 0.1% Triton X- 100 (Sigma; Cat #X100)) and 0.05% Tween-20 (Fisher; Cat # BP337-500) for 1 h and labeled overnight at 4 °C with primary antibodies against GFAP (1:100; Millipore-Sigma Cat. #SAB2500462), glutamine synthetase (1:250, Sigma Cat.#MAB302) and AQP1 (1:150, Alomone, AQP-001), followed by secondary antibodies in blocking solution for 2 hours RT. RNAscope and IF retina were counterstained with isolectin B4 (Alexa Fluor 594, I21413; Molecular Probes) or DAPI (Invitrogen; Cat #D21490). Retinal tissues were washed three times for 5 minutes in PBS before a cover slip was attached with Fluoromount Aqueous Mounting Medium (EMS; Cat # 17985). Retinas were then imaged with a Leica DME-6 microscope using a 20X dry objective (HC PL APO 20X/0.75 CS2) and analyzed with ImageJ (NIH). Labeled retinas were examined with a laser scanning confocal microscope (Leica, SP8 DLS).
Intravitreal injection of AAV
AAV-GFAP-Cre plasmid was obtained from Addgene (Plasmid #105550). AAV2/ShH10-GFAP-GFP and AAV2/ShH10-GFAP-Cre vectors were produced and highly purified from an established cell line (HEK293) at Boston Children’s Hospital Viral Core. The ShH10 variant of the AAV-derived capsid has been shown to preferentially infect glial cells and produce sustained transgene expression following intravitreal injection37. The titer of AAV2/SHH10-GFAP-GFP was 1.49 × 1013 gc/ml and AAV2/SHH10-GFAP-Cre was 1.55 × 1012 gc/ml. Mice were anesthetized with 3% isoflurane, and intravitreal injections were performed on deeply sedated animals as we described72. Intravitreal injections of PBS, AAV2/ShH10-GFAP-GFP or AAV2/ShH10-GFAP-Cre vectors (1 μl each) were performed through the eyelid using a 50-gauge glass capillary attached to a micropipette (Hamilton; Cat # 7681C15) that was inserted 1–2 mm behind the ora serrata into the vitreous cavity to avoid damaging the lens. Once the animals had fully recovered from anesthesia, they were subjected to the OIR model. The animals were euthanized 10 days after intravitreal injection with AAV vectors.
Quantification of neovascularization (NV) and vaso-obliterated (VO) areas
Eyes were fixed for 1 hour in 4% paraformaldehyde at room temperature (RT). Retinas were dissected and stained overnight at RT with fluoresceinated isolectin B4 (Alexa Fluor 594, I21413; Molecular Probes) in 1 mM CaCl2 in PBS. Lectin-stained retinas were whole-mounted onto Superfrost Plus microscope slides (Fisher Scientific) with the photoreceptor side down and embedded in SlowFade Antifade Reagent (Invitrogen). Stained retinas were flat-mounted, and the pictures were taken with an epifluorescence slide scanner, Zeiss Axio Scan.Z1 (Zeiss) at 10x magnification. The neovascular (NV) and vaso-obliterated (VO) areas were quantified using the SWIFT_NV program73.
Cell culture
Human retinal astrocytes (HRAs) (1870, ScienCell, USA) free of pathogens were cultured in Astrocyte Medium (1801, ScienCell, USA), supplemented with 10% fetal bovine serum (FBS) and 1% antibiotic-antimycotic solution. Cells were maintained at 37 °C in a 5% CO₂, and only passages 5–10 were used for the experiments. HRAs were transfected with either siRNA targeting SIRT3 (20 nM, L-004827-01-0005, Dharmacon, Canada) or scrambled RNA control (scrRNA) using HiPerFect transfection reagent (301704, Qiagen, Germany) on the second day after seeding. Maximum gene depletion was achieved 72 hours post-transfection. Cells were then exposed to hypoxia (5% O₂) or normoxia for 6 hours before RNA extraction (2 × 105 cells/well) or 4 hours before Seahorse assays (3.5 × 104 cells/well).
Quantitative RT-PCR
Total RNA was extracted using the RNeasy Mini Kit (74106, Qiagen, Germany) according to the manufacturer’s instructions. For RT-qPCR, 1 μg of total RNA was reverse-transcribed using the QuantiTect Reverse Transcription Kit (205314, Qiagen). Quantitative PCR was performed with iTaq Universal SYBR Green SuperMix (1725124, Bio-Rad, USA) on a LightCycler® 480 System (Roche, Switzerland). Melt curve analysis was conducted to confirm the specificity of the PCR products. Gene expression fold-changes were calculated to GAPDH from normoxic control (norm scrRNA) using the ΔΔCt method.
Primer sequences were:
Sirt3_human_F = ACCCAGTGGCATTCCAGAC, Sirt3_human_R = GGCTTGGGGTTGTGAAAGAAG, Vegfa_Human_F = AGGGCAGAATCATCACGAAGT, Vegfa_Human_R = AGGGTCTCGATTGGATGGCA, Gapdh_human_F = GAAGGTGAAGGTCGGAGT, Gapdh_human_R = GAAGATGGTGATGGGATTTC.
Seahorse assay
The oxygen consumption rate (OCR) and extracellular acidification rate (ECAR) were measured using a Seahorse XFe 96 Flux Analyzer. Human retinal astrocytes (HRAs) transfected with siSIRT3 (20 nM) or scrRNA were seeded in 96-well plates at a density of 3.5 × 10⁴ cells per well. Two days post-transfection, cells were exposed to hypoxia (FiO2 5%) or normoxia for four hours. One hour before the assay, cells were incubated in either Mito Stress Test or Glycolysis Stress Test media under their respective oxygen conditions. The Mito Stress Test medium contained DMEM 5030 supplemented with 10 mM D-glucose (GLU501.5, BioShop Canada), 1 mM sodium pyruvate (P2256, Sigma-Aldrich), 2 mM L-glutamine (609-065-EL, WISENT, INC), and 5 mM HEPES (600-032-CG, WISENT). The Glycolysis Stress Test medium contained DMEM 5030 (Sigma-Aldrich) supplemented with 2 mM glutamine. Following equilibration, OCR and ECAR were measured. The Seahorse Mito Stress Assay (Agilent) consisted of sequential injections of oligomycin (3 µM, O4876, Sigma-Aldrich, USA), FCCP (2 µM, ab120081, Abcam, USA), and rotenone (1 µM, R887, Sigma-Aldrich, USA)–antimycin A (1 µM, A8674, Sigma-Aldrich, USA) (RAA). For the Glycolysis Stress Assay, cells were treated with 10 mM D-glucose, 3 µM oligomycin, and 100 µM 2-deoxy-D-glucose (SC-202010A, Santa Cruz, USA). These assays were used to assess basal respiration and ATP-linked respiration in the Mito Stress Test, as well as glycolysis and glycolytic capacity in the Glycolysis Stress Test. Results were normalized to the number of cells per well (quantified with DAPI).
Retinal glucose uptake assay
Consumption of glucose was measured using 2-[3H]deoxyglucose (DG) as we reported46. Mice received a daily intraperitoneal injection of 0.5 µL of 2-[3H]DG (1 µCi/µL) from P12 to P17. Animals were sacrificed at P17, 60 minutes after the last injection, to ensure cellular incorporation of the radiotracer. Retinas were collected and homogenized in a scintillation cocktail (Ecolite +; MP Biomedicals), and beta counts were measured using an LS6500 Multipurpose Scintillation Counter (Beckman). Disintegrations per minute (DPM) counts were normalized to the total injected dose and the weight of each animal.
Electroretinogram (ERG) analysis
Experiments were performed on P21 Sirt3−/− and WT S129 mice after OIR according to ISCEV extended protocol for PhNR ERG40. A computerized system with an electronically controlled Ganzfeld dome was used (Espion E2 with Colordome; Diagnosys LLC, USA). ERGs were recorded from the corneal surface of each eye after pupil dilation with ophthalmic solution (1% Isopto®, Atropine Sulfate and 2.5% Mydfrin™, phenylephrine hydrochloride) using a DTL plus fiber electrode™ (Diagnosys LLC, USA). For all the recordings, ground and reference needle electrodes were placed subcutaneously in the tail and in the front of the head, respectively. Impedance was maintained at <5 kΩ. P21 mice were anesthetized by intraperitoneal injection of ketamine (10 mg/kg) and xylazine (20 mg/kg), and the mice were placed on a temperature-regulated heating pad during recording periods. The photopic negative response (PhNR) is a component of the full-field photopic electroretinogram (ERG). The PhNR was elicited by a 10 and 25 cd·s/m2 white flash presented on a 100 cd/m2 cones-saturating green background 1-Hz and 25 sweeps were averaged for each intensity. All ERG responses were filtered at 0.312–45 Hz, and signal averaging was applied. The PhNR amplitude was measured from the baseline to the maximum amplitude in the trough of the negative wave that comes after the b-wave, and also measured from the peak of the b-wave to the maximum amplitude in the same trough (Global PhNR). The template file that allowed the analysis of the electroretinogram data is available at https://github.com/Aghilusius/Template-ERG-Analysis.
Quantification and statistical analysis
Statistical analysis was performed using GraphPad Prism (10.0.3) for Mac (GraphPad Software) or R statistical programming language (4.4.0, R-project.org). Exact n, statistical test, and significance are reported in the Figure Legends. Data are presented as means \(\pm\)± the standard error of the mean (s.e.m.). Between-subject statistical tests were completed with two-tailed independent Student’s t-tests. Comparisons between groups were made using 1-way or 2-way ANOVA followed by the post hoc Tukey or Bonferroni multiple comparisons test among means. The D’Agostino-Pearson or Kolmogorov-Smirnov normality tests were used to confirm a normal distribution. Animals were not randomized, but quantification of the data was performed in a blinded fashion when possible. Outlier results were identified and removed using the ROUT method (Q5%) in GraphPad Prism. Results are presented as mean ± SEM. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. P < 0.05 was considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data supporting the findings of this study are available in the article, its Supplementary information, and the Source Data file. The single-cell RNA-seq data have been deposited in GEO (GSE216676 https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE216676). Publicly available data (GSE174400 https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE174400, GSE150703 https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE150703, GSE148077 https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE148077, GSE165784 https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE165784) were also used in this study. The human metabolomics data has been deposited in Metabolomics Workbench under Project ID: PR002423; Project DOI: doi: 10.21228/M8FC13. Additional information is available from the corresponding authors upon request. Source data are provided with this paper.
Code availability
Custom-written scripts used in this study are available from the corresponding author upon reasonable request. Any additional information required to reanalyze data reported in this paper is available from the lead contact and on github https://github.com/gaelcge/OIRDropseq.
References
Sapieha, P. et al. Retinopathy of prematurity: understanding ischemic retinal vasculopathies at an extreme of life. J. Clin. Invest. 120, 3022–3032 (2010).
Manavski, Y. et al. Clonal expansion of endothelial cells contributes to ischemia-induced neovascularization. Circ. Res. 122, 670–677 (2018).
Duh, E. J., Sun, J. K. & Stitt, A. W. Diabetic retinopathy: current understanding, mechanisms, and treatment strategies. JCI Insight 2, e93751 (2017).
Selvam, S., Kumar, T. & Fruttiger, M. Retinal vasculature development in health and disease. Prog. Retin. Eye Res. 63, 1–19 (2018).
Joyal, J. S., Gantner, M. L. & Smith, L. E. H. Retinal energy demands control vascular supply of the retina in development and disease: The role of neuronal lipid and glucose metabolism. Prog. Retin Eye Res. 64, 131–156 (2018).
Stone, J. et al. Development of retinal vasculature is mediated by hypoxia-induced vascular endothelial growth factor (VEGF) expression by neuroglia. J. Neurosci. J. Soc. Neurosci. 15, 4738–4747 (1995).
Rattner, A., Williams, J. & Nathans, J. Roles of HIFs and VEGF in angiogenesis in the retina and brain. J. Clin. Investig. 129, 3807–3820 (2019).
Sapieha, P. et al. The succinate receptor GPR91 in neurons has a major role in retinal angiogenesis. Nat. Med. 14, 1067–1076 (2008).
Joyal, J.-S. et al. Ischemic neurons prevent vascular regeneration of neural tissue by secreting semaphorin 3A. Blood 117, 6024–6035 (2011).
Fukushima, Y. et al. Sema3E-PlexinD1 signaling selectively suppresses disoriented angiogenesis in ischemic retinopathy in mice. J. Clin. Investig. 121, 1974–1985 (2011).
Pierce, E. A., Avery, R. L., Foley, E. D., Aiello, L. P. & Smith, L. E. Vascular endothelial growth factor/vascular permeability factor expression in a mouse model of retinal neovascularization. Proc. Natl. Acad. Sci. USA 92, 905–909 (1995).
Dorrell, M. I. et al. Maintaining retinal astrocytes normalizes revascularization and prevents vascular pathology associated with oxygen-induced retinopathy. Glia 58, 43–54 (2010).
Eelen, G., de Zeeuw, P., Simons, M. & Carmeliet, P. Endothelial cell metabolism in normal and diseased vasculature. Circ. Res. 116, 1231–1244 (2015).
De Bock, K. et al. Role of PFKFB3-driven glycolysis in vessel sprouting. Cell 154, 651–663 (2013).
Buchwald, P. A local glucose-and oxygen concentration-based insulin secretion model for pancreatic islets. Theor. Biol. Med. Model 8, 20 (2011).
Gatenby, R. A. & Gillies, R. J. Why do cancers have high aerobic glycolysis?. Nat. Rev. Cancer 4, 891–899 (2004).
Schoors, S. et al. Partial and transient reduction of glycolysis by PFKFB3 blockade reduces pathological angiogenesis. Cell Metab. 19, 37–48 (2014).
Schoors, S. et al. Fatty acid carbon is essential for dNTP synthesis in endothelial cells. Nature 520, 192–197 (2015).
Houtkooper, R. H., Pirinen, E. & Auwerx, J. Sirtuins as regulators of metabolism and healthspan. Nat. Rev. Mol. Cell Biol. 13, 225–238 (2012).
Ahn, B.-H. et al. A role for the mitochondrial deacetylase Sirt3 in regulating energy homeostasis. Proc. Natl. Acad. Sci. USA 105, 14447–14452 (2008).
He, W., Newman, J. C., Wang, M. Z., Ho, L. & Verdin, E. Mitochondrial sirtuins: regulators of protein acylation and metabolism. Trends Endocrinol. Metab. 23, 467–476 (2012).
Hirschey, M. D. et al. SIRT3 regulates mitochondrial fatty-acid oxidation by reversible enzyme deacetylation. Nature 464, 121–125 (2010).
Xia, J. & Wishart, D. S. Using metaboAnalyst 3.0 for comprehensive metabolomics data analysis. Curr. Protoc. Bioinforma. 55, 14.10.11–14.10.91 (2016).
Paris, L. P. et al. Global metabolomics reveals metabolic dysregulation in ischemic retinopathy. Metabolomics 12, 15 (2016).
Nawaz, I. M. et al. Human vitreous in proliferative diabetic retinopathy: Characterization and translational implications. Prog. Retin Eye Res. 72, 100756 (2019).
Hu, Z. et al. Single-cell transcriptomics reveals novel role of microglia in fibrovascular membrane of proliferative diabetic retinopathy. Diabetes 71, 762–773 (2022).
Smith, L. E. et al. Oxygen-induced retinopathy in the mouse. Investig. Ophthalmol. Vis. Sci. 35, 101–111 (1994).
Binet, F. et al. Neutrophil extracellular traps target senescent vasculature for tissue remodeling in retinopathy. Science 369, eaay5356 (2020).
Zarkada, G. et al. Specialized endothelial tip cells guide neuroretina vascularization and blood-retina-barrier formation. Dev. Cell 56, 2237–2251.e2236 (2021).
Smith, T. L. et al. eNOS controls angiogenic sprouting and retinal neovascularization through the regulation of endothelial cell polarity. Cell. Mol. Life Sci. 79, 37 (2022).
Schey, K. L., Wang, Z., L. Wenke, J. & Qi, Y. Aquaporins in the eye: Expression, function, and roles in ocular disease. Biochim. et. Biophys. Acta (BBA) - Gen. Subj. 1840, 1513–1523 (2014).
Yu, W., Dittenhafer-Reed, K. E. & Denu, J. M. SIRT3 protein deacetylates isocitrate dehydrogenase 2 (IDH2) and regulates mitochondrial redox status. J. Biol. Chem. 287, 14078–14086 (2012).
Cimen, H. et al. Regulation of succinate dehydrogenase activity by SIRT3 in mammalian mitochondria. Biochemistry 49, 304–311 (2010).
Vassilopoulos, A. et al. SIRT3 deacetylates ATP synthase F1 complex proteins in response to nutrient- and exercise-induced stress. Antioxid. Redox Signal 21, 551–564 (2014).
Yang, W. et al. Mitochondrial Sirtuin network reveals dynamic SIRT3-dependent deacetylation in response to membrane depolarization. Cell 167, 985–1000.e1021 (2016).
Skinnider, M. A. et al. Cell type prioritization in single-cell data. Nat. Biotechnol. 39, 30–34 (2021).
O’Carroll, S. J., Cook, W. H. & Young, D. AAV targeting of glial cell types in the central and peripheral nervous system and relevance to human gene therapy. Front. Mol. Neurosci. 13, 618020 (2021).
Meng, H., Yaari, G., Bolen, C. R., Avey, S. & Kleinstein, S. H. Gene set meta-analysis with Quantitative Set Analysis for Gene Expression (QuSAGE). PLoS Comput. Biol. 15, e1006899 (2019).
Helker, C. S. et al. Apelin signaling drives vascular endothelial cells toward a pro-angiogenic state. Elife 9, e55589 (2020).
Frishman, L. et al. ISCEV extended protocol for the photopic negative response (PhNR) of the full-field electroretinogram. Doc. Ophthalmol. 136, 207–211 (2018).
Claesson-Welsh, L., Dejana, E. & McDonald, D. M. Permeability of the endothelial barrier: identifying and reconciling controversies. Trends Mol. Med. 27, 314–331 (2021).
Zou, L. B. et al. Aquaporin-1 plays a crucial role in estrogen-induced tubulogenesis of vascular endothelial cells. J. Clin. Endocrinol. Metab. 98, E672–E682 (2013).
Saadoun, S., Papadopoulos, M. C., Hara-Chikuma, M. & Verkman, A. S. Impairment of angiogenesis and cell migration by targeted aquaporin-1 gene disruption. Nature 434, 786–792 (2005).
Li, X., Sun, X. & Carmeliet, P. Hallmarks of endothelial cell metabolism in health and disease. Cell Metab. 30, 414–433 (2019).
Lee, H. W. et al. Role of venous endothelial cells in developmental and pathologic angiogenesis. Circulation 144, 1308–1322 (2021).
Joyal, J.-S. et al. Retinal lipid and glucose metabolism dictates angiogenesis through the lipid sensor Ffar1. Nat. Med. 22, 439–445 (2016).
Mackenzie, F. & Ruhrberg, C. Diverse roles for VEGF-A in the nervous system. Development 139, 1371–1380 (2012).
The STOP-ROP Multicenter Study Group. Supplemental Therapeutic Oxygen for Prethreshold Retinopathy of Prematurity (STOP-ROP), a randomized, controlled trial. I: primary outcomes. Pediatrics 105, 295–310 (2000).
Network, S. et al. Target ranges of oxygen saturation in extremely preterm infants. N. Engl. J. Med. 362, 1959–1969 (2010).
Jain, I. H. et al. Hypoxia as a therapy for mitochondrial disease. Science 352, 54–61 (2016).
Bertout, J. A., Patel, S. A. & Simon, M. C. The impact of O2 availability on human cancer. Nat. Rev. Cancer 8, 967–975 (2008).
Hoppe, G. et al. Comparative systems pharmacology of HIF stabilization in the prevention of retinopathy of prematurity. Proc. Natl Acad. Sci. 113, E2516–2525 (2016).
Finley, L. W. S. et al. SIRT3 opposes reprogramming of cancer cell metabolism through HIF1α destabilization. Cancer Cell 19, 416–428 (2011).
Ban, N. et al. Neuroprotective role of retinal SIRT3 against acute photo-stress. NPJ Aging Mech. Dis. 3, 19 (2017).
Lin, J. B. et al. NAMPT-mediated NAD + biosynthesis is essential for vision in mice. Cell Rep. 17, 69–85 (2016).
Lin, J. B., Lin, J. B., Chen, H. C., Chen, T. & Apte, R. S. Combined SIRT3 and SIRT5 deletion is associated with inner retinal dysfunction in a mouse model of type 1 diabetes. Sci. Rep. 9, 3799 (2019).
Kane, A. E. & Sinclair, D. A. Sirtuins and NAD(+) in the development and treatment of metabolic and cardiovascular diseases. Circ. Res. 123, 868–885 (2018).
Oellerich, M. F. & Potente, M. FOXOs and sirtuins in vascular growth, maintenance, and aging. Circ. Res. 110, 1238–1251 (2012).
Williamson, M. R., Fuertes, C. J. A., Dunn, A. K., Drew, M. R. & Jones, T. A. Reactive astrocytes facilitate vascular repair and remodeling after stroke. Cell Rep. 35, 109048 (2021).
Mills, E. L. et al. Accumulation of succinate controls activation of adipose tissue thermogenesis. Nature 560, 102–106 (2018).
Macosko, E. Z. et al. Highly parallel genome-wide expression profiling of individual cells using nanoliter droplets. Cell 161, 1202–1214 (2015).
Satija, R., Farrell, J. A., Gennert, D., Schier, A. F. & Regev, A. Spatial reconstruction of single-cell gene expression data. Nat. Biotechnol. 33, 495–502 (2015).
Villanueva, R. A. M. & Chen, Z. J. ggplot2: Elegant graphics for data analysis, 2nd edition. Meas. -Interdiscip. Res. 17, 160–167 (2019).
Hänzelmann, S., Castelo, R. & Guinney, J. GSVA: gene set variation analysis for microarray and RNA-Seq data. BMC Bioinform. 14, 7 (2013).
Kuleshov, M. V. et al. Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 44, W90–W97 (2016).
Macnair, W., Gupta, R. & Claassen, M. psupertime: supervised pseudotime analysis for time-series single-cell RNA-seq data. Bioinformatics 38, i290–i298 (2022).
Browaeys, R., Saelens, W. & Saeys, Y. NicheNet: modeling intercellular communication by linking ligands to target genes. Nat. Methods 17, 159–162 (2020).
Aibar, S. et al. SCENIC: single-cell regulatory network inference and clustering. Nat. Methods 14, 1083–1086 (2017).
Qiu, X. et al. Reversed graph embedding resolves complex single-cell trajectories. Nat. Methods 14, 979–982 (2017).
Melsted, P. et al. Modular, efficient and constant-memory single-cell RNA-seq preprocessing. Nat. Biotechnol. 39, 813–818 (2021).
La Manno, G. et al. RNA velocity of single cells. Nature 560, 494–498 (2018).
Joyal, J.-S. et al. Subcellular localization of coagulation factor II receptor-like 1 in neurons governs angiogenesis. Nat. Med. 20, 1165–1173 (2014).
Stahl, A. et al. Computer-aided quantification of retinal neovascularization. Angiogenesis 12, 297–301 (2009).
Acknowledgements
We thank Marie-Josée Lacombe, Ferhat Djail, Zhongjie (Kira) Fu and Adriana Di Polo for their technical assistance. We thank Elke Küster-Schöck and the Platform for Imaging by Microscopy of CHU Sainte-Justine Research Center (CHUSJRC), supported by Leica Microsystems and funded by CHUSJRC, the Quebec government, CHUSJ Foundation and Canada Foundation for Innovation and the Vision Health Research Network for funding of the Single-cell Genomics Analysis Platform. GC was supported by a MITACS Elevate fellowship. J.-S.J. was supported by the Burroughs Wellcome Fund, the Canadian Institute of Health Research (CIHR; 390615, 479607, 506601), the National Sciences and Engineering Research Council of Canada (NSERC; 06743), and the Fonds de Recherche du Québec–Santé (FRQS). P.S. was supported by CIHR (353770), Heart & Stroke Foundation Canada (G-16-00014658), Foundation Fighting Blindness Canada, and the Canadian Diabetes Association (DI-3-18-5444-PS).
Author information
Authors and Affiliations
Contributions
G.C., S.P., and J-S.J. conceived and designed all experiments and wrote the manuscript; F.R. and P.S. collected human samples; C.B.C. generated the metabolomic data of human samples; G.C. analyzed the human metabolomics data; B.M. and S.P. performed the carnitine quantification of mouse retinal sample, and G.C. analyzed the data; J.C.R., T.A., A.R., S.P. and P.G. performed the Seahorse experiments; G.C., F.W., S.L., and G.A. generated single-cell RNAseq (Drop-seq) data; G.C., A.S., and M.X.C. analyzed single-cell RNAseq data; S.P., J.S.K., N.R.H., A.Das, T.A., A.R. and C.B. performed OIR experiments and phenotypic quantification; S.P, J.S.K., E.H., N.R.H., T.A., J.C.R., N.K., L.B. and A.R. performed in vivo and in vitro metabolic experiments; J.C.R. performed intravitreal injection and immunohistochemistry experiments; A.R. performed in vitro culture and qPCR analysis on astrocytes; E.H. performed RNAscope experiments; C.B. performed ERG experiments; S.C.G. provided graphic design expertise; A.Dubrac., L.E.H.S. and P.S. offered valuable insight regarding retinal vascular biology; all authors analyzed the data.
Corresponding author
Ethics declarations
Competing interests
The authors have no conflicts of interest to declare relevant to this article’s content. F.R. is an advisory board member for Bayer AG (Germany) and F. Hoffmann-La Roche AG (Switzerland). P.S. is the founder and Chief Scientific Officer of SemaThera Inc. (Montreal, Canada) and Chief Scientist of UNITY Biotechnology (California, US) and holds equity in both companies.
Peer review
Peer review information
Nature Communications thanks Rui Chen, and the other, anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cagnone, G., Pundir, S., Betus, C. et al. Metabolic reprogramming of the neovascular niche promotes regenerative angiogenesis in proliferative retinopathy. Nat Commun 16, 5377 (2025). https://doi.org/10.1038/s41467-025-60061-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-60061-4